Abstract
Introduction: Anxiety disorders are highly prevalent in individuals with autism spectrum disorder (ASD), but knowledge is limited regarding identification and treatment of these disorders in individuals with ASD and more severe levels of intellectual disability (ID). The current case study aims to explore and describe the inpatient, psychiatric assessment in an adolescent male with ASD, severe ID and self-injurious behaviour (SIB) who was diagnosed with a co-occurring anxiety disorder. The study further aims to explore the implications of this diagnosis for subsequent intervention and care, including management of SIB.
Materials and methods: Case study including multimodal, psychiatric assessment and subsequent intervention.
Results: Following changes in care strategies attempting to incorporate the understanding of anxiety/trauma as contributing to SIB, a reduction of SIB was observed, and this reduced frequency was maintained when the patient was discharged from the inpatient setting.
Conclusions: Though no causal inferences are possible, these experiences indicate that further research is needed regarding possible associations between SIB and anxiety in individuals with ASD, including implications for treatment. Experiences from the current case further indicate that it is possible to recognize and diagnose anxiety disorder in complex cases involving ASD, severe ID, limited verbal language skills, and severe SIB.
Introduction
Identification of psychiatric disorder in individuals with autism spectrum disorder (ASD) and intellectual disability (ID) is generally challenging (Rosen et al. Citation2018, Bakken et al. Citation2016a, Helverschou et al. Citation2011a). Individuals with ASD and ID often have difficulties in self-report of symptoms, and even use of multiple informants may not compensate for this with regard to intra-psychic phenomena (Helverschou et al. Citation2020, Santore et al. Citation2020, Kildahl et al. Citation2017). There is a lack of appropriate diagnostic instruments and symptoms of ASD may overlap with symptoms of psychiatric disorder (Appleton et al., Citation2019, Helverschou et al. Citation2011a). Symptoms of psychiatric disorder may also present in atypical or unusual ways (Rosen et al. Citation2018, Helverschou et al. Citation2011a). Finally, there is a risk of diagnostic overshadowing (Reiss et al. Citation1982), where symptoms of psychiatric disorder are misinterpreted and misattributed to the underlying condition(s) rather than a co-occurring disorder. These challenges are increased for individuals with ASD and co-occurring ID (Bakken et al. Citation2016a), in particular in cases of severe or profound levels of ID, and are present for the entire range of psychiatric disorders, including anxiety- and trauma-related disorders (Kildahl et al. Citation2020a, Citation2019a, Appleton et al. Citation2019, Kerns et al. Citation2015, Citation2014, Mevissen et al. Citation2016, Bakken et al. Citation2016a, Helverschou et al. Citation2011a).
One of the atypical ways symptoms of psychiatric disorder may manifest in individuals with ASD and ID is as “challenging” behaviours, including self-injurious behaviours (SIB) (Rittmannsberger et al. Citation2020, Painter et al. Citation2018, Bitsika et al. Citation2016, Rzepecka et al. Citation2011). “Challenging” behaviours are complex social phenomena developing due to transactional processes between the individual and contextual/social factors (Wolkorte et al. Citation2019, van den Bogaard et al. Citation2019, Cooper Citation2016, Hemmings Citation2007, Emerson Citation2001). Studies investigating the views of people with ASD/ID have reported that a wide range of causes may contribute to these behaviours (van den Bogaard et al. Citation2019), including lack of structure and clarity in their daily lives leading to feelings of fear and restlessness (Wolkorte et al. Citation2019). However, the relationship between “challenging” behaviours and psychiatric disorder remains poorly understood (Cooper Citation2016). While these behaviours may constitute behavioural manifestations of psychiatric disorders, including anxiety and trauma-related disorders (Kildahl et al. Citation2020b, Citation2019a, Bakken et al. Citation2016a, Kerns et al., Citation2015, Helverschou et al. Citation2011a, Bitsika et al. Citation2016, Rzepecka et al. Citation2011), particularly in more severe levels of ID (Painter et al. Citation2018), all instances of problematic behaviours are unlikely to be associated with underlying psychiatric disorder (Cooper Citation2016, Hemmings Citation2007, Emerson Citation2001).
Anxiety disorders are a group of psychiatric disorders primarily characterised by feelings of worry and fear (DSM 5; American Psychiatric Association, Citation2013). Individuals with ASD are particularly vulnerable to anxiety disorders (Nimmo-Smith et al. Citation2020, Kerns et al., Citation2020, Hollocks et al. Citation2019, van Steensel et al., Citation2011, Bakken et al. Citation2010, Simonoff et al. Citation2008). Even though 37-45% of individuals with ASD are estimated to have a co-occurring ID (Rivard et al. Citation2015, Lai et al. Citation2014), research to date has primarily examined anxiety disorders in people with ASD and average to above average IQs (Appleton et al. Citation2019, Hollocks et al. Citation2019, Postorino et al. Citation2017). In a recent review, Appleton et al. (Citation2019) identified only two studies reporting prevalence of anxiety disorders in individuals with co-occurring ASD and ID; 43% in children (Sukhodolsky et al. Citation2008) and 37% in adults (Bakken et al. Citation2010, Helverschou et al. Citation2011b). These numbers suggest that anxiety disorders constitute a significant clinical issue in individuals with ASD and co-occurring ID, but knowledge regarding identification and treatment remains limited, particularly for individuals with severe or profound levels of ID (Appleton et al. Citation2019).
Green (Citation2020) recently suggested that the understanding of problems involving anxiety in ASD merely as co-morbidities that are analogous to presentations in typically developing individuals may be over-simplistic. This is in line with findings in a recent study from Kerns et al. (Citation2020, Kerns et al. Citation2014) who identified two broad types of anxiety-related problems in children with ASD: DSM-specified anxiety disorders and ‘distinct’ anxiety presentations. The latter was only found in children with ASD, not in the typically developing comparison group, and included fear of change, as well as fears associated with special interests, idiosyncratic stimuli, and social confusion. The DSM-specified anxiety disorders were more common in children with average or higher IQs, while the ASD-specific anxieties were not related to intellectual abilities. Other studies have found associations between anxiety and intolerance of uncertainty or insistence on sameness in children with ASD (Baribeau et al. Citation2020, Keen et al. Citation2019, Joyce et al. Citation2017, Boulter et al. Citation2014). Kerns et al. (Citation2020) also noted that the sensitivities of anxiety scales were moderate to poor, particularly so for children with ID. While some findings indicate that prevalence of anxiety disorder may be associated with either lower (van Steensel et al. Citation2011) or higher (Sukhodolsky et al. Citation2008) levels of intellectual functioning, others have concluded that intellectual ability may have bigger effects on the presentation of anxiety disorder rather than its prevalence in individuals with ASD (Kerns et al. Citation2020, Kerns et al. Citation2012).
Also for treatment, most research on anxiety disorder in individuals with ASD has focussed on individuals with average to above average IQs (Appleton et al. Citation2019, Postorino et al. Citation2017). Current knowledge regarding treatment for anxiety disorder in ASD and mild/moderate ID seems to be limited to case studies (Moskowitz et al. Citation2017b, Chok et al. Citation2010), while in severe/profound ID the published case studies have primarily focussed on behavioural treatment of problematic avoidance (Rosen et al. Citation2016), targeting phobic avoidance of specific situations or stimuli. In spite of previous studies identifying associations between anxiety disorders and SIB in youth with ASD (Kerns et al., Citation2015), treatments targeting more complex manifestations of anxiety have been sparsely described in individuals with ASD and severe levels of ID.
The current study aims to explore and describe the psychiatric assessment and subsequent intervention in an adolescent male with ASD, severe ID and SIB who was referred for re-assessment following several unsuccessful attempts of SIB treatment. He was diagnosed with a co-occurring anxiety disorder, and the study aims to explore how this understanding was used to guide care and support for the young man in question.
Materials and methods
Design
Case study methodology (Yin Citation2014) was chosen to explore the assessment and how the understanding gleaned from this assessment was used. There is a lack of real-world investigations into ASD interventions, and case studies are viewed as making helpful contributions to the field (Bulkeley et al. Citation2013).
Research ethics
The study was approved by the Data Protection Official at the Oslo University Hospital and consent was provided by the patient’s parents/legal guardians. The patient has been anonymised.
Case description
Referral and background
At referral, “Philip” was 16 years old and had diagnoses of ASD and severe ID. He had limited verbal language skills but asked for familiar objects and different kinds of food using single- or two-word utterances. Philip also displayed extensive echolalia, repeating phrases which were challenging to connect to the current situation. Philip was referred to a specialised psychiatric inpatient unit for adults with ASD/ID for re-assessment due to several unsuccessful treatment attempts of his severe SIB.
Philip is the oldest child of unrelated parents. Philip was diagnosed with ASD and unspecified ID when he was 4. The latter diagnosis was later changed to moderate ID, and again to severe ID when Philip was 14. The births of his two younger siblings and his behaviour becoming increasingly challenging for his parents to manage resulted in Philip spending increasing periods of time in a care home during his school-age years. Philip moved into full-time care when he was 10 and into a new care home at 14. He received frequent visits from his family in both homes.
Self-injurious behaviour
At referral, Philip on average had 20-30 daily episodes involving severe head banging against walls or the floor. Attempts to interrupt these episodes by professional caregivers usually led to aggression, including Philip attempting to kick, bite or hit caregivers. Both Philip himself and several caregivers had sustained physical injuries during such episodes. Due to the severity of episodes and caregivers lacking other options to limit physical injury, at the time of the referral SIB was managed by two to three caregivers manually restricting Philip face down on the floor on a rubber mat until episodes subsided.
Philip’s SIB had developed gradually, starting in his preschool years with frequent wrist biting and Philip occasionally hitting his face with his fist. When Philip was about 13 years old, he had an episode of passivity and social withdrawal where he refused to go to school or leave his room, lost weight and seemed generally unhappy. During this episode, his professional caregivers targeted these behaviours as passivity, working systematically to increase Philip’s compliance to everyday demands. These interventions increased his participation in basic tasks such as hygiene, mealtimes and going to school, but it was also during this period that Philip’s SIB became more severe and he started banging his head against hard surfaces. At referral, episodes of SIB had reached a level of severity that limited Philip’s activities and he mostly stayed inside his apartment.
Previous treatment attempts
Several previous attempts had been made to reduce Philip’s SIB. These attempts had included varying strategies from applied behaviour analysis. Reinforcement-based strategies had been attempted initially, with subsequent attempts including overcorrection and punishment-based strategies (see Morano et al. Citation2017). In spite of this, Philip’s SIB had gradually worsened in frequency and intensity. No previous psychiatric assessment had been conducted. Pharmacological interventions had been attempted, including use of antipsychotics, benzodiazepines and antiepileptics, but none of these attempts resulted in any lasting change to the frequency or intensity of Philip’s SIB. At referral Philip received 30 mg. of alimemazine for sleep.
Assessment
Previous studies have emphasized the importance of using multimodal assessment strategies in psychiatric assessment in people with ASD and ID (Helverschou et al. Citation2020, Bakken et al., Citation2016a, Helverschou et al. Citation2011b), in particular to help differentiate ASD symptoms from comorbid psychiatric symptomology (van Steensel et al., Citation2011, Appleton et al., Citation2019). This includes combining general and anxiety-specific assessment tools, direct observation, and interviews with family members and professional caregivers (Moskowitz et al. Citation2017a, Helverschou et al. Citation2020, Helverschou et al. Citation2011b).
Philip was admitted to a specialised, inpatient psychiatric ward for adults with ASD/ID, where a multimodal, six-week assessment was conducted involving use of multiple assessment tools with multiple informants, and clinical observation by different professionals. The team in charge of the assessment consisted of a clinical psychologist, a psychiatrist, mental health and intellectual disability nurses. Professional caregivers from Philip’s home were also present throughout the admission, working alongside ward staff. Ward staff carried out initial observations of Philip in his home on three occasions shortly before his admission.
For assessment of ASD and ID, the Autism Diagnostic Interview-Revised (Lord et al. Citation1994) and the Vineland Adaptive Behavior Scales (Sparrow et al. Citation2005) were used. These instruments were completed separately with Philip’s parents and professional caregivers from his home, and results were in line with Philip meeting criteria for ASD and severe ID.
For psychiatric symptoms, the assessment combined an assessment tool developed for individuals with severe/profound ID: the Diagnostic Assessment of the Severely Handicapped –II (DASH-II; Matson Citation1995), and a tool developed for individuals with co-occurring ASD and ID: the Psychopathology in Autism Checklist (PAC; Helverschou et al. Citation2009). For behavioural symptoms, a tool originally developed to monitor treatment effects in individuals with ID, the Aberrant Behavior Checklist (ABC; Aman Citation2012, Aman et al. Citation1986) was used. These were supplemented with one of the most commonly used conventional assessment tools for psychiatric disorder in children and adolescents, the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (Kiddie-SADS; Chambers et al. Citation1985, Jarbin et al. Citation2017). While the psychometric properties of the Kiddie-SADS in children and adolescents with ASD and ID remain unclear, it has been described as having excellent validity for most major child psychiatric disorders in clinical outpatient samples (Jarbin et al. Citation2017), and as useful in identifying co-occurring psychiatric disorder in children with ASD and ID (Gjevik et al. Citation2015, Citation2011). The Kiddie-SADS was completed separately with Philip’s parents and professional caregivers from his home, while ABC, PAC and DASH-II were completed by his parents, professional caregivers from his home, and a selection of nursing staff from the inpatient ward during the second week of the admission. The PAC and ABC were repeated at discharge and six months after discharge, see .
Table 1. PAC and ABC scores at admission, discharge and follow-up, with reliable change index (RCI).
On the DASH-II, scores were elevated on scales measuring depression, anxiety, and pervasive developmental disorders, as well as challenging behaviour/impulsivity and organic syndrome. There was a high degree of overlap with the results from the Kiddie-SADS, which indicated a former depressive episode, possible panic disorder, unspecified anxiety disorder, unspecified behavioural disorder, as well as ASD. No specific, traumatic incidents meeting criteria for post-traumatic stress disorder were unearthed (American Psychiatric Association, Citation2013), but Philip’s parents and his professional caregivers suggested the possibility that the management of Philip’s SIB, his changes in living arrangements, and having to live full-time in a care home, could all constitute potentially traumatic experiences. These suggestions were made both during the Kiddie-SADS and in more informal conversations. On the PAC, all five scales were on or above the cut-off values, see .
Direct observations were carried out in the ward, both by nursing staff and the psychologist and psychiatrist. It was observed that Philip frequently, up to 20-30 times daily, seemed agitated and restless, displaying more negative, repetitive utterances (e.g. “we’re done now”) and observably dilated pupils. He also seemed more easily startled, smiled less, and gave an impression of being frightened or scared. While these symptoms did not always escalate into SIB, all episodes of severe SIB were precipitated by these symptoms. During SIB these symptoms would continue, and Philip would start sweating – sometimes only in his hands and sometimes all over his body, and display facial redness. During SIB, Philip did not respond to verbal initiatives from staff in the same ways that he did outside of episodes, indicating altered responsivity. Both nursing staff and the psychologist/psychiatrist perceived Philip to be frightened or scared prior to episodes, and panicked during them.
Systematic patterns of external triggers for these behaviours were challenging to identify and they occurred in a wide range of situations. However, there were numerous observations that Philip displayed difficulties waiting for activities, objects or food. These difficulties seemed to be more severe if Philip was going to perform an activity with a member of staff with whom he had not previously done the activity in question, while these difficulties seemed to decrease somewhat if the same staff member initiated the same activity several times. If Philip had to wait, he seemed flustered, stressed and slightly confused, but there were few observations that Philip seemed impatient or tried to start the activity himself.
Diagnostic formulation
There was a high degree of overlap in results from the DASH-II and the Kiddie-SADS, suggesting that Philip might meet criteria for an anxiety disorder, a previous depressive episode, and that he had difficulties involving problematic behaviours and impulsivity. While all scales on the PAC were on or above cut-off values, the score for anxiety was very high, even when compared to previously published results for individuals with co-occurring ASD, ID, and anxiety disorder (Helverschou et al. Citation2009, Citation2011b, Bakken et al. Citation2010, Kildahl et al. Citation2019b). In light of previous findings that anxiety is associated with and has been suggested as a causal mechanism for SIB in individuals with ASD (Oliver et al. Citation2017, Soke et al. Citation2017, Kerns et al. Citation2015), Philip’s history, direct observation, and results from the assessment tools were understood as indicating that Philip met criteria for an anxiety disorder. He was also understood to have gone through a previous, depressive episode, during which his anxiety problems had worsened.
It may be challenging to differentiate physiological activation associated with anxiety from physiological activation due to other causes such as physical activity (Chiu et al. Citation2016). However, Philip clearly displaying signs of physiological activation for several minutes prior to episodes of SIB, was viewed as suggesting that the physical exertion of SIB could not alone explain these symptoms. Specific triggers typical of DSM or ICD anxiety disorder were challenging to identify, and Philip was not able to convey information about his experience of these symptoms verbally. However, it was observed that waiting for an activity or other stimuli occasionally triggered anxiety symptoms and SIB, suggesting that uncertainty (Boulter et al. Citation2014, Bitsika et al. Citation2016, Kerns et al. Citation2020) was one possible trigger for Philip’s anxiety.
Differentiating anxiety and trauma-related symptoms is challenging in people like Philip (Kildahl et al. Citation2020a, Citation2020b, Citation2019a), and it has previously been reported that behavioural management practices involving use of physical restraint may lead to development of post-traumatic stress disorder in individuals with ASD and ID (Kildahl et al. Citation2020a). While the previous strategy used to manage Philip’s SIB may be considered a form of abuse, it is unclear whether it may be considered a traumatic event according to current diagnostic criteria for post-traumatic stress disorder (American Psychiatric Association, Citation2013). Based on direct observation, it was viewed as a possibility that the panic-like state observed in Philip during SIB constituted a behavioural manifestation of re-experiencing or flashbacks (Kildahl et al. Citation2020b), triggered by being held face down on the floor. Because he did not have the verbal language skills to disclose his mental state during these episodes, however, the differentiation between panic, flashbacks and other possible explanations was not possible. Furthermore, as the restrictive management practices had been introduced as a consequence of SIB, their use did not precipitate development of anxiety and SIB. Thus, while a possible trauma reaction due to the use of invasive physical restriction practices were understood as possibly contributing to maintaining or exacerbating Philip’s SIB, SIB was not understood to have developed primarily as a trauma response.
In conclusion, a diagnosis of ICD 10 “mixed anxiety disorder” (World Health Organisation Citation1992) was made due to the observed combination of panic-like states, and observable signs of physiological activation occurring prior to, during, and outside of the panic-like states. Based on the observations and Philip’s developmental history, it was also concluded that Philip had not developed strategies to regulate his own experiences of anxiety beyond SIB, indicating that he would be in need of assistance from staff in the development of more appropriate and less harmful strategies.
Intervention
Due to the short time available in the inpatient ward, the intervention was designed with the aim of being transferrable to Philip’s home. The intervention was fully effectuated two weeks into his six-week stay. Based on the assumption of SIB being anxiety- and possibly trauma related, and in line with literature on anxiety treatment in children emphasizing family/contextual factors (Lebowitz et al. Citation2013) and approaches from mental health nursing (Townsend et al. Citation2018, Bakken et al. Citation2017, Citation2016b, Citation2014), it was assumed that changes to staff behaviour could facilitate changes to Philip’s anxiety and thus his behaviour. Seven goals were chosen for the intervention: (1) changed management of SIB episodes to encompass the contribution of anxiety in these episodes and focussing on reducing anxiety throughout episodes, (2) adapting his care to his assumed levels of anxiety at any time to aid him in reducing his experienced anxiety, (3) facilitate development of alternative behavioural strategies for Philip when he experienced anxiety, (4) aiding all staff involved in Philip’s care to maintain low arousal throughout and outside of episodes involving SIB, (5) reinforce and validate any verbal communication from Philip, (6) facilitate positive activities, (7) reduce uncertainty by aiding Philip in experiencing his days as structured and predictable. No goals were specified concerning reduction of SIB.
Ward staff were already familiar with the different components of the intervention, with many having been previously involved in similar cases. Staff training and discussions regarding adaptions and adjustments to the intervention were conducted in hourly, weekly team meetings and hourly, weekly supervisions for all ward staff and caregivers by the clinical psychologist in charge of the admission. Supervision involved providing all caregivers with specific training in recognising symptoms of anxiety and discussion of the ways in which anxiety symptoms manifested in Philip, as suggested by Helverschou et al. (Citation2011b). In addition, either the psychologist or one of the two nurses in charge of the intervention was present for all shift changes, providing supervision for remaining staff. Finally, staff and caregivers completed weekly, practical training sessions concentrating on the changed restraint policy.
There were no changes in medication during the stay beyond a gradual reduction of alimemazine dosage from 30 to 10 mg. daily. Complete discontinuation was attempted but resulted in earlier awakenings and disturbed sleep patterns. This improved again with reinstating it at 10 mg.
(1) Loss of control is a frequently reported fear in typically developing individuals experiencing panic attacks, as is fear of dying (Raffa et al. Citation2004, Krystal et al. Citation1991). It was hypothesised that the previous management strategy to prevent serious injury during SIB, holding Philip face down on the floor, could be contributing to exacerbating anxiety symptoms or possibly triggering trauma-related symptoms. Held this way, Philip was unable to see who was holding him or observe what was going on around him. A new strategy was devised to allow Philip to have visual overview of the situation and his surroundings during episodes. Whenever use of physical restriction was necessary to avoid injury, caregivers would hold Philip sitting in a large sofa with one caregiver holding each arm/shoulder. A third caregiver would carefully be in control of Philip’s legs by holding a bean bag over them to avoid him kicking caregivers. Risk of biting was managed by caregivers wearing protection on their arms. Due to ethical concerns with the prior strategy, along with the observations made prior to the admission, this changed management of SIB was effectuated within the first day of Philip’s stay.
(2) It was observed that Philip’s levels of physiological arousal fluctuated considerably throughout the day, and thus also his assumed levels of experienced anxiety. The goal of this aspect of the intervention was to allow Philip to repeatedly experience that his anxiety could be decreased without escalating into SIB, and to aid caregivers in identifying effective strategies to reduce Philip’s anxiety before it escalated into SIB. This approach is similar to approaches used in trauma treatment, such as the window of tolerance model (Siegel Citation2012, Bakken et al. Citation2014).
Timing interventions according to Philip’s observed level of physiological activation at any time was a particular focus for this aspect of intervention; for instance if Philip seemed slightly agitated, caregivers would attempt to divert his attention to a positive activity like putting on a song they knew he liked, looking in a book or suggesting going for a walk. If Philip seemed more agitated, tactile sensory diversions were introduced, such as caregivers taking initiative to kick a ball and get Philip to throw or kick it back, offering Philip a snack or a drink. These strategies are similar to those described as “exposure paired with anti-anxiety stimuli” or “counterconditioning” by Moskowitz et al. (Citation2017b) and “anxiety relief” or “grounding” by Bakken et al. (Citation2014). “Grounding” in trauma treatment may refer to any technique that aids the patient in re-establishing an awareness of the present (Kennerley, Citation1996). For patients with ID, it has previously been suggested that such techniques may need to be implemented by caregivers rather than the patient themselves (Bakken et al., Citation2014). For Philip, the hierarchical system of distractors was based on the assumption that more comprehensive, multi-sensory experiences involving some kind of motor activity would be more effective in diverting Philip’s attention at higher levels of agitation, while auditory/visual stimuli would be sufficient at lower levels of agitation. Systematic preference assessment was not possible at admission due to the frequency of SIB, but information about what had previously constituted enjoyable activities for Philip was obtained during informal conversations with his family and professional caregivers and informed the choice of distractors.
During panic-like states and SIB episodes, Philip was not responsive to caregiver communication, and the focus of intervention was to help Philip calm down and feel safe. If Philip was calm and relaxed, caregivers were encouraged to sit down, maintain a nice and calm environment, and occasionally introduce positive activity. This component of the intervention was implemented in the second week of the admission, but required several updates throughout the stay as caregivers used their experiences concerning what was effective at what times to improve their precision in timing initiatives and activities in relation to Philip’s anxiety level.
(3) SIB was understood to have developed as a consequence of anxiety (Oliver et al. Citation2017, Soke et al. Citation2017, Kerns et al. Citation2015), increasing in frequency and severity over time due to operant and automatic reinforcement (Furniss et al. Citation2020). It was hypothesised that Philip would need assistance from care staff to develop alternative behavioural responses to experiencing anxiety. Caregivers were therefore encouraged to observe what Philip did whenever he seemed anxious, both prior to SIB and during anxiety that did not involve SIB. Occasionally, diverting Philip’s attention would help him calm down, but other times his agitation increased quickly to a level where this was not feasible.
In the second week of the admission, Philip started occasionally taking the initiative to be held by staff without engaging in SIB. He would grab a caregiver by the arm while saying “sit” or pull a caregiver by the arm towards the sofa. This was interpreted to suggest that Philip experienced being held in this manner as somehow helpful. To validate and reinforce Philip’s communication of assumed distress prior to becoming severely agitated (Bakken et al. Citation2017) caregivers were encouraged to follow Philip’s initiatives. Episodes where holding had been initiated by Philip himself often escalated with Philip becoming tense or agitated, but rarely resulted in severe SIB, further suggesting that these interactions with staff were helpful to Philip. The frequency of Philip’s initiatives to be held increased gradually during the rest of the admission. These observations also lead to the introduction of a weighted blanket (Mullen et al. Citation2008) by caregivers (week 3), which seemed to help Philip calm down at lower levels of agitation but seemed insufficient when his agitation reached a level of agitation where he would take the initiative to be held.
(4) Low arousal/low expressed emotion in caregivers is viewed as important in the management of problematic behaviours in ASD and ID (McDonnell et al. Citation2015, Greenberg et al. Citation2006). Strategies to maintain lowered arousal in caregivers constitutes a central aspect of the standard approach in the ward, and were implemented from day one of Philip’s admission. To increase the likelihood of caregivers being able to manage SIB while maintaining low arousal, a theoretical understanding of the approach was provided to all caregivers. Because Philip’s behaviour was unpredictable, emphasis was placed on the development of a shared understanding of his abilities and difficulties, rather than the development of a rigorous intervention plan. During episodes of SIB, caregivers worked systematically to lower their own arousal, talking pleasantly among themselves and involving Philip in the conversation. If it seemed like Philip preferred certain caregivers, these were encouraged to maintain the primary interaction with him.
Other problematic behaviours were ignored whenever possible and caregivers showed high tolerance for loud or restless behaviour. If difficult to ignore, for instance when Philip threw food on the floor, the meal continued with staff cleaning up without reacting or commenting. Moreover, the choice not to specify a goal for the intervention concerning reduction of SIB was primarily made to aid caregivers working with Philip to maintain low arousal during SIB episodes, particularly on days where Philip had many such episodes.
(5) SIB and other “challenging” behaviours in ASD and ID may have significant communicative aspects (Soke et al. Citation2017, Carr et al. Citation1987). To counter these, attempting to give Philip the experience of verbal communication as useful, it was emphasised to positively reinforce and/or validate (Bakken et al. Citation2017) any perceived social initiative or verbal communication from Philip. Whenever Philip verbally asked for a specific food, for instance, staff would go to great lengths to provide him with it. Discussions among staff about how to understand Philip’s verbal utterances and other behaviours were encouraged (Donner et al. Citation2020). The emphasis on interpretation of Philip’s communication was implemented during the first week of the admission and was a particular focus during shift changes.
(6) Because so much of Philip’s time had been spent displaying agitation or SIB, and because he made few initiatives, it was chosen to specifically focus on the introduction of positive activity such as listening to music, watching tv, singing a song, going for a walk, getting snacks etc. Play and positive activities were initiated by caregivers, and observations that Philip found an activity enjoyable led to repetition or careful expansion of the respective activity. During previous treatment attempts, activities Philip enjoyed had been used as conditional reinforcements. In the current intervention, attempts were made to avoid connecting enjoyable activity to demands, allowing Philip to seek out or participate in positive activities without conditions. If Philip asked for a snack, he would get it. Introduction of positive activities was systematically implemented during the second week of the admission.
(7) Intolerance of uncertainty seems to contribute in the development of anxiety disorder in individuals with ASD as well as in others (Joyce et al. Citation2017, Boulter et al. Citation2014, Keen et al. Citation2019, Baribeau et al. Citation2020), and has been the target for recently developed interventions for anxiety in ASD (Rodgers et al. Citation2018, Citation2017). Intolerance of uncertainty has also been reported by individuals with ASD/ID themselves to contribute to “challenging” behaviours (Wolkorte et al. Citation2019). To minimise perceived uncertainty and increase predictability and structure for Philip, an attempt was made to re-introduce a visual schedule previously used by Philip’s caregivers. He proceeded to tear it down from the wall, throwing it in a corner. Following several repetitions of this, including several instances where Philip hid the schedule under the sofa, caregivers ceased introducing it. Philip did not look or ask for it. Days were instead organized by introducing activities in the same sequence every day, with caregivers being flexible and allowing Philip to control the pace.
Waiting seemed particularly challenging for Philip and suggested activities had to be carried out immediately to be successful. This was managed by care staff changing the sequence of their own actions to avoid Philip having to wait. Transitions were organized with his perspective in mind, staff preparing the activity before suggesting it to him. This change was fully implemented towards the end of the second week of the admission.
Results
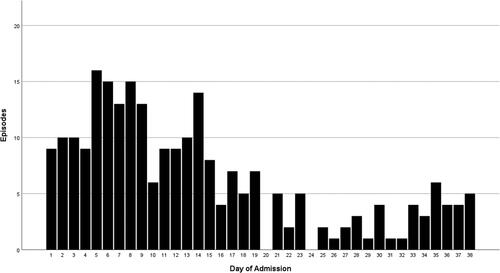
During Philip’s stay, there was a reduction in the frequency of SIB episodes, see . Prior to admission the average number of episodes had been above 20 for several months. In the first two weeks of admission the average number of episodes was above 10, with up to 16 episodes on a single day, while in the last three weeks no day had more than 6 episodes. Parallel to this reduction in the number of episodes, Philip himself started taking the initiative to be held without engaging in SIB. The changed strategy proved sufficient to manage SIB episodes without serious injury to Philip or staff throughout the remaining stay, and Philip was not held on the floor again.
Figure 1. Number of SIB episodes for each day during the admission. The figure was made using SPSS version 25.
The Reliable Change Index (RCI; Bauer et al. Citation2004, Jacobson et al. Citation1991) was used to determine whether the differences in PAC and ABC scores between admission, discharge, and follow-up were significant, see . There was a significant reduction in scores on the PAC scales for psychosis, anxiety, OCD and general adjustment problems, as well as on several ABC scales, from admission to discharge. For the PAC scales, there were no significant changes from discharge to follow-up, while findings for ABC scales were more mixed. However, this may also be due to these reports relying on different informants.
Clinically, it was observed that Philip smiled and laughed more towards the end of the admission, and this change seemed to be gradual. Use of language increased, including an apparent expansion of his active vocabulary. Due to the reduced frequency of SIB, Philip also gained access to activities he had not participated in for years. He spent increasing amounts of time engaged in positive activity, including going for walks and car rides. The principles of the intervention were continued after discharge from the hospital ward. Frequency and intensity of episodes requiring intervention by physical restraint are reported to be further reduced a year after discharge, averaging approximately two daily episodes.
Discussion
In the current case, re-assessment of an adolescent male with ASD, severe ID and SIB unearthed an underlying anxiety disorder which was understood to have contributed to the development of his SIB, and a possible trauma response due to use of an invasive, physical restriction policy in the management of SIB. An intervention was designed based on the understanding of SIB as caused by anxiety and maintained or exacerbated by trauma. The specified aims involved decreasing the patient’s anxiety during SIB episodes, adapting his care to his assumed levels of anxiety at any time to aid him in reducing anxiety, facilitate alternative behavioural responses, lowering staffs’ arousal/expressed emotion, reinforcing all communicative initiatives from the patient, facilitating positive activity, and increasing predictability for the patient and his caregivers. Following this intervention, there was a significant reduction in SIB. However, due to the risk of severe injury and use of restrictive measures, removing and reintroducing the intervention for research purposes was considered unethical. Thus, no causal inferences can be made.
The current study indicates that anxiety disorder is identifiable in ASD and severe ID, even in a complex clinical picture involving SIB. In the current case, PAC, DASH-II, Kiddie-SADS, and clinical observation all proved helpful in identification of anxiety. Reports based on checklists completed by families and professional caregivers may vary according to their previous experience and knowledge regarding manifestations of psychiatric disorder in this population (Kildahl et al. Citation2017). In line with previous suggestions (Appleton et al. Citation2019, Valdovinos et al. Citation2019, Helverschou et al. Citation2011b), direct observation by mental health professionals with specific knowledge and experience concerning psychiatric disorder in ASD and ID may thus be particularly important as the diagnostic complexity increases, and was helpful also in the current study. Recent findings suggest that the challenges present in assessment of psychiatric disorder in this population are present also in evaluation of treatment effects (Rysstad et al. Citation2020), and the use of similar, multimodal strategies proved helpful for evaluation in the current case. This included taking account of observations made by the patient’s family, his professional caregivers and ward staff regarding his condition and development during the admission, as well as systematic monitoring of SIB and use of checklists. While ward staff were able to observe reductions of SIB and anxiety symptoms, observations from the patient’s family were particularly important in interpretation of the patient’s emerging expressions of positive emotionality and initiative.
The current results are in line with previous reports of anxiety in ASD and ID being associated with SIB (Oliver et al. Citation2017, Soke et al. Citation2017, Kerns et al. Citation2015), and the results from Moskowitz et al. (Citation2017b) where problem behaviours decreased as anxiety markers decreased in children with ASD and ID. These findings highlight the importance of conducting thorough psychiatric assessment in cases involving ASD, ID and “challenging” behaviours such as SIB.
Due to several components in the patient’s care being changed simultaneously, no conclusions may be drawn regarding specific mechanisms facilitating the reduction in SIB. However, it may also have been the totality of the current intervention contributing to the observed reduction of SIB. In a recent, comprehensive review of research on SIB in ASD, Furniss et al. (Citation2020) hypothesised that ASD may be associated with generally heightened feelings of threat due to difficulties in recognising and tracking contextual stimuli signalling safety. Building on this hypothesis, they suggested that:
…in cases where people experience “generalized habitual” SIB, a possible intervention is to introduce them to a “safe situation” in which they can experience an environment free from the aversive experiences which initially motivated their SIB and then to use stimuli associated with the safe environment as “safety signals” to indicate the ongoing absence of the aversive experience as the person enter other environments (p. 299).
This understanding implies that future studies on treatment for both SIB and anxiety in individuals with ASD and ID would be recommended to strive not only to identify effective components in interventions, but to comprehensively describe the wider context of the intervention. Intervention and treatment for these issues always occur in complex social systems, and there is a need for future research to examine and describe the contexts and the social systems in which these interventions are carried out. In light of the current results, the suggestion by Furniss et al. ( Citation2020) implies that admission to a specialist hospital ward or similar may be one possible approach in severe cases of SIB if it is used to create a “safe situation” for the individual in question.
The intervention chosen for uncertainty anxiety in the current case may be described as accommodation, i.e. that caregivers changed their behaviours to reduce the patient’s anxiety, which in the anxiety treatment literature is frequently viewed as enhancing rather than mitigating anxiety (Frank et al. Citation2020, Kagan et al. Citation2017, Lebowitz et al. Citation2013). Also the interventions developed by Rodgers et al. (Citation2018, Citation2017) aim to increase flexibility in children and adults with ASD rather than reducing uncertainty. However, it is a basic tenet of anxiety treatments aiming to increase flexibility or tolerance of uncertainty through gradual exposure or similar, that the level of anxiety is tolerable and manageable for the individual concerned (Lebowitz et al. Citation2013). In the current case, the patient was understood to be overwhelmed by anxiety, and part of the intervention involved aiding caregivers in differentiating situations in which accommodation was needed from situations where new activities or stimuli could be introduced. It is thus possible that accommodation is sometimes needed to aid the individual concerned in keeping anxiety within tolerable levels, and that strategies aimed at gradually increasing flexibility need to be timed appropriately to avoid the individual feeling overwhelmed. In the current case, the patient’s flexibility, and thus his access to various activities, increased during the admission.
Moreover, interventions aiming to increase flexibility and tolerance of uncertainty in individuals with ASD have primarily been explored in individuals without co-occurring ID (Rodgers et al. Citation2018, Citation2017). According to theories of emotional development (Sappok et al. Citation2014), individuals with ASD and more severe levels of ID may not be able to understand that their subjective experience of their surroundings does not constitute objective reality, and this has previously been suggested to affect how trauma-related symptoms are experienced and expressed in this population (Kildahl et al. Citation2020b). For anxiety, this may suggest that individuals such as the current patient may have difficulties distinguishing situations that feel dangerous from situations that are objectively dangerous. Because limited verbal language skills limit the use of psychoeducative interventions that frequently constitute part of anxiety treatment (Lebowitz et al. Citation2013), these difficulties may be challenging to alleviate, indicating that strategies for anxiety treatment used in individuals with ASD and average to above average IQs may need considerable adaptation for use with individuals who have co-occurring severe ID.
Suggestions for future research
The current case raises several issues deserving of further study, in particular further investigations of the relationship between anxiety and SIB in ASD and ID, including the possible contributions of level of ID, verbal communication skills and emotional development as moderating or mediating mechanisms in this relationship. While accommodation is often viewed as likely to enhance rather than mitigate anxiety, further studies are needed to explore whether the relationship between accommodation and strategies to increase flexibility may differ for individuals with more severe levels of ID, and how interventions targeting accommodation may be adapted for these individuals. The current study also highlights that the approach suggested by Furniss et al. (Citation2020), that a change of environment involving a “safe space” deserves further empirical examination in cases of severe SIB in ASD and ID where less invasive strategies have proved insufficient. Finally, the current case underlines the importance that future studies describe the wider social context for intervention and treatment of SIB and/or anxiety.
Conclusions
SIB presents a dramatic, profound and sometimes dangerous issue for individuals with ASD and ID, their families and caregivers. More research into the characteristics of SIB in ASD and ID is urgently needed, in particular in more severe levels of ID, as well as investigations of possible associations with psychiatric disorder. While the current study indicates that clinical observation and certain assessment tools may be helpful in the identification of anxiety in ASD and severe ID, there is an urgent need for larger-scale and group studies investigating the identification and treatment of anxiety in this population. Finally, the current case provides an example that treatment of SIB is possible, even in cases where several previous treatment attempts have been unsuccessful. Re-assessment, including investigation of possible psychiatric symptoms, may be helpful in developing more appropriate management strategies.
Acknowledgements
The authors would like to thank Philip, his family and his professional caregivers, as well as the ward staff and Dina Tegle Stenstad for making this study possible.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Aman, M. G. 2012. Annotated biography on the Aberrant Behavior Checklist (ABC). Unpublished Manuscript, June. Columbus, OH: The Ohio State University.
- Aman, M. G. and Singh, N. N. 1986. Aberrant behavior checklist: Manual. East. Aurora, NY: Slosson Educational Publications.
- American Psychiatric Association. 2013. Diagnostic and statistical manual of mental health disorders. 5th ed. Washington, DC: American Psychiatric Association.
- Appleton, H., Roberts, J. and Simpson, K. 2019. How is anxiety identified and diagnosed in individuals with autism spectrum disorder and intellectual disability? A scoping review. Journal of Mental Health Research in Intellectual Disabilities, 12, 152–124. https://doi.org/https://doi.org/10.1080/19315864.2019.1679299
- Bakken, T. L., Gjersoe, V., Matre, E., Kristiansen, T., Ro, A., Tveter, A. L., Hoeidal, S. H. and Kildahl, A. N. 2014. PTSD in adults with intellectual disabilities: Stabilisation during inpatient stay. Advances in Mental Health and Intellectual Disabilities, 8, 237–247. https://doi.org/https://doi.org/10.1108/AMHID-10-2013-0061
- Bakken, T. L., Helverschou, S. B., Eilertsen, D. E., Heggelund, T., Myrbakk, E. and Martinsen, H. 2010. Psychiatric disorders in adolescents and adults with autism and intellectual disability: A representative study in one county in Norway. Research in Developmental Disabilities, 31, 1669–1677.
- Bakken, T. L., Helverschou, S. B., Høidal, S. H. and Martinsen, H. 2016a. Mental illness with intellectual disabilities and autism spectrum disorder. In: C. Hemmings and N. Bouras, eds. Psychiatric and behavioral disorders in intellectual and developmental disabilities. 3rd ed. Cambridge, UK: Cambridge University Press, pp.119–128.
- Bakken, T. L. and Sageng, H. 2016b. Mental health nursing of adults with intellectual disabilities and mental illness: A review of empirical studies 1994–2013. Archives of Psychiatric Nursing, 30, 286–291.
- Bakken, T. L., Sageng, H., Hellerud, J., Kildahl, A. and Kristiansen, T. 2017. The use of validation in mental health nursing for adults with intellectual disabilities and mental illness: A descriptive study. Issues in Mental Health Nursing, 38, 619–623.
- Baribeau, D. A., Vigod, S., Pullenayegum, E., Kerns, C. M., Mirenda, P., Smith, I. M., Vaillancourt, T., Volden, J., Waddell, C., Zwaigenbaum, L., Bennett, T., Duku, E., Elsabbagh, M., Georgiades, S., Ungar, W. J., Zait, A. Z. and Szatmari, P. 2020. Co-occurring trajectories of anxiety and insistence on sameness behaviour in autism spectrum disorder. The British Journal of Psychiatry.
- Bauer, S., Lambert, M. J. and Nielsen, S. L. 2004. Clinical significance methods: A comparison of statistical techniques. Journal of Personality Assessment, 82, 60–70.
- Bitsika, V. and Sharpley, C. F. 2016. Which aspects of challenging behaviour are associated with anxiety across two age groups of young males with an autism spectrum disorder? Journal of Developmental and Physical Disabilities, 28, 685–701. https://doi.org/https://doi.org/10.1007/s10882-016-9502-4
- Boulter, C., Freeston, M., South, M. and Rodgers, J. 2014. Intolerance of uncertainty as a framework for understanding anxiety in children and adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44, 1391–1402.
- Bulkeley, K., Bundy, A., Roberts, J. and Einfeld, S. 2013. ASD intervention research in real world contexts: Refining single case designs. Research in Autism Spectrum Disorders, 7, 1257–1264.
- Carr, E. G. and Durand, V. M. 1987. See me, help me. Psychology Today, 21, 62–65.
- Chambers, W. J., Puig-Antich, J., Hirsch, M., Paez, P., Ambrosini, P. J., Tabrizi, M. A. and Davies, M. 1985. The assessment of affective disorders in children and adolescents by semistructured interview. Test-retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version . Archives of General Psychiatry, 42, 696–702.
- Chiu, T. A., Anagnostou, E., Brian, J., Chau, T. and Kushki, A. 2016. Specificity of autonomic arousal to anxiety in children with autism spectrum disorder. Autism Research : Official Journal of the International Society for Autism Research, 9, 491–501.
- Chok, J. T., Demanche, J., Kennedy, A. and Studer, L. 2010. Utilizing physiological measures to facilitate phobia treatment with individuals with autism and intellectual disability: A case study. Behavioral Interventions, 25, 325–337.
- Cooper, S.A. 2016. Problem behaviors and the interface with psychiatric disorders. In: C. Hemmings and N. Bouras, eds. Psychiatric and behavioural disorders in intellectual and developmental disabilities. 3rd ed. Cambridge, UK: Cambridge University Press, pp.224–230.
- Donner, L. and Gustin, L. W. 2020. Navigating between compassion and uncertainty–psychiatric nurses’ lived experiences of communication with patients who rarely speak. Issues in Mental Health Nursing.
- Emerson, E. 2001. Challenging behaviour: Analysis and intervention in people with severe intellectual disabilities. Cambridge, UK: Cambridge University Press.
- Frank, H. E., Kagan, E. R., Storch, E. A., Wood, J. J., Kerns, C. M., Lewin, A. B., Small, B. J. and Kendall, P. C. 2020. Accommodation of anxiety in youth with autism spectrum disorder: Results from the TAASD study. Journal of Clinical Child & Adolescent Psychology.
- Furniss, F. and Biswas, A. B. 2020. Self-injurious behaviour in individuals with neurodevelopmental conditions. Cham: Springer.
- Gjevik, E., Eldevik, S., Fjaeran-Granum, T. and Sponheim, E. 2011. Kiddie-SADS reveals high rates of DSM-IV disorders in children and adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders, 41, 761–769.
- Gjevik, E., Sandstad, B., Andreassen, O. A., Myhre, A. M. and Sponheim, E. 2015. Exploring the agreement between questionnaire information and DSM-IV diagnoses of comorbid psychopathology in children with autism spectrum disorders. Autism : The International Journal of Research and Practice, 19, 433–442. https://doi.org/10.1177/1362361314526003
- Green, J. 2020. Commentary: Anxiety and behaviour in and beyond ASD; does the idea of 'PDA' really help? - a commentary on Stuart et al. (2020). 2020. Child and Adolescent Mental Health, 25, 74–76.
- Greenberg, J. S., Seltzer, M. M., Hong, J. and Orsmond, G. I. 2006. Bidirectional effects of expressed emotion and behavior problems and symptoms in adolescents and adults with autism. American Journal of Mental Retardation : AJMR, 111, 229–249.
- Halvorsen, M., Aman, M. G., Mathiassen, B., Brøndbo, P. H., Steinsvik, O. O. and Martinussen, M. 2019. Psychometric properties of the Norwegian aberrant behavior checklist and diagnostic relationships in a neuro-pediatric sample. Journal of Mental Health Research in Intellectual Disabilities, 12, 234–255. https://doi.org/https://doi.org/10.1080/19315864.2019.1630872
- Helverschou, S. B., Bakken, T. L. and Martinsen, H. 2009. The Psychopathology in Autism Checklist (PAC): A pilot study. Research in Autism Spectrum Disorders, 3, 179–195.
- Helverschou, S. B., Bakken, T. L. and Martinsen, H. 2011a. Psychiatric disorders in people with autism spectrum disorders: Phenomenology and recognition. In: J. L. Matson and P. Sturmey, eds. International handbook of autism and pervasive developmental disorders. New York: Springer Science & Business Media, pp.53–74.
- Helverschou, S. B., Kildahl, A. N. and Bakken, T. L. 2020. Checklists and structured interviews. In: J. Matson, ed. Handbook of dual diagnosis. Cham: Springer, pp.167–193.
- Helverschou, S. B. and Martinsen, H. 2011b. Anxiety in people diagnosed with autism and intellectual disability: Recognition and phenomenology. Research in Autism Spectrum Disorders, 5, 377–387.
- Hemmings, C. 2007. The relationships between challenging behaviours and psychiatric disorders in people with severe intellectual disabilities. In N. Bouras and G. Holt, eds. Psychiatric and behavioural disorders in intellectual disabilities and developmental disabilities. 2nd ed. Cambridge UK: Cambridge University Press, pp.62–75.
- Hollocks, M. J., Lerh, J. W., Magiati, I., Meiser-Stedman, R. and Brugha, T. S. 2019. Anxiety and depression in adults with autism spectrum disorder: A systematic review and meta-analysis. Psychological Medicine, 49, 559–572.
- Jacobson, N. S. and Truax, P. 1991. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. doi:https://doi.org/10.1037/0022-006X.59.1.12
- Jarbin, H., Andersson, M., Råstam, M. and Ivarsson, T. 2017. Predictive validity of the K-SADS-PL 2009 version in school-aged and adolescent outpatients. Nordic Journal of Psychiatry, 71, 270–276.
- Joyce, C., Honey, E., Leekam, S. R., Barrett, S. L. and Rodgers, J. 2017. Anxiety, intolerance of uncertainty and restricted and repetitive behaviour: Insights directly from young people with ASD. Journal of Autism and Developmental Disorders, 47, 3789–3802.
- Kagan, E. R., Frank, H. E. and Kendall, P. C. 2017. Accommodation in youth with OCD and anxiety. Clinical Psychology: Science and Practice, 24, 78–98.
- Keen, D., Adams, D., Simpson, K., den Houting, J. and Roberts, J. 2019. Anxiety-related symptomatology in young children on the autism spectrum. Autism : The International Journal of Research and Practice, 23, 350–358.
- Kennerley, H. 1996. Cognitive therapy of dissociative symptoms associated with trauma. The British Journal of Clinical Psychology, 35, 325–340.
- Kerns, C. M. and Kendall, P. C. 2012. The presentation and classification of anxiety in autism spectrum disorder. Clinical Psychology: Science and Practice, 19, 323–347. https://doi.org/https://doi.org/10.1111/cpsp.12009
- Kerns, C. M., Kendall, P. C., Berry, L., Souders, M. C., Franklin, M. E., Schultz, R. T., Miller, J. M. and Herrington, J. 2014. Traditional and atypical presentations of anxiety in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 2851–2861.
- Kerns, C. M., Kendall, P. C., Zickgraf, H., Franklin, M. E., Miller, J. and Herrington, J. 2015. Not to be overshadowed or overlooked: Functional impairments associated with comorbid anxiety disorders in youth with ASD. Behavior Therapy, 46, 29–39.
- Kerns, C. M., Winder-Patel, B., Iosif, A. M., Nordahl, C. W., Heath, B., Solomon, M. and Amaral, D. G. 2020. Clinically significant anxiety in children with autism spectrum disorder and varied intellectual functioning. Journal of Clinical Child & Adolescent Psychology.
- Kildahl, A. N., Bakken, T. L., Holm, O. H. and Helverschou, S. B. 2017. Assessment of psychosis in ASD/ID: A case study. Advances in Mental Health and Intellectual Disabilities, 11, 17–23. https://doi.org/https://doi.org/10.1108/AMHID-11-2016-0036
- Kildahl, A. N., Bakken, T. L., Iversen, T. E. and Helverschou, S. B. 2019a. Identification of post-traumatic stress disorder in individuals with autism spectrum disorder and intellectual disability: A systematic review. Journal of Mental Health Research and Intellectual Disabilities, 12, 1–25. https://doi.org/https://doi.org/10.1080/19315864.2019.1595233
- Kildahl, A. N., Engebretsen, M. H., Horndalsveen, K., Hellerud, J. M. A., Wiik, J. Y., Aasen, G. and Helverschou, S. B. 2019b. Psychiatric assessment in congenital blindness, ASD and ID: Experience from two clinical cases. Advances in Mental Health and Intellectual Disabilities, 13, 194–203. https://doi.org/https://doi.org/10.1108/AMHID-03-2019-0007
- Kildahl, A. N., Helverschou, S. B., Bakken, T. L. and Oddli, H. W. 2020a. “If we do not look for it, we do not see it”: Clinicians' experiences and understanding of identifying post-traumatic stress disorder in adults with autism and intellectual disability. Journal of Applied Research in Intellectual Disabilities : Jarid, 33, 1119–1132.
- Kildahl, A. N., Helverschou, S. B., Bakken, T. L. and Oddli, H. W. 2020b. Driven and tense, stressed out and anxious”: Clinicians’ perceptions of post-traumatic stress disorder symptom expressions in adults with autism and intellectual disability. Journal of Mental Health Research in Intellectual Disabilities, 13, 201–230. https://doi.org/https://doi.org/10.1080/19315864.2020.1760972
- Krystal, J. H., Woods, S. W., Hill, C. L. and Charney, D. S. 1991. Characteristics of panic attack subtypes: Assessment of spontaneous panic, situational panic, sleep panic, and limited symptom attacks. Comprehensive Psychiatry, 32, 474–480. https://doi.org/https://doi.org/10.1016/0010-440X(91)90026-9
- Lai, M.C., Lombardo, M.V. and Baron-Cohen, S. 2014. Autism. Lancet (London, England), 383, 896–910. https://doi.org/https://doi.org/10.1016/S0140-673661539-1
- Lebowitz, E. R. and Omer, H. 2013. Treating childhood and adolescent anxiety: A guide for caregivers. Hoboken, NJ: John Wiley & Sons.
- Lord, C., Rutter, M. and Le Couteur, A. 1994. Autism diagnostic interview-revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24, 659–685.
- Matson, J. L. 1995. The diagnostic assessment for the severely handicapped-revised (DASH-II). Baton Rouge, LA: Disability Consultants, LLC.
- McDonnell, A., McCreadie, M., Mills, R., Deveau, R., Anker, R. and Hayden, J. 2015. The role of physiological arousal in the management of challenging behaviours in individuals with autistic spectrum disorders. Research in Developmental Disabilities, 36, 311–322. https://doi.org/https://doi.org/10.1016/j.ridd.2014.09.012
- Mevissen, L., Didden, R. and de Jongh, A. 2016. Assessment and treatment of PTSD in people with intellectual disability. In: C. R. Martin, V. R. Preedy and V. B. Patel, eds. Comprehensive Guide to Post-Traumatic Stress Disorder. New York: Springer International Publishing, pp. 281–299.
- Morano, S., Ruiz, S., Hwang, J., Wertalik, J. L., Moeller, J., Karal, M. A. and Mulloy, A. 2017. Meta-analysis of single-case treatment effects on self-injurious behavior for individuals with autism and intellectual disabilities. Autism & Developmental Language Impairments, 2, 1–26.
- Moskowitz, L. J., Rosen, T., Lerner, M. D. and Levine, K. 2017a. Assessment of anxiety in youth with autism spectrum disorder. In: C. M. Kerns, P. Renno, E. A. Storch, P. C. Kendall, and J. J. Wood, eds. Anxiety in children and adolescents with autism spectrum disorder. Cambridge, MA: Academic Press, pp.79–104.
- Moskowitz, L. J., Walsh, C. E., Mulder, E., McLaughlin, D. M., Hajcak, G., Carr, E. G. and Zarcone, J. R. 2017b. Intervention for anxiety and problem behavior in children with autism spectrum disorder and intellectual disability. Journal of Autism and Developmental Disorders, 47, 3930–3948.
- Mullen, B., Champagne, T., Krishnamurty, S., Dickson, D. and Gao, R. X. 2008. Exploring the safety and therapeutic effects of deep pressure stimulation using a weighted blanket. Occupational Therapy in Mental Health, 24, 65–89. https://doi.org/https://doi.org/10.1300/J004v24n01_05
- Nimmo-Smith, V., Heuvelman, H., Dalman, C., Lundberg, M., Idring, S., Carpenter, P., Magnusson, C. and Rai, D. 2020. Anxiety disorders in adults with autism spectrum disorder: A population-based study. Journal of Autism and Developmental Disorders, 50, 308–318.
- Oliver, C., Licence, L. and Richards, C. 2017. Self-injurious behaviour in people with intellectual disability and autism spectrum disorder. Current Opinion in Psychiatry, 30, 97–101.
- Painter, J., Hastings, R., Ingham, B., Trevithick, L. and Roy, A. 2018. Associations between mental health problems and challenging behavior in adults with intellectual disabilities: A test of the behavioral equivalents hypothesis. Journal of Mental Health Research in Intellectual Disabilities, 11, 157–172. https://doi.org/https://doi.org/10.1080/19315864.2018.1431747
- Postorino, V., Kerns, C. M., Vivanti, G., Bradshaw, J., Siracusano, M. and Mazzone, L. 2017. Anxiety disorders and obsessive-compulsive disorder in individuals with autism spectrum disorder. Current Psychiatry Reports, 19, 92.
- Raffa, S., White, K. and Barlow, D. 2004. Feared consequences of panic attacks in panic disorder: A qualitative and quantitative analysis. Cognitive Behaviour Therapy, 33, 199–207.
- Reiss, S., Levitan, G. W. and Szyszko, J. 1982. Emotional disturbance and mental retardation: Diagnostic overshadowing. American Journal of Mental Deficiency, 86, 567–574.
- Rittmannsberger, D., Yanagida, T., Weber, G. and Lueger-Schuster, B. 2020. The association between challenging behaviour and symptoms of post‐traumatic stress disorder in people with intellectual disabilities: A Bayesian mediation analysis approach. Journal of Intellectual Disability Research : Jidr, 64, 538–550. https://doi.org/https://doi.org/10.1111/jir.12733
- Rivard, M., Terroux, A., Mercier, C. and Parent-Boursier, C. 2015. Indicators of intellectual disabilities in young children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 45, 127–137.
- Rodgers, J., Herrema, R., Honey, E. and Freeston, M. 2018. Towards a treatment for intolerance of uncertainty for autistic adults: A single case experimental design study. Journal of Autism and Developmental Disorders, 48, 2832–2845.
- Rodgers, J., Hodgson, A., Shields, K., Wright, C., Honey, E. and Freeston, M. 2017. Towards a treatment for intolerance of uncertainty in young people with autism spectrum disorder: Development of the coping with uncertainty in everyday situations (CUES©) programme. Journal of Autism and Developmental Disorders, 47, 3959–3966.
- Rosen, T. E., Connell, J. E. and Kerns, C. M. 2016. A review of behavioral interventions for anxiety‐related behaviors in lower‐functioning individuals with autism. Behavioral Interventions, 31, 120–143.
- Rosen, T. E., Mazefsky, C. A., Vasa, R.A. and Lerner, M. D. 2018. Co-occurring psychiatric conditions in autism spectrum disorder. International Review of Psychiatry (Abingdon, England)), 30, 40–61.
- Rysstad, A. L., Kildahl, A. N., Skavhaug, J. O., Dønnum, M. S. and Helverschou, S. B. 2020. Case study: Organizing outpatient pharmacological treatment of bipolar disorder in autism, intellectual disability and Phelan-McDermid Syndrome (22q13.3 deletion syndrome). International Journal of Developmental Disabilities.
- Rzepecka, H., McKenzie, K., McClure, I. and Murphy, S. 2011. Sleep, anxiety and challenging behaviour in children with intellectual disability and/or autism spectrum disorder. Research in Developmental Disabilities, 32, 2758–2766.
- Santore, L. A., Gerber, A., Gioia, A., Bianchi, R., Talledo, F., Peris, T. S. and Lerner, M. D. 2020. Felt but not seen: Observed restricted repetitive behaviors are associated with self-report-but not parent-report-obsessive-compulsive disorder symptoms in youth with autism spectrum disorder . Autism : The International Journal of Research and Practice, 24, 983–994.
- Sappok, T., Budczies, J., Dziobek, I., Bölte, S., Dosen, A. and Diefenbacher, A. 2014. The missing link: Delayed emotional development predicts challenging behavior in adults with intellectual disability. Journal of Autism and Developmental Disorders, 44, 786–800.
- Siegel, D. J. 2012. Developing mind. 2nd ed. New York: Guilford Publications.
- Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T. and Baird, G. 2008. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 921–929.
- Soke, G. N., Rosenberg, S. A., Hamman, R. F., Fingerlin, T., Rosenberg, C. R., Carpenter, L., Lee, L. C., Giarelli, E., Wiggins, L. D., Durkin, M. S., Reynolds, A. and Diguiseppi, C. 2017. Factors associated with self-injurious behaviors in children with autism spectrum disorder: Findings from two large national samples. Journal of Autism and Developmental Disorders, 47, 285–296.
- Sparrow, S. S., Cicchetti, D. V. and Balla, D. A. 2005. Vineland adaptive behavior scales. 2nd ed. San Antonio, TX: Pearson Clinical Assessment.
- Sukhodolsky, D. G., Scahill, L., Gadow, K. D., Arnold, L. E., Aman, M. G., McDougle, C. J., McCracken, J. T., Tierney, E., White, S. W., Lecavalier, L. and Vitiello, B. 2008. Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology, 36, 117–128.
- Townsend, M. C. and Morgan, K. I. 2018. Psychiatric mental health nursing: Concepts of care in evidence-based practice. 9th ed. Philadelphia, PA: F.A. Davis Company.
- Valdovinos, M. G., Seibert, H. N., Piersma, D., Wilkinson, A., Griffith, G., Hillring, S. and Boyle, B. 2019. Characterizing mood states in individuals diagnosed with bipolar disorder and intellectual disability. Journal of Mental Health Research in Intellectual Disabilities, 12, 26–44.
- van den Bogaard, K. J. H. M., Lugtenberg, M., Nijs, S. and Embregts, P. J. C. M. 2019. Attributions of people with intellectual disabilities of their own or other clients’ challenging behavior: A systematic review of qualitative studies. Journal of Mental Health Research in Intellectual Disabilities, 12, 126–151. https://doi.org/https://doi.org/10.1080/19315864.2019.1636911
- van Steensel, F. J. A., Bögels, S. M. and Perrin, S. 2011. Anxiety disorders in children and adolescents with autistic spectrum disorders: A meta-analysis. Clinical Child and Family Psychology Review, 14, 302–317. https://doi.org/https://doi.org/10.1007/s10567-011-0097-0
- Wolkorte, R., van Houwelingen, I. and Kroezen, M. 2019. Challenging behaviours: Views and preferences of people with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities : Jarid, 32, 1421–1427.
- World Health Organisation. 1992. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organisation.
- Yin, R. K. 2014. Case study research. Design and methods. 5th ed. Los Angeles, CA: Sage Publishing.
