ABSTRACT
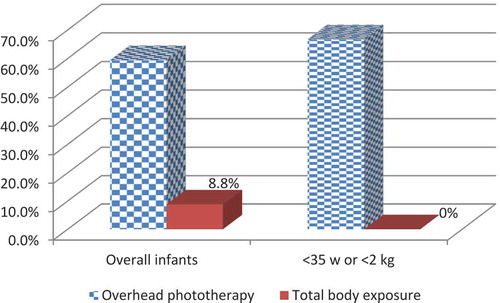
Background: In Nigeria, neonatal jaundice is commonly treated by overhead phototherapy with neonates lying supine, often with effective exposure of less than one half of the body surface. Total body exposure in phototherapy has been in use for less than 2 years in Nigeria, but is available in only five neonatal centres.
Aim: To compare the effectiveness of total body exposure (TBPE) with the conventional partial exposure (COPT) for treatment of hyperbilirubinaemia.
Methods: Eleven datasets from 10 neonatal units across Nigeria were retrieved. They included neonates with severe hyperbilirubinaemia treated with TBPE using the Firefly® device (MTTS Asia) as a test group. The remainder of the patients, the controls, were treated with COPT. Any requirement for exchange blood transfusion (EBT) in either group was documented. Total serum bilirubin (TSB) >213.8 μmol/L (12.5 mg/dL) was treated as severe hyperbilirubinaemia. The efficiency of the intervention was determined according to the time taken for a severe case to be downgraded to mild at ≤213.8 μmol/L.
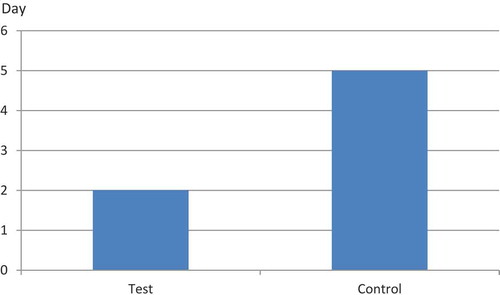
Results: A total of 486 patients were studied, 343 controls and 143 cases. Mean (SD) postnatal age was 6 days (0.7) for cases and 5 (0.9) for controls, for gestational age (GA) in completed weeks was 36 (0.5) for cases and 37 (0.7) for controls and for birthweight was 2.7 kg (0.25) for cases and 2.7 (0.22) for controls. Mean (SD) pre-intervention TSB was 299.3 (35.7) μmol/L for cases and 327.3 (13.9) for controls. Severity downgrade day was Day 2 (0.4) for cases and Day 5 (1.1) for controls. Overall relative EBT rate was 6% for cases and 55% for controls (p= 0.0001), and early preterm relative EBT rate was 0% for cases and 68% for controls (p < 0.01).
Conclusion: TBPE was quicker and safer for reduction of hyperbilirubinaemia and patients rarely required EBT. TBPE is recommended for rapid reduction of serum bilirubin levels and the reduction of treatment costs, morbidity and mortality in low- and middle-income countries.
Abbreviations: EBT, exchange blood transfusion; TBPE, total body exposure technique; COPT, conventional partial exposure; TSB, total serum bilirubin; SB, serum bilirubin; NNJ, neonatal jaundice; SCNU, special care neonatal unit; LMIC, low- and middle-income countries; HIC, high-income countries; LED, light-emitting diode
Introduction
Hyperbilirubinaemia is the accumulation of abnormally high levels (17.1 μmol/L or >1 mg/dl) of unconjugated, non-polar, lipid-soluble bilirubin [Citation1]. The most important causes of neonatal jaundice (NNJ) in Nigeria are associated with outborn infants, especially with late presentation, glucose-6-phosphate dehydrogenase deficiency, prematurity, infection and blood groups ABO incompatibility [Citation2]. The condition is usually benign (physiological jaundice) [Citation1], except in severe cases which are usually associated with delay in diagnosis and lack of effective therapy. Associated risks include acute and chronic bilirubin encephalopathy [Citation3] and other long-term morbidities such as hearing impairment, cerebral palsy, especially the choreoathetoid type [Citation4], epilepsy, speech and language disorders, mental retardation and the wider complications of kernicterus spectrum disorders [Citation5,Citation6].
With improvements in prevention and treatment, the incidence of severe neonatal hyperbilirubinemia and associated morbidities has decreased significantly in high-income countries (HIC) [Citation7]. In contrast, it remains a major disorder in many low- and middle-income countries (LMIC). Mortality from neonatal hyperbilirubinemia is estimated to be 119/100,000 in LMIC compared with 1/100,000 in HIC [Citation7]. Similarly, the incidence of kernicterus is estimated to be 73/100,000 in LMIC compared with 2.7/100,000 in HIC. In Nigeria, 23–60% of neonatal admissions are owing to hyperbilirubinaemia with the diagnosis of bilirubin encephalopathy and kernicterus in 2.3–3.4% of these cases [Citation8,Citation9]. However, the reported incidence of bilirubin encephalopathy is likely to be an underestimate owing to poor follow-up and a lack of routine hearing screening for infants treated for NNJ. This is reflected in a recent community-based study of screening infants for hearing using oto-acoustic emission and auditory brainstem response audiometry [Citation2]. It was reported that 17.3% of those who failed the test had severe hyperbilirubinaemia treated with phototherapy while 11.3% had additional exchange blood transfusion (EBT). A study in south-east Nigeria found that 16.9% of neonates admitted to the special care baby unit required EBT with an associated mortality of 17.5% [Citation10]. In standard Nigerian practice, neonates with jaundice are treated with overhead phototherapy and EBT, depending on the total serum bilirubin (TSB) level. Paediatricians work without photo-radiometers but intuitively identify the more effective phototherapy units at their centres, such as those with newer fluorescent tube replacement or newer LED models and they therefore assign these to neonates with very high TSB values.
Effective first-line management with phototherapy requires light emission spectra with bilirubin absorption of 400–520 nm, irradiance of ≥10 µW/cm2/nm, optimised duration of exposure to light and exposure to the light of ≥80% of the neonate’s body surface area [Citation11]. The surface area exposure can be increased by removing the clothing and increasing the number of lights or lighting devices used to deliver phototherapy. However, in a majority of health-care facilities in Nigeria, these requirements are largely unmet [Citation11]. This has resulted in high rates of EBT, prolonged hospital stays and long-term complications of severe NNJ owing to sub-therapeutic phototherapy coupled with late presentation [Citation11,Citation12]. Owing to the potential exposure to infection which increases morbidity, neonatal EBT is a time-consuming and high-risk procedure [Citation13]. Some Nigerian centres have introduced other treatment variables which could help to reduce the need for invasive EBT with its attendant high risks. Some of these include: (i) the use of light reflective foil to maximize the reach of phototherapy light rays [Citation14]; (ii) algorithms for rigorous classification of diagnoses to carefully select a preferred combination of treatment options; (iii) placing LED phototherapy units at varying distances between the light source and the patient [Citation3]; and (iv) anticipatory techniques and prophylactic interventions which include rehydration of the neonate, administration of intravenous albumin and early initiation of phototherapy for all very low-birthweight infants [Citation15,Citation16]. All of these are practised across Nigeria with little modification; hence, there are small inter-centre variables which have not been shown to create significant differences in overall outcome across the country. However, the fundamental techniques of overhead phototherapy and EBT have remained the most common and consistent therapies across all Nigerian centres, irrespective of the variables in use. EBT is used as an emergency measure when cases become extremely severe, regardless of the mode of treatment.
A prospective study from Myanmar actively applied a combination of photo-radiometer, LED phototherapy units and staff-training to ensure that neonates received intensive phototherapy, delivering irradiance of 40 μW/nm/cm2 which was up to five times more intensive than that previously achieved with conventional blue-light fluorescent tubes [Citation13]. The study resulted in relative EBT reduction of up to 68% for neonates born in one of the participating hospitals [Citation13]. A good number of Nigerian centres apply overhead LED phototherapy units in small numbers but not with similarly effective combinations of photo-radiometer as demonstrated in Myanmar. Hence, to improve child survival in Nigeria, there is a need for a more radical interventional technique to reduce the number of neonates requiring EBT for neonatal jaundice whilst also intensifying efforts at prevention and to achieve early diagnosis. Specially designed, double-sided LED units capable of delivering total body irradiation of the neonate do exist in Nigeria but only in small numbers in five neonatal centres. This study therefore aimed to assess the outcome across entire regions of Nigeria and to investigate whether total body phototherapy exposure (TBPE) may achieve a better result than the currently popular conventional overhead phototherapy (COPT) using fluorescent tubes and LED lights.
It is hypothesized that the use of effective TBPE can significantly reduce the number of neonates requiring invasive EBT.
Materials and methods
A comparative investigatory protocol to establish the outcomes of treatment of severe NNJ in Nigeria was designed. This involved a multi-centre study involving special care neonatal units (SCNU) at tertiary neonatal referral hospitals across all geographical regions (). Data were extracted from previous case notes of cases of severe NNJ in all the participating hospitals. Two groups of datasets were extracted for controls and the test group (cases).
Table 1. National distribution of the participating hospitals.
SCNUs were recruited on the basis of confirmation that they used COPT as the primary intervention and additional EBT as an emergency measure for treatment of severe hyperbilirubinaemia. The models of the overhead devices and any variation in practices to enhance the effectiveness of COPT such as reflective foil were not considered separately. Therefore, extracted COPT intervention data retrospectively reflected the actual and real-time odds and advantages of phototherapy in Nigeria before the concept of total body irradiation. All the recruited SCNUs used eye-shields and nappies to protect patients during the intervention. They also all adhered to a practice whereby practitioners assessed intuitively the effectiveness of the phototherapy and the more effective systems were assigned to neonates with higher TSB. The TBPE group involved similar SCNUs which practised the same standards, but in addition, applied devices that could deliver total body irradiation. The common TBPE standards at the recruited centres involved delivering up to 6 h of total body irradiation as the first course of treatment to neonates presenting with excessively high TSB. A data extraction proforma was designed on a Microsoft Excel spreadsheet to enable each participating centre to retrieve all relevant study information for every neonate included based on a set of predefined criteria. Information on devices’ irradiance or frequency of light source replacements at the ‘control’ SCNUs was not normally documented and could therefore not be assessed. Control data from all the hospitals were extracted retrospectively and restricted to cases who presented after June 2016 but within consecutive months of practice covering up to 12 months but not fewer than 5 months (). Cases were identified and case notes retrieved from the records departments. Information extracted from each case note included birthweight, gestational age, postnatal age in days at commencement of treatment, mode of treatment (COPT, EBT or both), serum bilirubin (SB) levels (total and glycated) at commencement of treatment and levels measured after 6, 12 and 24 h and daily thereafter until discharge. Severe jaundice was frequently defined as an SB level >213.8 μmol/L (12.5 mg/dL) for term and late preterm neonates (35 completed weeks) and an SB >171 μmol/L (10 mg/dL) for birthweight <2000 g or early preterm neonates of <35 completed weeks gestation [Citation16]. Mild jaundice was defined as SB less than or equal to these levels. The data submitted by each hospital were used to determine how the combination of COPT and any other variable in application relied on EBT intervention to achieve a successful outcome. This was determined on the basis of the number of cases who successfully received additional EBT as a proportion of all successfully treated neonates. Daily records of SB during the treatment period were used to identify how many days it took for SB to fall below the critical values of 213.8 or 171 μmol/L.
Four hospitals, in Southern Nigeria (T1 and T4) and Northern Nigeria (T2 and T3), participated as test-group centres (cases). These were among the very few Nigerian hospital SCNUs in which TBPE was available for treating NNJ. Each of the test-group SCNUs accomplished total body irradiation using the Firefly® phototherapy system (MTTS Asia, Hanoi Vietnam; ). The Firefly machine is designed to radiate both from above and below the body, delivering irradiance of up to 32μW/nm/cm2 from the top light source and 36μW/nm/cm2 from the bottom [Citation17]. It is available in Nigeria at a cost equivalent to US$2000 and two were in use at each of the test-group centres. The test-group hospitals used TBPE as the first course of treatment for neonates presenting with severe hyperbilirubinaemia. Data were extracted from the files of neonates who received TBPE in a fashion similar to that of the controls. Neonates were matched across the groups on the basis of significant similarities of centre averages of birthweight, gestational age, TSB on admission and postnatal age (null hypothesis p < 0.05). The submission from each SCNU was independently analysed and used to compare outcomes from COPT datasets. The Federal Teaching Hospital in Abakaliki submitted dataset C1, covering a period from February 2017 to January 2018 when the centre had no facility for TBPE. Beyond this date, they used the Firefly devices, thus facilitating submission of the T1 dataset extracted between February 2018 and January 2019. This allowed a special opportunity for intra-centre comparison of outcome, particularly how introduction of TBPE affected the need for EBT in the SCNU.
Figure 1. Firefly® total body irradiation phototherapy system. Photograph reproduced with the permission of MTTS Asia, Hanoi, Vietnam. System delivers phototherapy irradiation to neonate in both directions, above and below.

Inclusion/exclusion criteria
Datasets submitted by some of the hospitals revealed cases with incomplete or missing SB information. All neonates identified as having died during treatment were excluded from analyses as this comparative investigation was restricted to successful cases only. Also excluded were cases without clearly identifiable methods of treatment and those with total SB lower than the set critical values for severe NNJ. All successful cases for whom SB was recorded on admission but with no SB values after commencement of treatment were included only for comparison of methods of treatment. The common practice at all the test centres was to apply TBPE as the first choice of intervention ahead of EBT in all cases classified as severe hyperbilirubinaemia; hence, any submitted test case was removed if records showed that EBT was undertaken before TBPE.
Statistical analysis
Justification for comparing data from all the hospitals was based on the null hypothesis that the sample populations from all centres were not significantly different in terms of birthweight, gestational age, TSB and postnatal ages at presentation, and quantified from the two-tailed distribution t-test of the groups’ sample means. Statistical interpolation and extrapolation techniques were applied to estimate the SB for missing day records, as long as the recorded days after commencement of treatment were adequate for statistical application [Citation18]. The available SBs in each case were used to compute infants’ mathematical best-fit linear, and its non-linear quadratic and third-degree polynomial regression models [Citation19]. Computed SBs were related to the actual values. The resultant coefficient of correlation for each model was computed, and the model with the highest coefficient was used to interpolate or extrapolate to predict the missing values. The EBT rate for each of the control hospitals was computed over the audit period. This was the fraction of the successful cases requiring EBT for survival. This was used as the survival index factor in a two-tailed t-test analysis to test the significance level of the differences in EBT rates between SCNUs in the two groups (significance set at p = 0.05).
Results
Mean (SD) gestational age of the control group was 37 (0.7) completed weeks and 36 (0.5) weeks for the test group; mean (SD) birthweight of the controls was 2.7 (0.22) kg and 2.7 (0.25) kg for the test group; mean (SD) point-of-admission TSB was 327 (13.9) μmol/L in the controls and 299 (35.7) μmol/L for the test group; and mean (SD) postnatal age on admission was 5 (0.9) completed days for the controls and 5 (0.7) days for the test group. There were no significant differences between these neonatal parameters across all centres ().
Table 3. Data quality applicability and likelihood of EBT in accepted datasets.
Five of the 16 hospitals initially invited to participate were excluded because of their inability to produce useful retrospective data for comprehensive analyses, either for the control or test groups. Eleven sets of SCNU data from 10 tertiary hospitals were assessed to be above the minimum quality for inclusion in the study. None of the datasets included was able to document or demonstrate complete daily assessment of patients’ SB for the entire duration of treatment. Some patients’ entries contained few or no records of SB after the initial admission value was entered. A total of 347 individual neonatal entries representing 71% of all cases in the accepted datasets qualified for assessment of EBT rates. Altogether, 320 neonatal cases representing 66% of all cases in the accepted datasets were sufficiently comprehensive to compute the average days until SB decreased and was downgraded from severe to mild (). The test centres reported no observed adverse effect of the use of TBPE apart from the side-effects already known such as hyperthermia and dehydration, which also occur with the use of other types of phototherapy [Citation20,Citation21].
EBT was required for many neonates in the control group to guarantee survival but was rarely required for those in the test group (). There was an overall 49% relative EBT rate difference between the two groups which was statistically significant (p < 0.001). In the controls, relatively more (68%) EBT was required for survival of neonates with a gestational age <35 completed weeks or birthweight <2000 g (p < 0.01) (). On average, neonatal conditions were successfully downgraded from ‘severe’ to ‘mild’ on Day 5 in the controls but on Day 2 in the test group (). A χ2 test for significant similarity showed that time to downgrading of SB was similar in the control SCNUs, an average of 5 days (p = 0.93). The test-group SCNUs downgrade day was also similar, an average of 2 days (p = 0.94).
Figure 2. EBT requirement for total (test) and partial (control) body exposure in all study infants.
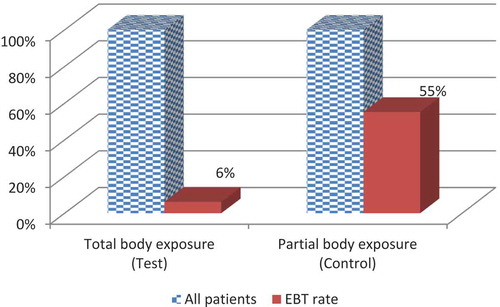
Figure 3. EBT requirement in test and control groups in neonates with a gestational age of <35 w and birthweight of <2000 g.
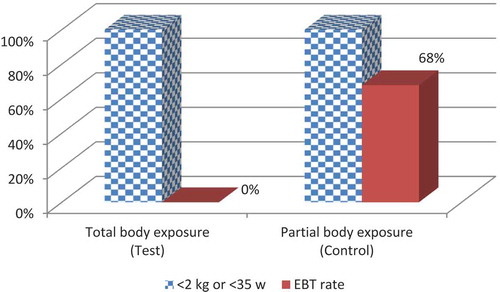
Figure 4. Mean number of days to successful downgrading of serum bilirubin level from severe to mild.
Intra-centre comparison of Abakaliki hospital datasets
In the C1 dataset, 32 cases, 12 of whom were <2 kg or <35 w, qualified for inclusion and in the T1 dataset, 34 cases, 11 of whom were <2 kg or <35 w, qualified for inclusion. Two-tailed t-tests comparing the two datasets did not demonstrate any significant differences between birthweight, gestation, age on admission or TSB on admission; however, there was a significant difference in duration of treatment with averages of Day 2 and Day 6, respectively (p < 0.0001) (). There were higher rates of EBT use in the overhead phototherapy group and EBT was not required for any of the 11 neonates who were <2 kg or <35 w in the TBPE group ().
Table 2. Key infant characteristics by hospital.
Table 4. Key infant characteristics during two periods at Abakaliki hospital.
Discussion
Neonatal jaundice is a major contributor to Nigeria’s high rate of neonatal morbidity and is associated with a greater requirement for EBT, exposing many neonates to the risk of infection and post-treatment auditory problems [Citation2,Citation10]. It is essential that improvement in the treatment of NNJ in LMIC focuses on techniques that could reduce such complications and minimise costs related to lengthy admission. Total body phototherapy irradiation for the treatment of jaundice has been available in Nigeria for less than 2 years and is not yet a common practice. This study demonstrates comparative techniques to measure the relative impact of TBPE in minimising the high rate of EBT and total length of hospital stay. The results show that the total body exposure technique in phototherapy intervention can reduce the high neonatal morbidity and length of hospital stay owing to NNJ throughout Nigeria, similar to results of a prospective study in Vietnam [Citation17]. This study demonstrates a relative reduction in the need for EBT from 55% to 6% across the two audited groups, and the results indicate that high-risk EBT will be significantly reduced by up to 89% when severely jaundiced neonates receive TBPE as a first course of treatment, the current Nigerian practice standards remaining unaltered (p < 0.001, ). A marked reduction or near total elimination of EBT complications would save an enormous amount in terms of materials and clinical/nursing time and, above all, would greatly reduce morbidity and mortality.
The special opportunity presented by the SCNU of the Federal Teaching Hospital, Abakaliki clearly demonstrates the significant differences any Nigerian SCNU could expect with implementation of TBPE using the Firefly system or any other effective device. Similar to the other test hospitals, the Abakaliki hospital did not require EBT for any of their 11 neonates treated with TBPE who were <2 kg or <35 w. This is very different from experience in the same centre during the preceding 12 months when no TBPE was available and 8 of 12 infants required EBT.
Previous prospective studies in Myanmar and Vietnam also found TBPE to be more successful than other techniques [Citation13,Citation17]. However, the present study was carefully designed to rely on retrospective data extracted from centres considered to be among the best Nigerian neonatal units and selected across all regions to fully represent the national situation. Assessments on admission, initial treatment given, evidence-based techniques and daily monitoring of SB were the standards of documentation expected of such referral centres. Data were collected retrospectively rather than prospectively because it was thought that this would more clearly indicate the true standards in Nigerian practice when ‘no one was watching’. It was suspected that a typical Nigerian centre might quickly set up ideal situations in response to pre-announced, prospective data collection; hence, study outcomes would not represent true everyday practices. None of the invited or participating centres was aware of the full details of the investigative methodology until datasets had been received. The true situation at every centre was recorded and analysed. The prospective studies in Myanmar and Vietnam reported fewer days of treatment than the 5 days in the present study [Citation13,Citation17]. The greater duration in the present study might have been owing to the well known frequent and unannounced power-cuts of several hours in Nigerian hospital centres; a reported 1 day of electricity-dependent phototherapy in Nigeria could actually be fewer than 10 h of intervention [Citation22].
The comprehensive data extraction spreadsheet given to the 16 carefully selected SCNUs was sufficient for each centre to retrieve the essential clinical information which was documented whilst the infant was being treated. Patient files were expected to have captured the requested information and it was emphasised that all spreadsheet cells should be completed; however, to discourage data ‘doctoring’, it was further stressed that it would not matter if cells were empty if such information was missing from the patient file. Therefore, it was concluded that every empty cell represented information not documented during the actual treatment of the neonate. The exclusion of five of the 16 SCNUs (>31%) as a result of poor data quality suggests a worrisome situation in Nigeria neonatal practice. The remainder of the datasets were often subjected to statistical interpolation/extrapolation in order to enhance their applicability. The presence of large numbers of empty SB cells in the spreadsheets suggested that many treatments were given on the basis of judgment of skin colour rather than actual measurement of SB. Infrequent measurement of SB might be owing to a lack of adequate funding for the tests, but this deficiency must be addressed in Nigeria and other LMIC settings.
To conclude, TBPE has demonstrated a marked reduction in the use of EBT and its complications and also a 60% reduction in hospital stay (). The use of effective devices for implementing TBPE is therefore recommended to supplement or replace overhead phototherapy as the first choice for treating severe hyperbilirubinaemia in LMICs.
Acknowledgments
This project was independently funded by Neonatal Concerns for Africa without any conflicts of interest. H. Amadi’s neonatal work in Nigeria was partly supported by Hornchurch Baptist Church, England, UK. The assistance of Dr Ukadike Ugbolue is appreciated.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Notes on contributors
Hippolite O. Amadi
Hippolite Amadi is professor of medical engineering and technology at Imperial College London, and a consultant clinical engineer with over 25 years of experience in neonatal systems. His interest is in clinical systems investigation and development of frugal medical devices/procedures appropriate for low- and middle-income countries of the world. He has held a visiting consultant position at over 25 tertiary neonatal centres across all geographical zones of Nigeria enabling a full national coverage of his research group.
Ruqayya A. Abdullahi
Ruqayya A. Abdullahi is a senior medical officer at the neonatal unit of Jummai Babangida Maternal Neonatal Hospital, Minna. She has 12 years’ experience in clinical practice with special interest in maternal and paediatric health, particularly jaundice and thermal control in the newborn.
Olugbenga A. Mokuolu
Olugbenga A. Mokuolu is a Professor of Neonatology with over 24years of experience in care of the Newborn. He is very passionate about use of appropriate technology in saving the lives of newborns in resource-challenged settings.
Obumneme B. Ezeanosike
Obumneme B. Ezeanosike is a Consultant Neonatologist and Head of the Neonatology unit of the Federal Teaching Hospital Abakaliki, Ebonyi State Nigeria. He has interests in Clinical Trials and Neonatal Pharmacology.
Christiana T. Adesina
Amina L. Abubakar is a consultant obstetrician and Gynaecologist and a Lecturer at the Kaduna State University. Her main speciality is in fetomaternal medicine with interest in neonatology. She also holds a position of senior consultant at Jummai Babangida Maternal Neonatal Hospital, Minna.
Isyaku L. Mohammed
Eyinade K. Olateju is the chief consultant paediatrician with over 14 years of experience as a fellow working with University of Abuja Teaching Hospital. She has keen interest in peri-neonatal medicine including clinical practice and research.
Eyinade K. Olateju
Christiana T. Adesina is a paediatrician with 10years of experience in clinical practice. She is interested in innovative developments focused on reducing childhood mortality in Africa.
Amina L. Abubakar
Bessie Eziechila is a consultant paediatrician/neonatologist and the Head of Paediatrics Department at the Federal Medical Centre Jabi Abuja. She has many years of practise experience with special interest in neonatology.
Mustapha A. Bello
Mustapha Bello is a Professor of Paediatrics involved in Perinatal and Neonatal Care with over 15 years’ experience as a fellow working with the University of Maiduguri and University of Maiduguri Teaching Hospital. Professor Bello is currently the President, Nigerian Society of Neonatal Medicine and has keen interest in peri-neonatal medicine including clinical practice, teaching and research.
Augusta U. Eneh
Isyaku Lawal Mohammed is a Tropical Paediatrician with more than 15 years working experience at Federal Medical Centre (FMC) Nguru, Nigeria. He has passionate concern on the increasing rate of neonatal mortality and morbidly in Nigeria, hence his research investigations to counter this. He has served as the head of paediatrics department at FMC Nguru for over eight years.
Emeka Onwe Ogah
Augusta U. Eneh is Professor of Neonatology at the Paediatrics Department of University of Port Harcourt Teaching Hospital, Nigeria.
Bessie C. Eziechila
Emeka Onwe Ogah is a chief consultant neonatologist with many years’ of experience in the healthcare system. Dr Onwe Ogah formerly served as the head of the neonatal unit of Ebonyi State University Teaching Hospital. He is currently the Chief Medical Director of the Federal Teaching Hospital Abakaliki, Nigeria.
Assumpta U. Chapp-Jumbo
Assumpta Chappjumbo is Associate Professor of Paediatrics with speciality in neonatology at the Paediatrics department of Abia State University Teaching Hospital Aba, Nigeria.
Abdulrasheed Jimoh
Abdulrasheed Jimoh is a senior specialist registrar at Department of Paediatrics of the University of Calabar Teaching Hospital Nigeria with special bias in neonatology. He has over five years’ experience in research and neonatal care.
Jacob J. Udo
Jacob Jackson Udo is a Professor of Neonatology, University of Calabar and Chief Consultant Paediatrician, University of Calabar Teaching Hospital Calabar. He has 24 years’ experience as a consultant with special interest in neonatal prematurity and jaundice.
References
- Stoll BJ, Kliegman RM. Jaundice and hyperbilrubinemia in the newborn. In Kliegman RM, Schor NF, St Geme JW, et al., editors. Nelson textbook of pediatrics. 20th ed. Philadelphia:Elsevier; 2016. p.871.e1.
- Olusanya BO, Wirtz SL, Luxon LM. Community-based infant hearing screening for early detection of permanent hearing loss in Lagos, Nigeria: a cross-sectional study. Bull WHO. 2008;86:956–963.
- Borden AR, Satrom KM, Wratkowski P, et al. Variation in phototherapy practices and irradiance devices in a major metropolitan area. Neonatology. 2018;113:269–274.
- Bhutani VK, Zipursky A, Blencowe H, et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatr Res. 2013;74:86–100.
- Le Pichon JB, Riordan SM, Watchko J, et al. The neurological sequelae of neonatal hyperbilirubinemia: definitions, diagnosis and treatment of the kernicterus spectrum disorders (KSDs). Curr Pediatr Rev. 2017;13:199–209.
- Bech LF, Donneborg ML, Lund AM, et al. Extreme neonatal hyperbilirubinemia, acute bilirubin encephalopathy, and kernicterus spectrum disorder in children with galactosemia. Pediatr Res. 2018;84:228–232.
- Greco C, Arnolda G, Boo N, et al. Neonatal jaundice in low- and middle-income countries: lessons and future directions from the 2015 Don Ostrow Trieste Yellow Retreat. Neonatology. 2016;110:172–180.
- Ogunlesi TA, Dedeke I, Adekanmbi AF, et al. The incidence and outcome of bilirubin encephalopathy in Nigeria; a bi-centre study. Niger J Med. 2007;16:354–359.
- Ochigbo SO, Venn I, Anachuna K. Prevalence of bilirubin encephalopathy in Calabar, South-South Nigeria: a five-year review study. Iran J Neonatol. 2016;7:9–12.
- Ibekwe RC, Ibekwe MU, Muoneke VU. Outcome of exchange blood transfusions done for neonatal jaundice in Abakaliki, South Eastern Nigeria. J Clin Neonatol. 2012;1:34.
- Cline BK, Vreman HJ, Faber K, et al. Phototherapy device effectiveness in Nigeria: irradiance assessment and potential for improvement. J Trop Pediatr. 2013;59:321–325.
- Olusanya BO, Osibanjo FB, Mabogunje CA, et al. The burden and management of neonatal jaundice in Nigeria: a scoping review of the literature. Niger J Clin Pract. 2016;19:1–16.
- Anorlda G, Thein AA, Trevisanuto D, et al. Evaluation of a simple intervention to reduce exchange transfusion rates among inborn and outborn neonates in Myanmar, comparing pre- and post-intervention rates. BMC Pediatr. 2015;15:216.
- Patel A, Owa JA, Harvey D. Use of aluminum foil in phototherapy. Niger J Paediatr. 1992;19:93–95.
- Maisels MJ, Watchko JF. Treatment of jaundice in low birth weight infants. Arch Dis Child Fetal Neonatal. 2003;88:459–463.
- Hansen TWR. Therapeutic approaches to neonatal jaundice: an international survey. Clin Pediatr. 1996;35:309–316.
- Arnolda G, Chien TD, Hayen A, et al. A comparison of the effectiveness of three LED phototherapy machines, single- and double-sided, for treating neonatal jaundice in a low resource setting. PLoS One. 2018;13:e0205432.
- Karadzhov GE, Milman M. Extrapolation theory: new results and applications. J Approx Theory. 2005;133:38–99.
- Amadi HO, Gupte CM, Lie DTT, et al. A biomechanical study of the meniscofemoral ligaments and their contribution to contact pressure reduction in the knee. Knee Surg Sports Traumatol Arthrosc. 2008;16:1004–1008.
- Zhang XR, Zeng CM, Liu J. Effect and safety of intensive phototherapy in treatment of neonatal hyperbilirubinemia. Chinese J Contemp Pediatr. 2016;18:195–200.
- Sherbiny HS, Youssef DM, Sherbini AS, et al. High-intensity light-emitting diode vs fluorescent tubes for intensive phototherapy in neonates. Paediatr Int Child Health. 2016;36:127–133.
- Amadi HO, Osibogun AO, Olateju EK, et al. Challenges and frugal remedies for lowering facility based neonatal mortality and morbidity: a comparative study. Int J Pediatr. 2014;2014:986716.
Table A1. Audit period by hospital.