ABSTRACT
Digital transformation is demanding for incumbent organizations such as healthcare, where legacy-based IT architectures challenge the establishment of effective digital services. We refer to this as the IT silo problem, where multiple non-consolidated IT systems are implemented to support expert practices. In this paper, we analyze this challenge using a mirroring lens. Our research question is, how can we create efficient digital services, utilizing the existing legacy systems in healthcare IT architectures? Our empirical evidence comes from a Norwegian case and contributes to the literature on IT architecture within Healthcare. First, we demonstrate how strict mirroring leading to sub-optimization and silofication is a major cause for the presence of IT silos. Second, we describe a process towards adaptive mirroring, and the resulting adaptive mirroring architecture. Adaptive mirroring is an architectural combinatory device that facilitates the design and use of efficient services, while also improving the flexibility of IT architectures.
1. Introduction
In this paper, we investigate how incumbent organisations with multiple legacy systems can improve their efficiency by reconfiguring the IT architecture. By IT Architecture we refer to “the structure and organization by which modern system components and subsystems interact to form systems, and the properties of systems that can best be designed and analyzed at the system level”. (Kruchten et al., Citation2006). In particular, we investigate a certain problem within healthcare, which is the presence of IT silos. IT silos can be understood as the “combination of large, diverse, unintegrated and frequently aging system” (Bannister, Citation2001, p. 66). Inspired by Bannister (Citation2001, p. 66) we see IT silos as “the legacy of decades of introspective development”. IT silos are a known problem in incumbent firms (Ross et al., Citation2019) not least within healthcare (Cebul et al., Citation2008). What causes this problem?
Healthcare organisations can be seen as professional bureaucracies (Mintzberg, Citation1993) consisting of multiple specialised practices such as neurology, pathology, oncology, heart surgery, and so on. The experts need to be innovative, and innovation is best cultivated by allowing decentralised freedom. But innovation based on local and particular needs creates fragmentation (Cebul et al., Citation2008). Thus, while decentralised liberty to innovate and perform complex knowledge processes is an advantage of healthcare organisations, the drawback is the lack of alignment between each group of experts and the health institutions (Lawrence & Lorsch, Citation1967). The downside of the misalignment is inefficient patient logistics when patients move between health institutions. Healthcare IT architectures have emerged on the base of this decentralised logic and are thus characterised by a high degree of diversity but a low degree of integration between institutions (Lawrence & Lorsch, Citation1967). Healthcare IT architectures consist of separate software applications – IT systems – which are difficult to integrate (Bygstad et al., Citation2015). Disconnected IT systems dominated by different expert knowledge standards, reduce the speed and effectiveness of the performance of the system as a whole (Gleiss & Lewandowski, Citation2021). It also challenges patient security and efficient treatment (Feldman, Citation2020).
The tight coupling between clinical practice and IT systems is, thus, considered the main practical cause of the IT silo problem. But the causes for the silo problem are to a lesser extent understood theoretically.
IT silos challenge the fundamental task of coordination within the system as a whole (Castaneda et al., Citation2015; Cebul et al., Citation2008; Miller & Tucker, Citation2014). However, these IT systems are professional legacies that have gradually grown over time in tandem with new expert practices and knowledge. Their legacy is crucial for the institution (Hanseth & Lyytinen, Citation2010). This also means that the digital legacy must be treated with care during transformation processes.
Although the IT silo problem is a logical consequence of expert organisations, it creates difficulties that we need to solve.
Earlier literature has framed this as a strategic problem (Mettler et al., Citation2014) that can be solved by large integrated enterprise architectures or monoliths, that introduce manageable and holistic architectures (Bradley et al., Citation2012). Others have emphasised the need for a bottom-up approach where clinicians’ freedom must be in the front seat (Aanestad & Grisot, Citation2017).
We frame the challenge of tight coupling between expert work and IT systems as mirroring (Colfer & Baldwin, Citation2016). Previous literature has been more occupied with either the system perspective or the user perspective. Using the Mirroring lens enables us to focus on IT architecture challenges from a service perspective in the relationship between the user and the system, and provides a basis for discussing how the relationship can become more adaptive (Lusch & Nambisan, Citation2015).
The mirroring hypothesis suggests “that the formal structure of an organization will (or should) ‘mirror’ the design of the underlying technical system” (Colfer & Baldwin, Citation2016). We frame this as strict mirroring (Colfer & Baldwin, Citation2016). While earlier work has emphasised the importance of strict mirroring between the organisation and IT architecture (Henderson & Clark, Citation1990), we are occupied by how the drawbacks can be reduced. Based on these interests, our research question is, how can we create efficient digital services, utilizing the existing legacy systems in healthcare IT Architectures?
To address this question we investigated a case from Norway, a Nordic country where healthcare is governed by the state. These health systems are increasingly relevant also for a global audience since EPIC – the large American provider of health care, with a different system logic – is being implemented in Denmark, Finland, and Norway (Hertzum et al., Citation2022).
We analyse the case using the mirroring hypotheses and introduce the concept of adaptive mirroring. Adaptive mirroring is generally an architectural principle to facilitate efficient information flow from several sources to the target system. Adaptivity is salient in improving information flow within healthcare (Poba-Nzaou et al., Citation2021). In our framing, adaptive mirroring is an architectural combinatory device that facilitates the design and use of efficient services. To enable adaptive mirroring, the siloed architecture needs to be reconfigured and modularised. We proceed by outlining a couple of existing solutions that engage with the IT silo problem. Both have in our view some shortcomings.
2. The problem of siloed IT architecture in healthcare
The hospital sector is one of the most complex institutions in our society but is also a sector urgently in need of transformation in the years to come. Increasing life expectancy and public expectations accelerate the need for the development of new digital services (Kelly & Young, Citation2017; van Lent et al., Citation2012). Efficient digital services and improved patient logistics are fundamental to achieving a more effective healthcare system (Hertzum & Simonsen, Citation2013; Piening, Citation2011; van Lent et al., Citation2012). The health sector is, however, also dominated by risk-averse non-innovative culture (Kelly & Young, Citation2017; van Lent et al., Citation2012).
The main barrier to enabling transformation within healthcare is siloed IT architectures (Bradley et al., Citation2012; Gleiss & Lewandowski, Citation2021). Siloed IT architectures emerge because healthcare organisations are professional bureaucracies (Mintzberg, Citation1993) consisting of multiple specialised practices. Physicians must solve complex tasks, and specialisation is a way of enabling this (Bygstad & Hanseth, Citation2018). However, specialised organisations have great difficulties obtaining efficient coordination within and between hospital units (Cebul et al., Citation2008; Miller & Tucker, Citation2014; Øvrelid & Halvorsen, Citation2018). Particularly since expertise-related tasks are mirrored in the IT systems. Cebul et al. (Cebul et al., Citation2008) observe that “hospitals have a fragmented structure because of the special role played by physicians. Physicians are central to resource allocation and care processes in the hospital, yet they are typically independent of hospital management”.
Siloed IT architectures are configured to optimise local needs and have a low degree of integration (Lawrence & Lorsch, Citation1967). This is very ineffective when the goal is to facilitate digital services across diverse local settings.
There are two fundamental ways to address inefficiencies caused by a lack of integration within the literature on healthcare IT architecture. One is concentrated on allowing bottom-up innovation based on the needs of the local communities. This stream of literature emphasises cultivation and gradual growth strategies and suggests gateways to bridge the system modules (Grisot et al., Citation2014; Hanseth & Lyytinen, Citation2010). This literature is often based on cases from the Nordic countries, with public sector healthcare (Hertzum et al., Citation2022). The other sees large integrated enterprise architectures or monoliths, as the solution to create manageable and holistic architectures (Bradley et al., Citation2012; Guillemette et al., Citation2022; Mettler et al., Citation2014).
These approaches have clear strengths. One aligns with expertise practices and the clinical perspective but ignores the management needs (Bygstad et al., Citation2015). The other is concerned with top-down managerial control (Bradley et al., Citation2012). The drawback is, however, that centralisation may increase the bureaucratic burden, and reduce the pace of innovation at the local level.
These perspectives could also be combined with a platformization strategy (Bygstad & Hanseth, Citation2018), that introduces a combination of decentralised innovation and centralised alignment (Ross et al., Citation2019). Since platformization brings with it a completely different way of thinking and requires a radical restructuring of, not only the IT architecture but also the way the actors interact, this is very challenging within healthcare (Bygstad & Hanseth, Citation2018).
By splitting up the existing architecture and aligning local and global requirements, a less dramatic innovation effort can be obtained (Bygstad & Øvrelid, Citation2020). We proceed with this ambition by using the mirroring hypotheses. We develop adaptive mirroring as a capability to align local and global needs in healthcare IT architectures.
3. The mirroring hypotheses
The mirroring hypothesis observes that there is a structural correspondence between the IT architecture of a product or a system and the way labour is organised in the organisation (Colfer & Baldwin, Citation2016). A consequence of this is that each part of the organisation has corresponding IT systems. Previous mirroring literature (Colfer & Baldwin, Citation2016; Hylving & Schultze, Citation2020) categorises different degrees of mirroring into, strict mirroring, partial mirroring, and mirror-breaking. We add to this by developing adaptive mirroring as a combinatory capability.
Strict mirroring emphasises that the organisation and its IT architecture “mirror its own organization but not that of its industry”, and that “technical dependencies [are] correlated with communication linkages” (Colfer & Baldwin, Citation2016, p. 720). This condition is optimal when the institutional surroundings and the IT portfolio is relatively stable and the complexity is manageable. Strict mirroring is typical for organisations that operate in specific markets and knowledge organisations within the public sector like healthcare (Cebul et al., Citation2008; Miller & Tucker, Citation2014).
IT systems that support specialised expertise are important characteristics of knowledge organisations, but introduce challenges in two main areas. First, IT silos make communication linkages inefficient (Cebul et al., Citation2008). Secondly, IT silos are difficult to manage and change (Bygstad et al., Citation2015). A negative consequence of strict mirroring is that “firms focused on the current technical architecture may fall victim to architectural innovations arising outside their boundaries” (Colfer & Baldwin, Citation2016, p. 710). Thus, strict mirroring complicates the process of exploring new requirements and solutions (Colfer & Baldwin, Citation2016). This is termed “the mirroring trap”. As the pace of technological change increases and systems become more complex, organisations must also broaden their perspective and explore electronic markets.
Partial mirroring implies that firms engage and invest in knowledge and IT beyond their boundaries. This implies that the coupling between practices and the IT structure is looser. Partial mirroring is crucial for organisations that operate in dynamic markets but also for institutions where the citizen uses integrated services. Partial mirroring requires a more modularised and integrated IT architecture that enables communication across expert domains (Colfer & Baldwin, Citation2016) through modular interfaces (Ghazawneh & Henfridsson, Citation2013). In such cases, organisations can gradually reach a more service-oriented architecture (Erl, Citation2005).
We introduce adaptive mirroring as a specific form of partial mirroring. Adaptive mirroring emphasises the controlled management of information derived from multiple loosely coupled modules (Combs & Vagle, Citation2002; Gavrilovska et al., Citation2001). Specifically, adaptive mirroring enables the target system to adapt its behaviour according to the system and application needs of different types of actors. Adaptive mirroring, thus, facilitates a balance between variety at the local level and integration to strengthen centralised control (Yoo et al., Citation2010). This implies that adaptive mirroring is a capability to reduce silos and facilitate cross-coordination and management (Cebul et al., Citation2008). We see adaptive mirroring as a candidate to solve the challenges introduced by siloed architectures in large incumbent organisations.
While incumbent organisations in both the private and public sectors struggle with the transition from strict mirroring to partial mirroring, born-digital firms are often digital in their basic structure. Platforms have often a three-layer organisation that facilitates tight collaboration between third parties and the platform owner. These new ecosystems (Parker et al., Citation2016; Tiwana, Citation2013) is fundamentally extrovert; the whole point is to operate in multisided markets. Colfer and Baldwin frame this as mirror-breaking. Large digital platforms transform our societies and challenge the classic view of organisational configurations (Mintzberg, Citation1993). This is very challenging within healthcare (Bygstad & Hanseth, Citation2018).
In summary, we use the mirroring lens to identify challenges introduced by siloed IT architecture and identify adaptive mirroring as a conceptual device to align local and global requirements. We proceed by describing our method before we demonstrate the potential contributed enabled by the mirroring lens.
4. Method
This is an in-depth, multilevel qualitative case study (Greenhalgh et al., Citation2010) used to investigate the causes and consequences of the IT silo problem within healthcare. We studied a large-scale reform of the Norwegian health system where the government transferred the ownership of the hospitals from 19 counties to the government. We investigated the impact of the transformation on the IT silo problem at the national, regional, and local levels.
4.1. Data collection
We have engaged for more than 10 years with digitalisation efforts within healthcare in Norway. We have as researchers operated on multiple levels. We have interviewed regional and local CEOs and IT managers. We have also interviewed project managers and ward managers, as well as more than 10 doctors and nurses. We have also performed many observations within local hospitals such as the hospital at Kalnes.
In framing our case, we use the national reform as a point of departure for an in-depth investigation into a particular region (Health South East – HSE) and a particular hospital within that region (Kalnes). The regional and the local level may have different requirements regarding IT architecture, and different ways of addressing the IT silo problem. While the regional requirements address standardisation and integration to improve cross-hospital digital interaction, the local level is occupied with an IT architecture that facilitates innovation through configurable user services. We collected data through 60 semi-structured interviews with managers, strategists, entrepreneurs, project managers, developers, and clinicians, and were active in observing clinicians in action for more than 100 hrs. We also participated in more than 20 seminars and workshops. We had access to a rich library of documents, policies, and drafts. These documents contained organisational plans for IT innovations, including the IT architecture needed to reach the ambitions. In all, more than 1000 pages of written material from various sources were analysed
4.2. Data analysis
Inspired by abduction (Sætre & Van de Ven, Citation2021), we analysed our data in 4 steps (See below, and Appendix 1 for details). First, we did longitudinal analyses of national and regional e-health projects from 2002 to 2019. Our point of departure was the national reform in 2002, and we identified a local innovation project where a new IT architecture was established to reduce the IT silo problem. Then we analysed each level in detail to investigate how a relationship between the organisational unit and the IT architecture was established, and how this relationship changed during the project. We were occupied with how the IT architecture balanced local freedom and central control. In particular, we studied how the IT architecture facilitated the development and configuration of efficient user services for the clinical personnel at the local level, while still maintaining information consistency and security at the regional level. We saw that there was a tendency at the local level to optimise local factors at the expense of global requirements. We also saw that the counter-strategy to reduce the shortcomings of the local approach often led to centralised and distanced management. This reduced the freedom to create innovations and new efficient services at the local level. We then used the mirroring lens to identify the consequences of these challenges in the IT architecture at the three levels. In particular, our longitudinal study at the local hospital Kalnes enabled us to identify and theorise a more adaptive IT architectural approach. In debating with existing literature, we framed this as Adaptive mirroring. We found that adaptive mirroring was central to describing the alignment between regional and local requirements. Moreover, we found that this was a quite precise way of conceptualising a more flexible IT architecture. In the last step, we generalised our findings and found three particular challenges introduced by strict mirroring. Then we elaborated more in-depth on how an adaptive mirroring IT architecture can be described, and how it solves the challenges of strict mirroring.
Table 1. Data analyses.
5. Findings
In this multi-level case study, we demonstrate how the health reform (national level) (5.1) had implications at the regional (5.2) and local levels (5.3) and the measures that were taken to address the reform strategies.
5.1. National level: reforming the Norwegian health sector
Norway is a sparsely populated (5.4 million) but quite large country (324 000 km2). Norway is widely known for its social-democratic welfare state. Equal Healthcare for all citizens is a core motivation for the shifting governments. This also means that Hospitals are geographically spread to be as close as possible to the citizen. Equal healthcare is quite expensive but digitalisation enables new ways of organising and managing the system, as well as new ways of handling patient treatment.
Until 2000, 19 counties were in charge of the administration of the hospitals. This secured the local anchoring of important decisions. There were also important drawbacks. Yearly the 19 counties met up to agree upon budgeting. The negotiations between the 19 counties tended to be lengthy, cumbersome, and characterised by local optimisation. This organisation implied significant use of resources combined with poor financial management, insufficient degree of competence development, a limited amount of research, unclear divisions of overall responsibility, low level of goal management, as well as different management methods in each hospital (Herfindal, Citation2004). Moreover, the treatment had severe qualitative differences, depending on where the patient lived, and the specialised practices were poorly coordinated. In 2002, the government decided to transfer the responsibility of the hospitals from the 19 counties to the central government. They established five regional corporations.
Organisational change: The reform aimed to reduce challenges caused by local optimisation to ensure equity of access to health services for citizens in all parts of the country (Lægreid et al., Citation2005).
However, the reform was built on the existing governance structure of decentralised liberty granted to the practice environments and the local hospitals. The five health regions established boards and delegated ownership control to these boards. Thus, while the government took charge and established centralised ownership, the organisational logic of the previous system was maintained (Lægreid et al., Citation2005). At the same time, through its new role, the central government needed to secure overall coordination wherever this was necessary and appropriate ministerial responsibility. This implied strong vertical coordination and strong sector ministries that challenged the autonomy of the health enterprise (Lægreid et al., Citation2005).
Architectural change: The regions used extensive resources to implement electronic patient records (EPR) at each hospital. EPRs are crucial in creating more efficient patient care, lowering costs, and standardising information flow. Each hospital had extensive liberty to address its particular challenges. As each region and every hospital had its IT budget an abundant flora of IT systems was developed, without centrally governed strategies (Ellingsen & Monteiro, Citation2003). The reform, thus, had no IT strategy. The visionary strategy policies written during this period expressed the need to use the Internet and the newly established “Helsenettet” (health network) to create standardised messages and coordination between systems and devices. A visionary document stated:
A basic principle for a national health network is that one access point, a platform, should be able to support a wide and integrated range of services for electronic interaction, both email, mediation exchange, telemedicine and access to the Internet
Strict Local Mirroring: While the Government quite intrusively reorganised the system, implemented five health regions, and transferred around 40 hospitals to these regions, the attempts to solve the challenges caused by the lack of digital interaction and disruptive information flow were much less intrusive. Apart from some visions on the use of the Internet and a large national supply chain (“Helsenettet”), the task of reducing the impact of siloed architecture at each hospital was left to the five regions.
The individual hospital maintained the liberty to build their system portfolios undisturbed by regional management. These non-standardised systems had often emerged bottom-up, created by local vendors or even clinicians. The systems were not aligned with the goal of digital interaction between health units. We conceptualise this as strict local mirroring, with non-integrated systems and siloed architectures. This condition has two severe drawbacks. The system is very difficult to change and very challenging to manage.
5.2. Regional level: from strict local to strict centralised mirroring in Health South-East
Health South-East (HSE) was the result of a merger between Health South and Health in 2007. HSE is quite large and serves 60% of the Norwegian population.
Organisational change: After the merging in 2007, HSE consisted of 11 Health Enterprises (HE) and over 20 hospitals. Although the Ministry of Health and the corporate board managed HSE, each HE took the daily decisions. The pre-established autonomy regarding responsibility and medical treatment remained, while the interaction between HE and the political authorities was low (Rohde & Torvatn, Citation2017).
Architectural change: The IT strategy became the most important centralising factor in each region. Each region established an autonomous IT unit. In HSE, this IT strategy went through different phases (Øvrelid et al., Citation2017), but the common denominator was centralised management of the interaction between the hospitals and the regional IT unit. A crucial part of this strategic alignment was the centralised architecture created through a mega programme called Digital Renewal. The architecture followed the “best-of-breed” strategy using a BizTalk integration factory to integrate the systems. The factory was extremely complex but facilitated the exchange of digital messages between hospitals within a Health Enterprise (but not between Health Enterprises).
Strict Centralised Mirroring: HSE established a central IT unit and an integration architecture to address some of the coordination challenges between hospitals. The integration engine was very complex with 275 physical integrations and more than 700 system interfaces. The integration architecture required standardised messages, and the region consolidated the most important EPR system, reducing the number of local configurations. The change in the organising logic from local variety to centralised integration meant that IT architects became important actors and that the central IT unit at HSE, Sykehuspartner, became an obligatory passage point for changes in the clinical systems. The new communication linkages governed by the integration engine mirrored a tightly coupled organisation dominated by the central IT unit and IT architects. This strict centralised mirroring significantly reduced the local autonomy to such an amount that local innovation became very difficult. This led to protests from hospitals and clinicians that demanded a greater impact on the development of IT systems and architecture. The regional management established a new governance model to facilitate more local freedom. At the same time, there were also several innovation projects in HSE. One of these was Kalnes Hospital.
5.3. Local level: adaptive mirroring aligning regional and local requirements at Kalnes hospital
After several years of working with the centralised IT architecture, there were still fundamental challenges, exemplified in this quote from an internal strategy document.
With today’s ICT portfolio of applications and point-to-point integrations, Health South-East is unable to offer the necessary pace of change, sustainability, and scalability to adopt new and important functionality that supports the needs of the future. Information storage and end-user functionality are often designed in the same product and without open APIs, which has led to IT silos and technological complexity.
The Kalnes innovation project solved some of these challenges. The hospital opened in November 2015, with both somatic and psychiatric services. Kalnes has 4800 employees, and Kalnes is the first digital hospital in Norway (HIMSS level 6).
Organisational change: The new CIO established a management team, and several project groups with specific goals in mind: (i) to create a digital hospital, (ii) to facilitate a hospital where the patient is at the centre (patient’s health care), (iii) to make sure that the patient flow is based on well-designed processes supported by IT throughout the clinic. The manager for the project said:
I had been engaged with the relationship of process innovation and IT the past 15 years, both theoretically and practically, and I knew what I wanted to achieve: hospital processes should be well defined and supported by information.
The management team started an innovation project with around 25 clinicians working on designing the clinical processes, and a separate group that worked with the process technology.
Architectural change: EPRs and other clinical systems are primarily knowledge-oriented systems configured to optimise standardised clinical practices. These systems struggle to support efficient information sharing throughout the patient flow from admission to discharge. Kalnes acquired a modern and efficient process system with more configurable user services from a global vendor. The process technology consisted of check-in screens, mobile devices, and electronic whiteboards. More efficient user services enabled clinical personnel to configure the information to fit with the process flow. The process-oriented system also enabled integration towards logistics and alarm systems in the physical infrastructure, and thus facilitated integrated control mechanisms. Since Kalnes was the only hospital that acquired this system, it needed to be integrated with the regional infrastructure. The regional architectural “package” consisted of around 300 silo-applications, managed by the central IT unit. A new interface was created to align the “old” infrastructure and the new process system. This integration led to a modular architecture that includes innovative process IT that facilitates patient flow processes through configurable user services (Bygstad & Øvrelid, Citation2020). A nurse said:
Imatis is very configurable, it lets us do many things other systems do not allow
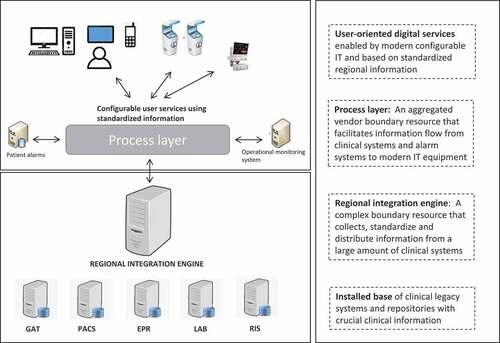
Adoptive Mirroring: Kalnes enjoyed the work done by the centralised IT unit to consolidate and integrate systems. This laid the foundation for an improved information flow. Kalnes developed the initiative further extensively by introducing a process technology that facilitated coordination across IT silos. By reducing the impact of strictly mirrored systems, more efficient services could be created. In particular, the splitting between knowledge systems (EPR, Lab systems, etc.) and locally configurable process systems (Imatis) created an IT architecture that significantly reduced the IT-silo problem. We refer to these combinatory capabilities as adaptive mirroring. summarises our findings and leads us to the discussion and contribution.
Table 2. Summary of the case and the action that changed the IT architecture.
6. Discussion: from strict to adaptive mirroring
We acknowledge that digital transformation is very challenging for the healthcare sector. We do, however, also realise that increasing life expectancy and public expectations accelerate the need for the development of new digital services (Kelly & Young, Citation2017; van Lent et al., Citation2012). Digital services and patient logistics are fundamental to achieving a more effective healthcare system (Hertzum & Simonsen, Citation2013; Piening, Citation2011; van Lent et al., Citation2012).
Siloed IT architecture is a significant barrier to efficient information sharing within healthcare (Cebul et al., Citation2008; Gleiss & Lewandowski, Citation2021; Miller & Tucker, Citation2014). IT silos lead to disconnected information flow, lack of quality in services to the workers and the citizens, and IT architectures that are very difficult to manage. Our research aims to improve the understanding of the IT Silo problems (Bygstad et al., Citation2015; Cebul et al., Citation2008; Miller & Tucker, Citation2014), and propose a possible solution.
6.1. Our research question was, how can we create efficient digital services, utilising the existing legacy systems in complex healthcare institutions?
We analysed the multilevel case using the mirroring hypotheses (Colfer & Baldwin, Citation2016), and provide two contributions regarding the IT silo problem. First, we identify and conceptualise strict mirroring as a central cause of the IT silo problem. This will be addressed in section 6.2. Second, we created a possible solution to the IT Silo problem in the healthcare context conceptualised as adaptive mirroring. We proceed by discussing some implications of these contributions. gives an overview and definitions.
Table 3. Types of mirroring.
6.2. Causes and consequences of IT silos
6.2.1. Strict local mirroring
Professional bureaucracies like healthcare institutions tend to mirror their organisational forms in the IT systems (Mintzberg, Citation1993). This tight coupling between expertise and IT challenges the emergent requirements of efficient digital interaction across organisations (Cebul et al., Citation2008). Important contributions within IS have emphasised the importance of mirroring since IT innovations should be closely adapted to practice innovations (Aanestad & Grisot, Citation2017; Grisot et al., Citation2014; Hanseth & Lyytinen, Citation2010).
A drawback of this form of organisation is sub-optimisation. Sub-optimisation concerns local optimisation at the expense of overall system performance. Our case describes how the pre-reform autonomy was extended after the reform. This gave the hospitals excessive autonomy to configure their IT architecture according to the requirements of the local expertise needs. Although the result was locally anchored IT architectures, they did not facilitate efficient services between hospitals. The overall system goal of efficient digital services within the region was not met.
Sub-optimisation emerges since the local expertise is primarily focused on a limited part of the healthcare system and is spared from the responsibility granted to overall system performance. Sub-optimisation may cause siloification. When each expert area’s organising form mirrors their respective IT systems, the result is multiple systems that are poorly integrated or non-integrated (Cebul et al., Citation2008; Miller & Tucker, Citation2014). This is often referred to as tight coupling (Perrow, Citation2011), which is understandable since standard procedures are an important part of expertise practice (Weick, Citation1976). The drawbacks caused by tight coupling lead to unmanageable IT architectures that are less configurable, and more difficult to change (Tilson et al., Citation2010).
6.2.2. Strict centralised mirroring
The national reform aimed to reduce the IT silo problem. In our case, the reform established a more centralised political control, but since there was no IT strategy, the hospitals continued as before. The weaknesses caused by strict local mirroring remained unsolved. Regional authorities took charge and established a more centralised IT architecture based on principles from enterprise architecture (Bradley et al., Citation2012; Mettler et al., Citation2014). The IT silo problem was reduced through the “best-of-breed” strategy, including the Biz Talk integration engine to enable architectural alignment (Bygstad & Øvrelid, Citation2020). The integration engine integrated a broad range of local systems. However, the centralisation of system management implied that the local hospitals’ autonomy was reduced (Øvrelid et al., Citation2017. Instead, a complex centralised IT unit governed by regional IT engineers gained power. We conceptualise this as strict centralised mirroring since the regional authorities incorporate each hospital in a centralisation logic that implies uniform performance independently of local particularities. This organising logic entails that innovation becomes a centralised activity, performed at a level significantly distanced from the practice environments.
6.3. How can we create efficient digital services, utilising the existing legacy systems in healthcare IT architectures?
We respond to our research question first by briefly describing the process of adaptive mirroring. Then we outline and explain the adaptive mirroring architecture.
6.3.1. From strict to adaptive mirroring
We find that a process from strictly mirrored architecture, towards a more adaptive mirrored architecture, contains at least three central activities: Reconfiguring the silos, modularising the architecture, and implementing a process layer.
First, reconfiguring the silos has similarities to what (Bygstad & Hanseth, Citation2018) conceptualise as platformization. However, reconfiguration (Øvrelid & Kempton, Citation2019) is less intrusive and builds more carefully on the installed base. Reconfiguration entails a splitting (Baldwin & Clark, Citation2000) into knowledge and process layers, as well as loose coupling (Parnas, Citation1972) between them. By the knowledge layer, we refer to clinical systems such as EPR. By process layer, we address logistics, information flow, and digital exchange of patient records (Øvrelid & Kempton, Citation2019).
Second, modularising the architecture implies rearranging the software to become service-oriented (Erl, Citation2005). Three-layer silo systems with few interfaces do not encourage efficient information flow (Ross et al., Citation2019). The introduction of a modularised architecture facilitates effective information exchange (Tiwana, Citation2013; Yoo et al., Citation2010). This requires the implementation of service-oriented boundary resources (Ghazawneh & Henfridsson, Citation2013) that encourage the use and re-use of information in the various systems.
Third, there is a need for a process layer that is deeply concerned with user services and the effective configuration of information. This is close to what Bygstad (Bygstad, Citation2017) frames as a lightweight IT knowledge regime. The process layer has a particular responsibility towards usability (Øvrelid & Sanner, Citation2020) to enable a user to swiftly implement changes when needed.
6.3.2. Adaptive mirroring architecture
In our framing, adaptive mirroring is a combinatory capability established to enable a balance between central and local requirements (see below for pros and cons). Adaptive mirroring, thus, allows both central and local innovation, and configuration of user services. The regional authorities must make sure that the IT architecture can operate efficiently, and that digital services can flow efficiently between hospitals. The local authorities must make sure that local innovation and configuration are possible. These different interests can be solved by establishing an architectural design that distinguishes between regional and local systems.
Table 4. Pros and cons of adaptive mirroring.
The adaptive mirroring architecture () is layered. The first layer consists of the basic infrastructural services such as clinical systems and repositories. These legacy systems’ content is crucial when more adaptive architectures are established (Aanestad & Grisot, Citation2017). The second layer is the regional integration engine, which is a complex boundary resource that collects and distributes clinical information (Bygstad & Øvrelid, Citation2020). In our case, the boundary resource is based on BizTalk technology, and through the Kalnes project, it was given an important role as a distributor of information to the process technology. The third layer is the local process layer, which is an aggregated vendor boundary resource that facilitates information flow from clinical systems to modern IT equipment (Bygstad & Øvrelid, Citation2020). This vendor boundary resource interacts with the physical infrastructure of logistics and alarm systems (Bygstad & Øvrelid, Citation2020). The fourth layer is the user-oriented digital services enabled by modern configurable IT (like smartphones, whiteboards, check-in screens, or medical-technical equipment). The local innovation project at Kalnes allows us to theorise adaptive mirroring. The Kalnes management group was from the start occupied with the profound need for a process-oriented solution that provided configurable user services to clinical expertise (Bygstad & Øvrelid, Citation2020). The harvesting of information from clinical systems to modern digital systems created a robust and powerful solution. The solution is also configurable for each hospital. While the regional integration engine is used by all the hospitals, the process system is used by Kalnes. A modularised and layered architecture (Tilson et al., Citation2010; Yoo et al., Citation2010), is a good base for a more service-oriented architecture with less siloification.
The adaptively mirrored IT architecture (used by Kalnes) is loosely coupled (Yoo et al., Citation2010) since it distinguishes between local and regional requirements, and between the organisation and IT architecture. This also means that the IT architecture will have more centralised control while simultaneously providing more appropriate user services (Bygstad & Øvrelid, Citation2020), more local innovation (Øvrelid & Sanner, Citation2020) while maintaining regional requirements (Bygstad & Hanseth, Citation2016). This type of adaptively mirrored IT architecture may also improve manageability by using standardised IT products (like mobile technology) with flexible interfaces (Hylving & Schultze, Citation2020). Looser coupling between the expertise and the IT architecture technology may improve overall performance, and facilitate practice innovation. Adaptive mirroring also provides a connection between innovative discourses and existing digital infrastructures (Øvrelid & Bygstad, Citation2019)
Despite several advantages, some demanding changes are needed to implement a system based on adaptive mirroring (see ). Firstly, it requires a transformation from a regime where either the local or the central authorities has full control, towards a governance regime that combines these control mechanisms. This requires a systematic balancing of which tasks can be done locally (like process and user innovation), and which must be done centrally (security, consolidation of technological core). Secondly, such a change requires a transformation of the IT architecture towards a modular and layered architecture that facilitates innovation. This change must probably take place incrementally through a gradual breakdown into different regimes (see chapter above). Thirdly, since user innovation can be implemented directly, mechanisms are needed to safeguard security in the service layer so that the functions implemented do not create a risk to the patient.
7. Conclusion
In this paper, we investigate a transformation initiative that had the purpose to improve digital interaction between healthcare institutions. We find that Siloed IT architectures make efficient digital interaction challenging. Our empirical evidence comes from a case in Norway, where we analysed a national transformation initiative and its consequences on the regional and local levels. We contribute to the literature on IT architecture within healthcare by improving the understanding of the IT silo problem, and by proposing a solution to it.
First, we find that strict mirroring that leads to sub-optimisation and silofication is a major cause for the presence of IT Silos. Second, we demonstrate how adaptive mirroring – a modular strategy for combining global and local requirements in IT architecture – improves the changeability and manageability of IT architectures. Changeability in the sense that it allows local innovation, while at the same time ensuring central control. Manageability since a decentralised regime that allows distributed governance that strengthens process and user innovation is implemented.
Disclosure statement
No potential conflict of interest was reported by the author.
References
- Aanestad, M., & Grisot, M. (2017). Information infrastructures within European Health Care, health informatics (O. Hanseth & P. Vassilakopoulou, Eds.). Springer International Publishing. https://doi.org/10.1007/978-3-319-51020-0
- Baldwin, C. Y., & Clark, K. B. (2000). Design rules: the power of modularity. MIT press.
- Bannister, F. (2001). Dismantling the silos: Extracting new value from IT investments in public administration. Information Systems Journal, 11, 65–84. https://doi.org/10.1046/j.1365-2575.2001.00094.x
- Bradley, R. V., Pratt, R. M. E., Byrd, T. A., Outlay, C. N., & Wynn, D. E., Jr. (2012). Enterprise architecture, IT effectiveness and the mediating role of IT alignment in US hospitals. Information Systems Journal, 22(2), 97–127. https://doi.org/10.1111/j.1365-2575.2011.00379.x
- Bygstad, B. (2017). Generative innovation: A comparison of lightweight and heavyweight IT - Bendik Bygstad, 2017. Journal of Information Technology, 32(2), 180–193. https://doi.org/10.1057/jit.2016.15
- Bygstad, B., & Hanseth, O. Governing e-health infrastructures: dealing with tensions. Presented at the ICIS 2016, Dublin, Ireland. 2016.
- Bygstad, B., & Hanseth, O., Transforming digital infrastructures through platformization, in: research papers. Presented at the European Conference of Information Systems (ECIS), Portsmouth, UK. 2018.
- Bygstad, B., Hanseth, O., & Le, D. T., From IT silos to integrated solutions. A study in e-health complexity. Presented at the European Conference of Information Systems, Münster, Germany. 2015.
- Bygstad, B., & Øvrelid, E. (2020). Architectural alignment of process innovation and digital infrastructure in a high-tech hospital. European Journal of Information Systems, 29(3), 220–237. https://doi.org/10.1080/0960085X.2020.1728201
- Castaneda, C., Nalley, K., Mannion, C., Bhattacharyya, P., Blake, P., Pecora, A., Goy, A., & Suh, K. S. (2015). Clinical decision support systems for improving diagnostic accuracy and achieving precision medicine. Journal of Clinical Bioinformatics, 5(1), 4. https://doi.org/10.1186/s13336-015-0019-3
- Cebul, R. D., Rebitzer, J. B., Taylor, L. J., & Votruba, M. E. (2008). Organizational fragmentation and care quality in the U.S Healthcare System. Journal of Economic Perspectives, 22(4), 93–113. https://doi.org/10.1257/jep.22.4.93
- Colfer, L. J., & Baldwin, C. Y. (2016). The mirroring hypothesis: Theory, evidence, and exceptions. Industrial and Corporate Change, 25(5), 709–738. https://doi.org/10.1093/icc/dtw027
- Combs, N., & Vagle, J., Adaptive mirroring of system of systems architectures,Proceedings of the First Workshop on Self-Healing Systems, WOSS ’02. Association for Computing Machinery, New York, NY, USA, pp. 96–98. 2002. https://doi.org/10.1145/582128.582147
- Ellingsen, G., & Monteiro, E. (2003). Big is beautiful: electronic patient records in large Norwegian hospitals 1980s – 2001. Methods of Information in Medicine, 42(04), 366–370. https://doi.org/10.1055/S-0038-1634231
- Erl, T. (2005). Service-oriented architecture: Concepts, technology, and design. Prentice Hall Professional Technical Reference.
- Feldman, S. S. (2020). Health informatics, healthcare quality and safety, and healthcare simulation: Continuing the discussion to advance healthcare operations. Health Systems, 9(1), 1. https://doi.org/10.1080/20476965.2020.1732013
- Gavrilovska, A., Schwan, K., & Oleson, V., Adaptable mirroring in cluster servers, Proceedings 10th IEEE International Symposium on High Performance Distributed Computing. pp. 3–13. 2001. https://doi.org/10.1109/HPDC.2001.945171
- Ghazawneh, A., & Henfridsson, O. (2013). Balancing platform control and external contribution in third-party development: The boundary resources model. Information Systems Journal, 23(2), 173–192. https://doi.org/10.1111/j.1365-2575.2012.00406.x
- Gleiss, A., & Lewandowski, S. (2021). Removing barriers for digital health through organizing ambidexterity in hospitals. Journal of Public Health, 30(1), 21–35. https://doi.org/10.1007/s10389-021-01532-y
- Greenhalgh, T., Stramer, K., Bratan, T., Byrne, E., Hinder, S., & Potts, H., THE DEVIL’S in the DETAIL: Final report of the independent evaluation of the summary care record and HealthSpace programmes. 2010. 1–23.
- Grisot, M., Hanseth, O., & Thorseng, A. (2014). Innovation of, in, on infrastructures: articulating the role of architecture in information infrastructure evolution. Journal of the Association for Information Systems, 15(4), 197–219. https://doi.org/10.17705/1jais.00357
- Guillemette, M. G., Raymond, L., & Paré, G. (2022). Assessing the maturity and performance of the IT function in acute-care hospitals: A configurational view. Health Systems, 0, 1–13. https://doi.org/10.1080/20476965.2022.2075797
- Hanseth, O., & Lyytinen, K. (2010). Design theory for dynamic complexity in information infrastructures: the case of building internet. Journal of Information Technology, 25(1), 1–19. https://doi.org/10.1057/jit.2009.19
- Henderson, R. M., & Clark, K. B. (1990). Architectural innovation: the reconfiguration of existing product technologies and the failure of established firms. Administrative Science Quarterly, 35(1), 9–30. https://doi.org/10.2307/2393549
- Herfindal, S. 2004. Veien frem til sykehusreformen: en studie av beslutningsprosessen bak lov om helseforetak (No. Rapport 5-2004). Bergen: Rokkansenteret.
- Hertzum, M., Ellingsen, G., & Cajander, Å. (2022). Implementing large-scale electronic health records: experiences from implementations of epic in Denmark and finland. International Journal of Medical Informatics, 167, 104868. https://doi.org/10.1016/j.ijmedinf.2022.104868
- Hertzum, M., & Simonsen, J. (2013). Work-practice changes associated with an electronic emergency department whiteboard. Health Informatics Journal, 19(1), 46–60. https://doi.org/10.1177/1460458212454024
- Hylving, L., & Schultze, U. (2020). Accomplishing the layered modular architecture in digital innovation: The case of the car’s driver information module. Journal of Strategic Information Systems, 29(3), 101621. https://doi.org/10.1016/j.jsis.2020.101621
- Kelly, C. J., & Young, A. J. (2017). Promoting innovation in healthcare. Future Hospital Journal, 4(2), 121–125. https://doi.org/10.7861/futurehosp.4-2-121
- Kruchten, P., Obbink, H., & Stafford, J. (2006). The past, present, and future for software architecture. IEEE Software, 23(2), 22–30. https://doi.org/10.1109/MS.2006.59
- Lægreid, P., Opedal, S., & Stigen, I. M. (2005). The Norwegian hospital reform: balancing political control and enterprise autonomy. Journal of Health Politics, Policy and Law, 30(6), 1027–1064. https://doi.org/10.1215/03616878-30-6-1027
- Lawrence, P. R., & Lorsch, J. W. (1967). Differentiation and integration in complex organizations. Administrative Science Quarterly, 12(1), 1–47. https://doi.org/10.2307/2391211
- Lusch, R. F., & Nambisan, S. (2015). Service innovation: A service-dominant logic perspective. MIS Quarterly, 39(1), 155–176. https://doi.org/10.25300/MISQ/2015/39.1.07
- Mettler, T., Fitterer, R., Rohner, P., & Winter, R. (2014). Does a hospital’s IT architecture fit with its strategy? An approach to measure the alignment of health information technology. Health Systems, 3(1), 29–42. https://doi.org/10.1057/hs.2013.10
- Miller, A. R., & Tucker, C. (2014). Health information exchange, system size and information silos. Journal of Health Economics, 33, 28–42. https://doi.org/10.1016/j.jhealeco.2013.10.004
- Mintzberg, H. (1993). Structure in fives: Designing effective organizations, structure in fives: Designing effective organizations. Prentice-Hall, Inc.
- Øvrelid, E., & Bygstad, B. (2019). The role of discourse in transforming digital infrastructures. Journal of Information Technology, 34(3), 221–242. https://doi.org/10.1177/0268396219831994
- Øvrelid, E., Bygstad, B., & Hanseth, O., Discursive formations and shifting strategies in e-health programmes, Research Papers. Presented at the European Conference of Information Systems (ECIS), Guimarães, Portugal, pp. 873–886. 2017.
- Øvrelid, E., & Halvorsen, M. R. (2018). Supporting process innovation with lightweight IT at an emergency unit. Journal of Integrated Design and Process Science, 22(2), 27–44. https://doi.org/10.3233/jid-2018-0009
- Øvrelid, E., & Kempton, A., 2019. From recombination to reconfiguration: Affording process innovation in digital infrastructure, Research Papers. Presented at the European Journal of Information Systems (ECIS).
- Øvrelid, E., & Sanner, T. A. (2020). Sense-able process innovation in digital health infrastructures. Scandinavian Journal of Information Systems, 32(1), 81–116.
- Parker, G. G., Alstyne, M. W. V., & Choudary, S. P. (2016). Platform Revolution: How Networked markets are transforming the economy and how to make them work for you. W. W. Norton & Company.
- Parnas, D. L. (1972). On the criteria to be used in decomposing systems into modules. Communications of the ACM, 15(12), 6. https://doi.org/10.1145/361598.361623
- Perrow, C. (2011). Normal accidents: Living with high risk technologies. Princeton University Press.
- Piening, E. P. (2011). Insights into the process dynamics of innovation implementation. Public Management Review, 13(1), 127–157. https://doi.org/10.1080/14719037.2010.501615
- Poba-Nzaou, P., Uwizeyemungu, S., Dakouo, M., Tchibozo, A., & Mboup, B. (2021). Patterns of health information exchange strategies underlying health information technologies capabilities building. Health Systems, 11(3), 1–21. https://doi.org/10.1080/20476965.2021.1952113
- Rohde, T., & Torvatn, H. (2017). A strategic document as a tool for implementing change. Lessons from the merger creating the South-East Health region in Norway. Health Policy, 121(5), 525–533. https://doi.org/10.1016/j.healthpol.2017.02.014
- Ross, J. W., Beath, C. M., & Mocker, M. (2019). Designed for digital: How to architect your business for sustained success. MIT Press.
- Sætre, A. S., & Van de Ven, A. (2021). Generating theory by abduction. Academy of Management Review, 46(4), 684–701. https://doi.org/10.5465/amr.2019.0233
- Sosial og helsedepartementet. 2000. “Si @!” : elektronisk samhandling i helse- og sosialsektoren : statlig tiltaksplan 2001-2003 (Statlig tiltaksplan 2001-2003).
- Tilson, D., Lyytinen, K., & Sørensen, C. (2010). Research commentary —digital infrastructures: The missing is research agenda. Information Systems Research, 21(4), 748–759. https://doi.org/10.1287/isre.1100.0318
- Tiwana, A. (2013). Platform ecosystems: Aligning architecture, governance, and strategy. Newnes.
- van Lent, W. A., Sanders, E. M., & van Harten, W. H. (2012). Exploring improvements in patient logistics in Dutch hospitals with a survey. BMC Health Services Research, 12(1), 232. https://doi.org/10.1186/1472-6963-12-232
- Weick, K. E. (1976). Educational organizations as loosely coupled systems. Administrative Science Quarterly, 21(1), 1–19. https://doi.org/10.2307/2391875
- Yoo, Y., Henfridsson, O., & Lyytinen, K. (2010). Research commentary—the new organizing logic of digital innovation: An agenda for information systems research. Information Systems Research, 21(4), 724–735. https://doi.org/10.1287/isre.1100.0322
Appendix
Appendix 1
Appendix 1 – Explanation for , steps 1–4
Definitions:
Iterations are rounds of processing to identify key events and key entities based on the researcher’s knowledge, empirical data, and new data.
Coding is used to describe the concrete empirical and theoretical use of concepts and how they are connected to data harvested from the research setting.
STEP 1: Number of iterations to identify key events: 3.
Point of departure:
investigating and exploring possible causes for inefficient digital services, we identified the IT silo problem as a major issue.
Iteration 1: The point of departure was the national reform, and the centralisation of management in 5 (later 4) health regions. At the regional level, the IT unit remained decentralised, attached to particular hospitals.
Code 1: Local optimisation of IT architecture
Iteration 2: The centralisation of the IT units from particular hospitals to a new central IT Unit
Code 2: Regional centralisation of IT unit
Iteration 3: Centralisation of IT program (It architecture and IT governance) at the region of HSE after 2010.
Code 3: Regional centralisation of IT architecture.
STEP 2:
Number of iterations to identify key events: 3
Iteration 1: Process innovation at the new hospital. A new system was acquired to improve patient flow services.
Code 4: Splitting the architecture into two parts: Process and clinical systems
Iteration 2: Alignment in the IT architecture between lightweight IT (local) and heavyweight IT (regional)
Code 5: Alignment between process and clinical systems
Iteration 3: The gradual transition in discourse from central to local innovation within the region
Code 6: New governance model
STEP 3: Abduction to address hunches and ideas (Sætre & Van de Ven, Citation2021), creation of the theoretical framework, and inductive testing of the framework
Iteration 1: Identification of trends: local freedom gives local optimisation, and central control limit local innovation. Kalnes innovation project introduces novel ideas in the region
Code 7: More open innovation
Iteration 2: Discourse on healthcare IT architecture to solve IT silo problems, bottom-up: occupied with practices, top-down: occupied with holistic management.
Iteration 3: theoretical reflection on various frameworks to describe the challenges introduced by shifting regimes. Mirroring is chosen
Code 8: Mirroring to describe the relation between organisation and technology.
Iteration 4: Construct a framework based on mirroring (using existing literature): strict, partial, and adaptive.
Iteration 5: Testing out the framework inductively on research data.
Code 9: Adaptive mirroring as a model with looser coupling
STEP 4: Theorising mirroring and describing a process to reach adaptive mirroring architecture.
Iteration 1: Comparing theoretical framework with existing theory in IS. Several rounds of debate. Theorise strict mirroring (local and centralised)
Iteration 2: Develop an architectural sketch to illustrate adaptive mirroring. Comparison with earlier mirroring forms. Pros and cons described.