ABSTRACT
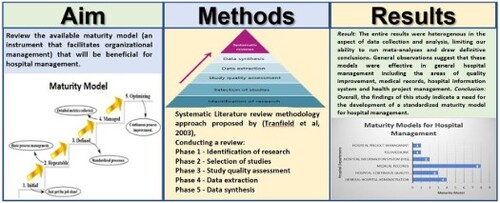
With the uncertainty that came with the COVID-19 Pandemic and its test on the healthcare system, the healthcare institutions around the world with their governments have realized some gaps in the management of the healthcare system. While some hospitals are still recovering from the adverse effect of the pandemic, it is important to review the available maturity model (an instrument that facilitates organizational management) that will be beneficial for hospital management. This article will help to identify various maturity models available for all areas of hospital management. Each identified maturity model will indicate the methods of development and validation, phase and scope.
1. Introduction
1.1. Background of the study
Maturity models have become ubiquitous tools across various domains, serving as frameworks for assessing the progress and capabilities of individuals, teams, and organizations. These models provide a structured roadmap for understanding current performance, identifying areas for improvement, and driving continuous growth. This research paper addresses areas relating to the concept of maturity models for hospital management, exploring their key characteristics, applications, and benefits.
1.1.1. Defining maturity models
At its core, a maturity model is a reference framework that defines different levels of proficiency or effectiveness in a specific domain. These levels are typically arranged hierarchically, each representing a more advanced and optimized performance state than the preceding ones. The model outlines each level's key characteristics, practices, and capabilities, allowing organizations or individuals to benchmark their current standing and chart an improvement course. Maturity models are tools that help manage organizations, and hospital organizations are no exception [Citation1]. Some countries have decided to reform their healthcare systems based on diagnostic-related groups (DRGs) to improve the transparency and stability of healthcare costs. DRGs are used to classify medical treatments and pay for individual cases, resulting in active competition between hospitals and forcing them to be more efficient and effective. As a result, hospitals invest heavily in process orientation and management. However, there is yet to be a consensus on the opportunities that hospitals need to adopt to become process-oriented, nor a general agreement on the sequence of development stages they must traverse [Citation2].
In the healthcare sector, maturity models can be used to address the complexities and vast needs of healthcare systems [Citation3,Citation4]. Rising costs, limited healthcare budgets, and low workforce segregation put pressure on the public health system [Citation5]. The effects of the COVID-19 pandemic on hospitals have shown the disparity in the preparedness of healthcare providers and the maturity level of quality management to achieve safe, effective, patient-centered, timely, and equitable patient care [Citation6]. The effectiveness of quality improvement intervention is highly dependent on its alignment with the specific needs and characteristics of the targeted health system [Citation7]. This research paper presents an overview of the ‘Maturity Models’ for hospital management; the research methods adopted in the literature review were discussed, and the results of the literature review, i.e. the 19 identified Maturity Models for hospital management, were discussed. The paper was concluded with a summary and recommendations.
Table 1. PICO framework.
1.2. Overview of maturity models for hospital management
Well-managed healthcare institutions can reflect the advanced planning and oversight process. Many maturity models have been developed in the health sector, although these are still in the early stages of development [Citation8]. The basic idea behind the maturity model is that mature organizations do things systematically. In contrast, immature organizations achieve results thanks to the courageous efforts of individuals using the methods they have developed and used. Healthcare institutions have tried to reduce costs and increase productivity by implementing enterprise resource planning systems [Citation9].
Academicians and practitioners have developed a broad maturity model in recent years to identify and understand the strengths and weaknesses of unit design [Citation10]. Maturity models have become an essential topic in management research and are defined as a multidisciplinary framework of concepts that describes typical patterns in developing organizational skills [Citation8]. The maturity models are based on the principle that human processes and development organizations develop to a higher capacity level after the development process, which includes the evolutionary sequence of the model stages [Citation11]. The maturity model can be used to support health managers with effective management and continuous improvement for complex and multifaceted initiatives in hospital management [Citation12]. While current research emphasizes increasingly rigorous approaches to developing maturity models, there needs to be more attention to the effective implementation of maturity models in complex organizations like hospitals [Citation13].
Many standards have been developed to address the integration of healthcare providers, particularly healthcare data exchange between healthcare organizations [Citation9,Citation14]. These are helpful indicators when examining patient quality of care. In the health sector, healthcare services often involve individuals and organizations that are more collaborative. Their ability to interact will significantly affect their ability to provide safe, reliable, efficient, and effective health services [Citation15]. The maturity model can foster better communication and alignment within the hospital as a healthcare organization.
1.3. Rationale/Gap of the study
Despite the widespread adoption of maturity models across various domains, several vital gaps still need to be in our understanding and utilization of these frameworks in hospital management. This systematic review tries to identify unique and specific maturity models for effective hospital management. Existing literature often focuses on specific models or applications, overlooking broader theoretical foundations and potential limitations. This study aims to provide a holistic understanding of maturity models, encompassing their essential characteristics and functions. While proponents often tout the advantages of maturity models, their potential drawbacks and limitations can be under-examined. This study critically assesses the benefits and challenges of implementing specific maturity models for hospital management, providing a balanced perspective for healthcare managers. More investigation is needed into adapting and customizing existing models to specific contexts and needs. Addressing these gaps will contribute to a more nuanced and grounded understanding of maturity models, enabling hospitals and other organizations to leverage their potential more effectively while mitigating potential risks. It will also inform the development of more rigorous and adaptive maturity models that better serve the needs of different stakeholders, including hospitals [Citation16]. Motivated by these considerations, the authors pose the research question: What are the available maturity models for hospital management?
1.4. Research aim and objective
This study aims to critically review the available maturity models that will benefit hospital management. This study's specific objectives include:
To identify and categorize existing maturity models applicable to all areas of hospital management, including their target domains, developers, and stage/level structures.
To evaluate the benefits and challenges associated with implementing hospital management maturity models.
2. Methodology
In order to conduct a comprehensive systematic review of the literature, it was decided to define strategies to identify and analyze the currently available literature on MM about hospital management that are relevant to be applied to this research paper. The study employed the PICO framework to ensure a reliable, valid, applicable, and complete review. This structure breaks down the research question into critical components: target population, intervention, comparison, and desired outcome. This facilitates a more organized approach to research design and analysis Table 1.
The method for conducting a review relevant to a maturity model for hospital management was the approach proposed by Tranfield et al. [Citation17]. They suggested five phases for a systematic literature review.
In the first phase, ‘identification of research,’ to ensure a neutral and thorough analysis, systematic reviews employ a comprehensive and unbiased search process starting with selecting precise keywords and search terms. The authors identified the terms, keywords, and combinations to be used as criteria for a literature review. The study employed a systematic search strategy across three databases: PubMed, Taylor & Francis, Springer, Elsevier, Science Direct, and Google Scholar. Utilizing the ‘Boolean Operators,’ advanced searches were conducted in each database using relevant keywords and phrases [].
Table 2. Search criteria for review of literature.
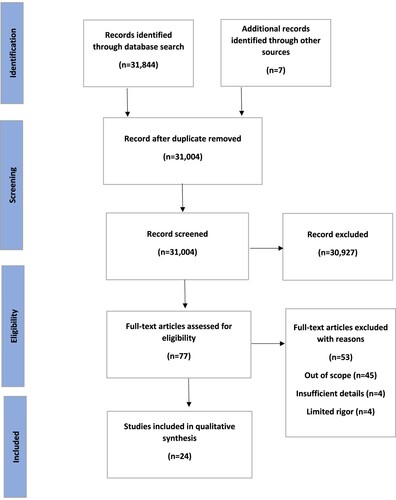
The second phase, ‘selection of studies,’ identifies the relevant work that contains the keywords and the identified term. Meeting strict inclusion criteria was essential for the review study; any mismatch or unwanted feature led to exclusion. The authors employed a rigorous multi-step process to ensure a comprehensive and unbiased selection of studies. They began by screening all potentially relevant citations from their search results. Subsequently, they retrieved and thoroughly evaluated the full text of promising sources, ultimately selecting only those that met the inclusion criteria for the systematic review. The number of studies included and excluded at each stage, along with the rationale for exclusions, is documented in .
2.1. Selection criteria
The paper selection process began with meticulously screening titles and abstracts to pinpoint papers relevant to hospital management maturity models. We searched for papers addressing aspects of hospital management maturity models. Subsequently, we selected papers that met the following criteria: peer-reviewed publication, English language, complete online accessibility, and publication within the last five years (with some exceptions for highly significant papers exceeding the five-year threshold). The literature review articles were found on various web search platforms: PubMed, Taylor & Francis, Springer, Elsevier, Science Direct, and Google Scholar. All studies where maturity models were mentioned were gathered to ensure more inclusive and quality criteria [].
Table 3. Selection criteria.
Each model was scrutinized, considering their scope, description, phases, and methods taken in their development and validity process. After removing irrelevant entries and duplications, 31,004 papers were included for title review. After reading the title, 30,927 papers on a maturity model that do not use the word healthcare or hospital in their title were excluded since they were not directly related to healthcare or hospital management, and 77 papers relevant to healthcare full-text criteria were reviewed. Fifty-three more were excluded due to other reasons like (Out of scope (n = 45), Insufficient details (n = 4), and Limited rigor (n = 4)). Finally, the remaining 24 papers that met all the inclusion criteria were retained. [] shows the steps followed in the selection criteria.
In the third phase, ‘study quality assessment,’ the identified research articles are evaluated, and a selection of papers that meet specific quality standards []. Assessing the trustworthiness of a study's findings by examining how effective its design, execution, and data analysis were in reducing potential biases and errors. To assess the quality of the literature, the CASP (Critical Appraisal Skills Programme) Checklist for systematic review was employed [Citation18].
Table 4. CASP Analysis for all studies addressed in the literature review.
In the fourth phase, ‘data extraction and monitoring,’ the authors employ data-extraction forms to reduce error and bias. Relevant information was extracted from the selected literature; this information was used to construct a summary table [] and to perform data synthesis.
Table 5. Summary and comparison of maturity models for hospital management.
The fifth phase, ‘data synthesis,’ the cumulation of the findings from the relevant literature, was done by narrative review that attempts to identify evidence to answer the research question.
3. Results
3.1. Identify and categorize existing maturity models applicable to all areas of hospital management, including their target domains, developers, and stage/level structures
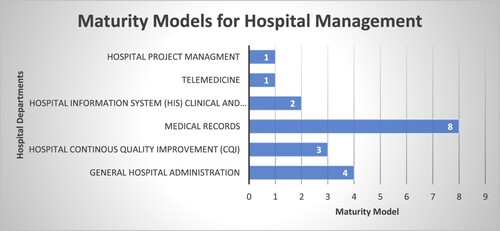
The literature review identified 19 maturity models relevant to hospital management adopted for this study [].
1. Hospital cooperation maturity model (HCMM)
HCMM took the following design decisions to create a maturity model. It considers new phenomena, e.g. Increased network and health cooperation. It focuses on intra-institutional and inter-institutional aspects related to improving the structure and cooperation process in the hospital. In addition, it intends to support beyond the decisions of hospital managers. Its design model uses multidimensional approaches to measure maturity, including elements of competency, strategy, organization, and technique. It also identifies challenges to cooperation and comprehensively supports cooperation improvement [Citation20]. The maturity model of hospital collaboration has three (3) structures: First, the strategic dimension – which measures the capacity of the hospital's external cooperation with external partners. Second is the organizational dimension – which measures the capacity for internal cooperation in the hospital; the third and final dimension is the information dimension – which measures the technical capabilities of the hospital to effectively and efficiently provide the information technology infrastructure necessary for internal and external cooperation [Citation20].
2. Maturity model of hospital (MMH)
It can be seen as an indicator of hospital improvement strategies and studies of achievable levels of improvement at all stages [Citation21]. It summarizes the evaluation criteria conducted by the hospital to assess the level of maturity using the Balanced Scorecard (BSC) used when using the CMMI strategy and framework as a model of process maturity. The framework has the following dimensions: (1) BSC is a framework that has been used strategically in management companies in recent years. It is also used for the PDCA cycle planning phase. Four (4) aspects make up the balanced scorecard: client finance, internal processes, learning, and growth. MMH Maturity Level Rules follow three basic rules: (1) Bmw (Keyword for Maturity Model), (2) Bmp (Medical Priority), and Bhfa (average hospital function). The level of MMH maturation is divided into six stages, from L0 (inactive phase) to L5 (optimized phase) based on CMMI [Citation21].
3. High reliability health care maturity model (HrHCM)
Despite significant efforts to improve the quality of care, medical errors in hospitals are growing alarmingly. Some of these errors that cause harm to patients can be prevented [Citation22]. HRHCM is a model for achieving the credibility of a risk-free medical error in healthcare organizations, including three critical areas of leadership, safety, and sustainable process improvement. The lack of tools to classify hospitals according to their characteristics of high-reliability organizations (HROs) has hindered the progress toward implementation and maintained the basis of high-reliability organization practice. The hospital will benefit from both an understanding of the nature of the organization that supports the implementation of high-reliability organizations and knowledge of the steps needed to achieve the HRO status to reduce the risk of disability and improve outcomes [Citation23].
4. Healthcare data quality maturity model (HDQM)
The credibility of healthcare data quality has been an issue within the development of the healthcare system. There is ample evidence that D.Q.s in registered patients have abnormalities and errors that must be evaluated and improved. If not improved, these problems can create issues in the health services provided. It operates from a scenario where the information system has the essential elements and the basis for its characteristics. This Healthcare data quality maturity model (HDQM) comprises the following elements: level of maturity, area performance, process, and value creation. HDQM focuses on precision, completeness, uniqueness, and duplication [Citation24].
5. Meaningful use (Forrester model)
There are many different systems and organizations for managing medical records and work processes around them. Healthcare providers meet these challenges by using different approaches. These differences in approach have resulted in a three-stage maturity model that uses content, collaboration, and workflow technologies as blocks for change. This model helps service providers evaluate the content, collaboration, and workflow status and, more importantly, identify the roadmaps needed to move on to the next level. Three (3) levels are involved: Level 1: Patient records based on paper or cover art. Level 2: Access to stand-alone databases (electronic health records) is improving. Level 3: Access to digital medical records is role-based [Citation25].
6. Healthcare analytics adoption model (HAAM)
The Health Analysis Approval Model (HAAM) allows healthcare organizations to approve and implement extensive data analyses to improve patient outcomes and reduce costs [Citation26]. This model focuses on analytical capabilities to continuously improve patient outcomes. This is a nine-level approach that involves the following: Level 1 deals with enterprise data operation system, level 2 standardized vocabulary and patient registries, level 3 automated internal reporting, level 4 automated external reporting, level 5 waste and care variability reduction, level 6 population health management and suggestive analytics, level 7 clinical risk intervention and predictive analytics, level 8 personalized medicine and prescriptive analytics and finally level 9 deals with direct-to-patient analytics & artificial intelligence [Citation27].
7. Business intelligence maturity model (BIMM)
Health care institutions management also involves the use of a business approach. The Business Intelligence Maturity Model (BIMM) is a framework that healthcare organizations can use to assess their business intelligence (B.I.) maturity. The BIMM comprises five maturity levels: 1. Ad hoc: Organizations at this level have no formal B.I. processes or systems. B.I. is used ad hoc, and there is no centralized data repository. 2. Initial: Organizations at this level have implemented some basic B.I. processes and systems, but they still need to be fully integrated. There is still much manual work involved in B.I., and data is not always accessible to decision-makers. 3. Repeatable: Organizations at this level have implemented more mature B.I. processes and systems. B.I. is more integrated, and data is more accessible to decision-makers. However, there is still room for improvement in data quality and analysis capabilities. 4. Managed: Organizations at this level have a well-defined B.I. strategy and processes. B.I. is fully integrated with other business processes, and data quality is high. B.I. is used to support decision-making at all levels of the organization. 5. Optimizing: Organizations at this level constantly seek ways to improve their B.I. capabilities. They are using B.I. to drive innovation and competitive advantage. The five levels of BIMM can be used to assess the healthcare institution's B.I. maturity in various ways. Firstly, identify areas where the healthcare institution can improve its B.I. capabilities – secondly, set goals for improving B.I. maturity. Thirdly, track progress over time and benchmark the healthcare institution's B.I. maturity against other healthcare organizations. [Citation28]. The model is valuable for helping healthcare institutions improve their B.I. capabilities [Citation29].
8. Healthcare usability maturity model (UMM)
The UMM model is a framework that helps healthcare organizations evaluate and improve the usability of their information and technology systems. Five models of maturity levels range from ad hoc – where health care organizations do not have formal usability practices that can be managed – health care organizations have some usability practices, but they are not defined or implemented, standardized – health care organization has a set of standardized usability practices that are regularly applied, quantitatively managed – Healthcare organizations measure and monitor their usability performance, and finally, optimization – as healthcare providers continue to improve usability practices, each stage is characterized by a set of practices and principles [Citation19]. UMM was established by the HIMSS team in 2011. Usability is a vital component of quality healthcare; usability can be improved systematically, and UMM guides on improving usability. Many healthcare organizations use UMM, including hospitals, clinics, and health departments. It is an effective tool for improving IST accessibility and patient care by assessing the level of maturity of their current use, identifying areas for improvement, developing and implementing improvement plans, and monitoring their progress over time [Citation30].
9. Hospital information system maturity model (HiSMM)
HISMM is a new model. Since its development in 2018 by a team of researchers in Portugal, it has gained acceptance in healthcare facilities seeking to improve their HIS and patient care outcomes. The HISMM framework is used to assess the maturity of HIS. This is based on maturity, defined as an organization's ability to improve its processes and procedures continuously. This model is designed to have six stages. Each level is defined by data analysis, strategy, people, systems, and infrastructure attributes. When he detects such attributes, the corresponding level and capabilities it possesses are reached. With measurable changes between levels, hospitals can use this scale to (1) determine the current level of maturity. (2) determine the next level of maturity to be achieved; (3) Identify the characteristics to be followed in order to reach a new level of maturity [Citation30].
10. Nhs infrastructure maturity model (NIMM)
For the NHS to improve its I.T. systems and ensure that they are relevant to the needs of healthcare organizations, the NIMM framework was developed to help the NHS evaluate and improve its I.T. infrastructure. The NHS Infrastructure Maturity Model (NIMM) is divided into 13 categories, 74 opportunities, and five perspectives. The perspectives are (1) Strategy: Aligning I.T. infrastructure with business strategy (2) Deployment: Acquisition, deployment, and maintenance of I.T. infrastructure (3) Operation: Daily operation of I.T. infrastructure (4) Security: Protecting I.T. infrastructure against unauthorized access, use, disclosure, tampering, modification or destruction. (5) Management: governance and control of I.T. infrastructure [Citation30,Citation41]. The NIMM framework is a valuable tool. Some of the benefits of using NIMM include providing a structured approach to assessing and improving information technology infrastructure; it helps identify and prioritize areas for improvement and provides roadmaps for improvement used to benchmark with other healthcare organizations [Citation31,Citation32].
11. Telemedicine service maturity model (TMSMM)
The Telemedicine Service Maturity Model (TMSMM) is a framework for evaluating and improving the maturity of telemedicine services. Researchers developed it from the University of Stellenbosch in South Africa to meet the need for tools to help organizations evaluate and improve the quality of telemedicine services. TMSMM is based on the concept of maturity level to describe the organization's progress in developing and implementing telemedicine services. Maturity Level Model 0–5 Level. Level 0 (Initial): This is where the organization is just beginning to understand the use of drugs. Level 1 Ad hoc: Organizations use telemedicine in limited ways without a clear strategy or plan. Level 2 (managed): The organization has a more structured approach to telemedicine, but there is still room for improvement. Level 3 (Defined): The organization has a well-defined, documented telemedicine service with clear goals and objectives. Level 4 (Quantitatively managed): The organization uses data and metrics to measure and improve the performance of its telemedicine service. Level 5 (Optimization): Organizations constantly seek ways to improve their telemedicine service. TMSMM can be used to assess the maturity of telemedicine service at the micro, meso, and macro levels. Micro-levels focus on individual components of telemedicine services, such as processes, technology, and the people involved. The meso level focuses on interactions between different service components. The macro level focuses on the general context of telemedicine services, such as healthcare systems and regulatory environments [Citation33].
12. Project management maturity model (PMMM)
In order to attain strategic goals, reap operational advantages, and establish business value, healthcare institutions must prioritize project management as a primary approach. With numerous project management maturity models available, the selection process should involve meticulous evaluation to determine the most suitable fit for the healthcare organization [Citation34]. A Project Management Maturity Model (PMMM) serves as a framework to gauge an organization's proficiency in accomplishing projects effectively and progressively enhancing this proficiency [Citation34]. This is achieved by assessing a company's project management procedures, where disorganized and inadequately controlled methods are situated at the lowest level, structured and standardized practices in the middle tier, and consistently refined practices occupy the highest position. Various PMMMs are accessible, each with specific criteria and development stages. Several renowned PMMMs encompass (1) The Organizational Project Management Maturity Model (OPM3) by the Project Management Institute (PMI), (2) The CHAOS Report by The Standish Group, (3) The Project Management Maturity Model (PMMM) by the Project Management Center of Excellence (PMCoE), and (4) The Capability Maturity Model Integration (CMMI) by the Software Engineering Institute (SEI). The advantages of employing a PMMM encompass identifying enhancement opportunities within project management processes, formulating strategies to augment project management maturity, ongoing measurement of advancement, establishing benchmarks against other organizations, and increasing the likelihood of successful project deliveries [Citation34]. When employing a PMMM, the initial phase involves choosing a suitable model for the healthcare institution. Factors such as the size and complexity of the organization, the sector it operates in, and the precise requirements should all be considered during this selection. Following model selection, hospital managers can appraise their organization's present level of maturity and create a strategy for enhancement. Enhancing the project management maturity is a task that may pose challenges, yet it brings forth substantial rewards. Using a PMMM, managers can access the perspectives and resources to accomplish successful project deliveries and advance their organization's effectiveness [Citation35].
13. Informatics capability maturity model (ICMM)
Developed in 2003 by the American Medical Informatics Association (AMIA). The Informatics Capability Maturity Model (ICMM) is a framework for assessing the maturity of an organization's use of informatics in health care based on the Capability Maturity Model Integration (CMMI) framework. The five levels of ICMM maturity are Basic: Health organizations have a basic knowledge of informatics and use it to a limited degree; controlled: H.O. has a more formal approach to informatics and uses it to improve processes and decisions. Standard: H.O. has standardized its informatics practices and used them to achieve consistency and efficiency. Optimized: H.O. continues to improve its informatics practices and use them for innovation and efficiency. Innovative excellence: Organizations use informatics to create new means of health care delivery. ICMM is a valuable tool for organizations that use informatics to improve healthcare [Citation19]. This can help them better understand their current capabilities, identify areas for improvement, and develop plans to achieve their goals.
14. Business process orientation maturity model (BpOMM)
In order to reduce the cost of providing healthcare services, a process must be put in place so that healthcare organizations can save costs by working efficiently. (BPOMM) is one of those models that will be useful for hospital management. The Business Process Orientation Maturity Model (BPOMM) is a framework healthcare organizations can use to assess the maturity of their business process (BPO). BPO is a management approach that optimizes business processes to increase efficiency, effectiveness, and customer satisfaction. BPOMM has five levels of maturity, ranging from the Ad Hoc Stage. The process is informal and ad hoc, with little or no coordination between departments or functions. Define Stage: Processes are documented and standardized, but coordination between departments or functions still needs to be improved. Linked Stage: The process is connected, but the focus on customer satisfaction still needs to be improved. Managed Stage: The process is constantly managed and improved, focusing on customer satisfaction. Integrated Stage: The process is fully integrated and optimized, focusing on continuous improvement and innovation [Citation36]. BPOMM can be used to identify areas where an organization can improve its BPO maturity. By understanding their current level of maturity, organizations can develop plans to move to the next level.
15. Health Industry Insights (IDC): Mobility maturity model (IDC-MMM)
IDC-MMM is a framework that helps healthcare organizations assess their maturity in adopting mobile solutions for their health information system (HIT). There are five stages: Stage 1-Ad hoc: Healthcare organizations are beginning to explore mobile solutions. They may have some mobile devices but need a general strategy or governance. Stage 2-Pilot: Organizations at this stage have begun testing mobile solutions in several areas. They may have limited users, and the solution must fully integrate with the organization's existing systems. Deployment: The healthcare organization has deployed mobile solutions to many users. Solutions are increasingly integrated with an organization's existing systems, but security and management issues may still arise. Optimization: The healthcare organization at this stage has optimized the use of mobile solutions. They have a well-defined strategy and governance, and the solution fully integrates with the organization's existing systems. Transformation: Healthcare organizations at this stage have changed their business processes to use mobile solutions. They use mobile solutions to innovate and improve care delivery [Citation37]. IDC-MMM can assess the organization's current maturity level and identify improvement areas. It can also be used to track the performance of an institution over time.
16. Electronic medical record adoption model (EmRAM)
The Electronic Medical Record Adoption Model (EMRAM) is a maturity model developed by the Healthcare Information and Management Systems Society (HIMSS) to measure the adoption and use of electronic medical record (EMR) features in hospitals. It is an eight-stage model that ranges from stage 0 (least mature) to stage 7 (most mature). The EMRAM model evaluates hospitals on various criteria, including (1) the extent to which EMRs support patient care and (2) the degree of integrating different EMR systems. (3) The use of tools to support clinical treatment decisions. (4) EMR data security and privacy. (5) Ability to share EMR data with other healthcare providers. Hospitals use the EMRAM model to benchmark their progress in EMR implementation and identify areas for improvement. It is also used by payers, regulators, and other stakeholders to assess the overall maturity of the healthcare I.T. industry. Here are the eight stages of the EMRAM model: Stage 0: No EMR. At this stage, the healthcare organization still needs to install all the essential ancillary systems such as laboratory, pharmacy, cardiology, radiology, and other departments. Stage 1: Basic EMR. Stage 2: Computerized Provider Order Entry (CPOE). Stage 3: Clinical Decision Support (CDS). Stage 4: Integration (The Computerized Practitioner Order Entry and Electronic prescribing are within an electronic medicines administration record. Clinical and Information governance are functional and well-defined. Monitoring of Clinical outcomes and patient satisfaction targets are met). Stage 5: Advanced Clinical Applications. Stage 6: Population Health Management. Stage 7: Interoperability (integration of data from multiple external sources. Service users receive notifications and reminders to support self-administered care and use automated tools for measuring patient outcomes. Digital infrastructure tools enable dynamic patient involvement in personal health management and care) [Citation38]. The EMRAM model is valuable for hospitals looking to improve their EMR performance. It provides a roadmap for progress and helps hospitals identify areas to improve.
17. Continuity of care maturity model (CCMM)
When discussing continuing care, we must look at it from two perspectives. Patient perspectives include not interrupting the patient care delivery throughout his or her care journey between the care facility and the caregiver. An industry perspective that aligns health care resources across care settings and is designed to provide the best health care and value for a specific population. The model improves coordination of care over various care settings. It engages three key stakeholder groups, which are Governance (Administrators, e.g. CEO/COO/CFO/CSOs), Clinical (Clinical/Medical Leaders, e.g. CMIO/CNO/CNIOs), and Information Technology (Technology Leaders CIOs). The model leverages seven stages to improve care setting orientation to achieve coordinated patient care, advanced analytics (patient-specific CDS, population health), and patient engagement (EMR access, input, mobile access, personalized alerts). The CCMM model starts from phase 0 (limited to no electronic communication), level 1 (peer-to-peer data exchange), level 2 (patient-centered clinical data using essential system-to-system exchange), level 3 (Normalized patient records using structural interoperability), level 4 (Care coordination based on data using a semantically interoperable patient record), level 5 (Community-wide patients record using information focused on patient engagement), level 6 (Closed loop, care coordination among care team members), level 7 (Knowledge-based participation for a dynamic, multiorganization interconnected healthcare delivery model) [Citation39]. Continuing care is more complicated than implementing information and technology in a single care setting. As mentioned above, many stakeholders must act in concert to ensure an environment that promotes the best care and value.
18. Interoperability maturity model (IMM)
Interoperability enables health information systems and devices to communicate, exchange, and use data efficiently and securely. This is important to improve healthcare delivery and coordination quality, safety, and efficiency. To achieve this, the Interoperability Maturity Model (IMM) framework helps Healthcare organizations assess and improve their interoperability capabilities. There are five levels of IMM: Ad hoc: This is the lowest level of interoperability, with no formal plan or process to ensure the systems can communicate. Repeat: Basic plans for interoperability exist at this level but need to be better documented and executed. Enhanced: This level of interaction is characterized by more formal plans and processes and a focus on ensuring the systems are communicating efficiently. Managed: At this level, interoperability is a core business process, and regular reviews and assessments ensure that it is maintained. Optimized: This is the highest level of interoperability, where systems can communicate and interoperate seamlessly [Citation19]. The IMM can be used to assess the interoperability of any organization, regardless of its size or industry. It can also be used to identify areas where interoperability can be improved.
19. Capability maturity model integration for services (CMMI-SVC)
CMMI-SVC, or the Capability Maturity Model Integration for Services, is a process improvement that helps health organizations improve their service delivery capabilities. It is based on the CMMI framework, a widely used model for process improvement in various industries [Citation19,Citation42]. CMMI-SVC identifies five levels of maturity that organizations can achieve to improve service delivery capabilities. These levels are Initial: The organization has no defined processes for service delivery. Managed: The organization has defined processes for service delivery, but they are not consistently followed. Defined: The organization has defined processes for service delivery that are consistently followed. Quantitatively Managed: The organization collects and analyzes data on its service delivery processes to improve them. Optimizing: The organization continuously improves its service delivery processes. The critical practices in CMMI-SVC are establishing a service strategy, managing customer expectations, providing quality services, managing risks, and continuously improving [Citation40] ().
3.2. Evaluate the benefits and challenges associated with implementing hospital management maturity models
Implementing the identified maturity models for hospital management offers several benefits. While maturity models offer significant benefits, their implementation also presents particular challenges. [] identified the possible benefits and considerable challenges of implementing maturity models for hospital management.
Table 6. Benefits and challenges of a hospital management maturity model.
4. Discussion and recommendations
This literature review identified 19 maturity models that are beneficial to hospital management. Maturity models help organizations assess and improve their performance [Citation1]. They are handy for complex organizations like hospitals, which need to manage a wide range of activities and ensure that they cost-effectively provide high-quality care to patients. The identified maturity models cover various areas, including hospital cooperation, process maturity, patient safety, hospital data quality, and healthcare analytics. Maturity models can be a valuable tool for hospital managers looking to improve their organizations’ performance. By assessing their current maturity level and identifying areas for improvement, hospitals can develop a roadmap for continuous improvement [Citation21]. The Practical Perspective of maturity model for hospital management look into improvement roadmaps. Identified maturity models for hospital management [] offer a structured framework for hospitals to assess their current state, identify improvement areas, and set advancement goals. This roadmap fosters continuous improvement and helps bridge the gap between where a hospital stands and where it aspires to be [Citation21–23]. Benchmarking provide a practical perspective by comparing their score against model benchmarks, hospitals can gauge their performance relative to industry standards [Citation20,Citation25,Citation27]. This provides valuable insights for setting realistic goals and prioritizing improvement efforts. Maturity models for hospital management can guide hospitals in allocating resources efficiently towards areas with the most significant impact on patient care and overall performance [Citation19]. This data-driven approach ensures that resources are well-spent on more impactful initiatives. The models provide evidence-based recommendations for specific improvement actions, helping managers make informed decisions about implementing new technologies, streamlining processes, and optimizing workflows [Citation19,Citation32]. The Managerial Perspective of maturity model for hospital management ensures leadership engagement. The maturity models serve as a tool to garner leadership buy-in for improvement initiatives [Citation22]. The visual representation of progress and the potential benefits can motivate leaders to commit resources and support change efforts. To ensure performance measurement, the models establish clear metrics and evaluation criteria, enabling managers to track progress, measure the effectiveness of interventions, and hold teams accountable for achieving set goals [Citation23]. Communication and collaboration are vital for hospital management, the maturity models facilitate communication across departments and stakeholders by providing a common language for discussing performance and improvement priorities. This fosters collaboration and breaks down silos that impede progress [Citation16]. Change management is important for organizational growth and sustainability, the models support effective change management by outlining a stepwise approach to improvement [Citation34]. Hospitals can implement changes iteratively, minimizing disruption and ensuring smooth adaptation to new processes and technologies. In view of the scientific perspective, the maturity models are grounded in research and validated against industry standards and best practices. This ensures that the models are reliable and provide accurate assessments of hospital performance [Citation22]. The models leverage data collection and analysis to identify patterns and trends in hospital performance [Citation21,Citation23]. This data-driven approach allows for evidence-based decision-making and continuous refinement of the models. Maturity models are valuable tools for researchers studying hospital performance and healthcare delivery systems. The data collected through model assessments can inform further research into factors influencing hospital effectiveness and patient outcomes [Citation19,Citation21,Citation40]. By providing a common framework for assessing hospital performance, maturity models can contribute to the standardization and interoperability of healthcare data across institutions [Citation19]. This facilitates benchmarking, research, and, ultimately, improvements in healthcare delivery across the board. It is important to note that no single maturity model fits every hospital perfectly. The model choice depends on each institution's specific needs, priorities, and context [Citation1,Citation3]. However, by understanding these models’ practical, managerial, and scientific perspectives, hospital leaders can make informed decisions about using them to drive continuous improvement and achieve excellence in patient care [Citation21]. The data collection and analysis results were heterogeneous, limiting our ability to run meta-analyses and draw definitive conclusions [Citation2]. General observations suggest that these models were effective in hospital management, including quality improvement, medical records, hospital information systems, and health project management [Citation20,Citation23,Citation39,Citation40]. Overall, the findings of this study indicate a need for developing a standardized maturity model for hospital management. Maturity models offer a valuable framework for hospital management to assess their current performance, identify areas for improvement, and drive continuous growth [Citation22]. By understanding their key characteristics, applications, and benefits, hospital managers can leverage the power of these identified maturity models to achieve greater effectiveness and success. However, addressing the potential challenges and ensuring that the chosen model is implemented thoughtfully and strategically to maximize its positive impact is crucial [Citation19, Citation22, Citation34]. Hospital managers considering a maturity model should first identify the specific areas of their organization that they want to improve. Once they have identified these areas, they can choose a maturity model relevant to their needs. The next step is to assess the current maturity level of the organization. This can be done through self-assessment, external assessment, or both. Once the current maturity level has been assessed, the hospital can develop a plan to improve its performance [Citation21]. This plan should identify the specific areas that need to be improved and the steps that need to be taken to achieve this. It is important to note that maturity models take time to fix. Implementing a maturity model and achieving lasting improvement takes time and effort. However, the benefits of using a maturity model can be significant, including improved patient care, reduced costs, and increased efficiency [Citation40]. Furthermore, hospital managers can use maturity models to improve their HCOs’ performance and provide better patient care by involving all stakeholders in the maturity model implementation process. This includes staff, clinicians, patients, and other stakeholders, and monitor progress and adjust the plan as needed.
5. Limitation of the study
Limited research on the potential drawbacks and unintended consequences of using maturity models.
There is a lack of robust empirical evidence on the impact of maturity models on hospital outcomes and performance.
6. Further research
This research paper provides a foundational understanding of maturity models for hospital management. Further research can be done to understand better specific models and their applications within different healthcare domains. Additionally, exploring the theoretical underpinnings of maturity models and their effectiveness in driving healthcare quality improvement can offer valuable insights for medical practitioners and researchers.
English Language Report .pdf
Download PDF (1.1 MB)Authors Response to Reviewers Feedback.docx
Download MS Word (14.1 KB)Acknowledgments
The authors thank the editors and anonymous reviewers for their insightful comments and suggestions.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Erhauyi Meshach Aiwerioghene
Dr. Erhauyi Meshach Aiwerioghene is a senior lecturer in Healthcare Management at Swansea University. He has experience in teaching and researching healthcare management, health information management, and human physiology across universities on three continents. His work is published in respected academic journals and presented at international conferences.
Janice Lewis
Dr. Janice Lewis is a public health professional with extensive experience in NHS and academia. Her doctoral research explored the influence of health visitors on policy using feminist frameworks.
David Rea
Dr. David Rea is an associate professor with expertise in healthcare management. Has taught internationally and supervised numerous graduate students. His research works focus on power dynamics in healthcare and promoting patient involvement. They excel in qualitative research methods.
References
- Cimini C, Lagorio A, Cavalieri S. Development and application of a maturity model for industrial agile working. Comput Ind Eng. 2024;188:109877. doi:10.1016/j.cie.2023.109877
- Shaygan A, Daim T. Technology management maturity assessment model in healthcare research centers. Technovation. 2023;120:102444. doi:10.1016/j.technovation.2021.102444
- Chong J, Jason T, Jones M, et al. A model to measure self-assessed proficiency in electronic medical records: validation using maturity survey data from Canadian community-based physicians. Int J Med Inf. 2020;141:104218. doi:10.1016/j.ijmedinf.2020.104218
- Liu Y, Evans L, Kwan T, et al. Developing a maturity model for cancer multidisciplinary teams. Int J Med Inf. 2021;156:104610. doi:10.1016/j.ijmedinf.2021.104610
- Mishra VT, Sharma MG. Digital transformation evaluation of telehealth using convergence, maturity, and adoption. Health Policy Technol. 2022;11(4):100684. doi:10.1016/j.hlpt.2022.100684
- Forliano C, Bullini Orlandi L, Zardini A, et al. Technological orientation and organizational resilience to COVID-19: the mediating role of strategy's digital maturity. Technol Forecast Soc Change. 2023;188:122288. doi:10.1016/j.techfore.2022.122288
- Ogueji IA, Motajo OO, Orjingene O, et al. "Allowing the community, that is the essential beneficiaries, to take the lead": Using the perspectives of health workers to inform a contextually relevant quality improvement intervention in the Nigerian health system. Curr Psychol. 2023;43(15):13679–13691. doi:10.1007/s12144-023-05359-6
- Caiado RGG, Scavarda LF, Gavião LO, et al. A fuzzy rule-based industry 4.0 maturity model for operations and supply chain management. Int J Prod Econ. 2021;231:107883. doi:10.1016/j.ijpe.2020.107883
- Liu CF, Hwang HG, Chang HC. E-healthcare maturity in Taiwan. Telemed e-Health. 2011;17(7):569–573. doi:10.1089/tmj.2010.0228
- Ifenthaler D, Egloffstein M. Development and implementation of a maturity model of digital transformation. TechTrends. 2020;64(3):302–309. doi:10.1007/s11528-019-00457-4
- Doctor E, Eymann T, Fürstenau D, et al. A maturity model for assessing the digitalization of public health agencies. Bus Inf Sys Eng. 2023;65(5):539–554. doi:10.1007/s12599-023-00813-y
- Menukin O, Mandungu C, Shahgholian A, et al. Guiding the integration of analytics in business operations through a maturity framework. Ann Oper Res. 2023: 1–22. doi:10.1007/s10479-023-05614-w
- Peña A, Bonet I, Lochmuller C, et al. A fuzzy ELECTRE structure methodology to assess big data maturity in healthcare SMEs. Soft comput. 2019;23(12):10537–10550. doi:10.1007/s00500-018-3625-8
- Alshammari FH. Design of capability maturity model integration with cybersecurity risk severity complex prediction using Bayesian-based machine learning models. Serv Oriented Comput Appl. 2023;17(1):59–72. doi:10.1007/s11761-022-00354-4
- Sullivan JL, Rivard PE, Shin MH, et al. Applying the high-reliability health care maturity model to assess hospital performance: a VA case study. Jt Comm J Qual Patient Saf. 2007;33(10):495–504. doi:10.1016/s1553-7250(16)42080-5
- Senna PP, Barros AC, Bonnin Roca J, et al. Development of a digital maturity model for Industry 4.0 based on the technology-organization-environment framework. Comput Ind Eng. 2023;185;109645. https://doi.org/10.1016/j.cie.2023.109645.
- Tranfield D, Denyer D, Smart P. Towards a methodology for developing evidence-informed management knowledge by means of systematic review. Br J Manage. 2003;14(3):207–222. doi:10.1111/1467-8551.00375
- Critical Appraisal Skills Programme. CASP (systematic Review) Checklist. https://casp-uk.net/casp-tools-checklists/. [Cited 2024 January 16]. 2018.
- Gomes J, Romão M. Information system maturity models in healthcare. J Med Syst. 2018;42(12):1–14. doi:10.1007/s10916-018-1097-0
- Mettler T, Blondiau A. HCMM is a maturity model for measuring and assessing the quality of cooperation between and within hospitals. 2012. doi:10.1109/CBMS.2012.6266397
- Mallek-Daclin S, Daclin N, Dusserre G, et al. Maturity model-driven assessment of Field Hospitals. IFAC-PapersOnLine. 2017;50(1):4642–4647. doi:10.1016/j.ifacol.2017.08.685
- Chassin MR, Loeb JM. High-reliability health care: getting there from here. Milbank Quarterly. 2013;91(3):459–490. doi:10.1111/1468-0009.12023
- Sullivan JL, Rivard PE, Shin MH, et al. Applying the high-reliability health care maturity model to assess hospital performance: a V.A. case study. Jt Comm J Qual Patient Saf. 2016;42(9):389–399. doi:10.1016/s1553-7250(16)42080-5
- de Carvalho JV, Rocha Á, Vasconcelos J. Towards an encompassing maturity model for the management of hospital information systems. J Med Syst. 2015;39(9):99. doi:10.1007/s10916-015-0288-1
- Carvalho VJ, Rocha Á, Abreu A. Maturity of hospital information systems: most important influencing factors. Health Informatics J. 2019;25(3):617–631. doi:10.1177/1460458217720054
- Wang Y, Kung L, Byrd T. Big data analytics: understanding its capabilities and potential benefits for healthcare organizations. Technol Forecast Soc Change. 2018;126:3–13. doi:10.1016/j.techfore.2015.12.019
- Muhunzi D, Kitambala L, Mashauri H. Big data analytics in the healthcare sector: opportunities and challenges in developing countries. A literature review. 2023. doi:10.21203/rs.3.rs-2869049/v1
- Gastaldi L, Pietrosi A, Lessanibahri S, et al. Measuring the maturity of business intelligence in healthcare: supporting the development of a roadmap toward precision medicine within ISMETT hospital. Technol Forecast Soc Change. 2018;128:84–103. ISSN 0040-1625. doi:10.1016/j.techfore.2017.10.023
- Thamir A, Theodoulidis B. Business intelligence maturity models: Information management perspective. 2013. doi:10.1007/978-3-642-41947-8_18
- Carvalho JV, Rocha A, Vasconcelos J, et al. A health data analytics maturity model for hospitals information systems. Int J Inf Manage. 2019;46:278–285. ISSN 0268-4012. doi:10.1016/j.ijinfomgt.2018.07.001
- Van Dyk L, Schutte C, Fortuin J. A maturity model for telemedicine implementation. Vol. 10. 2012. p. 56116. doi:10.1108/BPMJ-08-2019-0342
- Abreu A. Maturity models of healthcare information systems and technologies: a literature review. J Med Syst. 2016;40(6):1–10. doi:10.1007/s10916-016-0486-5
- Van Dyk L, Schutte CSL. The telemedicine service maturity model: a framework for the measurement and improvement of telemedicine services. InTech; 2013. doi:10.5772/56116
- Domingues L, Ribeiro P. Project management maturity models: proposal of a framework for models comparison. Procedia Comput Sci. 2023;219:2011–2018. ISSN 1877-0509. doi:10.1016/j.procs.2023.01.502
- Fabbro E, Tonchia S. Project management maturity models: Literature review and new developments. J Mod Proj Manag. 2021;8(3). doi:10.19255/JMPM02503
- Dewi F, Mahendrawathi ER. Business process maturity level of MSMEs in East Java, Indonesia. Procedia Comput Sci. 2019;161:1098–1105. doi:10.1016/j.procs.2019.11.221
- Ma Y, Sun C, Liang L. Maturity Model of Hospital Information System Based on AHP and TOPSIS. In 2022 International Conference on Computer Technologies (ICCTech). Melaka, Malaysia: Institute of Electrical and Electronics Engineers; 2022. p. 33-37. doi:10.1109/ICCTech55650.2022.00014
- Najjar A, Amro B, Macedo M. The adoption level of electronic medical records in Hebron hospitals based on the electronic medical record adoption model (EMRAM). Health Policy Technol. 2021;10(4):100578. ISSN 2211-8837. doi:10.1016/j.hlpt.2021.100578
- Woods L, Dendere R, Eden R, et al. Perceived impact of digital health maturity on patient experience, population health, health care costs, and provider experience: mixed methods case study. J Med Internet Res. 2023;25:e45868. PMID: 37463008; PMCID: PMC10394505. doi:10.2196/45868
- Collanus E, Kielo-Viljamaa E, Lahtiranta J, et al. We are measuring the Maturity of Healthcare Testbeds. In International Conference on Well-Being in the Information Society. Cham: Springer International Publishing; 2022. p. 179–191. doi:10.1007/978-3-031-14832-3_12
- Miloslavskaya N, Tolstaya S. Information security management maturity models. Procedia Comput Sci. 2022;213:49–57. doi:10.1016/j.procs.2022.11.037
- Cerdeiral CT, Santos G. Software project management in high maturity: a systematic literature mapping. J Syst Softw. 2019;148:56–87. doi:10.1016/j.jss.2018.10.002