Abstract
Purpose: A comparison of parents’ experiences of getting a diagnosis for their child with autism, attention deficit hyperactivity disorder (ADHD) and both diagnoses can inform our understanding of common and unique themes across these neurodevelopmental conditions.
Method: A quantitative and qualitative online anonymous survey of 288 New Zealand parents of children diagnosed with autism (n = 111), ADHD (n = 93), or both conditions (n = 84) was conducted. Open-ended questions were analysed using reflexive thematic analysis.
Results: Parents described an adversarial diagnosis and support system where seemingly arbitrary criteria and thresholds were applied. Key themes specific to the different diagnostic groups were also identified.
Conclusions: Common themes of parents’ experience across the different neurodevelopmental conditions highlight the need for changes to the diagnostic process.
Autism spectrum disorder (autism) and attention-deficit/hyperactivity disorder (ADHD) are neuro developmental conditions and typically emerge in early childhood (American Psychiatric Association, Citation2013). The conditions are separated by core symptoms; the autism diagnostic criteria include fixed, rigid behaviour and social difficulties, and ADHD is characterised by the presentation of attention difficulties, impulsivity and hyperactivity (American Psychiatric Association, Citation2013). Prevalence estimates in children are 5% for ADHD (Sayal et al., Citation2018) and 1.85% for autism (Maenner et al., Citation2020). The conditions also have high rates of co-occurrence with an estimated 32% of autistic 8 year-olds also having an ADHD clinical diagnosis (hereafter referred to as autism + ADHD)(Soke et al., Citation2018).
Obtaining a diagnosis in childhood for autism or ADHD often follows a typical diagnostic pathway. It begins with parents noticing their child’s atypical development, they then present with a particular concern(s) to a health professional before being referred to a specialist or a multidisciplinary team for diagnosis (Gibbs et al., Citation2019, Sayal et al., Citation2018). In New Zealand, parenting courses (e.g. Incredible Years Parent Programme®) are often offered by agencies and professionals before a referral to specialist as a means to rule out behaviour due to challenges around parenting (Fergusson et al., Citation2009).The autism diagnostic process will have cultural differences across national contexts, but is described in qualitative analyses in United Kingdom and Europe as remarkably similar to a New Zealand context (Braiden et al., Citation2010, Legg and Tickle, Citation2019), which has led to direct comparisons across national borders of the process (Eggleston et al., Citation2019).Fifty-six percent of parents in the United Kingdom (Crane et al., Citation2016) and 37% of parents in New Zealand (Eggleston et al., Citation2019) reported finding the autism diagnosis process very stressful. Similarly, across 10 European countries 33% of parents reported ‘a great deal of difficulty’ obtaining a referral and 31% ‘a great deal of difficulty’ obtaining a diagnosis of ADHD (Fridman et al., Citation2017).
Barriers to getting a diagnosis have been identified in large scale quantitative surveys (Crane et al., Citation2016, Eggleston et al., Citation2019, Fridman et al., Citation2017) and qualitative thematic analyses (Boshoff et al., Citation2021, Elder et al., Citation2016, Makino et al., Citation2021, Ryan and Salisbury, Citation2012). Barriers to diagnosis for both autism and ADHD include: the delay caused by seeing multiple specialists (Eggleston et al., Citation2019, Fridman et al., Citation2017), lengthy wait periods between presenting with a concern and eventual diagnosis (Fridman et al., Citation2017, Stevens et al., Citation2016) and difficulty accessing specialists who can diagnose reliably (Crane et al., Citation2016, Fridman et al., Citation2017). Parental distress can be compounded by premature reassurances that their children are developing typically, or ‘therapeutic nihilism’ whereby they are told nothing can be done so the diagnostic pathway is ignored (Elder et al., Citation2016, Ryan and Salisbury, Citation2012).
The factors that affect stress and create barriers during the diagnostic process often delay diagnosis and thus the opportunity for early intervention. Early intervention has been shown to be effective, with greater adaptability and life outcomes for children who obtain early evidenced-based interventions, particularly for autism (Whitehouse et al., Citation2021), but the evidence for the effectiveness of early intervention for ADHD is also mounting (Bannett et al., Citation2022).However, recent research on the wider effects of ADHD diagnosis indicates there are concerns around early diagnosis and some issues related to the impact of a possible diagnostic shift.
Recent studies compared matched symptomatic young people diagnosed with ADHD, and without, and found that young people with the label showed the same or worse on quality of life and relationship measures than those without the label (Kazda et al., Citation2022, O’Connor and McNicholas, Citation2020). O’Connor et al. (Citation2018) have highlighted the instability of childhood diagnoses and the ramifications for young people and their families when diagnostic shift occurs, that is, when a diagnosis is retracted, replaced, or supplemented. Clinicians can experience dilemmas when weighing up providing an early but possibly inaccurate diagnosis versus providing early access to support (Mitchell and Holdt, Citation2014). Diagnostic labels are also tools by which parents and young people make sense of their behaviour, their identity and stigma, therefore, it is important that accurate diagnosis occurs (O’Connor et al., Citation2018).
The most uncommon diagnostic shift and the one that has the most negative impact, is diagnostic retraction, so O’Connor et al. (Citation2018) speculate that the easiest option is to let a previous diagnosis ‘recede from active clinical attention’ (pg. 989), rather than retraction. However, the aim of this study is not to explore difficulties with accuracy of diagnosis, the system by which families can access support or whether they should begin the journey, but to examine the diagnostic process itself from the parent’s perspective. It has been shown that high satisfaction with the diagnostic process leads to lower levels of stress, better coping strategies, and quicker adoption of evidence-based interventions by parents (Crane et al., Citation2016). Therefore, improving understanding of and the experience of the diagnostic process is essential to improved immediate outcomes for families, who have already begun this process.
Previous studies have explored the issues and challenges that parents face getting a diagnosis and support for children with autism and, to a lesser extent, ADHD (Carr-Fanning and Mc Guckin, Citation2018, Makino et al., Citation2021). Qualitative analyses and systematic reviews have used several frameworks and identified key themes that give greater context to the parents experience of the autism diagnostic process(Legg and Tickle, Citation2019). Legg and Tickle (Citation2019) identified three key types of parent need; emotional, relational, and informational. These needs change over the diagnosis process. Parental emotional guilt during the search for a diagnosis was replaced by grief or affirmation of autism identity post diagnosis (Legg and Tickle, Citation2019). Information needs also changed with parents requiring more information in different formats at different points highlighting the need for strong relationships between clinicians and family (Legg and Tickle, Citation2019). The review also showed some parents of children with autism in the UK experienced dismissal of their concerns, longer wait times, and unsatisfactory assessment, communication of diagnosis and supports which contradicted best practice guidelines (Legg and Tickle, Citation2019).
In addition, qualitative analyses and systematic reviews show several frameworks have been used in research to understand: (i) how parents cope with an autistic label for their child (O’Connor et al., Citation2018; ii) causal-blame attribution (Dale et al., Citation2006; iii) grief or autistic identity celebration and (iv) whether they adopt a social or medical model of their child’s needs (Russell and Norwich, Citation2012). However, in all cases parents appear to have complex and evolving understandings. Russell and Norwich (Citation2012) identified that parents teeter between wanting to normalise their child’s status and resist diagnosis and the opposite of wanting to move towards diagnosis and advocating for the normalisation of autism.
However, no study has qualitatively compared the experience of getting a diagnosis across autism, ADHD and both diagnoses. The increasingly prevalence of co-occurring neurodevelopmental conditions (Soke et al., Citation2018) means that understanding transdiagnostic experiences will inform an understanding of the diagnosis process. Autism and ADHD are one of the most experienced co-occurring coupling, therefore comparative insights of a co-occurring group should strengthen and provide a more complex and nuanced understanding of the diagnostic process and experience. The seemingly different diagnosis pathways should suggest markedly different experiences because an autism diagnosis is possible from 12 months (Pierce et al., Citation2019) and usually requires an interactive-observational schedule (Hong et al., Citation2020), an ADHD assessment requires a multiple setting rating scale questionnaire and usually occurs after the age of 6 years (Izzo et al., Citation2019). However, any similarities in the experience, which sit outside of the expected differing developmental milestones or assessment tools, could suggest ecological and contextual factors that shape the process itself.
The current online survey aimed to collect a qualitative data to understand parents’ experiences and perceptions of the diagnosis process for either autism, ADHD or autism + ADHD. The parents’ perceptions reported in this article were drawn from open-ended questions (qualitative), which were part of a broader survey that also included closed questions (quantitative) examining the diagnostic pathway for these three groups in New Zealand. The value of open survey questions as a research method is that this is a 'wide-angle lens’ that can include a number of diverse voices, wide geographical participation, encourage openness in responses, and provide participants with autonomy and control over their participation (Braun et al., Citation2021). Reflexive thematic analysis was used to analyse the qualitative data due to the extensive response rate and depth of answer that required an understanding of latent themes, not anticipated at the outset (Braun and Clarke, Citation2021). This analysis was designed to aid our understanding of the diagnostic experience across these three groups.
Methods
Ethical clearance and informed consent
Ethical approval for this study was provided by the Human Ethics Committee at Victoria University of Wellington, New Zealand [Approval number 28993].Participation in the study was both voluntary and anonymous. All participants provided written and informed consent prior to enrolment in the study.
Participants
Parents of children with a diagnosis of autism, ADHD, or co-occurring autism and ADHD were invited to participate in a survey, eligibility criteria being: (a) they were parents, legal guardians, or caregivers (hereafter, parents), (b) their child had a clinical diagnosis of autism, ADHD orautism + ADHD, (c) their child was aged 18 years or younger, and (d) parents and child were living in New Zealand. A purposive, criterion-based convenience sampling strategy (Palinkas et al., Citation2015) was used to recruit a diverse range of participants who had children diagnosed with the three conditions. Participants were recruited by an email sent by Autism New Zealand and ADHD New Zealand and information about the study shared on various autism and ADHD social media groups. Participants were sent a link to the questionnaire within the advertisement.
Materials
This paper analyses qualitative data from an anonymous online survey hosted on Qualtrics (data collected from 15th March 2021to 1st June 2021) on the early development, diagnosis and experience of obtaining a diagnosis for parents of children, diagnosed with autism, ADHD or both in New Zealand. This was a quantitative and qualitative design (Braun et al., Citation2021). The survey included a combination of 25 closed (quantitative) questions and open-ended (qualitative) questions separated into six sections: (a) demographic characteristics, (b) atypical development, (c) first concerns, (d) specialists seen, additional diagnoses, and (e) age of diagnosis and (f) qualitative questions. The quantitative questions in sections (a-e) were used to obtain a comprehensive picture of characteristics of participants, their children, key aspects of diagnostic experiences and types of specialists seen. The details and analysis of sections (b) - (d) are reported in the quantitative analysis (Sainsbury et al., Citation2022). The open-ended (qualitative) questions in section (f) included focused on parent’s experiences of the diagnosis pathway and were designed to be broad, and to elicit both strengths and weaknesses of the diagnosis process, while also giving participants an opportunity to share other information about the diagnosis process. The three qualitative questions were:(1) What was helpful during the diagnostic process? (2) What was unhelpful about the diagnostic process? (3) What else would you like researchers to know about your experience of getting a diagnosis for your child? The survey questions and design were informed by consultation with a research and advocacy advisor at Autism New Zealand.
Data analysis
Descriptive statistics were used for demographic data and to describe the response rate and quantity across the quantitative responses in the survey. Reflexive Thematic Analysis (RTA)is a qualitative method emphasising the subjectivity of the researcher as a resource to be utilised in a continual reflexive engagement at all stages of the thematic process (Braun and Clarke, Citation2021). Unlike other qualitative methodologies it is not tied to a particular epistemological or theoretical perspective (Maguire and Delahunt, Citation2017), however, Braun and Clarke (Citation2021) articulate that reflexive thematic analysis is not done in a ‘vacuum’ and researchers must consider the standpoint from which they analyse (Braun and Clarke, Citation2021). A prerequisite for reflexive thematic methodology was a rich data set of qualitative responses. The high rate of participation and length of responses suggested this approach would be an appropriate method to analyse parents’ survey responses.
Braun and Clarke (Citation2021) reflexive TA has six key steps: The first and the second step involved reading and re-reading the data as a whole to obtain an initial impression of the experience and meaning and using an inductive approach to generate initial codes. The researcher coded participant responses by hand using open-coding, not using any pre-set codes but developing and modifying codes as she went through the process. This led to the third stage of reflexive TA and the creation of semantic (surface descriptive level) codes based on participants’ language, such as ‘child labelled naughty,’ ‘reluctance to diagnose’. These codes were then interrogated and refined again (recursive analysis). Participants’ responses were also placed along a diagnostic pathway, such as ordering responses into initial concerns, encounters with professionals, and post diagnosis support.
This led to the third step construction of topics corresponding to a diagnosis pathway and to codes suggestive of barriers and enablers at each step. All codes were grouped and corresponding quotes were listed under each to test the value, to describe the data and as an indication of prevalence to ensure key patterns across the dataset were being captured (Braun et al., Citation2021). The quotes may have been changed for spelling clarification and are not necessarily the full response of the participant (Terry et al., Citation2018).
The fourth step involved the search for themes and patterns across the data. This involved ‘dwelling with’ data and multiple reiterations of the data (Braun and Clarke, Citation2021). The guiding questions were: ‘Has the meaning behind the participant’s comments been captured? What has been left out and why? ‘Reflexivity was enhanced through the use of a self-reflective journal and visual modelling which was used to describe decisions and coding (e.g. development, revision, expanding a collapsing of codes and themes). Supervision and critical discussion of data, codes, construction of themes with peers also occurred (Braun and Clarke, Citation2021). This was structured by the authors’ (C.J. Bowden) and (H. Waddington) reviewing codes and themes and challenging greater reflexivity in the data.
This led to the latent analysis and a deeper interpretation and consideration of meaning of the experience for parents in their journey for diagnosis and support.
The fifth step involved defining and naming themes and returning to steps two and three to check accuracy and meaning of initial coding attempts, and mapping where the themes interacted and the relationships between themes. The coherency, overlap and distinctiveness of themes was also scrutinised with the acknowledgement that some subthemes were shared between themes. During this phase the specificity of the child’s diagnosis became relevant to seeing where themes were represented by all diagnostic categories, or when only one or two diagnoses were indicated in the analyses. The final step was writing up the analysis, research and this journal article.
Results
Sample characteristics
There were 288 participants, who met the criteria and had children diagnosed with either autism (38.5%, n = 111); ADHD (32.6%, n = 94); and autism + ADHD (28.8%, n = 83). The children in the sample were predominantly male (74.7%, n = 215) followed by female (22.6%, n = 65) and nonbinary (2.1%, n = 6) with a mean age of 9.5 years. On average the autistic children were diagnosed around 5.25 years (7.3 years for the autism diagnosis for the autistic + ADHD children) and 7.4 years for ADHD children (6.8 years for the ADHD diagnosis for the autistic + ADHD children).
Mothers (94.8%, n = 273) were more likely to have completed the survey than fathers (2.4%, n = 7) or legal guardians (2.8%, n = 8). The parents who completed the survey were more commonly NZ European (69.4%, n = 200) compared to Māori (22.2%, n = 64) or Pacific People and other cultural backgrounds (8%, n = 23), had completed university (42.4%, n = 131) and were in a household income bracket between $NZ 50,000 - 99,000 (36.5%, n = 105).
Supplementary Figures 1–3 show the rate of response and approximate length of responses to the three questions. There were a total of 694 responses across the three questions totalling 19,509 words, which ranged from one word to 500+ word responses. There were 26 participants who did not answer any of the three questions (n = 11 ADHD; n = 7 Autism; n = 8 autism + ADHD participants).There was no significant difference in the rate of ‘no response’ or length distribution across the three diagnostic groups. The responses produced a rich and varied qualitative data set.
Thematic analysis
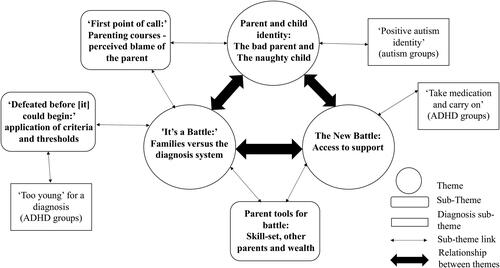
Analysis of the data led to the construction of three major themes: 1) it’s a battle, 2) parent and child identity, and 3) the new battle. The relationship between these three themes and subthemes are illustrated in . The answer to the question ‘what was helpful?’ was inverted by 25% of respondents, who answered this negatively, such as ‘Nothing, we really didn’t get any help’ (ADHD).
Theme 1: ‘it’s a battle’: families versus the diagnosis system
This first theme, which describes the battle and struggle parents of children with Autism and/or ADHD had with the diagnosis system, is made up of four subthemes, two of which also apply to another theme. These are: (i) defeated before it could begin, which pertains to parents’ perception of diagnostic-delay due to restrictive criteria; (ii) too young for a diagnosis, relating to a particular restrictive age criteria, which applied to obtaining an ADHD diagnosis (iii) first point of call, (described in Theme 3: Parent and child identity) and (iv) parent tools for battle (described in Theme 2: The new battle).
Parents described battling or fighting within a system for a diagnosis for their child, as being in a ‘longbattle’ (Autism + ADHD) and the diagnosis system as ‘broken’ (Autism), ‘a nightmare’ (ADHD) and ‘like walking to hell and back’. (Autism). Parents described an ‘us’ versus ‘them’ situation where they had to constantly ‘fight to get him seen’, (Autism + ADHD)or to better co-ordinate within the system; ‘I fight every single day to stay on top of the people/agencies […] to not get lost in the system’. (Autism + ADHD). When parents expressed that they had a positive experience they were compelled to acknowledge this as luck, or an exception to the normal experience of having to fight for their child: ‘For other families, I hear how much harder it is, so I consider our experience more of an outlying data point than indicative of the normal diagnostic process in New Zealand’ (Autism).
‘Defeated before [it] could begin’: application of criteria and thresholds
The application of criteria for assessment and diagnostic thresholds were a key component of the parents’ battle for access. Parents were told their child was ‘too mild’, ‘too social’ or ‘too young’ to get a diagnosis and were disappointed by not being given alternative options after their child failed to meet criteria. The resulting diagnosis-delay left parents feeling demoralised and shut out: ‘The public system said he was not bad enough therefore would not help us’ (Autism + ADHD). This created a fait accompli and some families felt beaten when advised not to try for assessment in the public system; ‘GP thought the wait in the public system would be too long and threshold of impairment too high to be accepted for assessment’ (ADHD). Meeting the threshold of ‘mild’ became something negative that often led to denied access, rather than acknowledgement and justification for accommodation for the needs of the child and family.
Sometimes professionals decided to delay a referral or diagnosis due to thresholds and criteria: ‘while you want to be thorough, delaying a diagnosis does not help children and families’ (Autism). In some cases professionals applied their own criteria, and did not diagnose because they believed ‘labels are bad’ (Autism), or because they had a lack of ‘belief’ that there was an issue (ADHD). In other cases, parents described being stonewalled by diagnosticians who declared that their child did not fit the diagnostic criteria, but who did not offer counter evidence or only spurious evidence. For example, a diagnostician was reluctant to diagnose because a child made eye-contact so was ‘not autistic’ (Autism + ADHD). Narrow criteria and subjectively applied thresholds denied or delayed diagnosis and lengthened the ‘battle’. This experience was in contrast to helpful professionals, who validated concerns, explained the diagnosis in relation to the child, and offered tangible help, such as, describing the doctor ‘who explained that’ our child’s brain just worked differently and explained it in a way for us all to understand’ (ADHD)
‘Too young’ for a diagnosis (ADHD groups)
Parents in the ADHD groups encountered the professional’s barricade of being told their child was ‘too young’ for a diagnosis: ‘We kept getting told he’s too young… age is sometimes irrelevant when there is obvious signs’ (Autism + ADHD). Parents were upset because this decision delayed diagnosis, reduced time for early support and left the family in limbo: ‘It is very, very hard to get a diagnosis for young children and all the research shows the earlier you get this the better’ (ADHD). Parents described how they were thwarted when told to wait until the child turned six or had started school and that this led to a feeling ‘of being defeated and overwhelmed’ (Autism + ADHD). Delays also meant parents were not able to access support and had to start the process again: ‘because he was too young I couldn’t get any support – We were discharged from service then had to get another referral when he turned 6. Then the wait list and re-referral process took another year to get through’ (ADHD).
Theme 2: the new battle: access to support
The second key theme was that, following their initial battle (getting a diagnosis), parents reported having to start a new fight to get support for their child. This theme has two subthemes: (i) Parent tools for battle(also relates to Theme 1); and (ii) Given medication and told to carry on which described the quandary parents felt around medication being given in isolation to children diagnosed with ADHD.
This second and new battle was described by some parents as harder than their initial fight for diagnosis: ‘The diagnosis part was easy. It’s getting the required support afterwards that is hard’ (Autism). The support was described as concealed and costly; ‘If she needs any support now, we have to find it and fund it ourselves, which we can’t really afford to do’ (ADHD). Parents described being disappointed and let down because the purpose of diagnosis was to get support for their children, so when no support was forthcoming the diagnosis seemed ‘pointless’ (Autism), for ‘everyone else’ (Autism) or that diagnosis was impractically treated as a ‘magic wand’ with no other support (Autism + ADHD).
Accessing support in the education system was challenging and parents encountered many obstacles including a lack of visibility, insufficient learning support, and limited teacher capacity. Some parents drew attention to the criteria for school support, including accessing teacher aides in the classroom, explaining that unless the child needed ‘help with toileting’ (Autism), or the child was ‘extreme and throwing chairs at teachers’ (Autism + ADHD) then there was no support from the education sector. One parent explained that the teacher aide hours had recently been cut to serve more children but with shorter amounts of time (ADHD).
Parents also identified that access to education support was adversarial in nature and seemed ad hoc, uncoordinated, and ‘un-planned’ (ADHD). They noted that support dropped off at the start of school enrolment rather than increased (Autism) and that there was a gap between diagnosis and support at school (Autism). One parent explained how they were caught between organisations over the responsibility for support; ‘Hospital thinks schools should support and schools think its hospital’s role to support. Parents are stuck in the middle’ (ADHD). The limited support was also not parent and family-focused and parents lamented a lack of parental counseling ‘to come to terms with diagnosis’, (Autism) and that overall ‘the system is not at all prepared to support us’ (Autism + ADHD).
Parent tools for battle: skill set, other parents, and wealth
Whether parents were starting their first battle with the system for diagnosis or beginning a new (second) battle with the system for support their experiences were shaped by the assets and tools they had at their disposal. Parents who were able to draw on previous knowledge, and knew how to research their child’s condition and navigate health systems were more prepared for their fight: ‘I feel like we only managed to get through the process because we are well educated and persistent’ (ADHD). The parent skill-set was seen as essential due to the level of difficulty required to navigate the pathway to diagnosis: ‘It was very difficult navigating the diagnosis pathway. My background is in the heath sector and I consider myself to be reasonably well informed’ (ADHD). Parents were acutely aware and concerned for other parents who might not have the necessary skill-set: ‘Following the diagnosis path to get help without having these tools and knowledge would be even harder’ (Autism).
Parents’ sense of empowerment that came with having assets was sometimes undermined during professional encounters. One parent explained that after a psychology degree and multiple parent courses one specialist told ‘“that sounds like parent diagnosis”, actually, I know my son best’ (Autism + ADHD). Parents sometimes felt better informed than professionals, with particular skill-sets such as in understanding girls with ADHD or autism: ‘There is not enough knowledge in the medical profession about autism in girls and how it presents differently. It’s draining’ (Autism + ADHD).
Another important tool parents used in their fight for diagnosis was support and comradery from other parents who became allies and shared information about how to navigate the system: ‘[We] only knew what to do (e.g. ask GP for a referral to specialist) as my friend had recently been via the process for her son’ (Autism + ADHD). Parents described how information, support, and helpful agencies were ‘very much word of mouth from other parents’, (Autism + ADHD), which was ‘invaluable’ (Autism). This skill-set sits outside of the system with a clear delineation between ‘us’ (parents of children with diagnoses) and ‘them’ (the systems and professionals involved along the diagnosis pathway).
The other tool for fighting the system was the personal financial resources parents used to access professionals and educational support in the private system. Parents often acknowledged how lucky they were to be able to go private: ‘Expensive but we are lucky that’s an option for us’ (Autism). Parents lamented the cost, but explained the private system fulfilled their expectations: ‘If you don’t come from a family with means to pay for assessments, tuition and support required you are left behind by our system’ (Autism + ADHD).
‘Given medsand carry on’ (ADHD and autism + ADHD)
A key subtheme in the ‘new battle’ was that support for children with an ADHD diagnosis often consisted solely of being given medication: ‘very little support given for practical strategies […]. Basically given meds. and carry on’ (ADHD). One parent of a child with both autism and ADHD contrasted the support after diagnoses by commenting that whilst no support, other medication had been offered for ADHD there and been, ‘information overload for autism’ (Autism + ADHD). Parents of children with ADHD also shared how medication had been ‘life changing’ (ADHD) with their child being able to engage in the classroom.
Theme 3: parent and child identity: the bad parent and the naughty child
The third key theme in the parents’ experience of diagnosis and support concerned parent and child identity. Parents’ competence and children’s behaviour were often blamed prior to diagnosis and a label led to a shift in blame and identity. This theme is connected to both ‘Battle’ themes and is made up of two subthemes: (i) ‘First point of call’ which pertains to the way parenting courses are offered (also relates to Theme 1) and (ii) ‘Positive autism identity’ which relates to an identity specific to the autism diagnosis.
Prior to diagnosis parents carried responsibility and blame for their child’s behaviour, making them particularly vulnerable to directly or indirectly implied parenting criticisms. Parents described being blamed by other parents and professionals and ‘Being made to feel like a horrible parent’ (Autism + ADHD). They felt their ability and expertise questioned and critiqued by other parents and services: ‘It is a very, very hard road with judgement from other parents and most of all the agencies who think it’s your parenting’ (Autism + ADHD). Professional sometimes appeared to locate the problem in the child or parent rather than in the condition and accompanied this with dubious parenting advice such as a doctor telling a parent it was ‘a testosterone surge and to go home and be a parent’ (ADHD), or that ‘maybe he just needed a smack and more discipline’ (Autism). The parents were also denied a referral to a specialist, and this created a diagnosis-delay.
For some parents, receiving a diagnosis for their child led to validation and a change in identity for parents. They experienced relief due to a reduction in social stigma and described how others no longer judged them as bad parents: ‘It no longer felt like a helpless situation due to bad parenting - people believed me finally’ (ADHD). Equally, upon diagnosis there was a change in identity and a shift in blame away from their child which was a relief for parents; ‘Realising we weren’t bad parents, our child wasn’t naughty’ (Autism). The diagnosis enabled parents to actively reframe their child’s identity at school and home, and rationalise their child’s behaviour.
‘First point of call’: parenting courses – perceived blame of parent
Parents were often offered parenting courses by professionals. This was perceived by parents as confirmation of their, sometimes self-imposed, ‘bad parent’ identity: ‘They blame you initially. Send you to parenting courses. Many different parenting courses. Then eventually after a few years on a wait list you see a specialist’ (Autism + ADHD). This subtheme was also shared with the first theme ‘It’s a battle’ by the timing of these parenting courses, which appeared to act as gatekeepers for accessing a diagnosis system and were perceived as an affront to parents: ‘[organisation]’s lack of interest in a person unless they do a parenting course first is pathetic’ (ADHD).
Although some parents could see the benefit of these courses, they nevertheless wanted the timing to be reconsidered: ‘I understand there needs to be a focus on parenting in some respect, but that shouldn’t be the first point of call’ (Autism + ADHD). Parents were often referred to parent education programmes instead of being referred for diagnosis, because professionals perceived this as a form of helpful support for parents. Parents highlighted the contradictory message inherent in the offering of parenting courses as support; ‘Although there is a strong push toward parents not having done anything wrong etc., but then the first thing offered is a parenting course… This is an issue’ (ADHD). By choosing parenting courses as a first course of action it was perceived that professionals ignored the competence and skill-sets of parents and undermined parents self-efficacy; ‘It was also humiliating being forced to do a parenting course as I have a background as a parenting educator!’ (Autism + ADHD). The courses were also criticised for not specifically addressing parenting of neuro-diverse children: ‘makes people feel bad and many of the strategies don’t work for kids with ASD/ADHD’ (Autism + ADHD).
Positives of an autism diagnosis (autism and autism + ADHD)
A second subtheme, related to parent and child identity, was that of a positive autism identity. Some experienced the opportunity to reposition their identity as parents of an ‘authentically autistic’ child (Autism), advocating the involvement of autistic adults in information and organisations: ‘Nothing about us, without us’ (Autism).
This second identity shift came from a number of different sources, including wider experience with autism in the family, autism community groups and sometimes professionals. The community groups saw labels as empowering and parents lamented how autism had been ‘medicalised and problematised’ (Autism) during the diagnostic process. Some professionals were described as having rigid concepts of normality and typicality, others encouraged parents to see autism through an inclusive lens and with positivity; ‘[Professional] treats autism as a normal variation and doesn’t stigmatise it’ (Autism + ADHD).
Discussion
The reported experiences of obtaining a childhood diagnosis for autism and ADHD were similar with common themes expressed by parents across diagnoses. Many parents experienced the diagnostic process as a battle, which was primarily motivated by the impetus to obtain support for their child. The analysis of the parents’ experiences shows that delays in diagnosis might be the result of factors including opaque systems, wait-and-see models, and requirements for parenting courses before diagnosis. The diagnosis appeared to have a particular benefit in allowing parents to reframe their parental ability and the behaviour of the diagnosed child to a more positive and less guilt-laden identity.
The findings from our study show that the ‘battle’ analogy was omnipresent throughout the process and informed each stage. Across all parents in this analysis, there was disappointment that they had to start a second fight for support after diagnosis, particularly within an education setting. These findings align with those of Daniels et al. (Citation2021), who studied diagnosticians’ understanding of parents’ experience of the journey to the autism diagnosis in United Kingdom, and created a subtheme ‘parental battle for services’ where diagnosticians used the battle analogy to describe their perspective of parents’ ‘fight’ for support.
Parents’ perception of parenting courses as part of this ‘battle’ was perhaps surprising because parenting courses are recognised as an evidenced-based support (Prata et al., Citation2018). As a ‘first point of call’ before diagnosis, these courses might rule out more mild issues and thus, reduce wait times, patient load, while also potentially benefitting the child and parent (Risley et al., Citation2020). There a number of recognised benefits of parenting courses, such as a reduction in school and relationship issues, and a sense of greater parent self-efficacy and well-being of the family (Leijten et al., Citation2018, Modesto-Lowe et al., Citation2008, Prata et al., Citation2018). However, parents in the present study viewed being offered parenting courses as evidence that their parenting was being blamed or implicated. The theme of parent and child identity indicates that parents may well be primed for this thinking both from internal and social pressures at the outset of the process to diagnosis. Whilst Kasilingam et al. (Citation2021) describe how 22% of New Zealand parents of autistic children specify parenting courses as the extra support that they would like, the question was posed after diagnosis. Parents may have experienced the referral differently had they been offered the courses as a support after diagnosis and specific to the child’s diagnosis.
The comparison of the three diagnoses in the present study highlighted unique themes for the ADHD group with the use of medication for treatment and with the application of the ‘too young’ for diagnosis criteria. In contrast to the ADHD groups, the autism only group did not report being told their child was too young for a diagnosis, perhaps because the message about early diagnosis being possible from age two is becoming more well-known (Waddington et al., Citation2021). Halperin and Marks (Citation2019) identify a number of reasons why practitioners are reluctant to diagnose ADHD in preschool including that the symptoms of ADHD are commiserate with typically developing preschool children, multi-informant assessments are more difficult to establish and that early childhood symptoms are not well established. Although there is growing body of research on the diagnosis of ADHD in pre-schoolers (Wallisch et al., Citation2020, Wigal et al., Citation2020), in the current clinical context the explanation of ‘too young’ is understandable, but nonetheless provides a mismatch between parents’ options for early diagnosis, intervention, and support.
A unique theme for the autism groups was that parents called for an introduction to thinking about a positive autism identity to occur along the diagnostic pathway. There is an important trend in the research literature and in community groups, away from ‘having autism’, and autism being framed using a bio-medical deficit-focused model, to ‘being autistic’ and the acknowledgement of a more social or neurodiversity affirming identity (Anderson-Chavarria, Citation2021). A more positive framing of ADHD abilities in the research literature is now occurring (Moore et al., Citation2021, Sedgwick et al., Citation2019), but there seems to be less advocacy and sense of a positive ADHD identity compared to autism within the community of parents’ surveyed in the current research.
The current research was limited in a number of ways. The survey represented a cross-section of New Zealand population based on the average highest education and income of the sample (OECD, Citation2019); however, certain groups may have been under-represented in responding to the survey. The majority of participants were mothers, which limited the voices of fathers, and a more gender-balanced sample might be considered for future research. This survey did not analyse parents’ responses to the diagnosis process over time or contextualise particular disparities, such as rural, cultural and low socio-economic groups. A further consideration is that parents of children in the survey answered if there child was between one year to eighteen years of age, which means that retrospective remembering of the process might differ between the different points of diagnosis and in relation to the current age of the child. In addition, the opt-in nature of the survey may have meant that participants felt compelled to answer if they were particularly aggrieved or if they had a negative diagnostic experience. This creates a less favourable picture of the process. An open-survey is also restrictive because it does not allow researchers to follow-up or probe further in understanding the diagnostic experience.
Support organisations and professionals might wish to consider working more collaboratively with parents, to acknowledge parental guilt and to signal upfront the process from diagnosis to support options. Understanding the centrality of parent and child identity might encourage professionals to be more sensitive around their interactions. An empowering of autism and ADHD identity might help parents along the diagnostic pathway. The criteria set of being ‘too young’ for ADHD families should be examined and the timing and appropriateness of recommending parenting courses reviewed. This might involve addressing parent experiences of the courses acting as a gatekeeper to diagnosis, the applicability of the courses to neuro-diverse children and the implied assumptions about parenting competence and expertise. The similarities of experience across the three diagnostic groups suggests that a wider parent community group might draw on greater expertise about access, support and advocacy of neurodiversity. Future research might examine further similarities across childhood neurodevelopmental disorders and those with co-occurring diagnosis experience.
Conclusions
This study has shown that, during the diagnostic pathway, parents of children, who have either ADHD, autism or autism and ADHD, experienced a similar battle to get a diagnosis for their child and access support for their child and family. Many of the issues found in this research, were similar to other research examining the experience of autism diagnosis, yet were found also to be applicable for ADHD and a co-occurring diagnosis. However, there were specific themes for the particular diagnoses, such as parent’s desire for the empowering of a positive autism identity, and the application of a ‘too young’ criterion for parents with ADHD children. Parents were sensitive to perceived parental and child blame in interactions along the diagnosis process, which meant parenting courses were problematic when offered prior to diagnosis.
Competing interests and funding
This publication forms part of the requirement for Willow Sainsbury’s doctorate by publication at Victoria University of Wellington.
Financial interests
Willow J. Sainsbury, Kelly D. Carrasco and Hannah Waddington declare they have no financial interests. Andrew J.O. Whitehouse is supported by an Investigator Grant National Health and Medical Research Council (1173896).
Compliance with ethical standards
Ethical approval for this study was provided by the Human Ethics Committee at Victoria University of Wellington, New Zealand [Approval number 28993]. All participants provided written informed consent prior to enrolment in this study.
Supplemental Material
Download MS Word (20.8 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders (DSM‐5®). Arlington, VA: American Psychiatric Publishing.
- Anderson-Chavarria, M. 2021. The autism predicament: models of autism and their impact on autistic identity. Disability and Society, 37, 1321–1341.
- Bannett, Y., Gardner, R. M., Posada, J., Huffman, L. C. and Feldman, H. M. 2022. Rate of pediatrician recommendations for behavioral treatment for preschoolers with attention-deficit/hyperactivity disorder diagnosis or related symptoms. JAMA Pediatrics, 176, 92–94.
- Boshoff, K., Bowen‐Salter, H., Gibbs, D., Phillips, R. L., Porter, L. and Wiles, L. 2021. A meta‐synthesis of how parents of children with autism describe their experience of accessing and using routine healthcare services for their children. Health & Social Care in the Community, 29, 1668–1682.
- Braiden, H.-J., Bothwell, J. and Duffy, J. 2010. Parents’ experience of the diagnostic process for autistic spectrum disorders. Child Care in Practice, 16, 377–389.
- Braun, V. and Clarke, V. 2021. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology, 18, 328–352.
- Braun, V., Clarke, V., Boulton, E., Davey, L. and McEvoy, C. 2021. The online survey as a qualitative research tool. International Journal of Social Research Methodology, 24, 641–654.
- Carr-Fanning, K. and Mc Guckin, C. 2018. The powerless or the empowered? Stakeholders’ experiences of diagnosis and treatment for attention-deficit hyperactivity disorder in Ireland. Irish Journal of Psychological Medicine, 35, 203–212.
- Crane, L., Chester, J. W., Goddard, L., Henry, L. A. and Hill, E. 2016. Experiences of autism diagnosis: a survey of over 1000 parents in the United Kingdom. Autism: The International Journal of Research and Practice, 20, 153–162.
- Dale, E., Jahoda, A. and Knott, F. 2006. Mothers’ attributions following their child’s diagnosis of autistic spectrum disorder: exploring links with maternal levels of stress, depression and expectations about their child’s future. Autism, 10, 463–479.
- Daniels, N. F., Coughlan, B. and Duschinsky, R. 2021. How UK health care professionals conceptualise parental experiences of the diagnostic process for autism spectrum disorder: a qualitative study. SAGE Open Medicine, 9, 20503121211031310.
- Eggleston, M. J., Thabrew, H., Frampton, C. M., Eggleston, K. H. and Hennig, S. C. 2019. Obtaining an autism spectrum disorder diagnosis and supports: New Zealand parents’ experiences. Research in Autism Spectrum Disorders, 62, 18–25.
- Elder, J. H., Brasher, S. and Alexander, B. 2016. Identifying the barriers to early diagnosis and treatment in underserved individuals with autism spectrum disorders (ASD) and their families: a qualitative study. Issues in Mental Health Nursing, 37, 412–420.
- Fergusson, D., Stanley, L. and Horwood, L. J. 2009. Preliminary data on the efficacy of the incredible years basic parent programme in New Zealand. The Australian and New Zealand Journal of Psychiatry, 43, 76–79.
- Fridman, M., Banaschewski, T., Sikirica, V., Quintero, J. and Chen, K. S. 2017. Access to diagnosis, treatment, and supportive services among pharmacotherapy-treated children/adolescents with ADHD in Europe: data from the caregiver perspective on pediatric ADHD survey. Neuropsychiatric Disease and Treatment, 13, 947–958.
- Gibbs, V., Aldridge, F., Sburlati, E., Chandler, F., Smith, K. and Cheng, L. 2019. Missed opportunities: an investigation of pathways to autism diagnosis in Australia. Research in Autism Spectrum Disorders, 57, 55–62.
- Halperin, J. M. and Marks, D. J. 2019. Practitioner review: assessment and treatment of preschool children with attention‐deficit/hyperactivity disorder. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 60, 930–943.
- Hong, J. S., Singh, V. and Kalb, L. 2020. Attention deficit hyperactivity disorder symptoms in young children with autism spectrum disorder. Autism Research, 14, 182–192.
- Izzo, V. A., Donati, M. A., Novello, F., Maschietto, D. and Primi, C. 2019. The Conners 3–short forms: evaluating the adequacy of brief versions to assess ADHD symptoms and related problems. Clinical Child Psychology and Psychiatry, 24, 791–808.
- Kasilingam, N., Waddington, H. and Van Der Meer, L. 2021. Early intervention for children with autism spectrum disorder in New Zealand: what children get and what parents want. International Journal of Disability, Development and Education, 68, 521–537.
- Kazda, L., McGeechan, K., Bell, K., Thomas, R. and Barratt, A. 2022. Association of attention-deficit/hyperactivity disorder diagnosis with adolescent quality of life. JAMA Network Open, 5, e2236364–e2236364.
- Legg, H. and Tickle, A. 2019. UK parents’ experiences of their child receiving a diagnosis of autism spectrum disorder: a systematic review of the qualitative evidence. Autism, 23, 1897–1910.
- Leijten, P., Gardner, F., Landau, S., Harris, V., Mann, J., Hutchings, J., Beecham, J., Bonin, E. M. and Scott, S. 2018. Research review: harnessing the power of individual participant data in a meta‐analysis of the benefits and harms of the incredible years parenting program. Journal of Child Psychology and Psychiatry, 59, 99–109.
- Maenner, M. J., Shaw, K. A. and Baio, J. 2020. Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveillance Summaries, 69, 1.
- Maguire, M. and Delahunt, B. 2017. Doing a thematic analysis: a practical, step-by-step guide for learning and teaching scholars. All Ireland Journal of Higher Education, 9, 1–14.
- Makino, A., Hartman, L., King, G., Wong, P. Y. and Penner, M. 2021. Parent experiences of autism spectrum disorder diagnosis: a scoping review. Review Journal of Autism and Developmental Disorders, 8, 267–284.
- Mitchell, C. and Holdt, N. 2014. The search for a timely diagnosis: parents’ experiences of their child being diagnosed with an autistic spectrum disorder. Journal of Child and Adolescent Mental Health, 26, 49–62.
- Modesto-Lowe, V., Danforth, J. S. and Brooks, D. 2008. ADHD: does parenting style matter? Clinical Pediatrics, 47, 865–872.
- Moore, C. B., McIntyre, N. H. and Lanivich, S. E. 2021. ADHD-related neurodiversity and the entrepreneurial mindset. Entrepreneurship Theory and Practice, 45, 64–91.
- O’Connor, C., Kadianaki, I., Maunder, K. and McNicholas, F. 2018. How does psychiatric diagnosis affect young people’s self-concept and social identity? A systematic review and synthesis of the qualitative literature. Social Science and Medicine, 212, 94–119.
- O’Connor, C. and McNicholas, F. 2020. What differentiates children with ADHD symptoms who do and do not receive a formal diagnosis? results from a prospective longitudinal cohort study. Child Psychiatry and Human Development, 51, 138–150.
- OECD. 2019. Education at a glance 2019 OECD indicators. Paris: OECD.
- Palinkas, L. A., Horwitz, S. M., Green, C. A., Wisdom, J. P., Duan, N. and Hoagwood, K. 2015. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health, 42, 533–544.
- Pierce, K., Gazestani, V. H., Bacon, E., Barnes, C. C., Cha, D., Nalabolu, S., Lopez, L., Moore, A., Pence-Stophaeros, S. and Courchesne, E. 2019. Evaluation of the diagnostic stability of the early autism spectrum disorder phenotype in the general population starting at 12 months. JAMA Pediatrics, 173, 578–587.
- Prata, J., Lawson, W. and Coelho, R. 2018. Parent training for parents of children on the autism spectrum: a review. Health, 5, 1–7.
- Risley, S., Ciesielski, H. A., Loren, R. E., Peugh, J. and Tamm, L. 2020. Effectiveness of behavioral parent training in the outpatient setting for preschoolers at risk for ADHD. Journal of Behavioral and Cognitive Therapy, 30, 291–300.
- Russell, G. and Norwich, B. 2012. Dilemmas, diagnosis and de-stigmatization: parental perspectives on the diagnosis of autism spectrum disorders. Clinical Child Psychology and Psychiatry, 17, 229–245.
- Ryan, S. and Salisbury, H. 2012. You know what boys are like’: pre-diagnosis experiences of parents of children with autism spectrum conditions. British Journal of General Practice, 62, e378–e383.
- Sainsbury, W. J., Carrasco, K., Whitehouse, A. J. O. and Waddington, H. 2022. Parent-reported early atypical development and age of diagnosis for children with co-occurring autism and ADHD. Journal of Autism and Developmental Disorders, 1–12.
- Sayal, K., Prasad, V., Daley, D., Ford, T. and Coghill, D. 2018. ADHD in children and young people: prevalence, care pathways, and service provision. The Lancet Psychiatry, 5, 175–186.
- Sedgwick, J. A., Merwood, A. and Asherson, P. 2019. The positive aspects of attention deficit hyperactivity disorder: a qualitative investigation of successful adults with ADHD. ADHD ttention Deficit and Hyperactivity Disorders, 11, 241–253.
- Soke, G. N., Maenner, M. J., Christensen, D., Kurzius-Spencer, M. and Schieve, L. A. 2018. Prevalence of co-occurring medical and behavioral conditions/symptoms among 4- and 8-year-old children with autism spectrum disorder in selected areas of the United States in 2010. Journal of Autism and Developmental Disorders, 48, 2663–2676.
- Stevens, T., Peng, L. and Barnard-Brak, L. 2016. The comorbidity of ADHD in children diagnosed with autism spectrum disorder. Research in Autism Spectrum Disorders, 31, 11–18.
- Terry, G., Braun, V., Jayamaha, S. and Madden, H. 2018. Negotiating the hairless ideal in Āotearoa/New Zealand: choice, awareness, complicity, and resistance in younger women’s accounts of body hair removal. Feminism and Psychology, 28, 272–291.
- Waddington, H., Shepherd, D., van der Meer, L., Powell-Hector, N., Wilson, E. and Barbaro, J. 2021. Brief report: training New Zealand well child/Tamariki Ora nurses on early autism signs using the social attention and communication surveillance-revised. Journal of Autism and Developmental Disorders, 52, 5050–5057.
- Wallisch, A., Little, L., Dean, E. and Dunn, W. 2020. Parent concerns: differentiating developmental diagnoses in young children. Research in Developmental Disabilities, 103, 103684.
- Whitehouse, A. J. O., Varcin, K. J., Pillar, S., Billingham, W., Alvares, G. A., Barbaro, J., Bent, C. A., Blenkley, D., Boutrus, M., Chee, A., Chetcuti, L., Clark, A., Davidson, E., Dimov, S., Dissanayake, C., Doyle, J., Grant, M., Green, C. C., Harrap, M., Iacono, T., Matys, L., Maybery, M., Pope, D. F., Renton, M., Rowbottam, C., Sadka, N., Segal, L., Slonims, V., Smith, J., Taylor, C., Wakeling, S., Wan, M. W., Wray, J., Cooper, M. N., Green, J. and Hudry, K. 2021. Effect of preemptive intervention on developmental outcomes among infants showing early signs of autism: a randomized clinical trial of outcomes to diagnosis. JAMA Pediatrics, 175, e213298–e213298.
- Wigal, S., Chappell, P., Palumbo, D., Lubaczewski, S., Ramaker, S. and Abbas, R. 2020. Diagnosis and treatment options for preschoolers with attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology, 30, 104–118.