?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background: Conscientious objection (CO) in healthcare is a controversial topic. Some perceive CO as freedom of conscience, others believe their professional duty-of-care overrides personal-perspectives. There is a paucity of literature pertaining to pharmacists’ perspectives on CO.
Aim: To explore Australian pharmacists’ decision-making in complex scenarios around CO and reasons for their choices.
Method: A cross-sectional, qualitative questionnaire of pharmacists’ perspectives on CO. Vignette-based questions were about scenarios related to medical termination, emergency contraception, IVF surrogacy for a same-sex couple and Voluntary Assisted Dying (VAD)
Results: Approximately half of participants (n = 223) believed pharmacists have the right to CO and most agreed to supply prescriptions across all vignettes. However, those who chose not to supply (n = 20.9%), believed it justifiable, even at the risk of patients failing to access treatment. Strong self-reported religiosity had a statistically significant relationship with decisions not to supply for 3 of 4 vignettes. Three emergent themes included: ethical considerations, the role of the pharmacist and training and guidance.
Conclusion: This exploratory study revealed perspectives of Australian pharmacists about a lack of guidance around CO in pharmacy. Findings highlighted the need for future research to investigate and develop further training and professional frameworks articulating steps to guide pharmacists around CO.
Background
Conscientious objection (CO) is a controversial topic in healthcare. In Australia CO is accommodated across various healthcare laws (New South Wales Parliament Legislative Council Standing Committee on Law and Justice Report no 79 Citation2021), with general statements indicating healthcare professionals have the right to conscientiously object. However, there are no clear instructions regarding how to manage such cases and no specificity towards any healthcare profession, including pharmacy. CO is described as, ‘a practitioner’s refusal to provide a service primarily because the action would violate their moral or ethical values' (Pharmaceutical Society of Australia, Citation2017). Some perceive CO as a freedom of conscience (Smith, Citation2006). Others deem it ‘a burden … that patients should not have to shoulder' (Cantor, Citation2009). In modern medicine CO is relevant to many situations, e.g. termination of pregnancy, contraception (Blaschke et al., Citation2019; Fujioka et al., Citation2018) and voluntary-assisted-dying (VAD) (Lawrence & Curlin, Citation2009).
From a patient perspective, CO by a healthcare professional can have far-reaching implications that may impact access to treatment. Justice and autonomy are central tenants of healthcare ethics (Beauchamp & Childress, Citation2019). Patients may feel these principles compromised when their provider objects. Existing literature primarily focuses on investigating CO held by physicians, nurses and midwives, more than pharmacists. For physicians this encompasses all disciplines, depending on specialities – e.g. abortion and contraception in women’s health, hormone replacement therapy for gender identity and VAD, to name a few. For example, a 2011 study of 1032 US physicians, found doctors divided about CO, with almost half disagreeing with referring, deeming referral itself as immoral (Combs et al., Citation2011). Another 2009 national survey of 1000 US primary-care physicians, concluded that doctors believed respecting ‘patient autonomy’ did not guide their decision-making (Lawrence, Citation2009). In Australia, a 2019 qualitative study identified that most doctors would not allow their moral/religious beliefs to impact patientcare (Keogh et al., Citation2019).
Implications of CO for nurses primarily involve abortions and women’s reproductive health, and it has been identified that nurses need additional support to address these issues (Lamb et al., Citation2019). Dobrowolska et al. (Citation2020) compared literature from Poland and the UK, concluding that regulation for nurses in the UK is limited to reproductive health, while in Poland, there are no specific procedures to which nurses can apply an objection (Dobrowolska et al., Citation2020). Even medical students’ views have been investigated across multiple studies (Card, Citation2012; Darzé & Barroso-Júnior, Citation2018; Hagen et al., Citation2011; Nordstrand et al., Citation2014; Strickland, Citation2012).
As medicine experts and gatekeepers of medicines, the implications of CO for pharmacists are across many scenarios, such as VAD in hospital pharmacy, contraception access in community pharmacies, medical abortion, hormone therapy or any service that requires a medication as part of treatment.
In Australia, legislation fails to define or detail what CO is and what should be done if a healthcare professional chooses to CO, especially for pharmacists. This ethical landscape has been left to professional organisation bodies to develop broad professional standards in an attempt to address complex ethical issues around CO. For example, the Pharmaceutical Society of Australia (PSA) has a set code of ethics in which they define CO and stipulate that a conscientious objector should ‘appropriately facilitate continuity of care for the patient’. However it is important to mention that this has not been updated since 2017 (Pharmaceutical Society of Australia, Citation2017). Additionally, the Australian Health Practitioner Regulation Agency (AHPRA) developed a shared code of conduct publication in 2022 (Australian Health Practitioner Regulation Agency (AHPRA) & National Boards, Citation2022) – applicable to 12 different allied healthcare professionals including pharmacists but excluded doctors, nurses and midwives. This publication shares the PSA’s same clause regarding CO and the need to ensure continuity of care, however falls short of clarifying what actions are required to achieve this. The only exception at current, is service specific examples. The most recent being the new VAD laws which have legislated clauses acknowledging and respecting the rights of all parties involved to conscientiously object.
The Act allows for registered health practitioners who have a CO to VAD to refuse to be involved in key parts of this process, including prescribing, supplying, administering, or being present for administration of a VAD substance. However those who conscientiously object to VAD cannot prevent or interfere with VAD access or associated processes that are being completed by other staff and are expected to provide the usual standard of care to their patients. (Callaghan & Vella, Citation2023)
Aim
This study aimed to explore Australian pharmacists’ decision-making in complex scenarios around CO and reasons for their choices.
Ethics approval
This study was approved by the University of Sydney Human Research Ethics Committee [Ref No. 2019/658] between October 2019 and March 2020.
Methods (See flowchart – supplement C)
Study design
A cross sectional, qualitative questionnaire for registered pharmacists in Australia was distributed between January and March 2020. The questionnaire was developed by the research team based on scenarios identified from previous research, and the general literature (Davidson et al., Citation2010; Hanlon et al., Citation2000; Isaac et al., Citation2019; Piecuch et al., Citation2014). Prior to piloting the questionnaire, five experts (with the inclusion criteria of having experience and academic expertise in bioethics, healthcare research and healthcare practice; and the exclusion of not having met inclusion criteria) helped establish face and content validity. They were asked to review whether the proposed questions in the questionnaire would adequately capture a pharmacist’s decision-making around CO, and whether the questions purportedly measured the intended diversity in responses.
A draft of the questionnaire was then piloted in 2019 with 62 pharmacists at an international conference (International Pharmaceutical Federation (FIP) Citation2019) for readability, content and platform useability (Isaac et al., Citation2023). Minor changes were made to response options, display of the questionnaire and typographical errors in response to both experts’ validation and the pilot feedback.
Final questionnaire
The full, online questionnaire (Supplement B) consisted of 20 questions divided into three sections: demographics (Q1-Q7), personal perspectives (Q8-Q13, Q18-Q20) and vignettes (Q14-Q17). The questionnaire instrument consisted of mixed formats, including multiple-choice, dichotomous responses, Likert scale-type questions, and open-ended, free text response sections.
The four key hypothetical vignettes portrayed challenging or ethically controversial issues in pharmacy practice relevant to the Australian context, which may evoke CO. The vignette topics incorporated the dispensing of the following medicines:
MS-2 Step® medical abortifacient (mifepristone + misoprostol)
Emergency contraception pill (ECP) – for a consenting 15-year-old female
Clomifene (IVF-therapy) for a surrogate, for a same-sex couple.
Pentobarbital for VAD (Voluntary Assisted Dying) – to the wife of a 75-year-old man with terminal pancreatic cancer.
Respondents were required to select either ‘Supply', ‘Conditional supply', or ‘Do not supply’. They were also asked to provide additional reasoning for their selection in a free-text response section, before progressing through the questionnaire. Mandatory response was enabled for all questions. The questionnaire programme prompted participants to complete mandatory questions prior to submitting that page. Participants could choose to go back through questions and change responses prior to submitting the final questionnaire. All responses were anonymous.
Analysis
Each question required an answer to progress to the next, therefore partially completed questionnaires could not be submitted, and hence not included for analysis. The analysis incorporated a mixed methods approach, as illustrated in flowchart (Supplement C). A convergent parallel (Creswell & Clark, Citation2017), mixed methods research design was utilised to collect quantitative and qualitative data simultaneously and analysed them separately to allow for the collection of numerical and non-numerical data that were mutually exclusive however still helped inform one another.
As part of the exploratory process and delving into the respondents’ reasoning, the open-ended responses were exported from Survey Planet to Excel for data organisation, then uploaded to NVivo (QSR,12.6.0-3841,2019) software for thematic coding by SI. For quality control, the research team (SI, BC and AJM) independently read, coded and reviewed respondents’ comments into emergent themes.
Thematic analysis was conducted for each vignette separately to identify trends and triangulate themes across the various responses (Green & Thorogood, Citation2018; Yin, Citation2015). These themes were then discussed and reviewed until consensus was achieved on the coding scheme for the thematic analysis. Data saturation was reached after the analysis of 135 responses; however, all responses were analysed to assure there was no new information or themes. The analytical technique of ‘constant comparison’ (a component of grounded theory; Glaser & Straus, Citation1967) was adopted to extract and code key themes.
For the quantitative data, statistical analyses were conducted using the statistical software R (Version3.6.0), with a series of bivariant and Chi-square analyses to compare responses to each vignette by participants from different demographics.
Methodological triangulation, specifically ‘data merging’ was utilised to integrate the reporting of both quantitative data with the incorporation of identified themes to support or refute the quantitative results (Alele & Malau-Aduli, Citation2023). Data analysis followed the Checklist for Reporting of Survey Studies (CROSS) and Standards for Reporting Qualitative Research (SRQR) checklists (O'Brien et al., Citation2014; Sharma et al., Citation2021).
Recruitment
Participants were recruited via snowball sampling, by circulation of an online invitation, linked to the electronic questionnaire via professional organisations’ websites (Pharmaceutical Society of Australia and Pharmacy Guild), social media platforms (LinkedIn©, Facebook©, Twitter©), and through sharing of emails in professional networks. The questionnaire was available online from January 2020 to March 2020 (coinciding with the COVID pandemic). The only inclusion criterion was that participants were registered pharmacists with the Australian Health Practitioner Regulation Agency (AHPRA). The questionnaire was distributed through the web-based application, Survey Planet© (https://surveyplanet.com/). This contactless method was in keeping with the COVID-19 pandemic restrictions in Australia at the time. Consent was implied by the voluntary submission of responses to the anonymous questionnaire, as stipulated in the Participant Information Statement (Supplement A).
Sample size
The sample calculated was based on the number of registered pharmacists in Australia in 2020 (n = 32,777) (Pharmacy Board of Australia AHPRA, Citation2020), with a 95% CI, an accepted margin of error of 7%, and the response distribution of 50%; generating a recommended sample size of 195 using an online sample size calculator (Maple Tech International LLC, Citation2023). This was in keeping with sizes of similar questionnaires of healthcare professionals in the literature and resourcing constraints related to the COVID-19 pandemic (Bawa et al., Citation2022; Benson et al., Citation2020; Karanges et al., Citation2018; Lakens, Citation2022). Calculator.net ™ was the online sample size calculator utilised to calculate the study sample size (Maple Tech International LLC, Citation2023). It required a projected confidence level, population size, proportion and margin of error which together allowed the automatic calculation of the target sample size. The mathematical algorithm used in this calculation is shown below (Maple Tech International LLC, Citation2023).
where: z is the z score ϵ is the margin of error N is the population size p^ is the population proportion
Results
Section 1: participant demographics
The questionnaire was completed by 223 eligible respondents (greater than the calculated sample size). As abovementioned, there were no incomplete responses. Respondents’ demographics were summarised in . The majority were female (69%, 155/223), with a range of practice experience between 1 and 49 years [M = 10.3, SD = 11.1], in various primary roles. Most (40%) respondents were from New South Wales. This closely emulated the overall demographic profile of Australia’s pharmacist workforce, that is, a predominately female (63.1%) and younger workforce (38.3% aged 25–34 years) (Pharmacy Board of Australia AHPRA, Citation2020).
Table 1. Demographic of participating registered pharmacists (n = 223).
Section 2: general personal perspectives
Findings indicated that almost half of respondents (n = 106, 48%) believed that pharmacists have the right to CO (). Some (8%) identified that personal religious belief ‘very much' shaped their decision-making in practice (i.e. religiosity), while the majority chose the ‘not at all' option (). This was also reflected in the responses to the vignettes.
Table 2. Response rates to remaining questionnaire questions related to personal perspectives (non-vignette questions).
presents a series of Chi-square analyses assessing correlations between demographics, religious influence on practice (i.e. religiosity) and participants’ responses across all four vignettes (). Chi-square analyses indicated self-reported religiosity was described as ‘very much’, and had a statistically significant relationship with pharmacists’ decision-making, whether that be to supply or not. This was demonstrated for Case-1: medical abortifacient (p < 0.001), Case-3: IVF for a same-sex couple (p < 0.001), and Case-4: VAD (p < 0.001).
Table 3. Chi Square analysis of demographics vs responses for each Vignette Case, using results from tables 4–7.
Table 4. Response groups vs characteristics for Case 1.
Table 5. Response groups vs characteristics for Case 2.
Table 6. Response groups vs characteristics for Case 3.
Table 7. Response groups vs characteristics for Case 4.
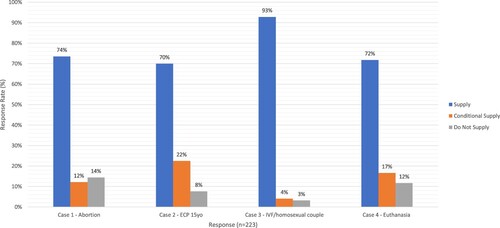
On average, approximately 77% of participants agreed to supply the relevant medicine across the four vignettes proposed (). The remainder 23% withheld access, with or without providing continuity of care.
Some respondents expressed strong disagreement with pharmacists choosing CO:
Religious zealotry has no place in healthcare! (Ph29)
shows 64% participants believed it is not ethically justifiable to enact CO if a patient is unable to access treatment. However, 9% of participants disagreed, irrespective of inconvenience, compromise of safety, or possible harm. The remaining 27% selected the conditional option of ‘only if', emphasising continuity of care in their free-text responses.
Only if the patient is directed to a location where the treatment is available (Ph25)
If you have moral values which impact your practice, then you shouldn’t put yourself in a position of exclusivity e.g. a pharmacist who objects to abortion should not work in an abortion clinic … (Ph79)
Our first role is to do no harm, and that is also to ourselves … . (Ph140)
As a rural pharmacist, I have real issues if people conscientiously object. (Ph68)
Continuity of care is for improving health outcomes, not for terminating human lives (Ph127)
Patients should take their own responsibility into their own hands … (Ph127)
Pharmacists should be held to a reasonable standard. Inconvenience to the patient should not be that standard (Ph74)
Section 3: vignettes
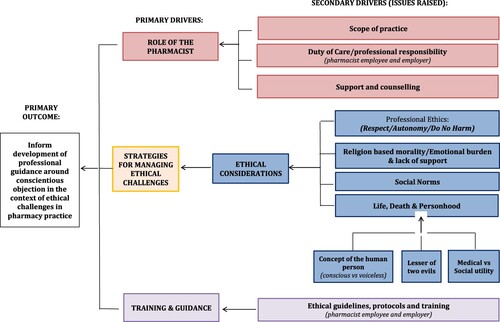
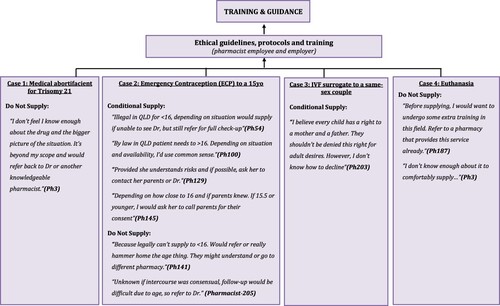
Thematic analysis of the qualitative data collected from these vignettes yielded three major themes:
The Role of the Pharmacist
Ethical Considerations
Training/Guidance
These emergent themes formulated the primary drivers, which were extrapolated into a driver diagram. () The primary drivers were triangulated from secondary drivers from the thematic analysis of open-ended responses to each vignette. To clarify this process, we present results of each case before categorising into primary and secondary drivers.
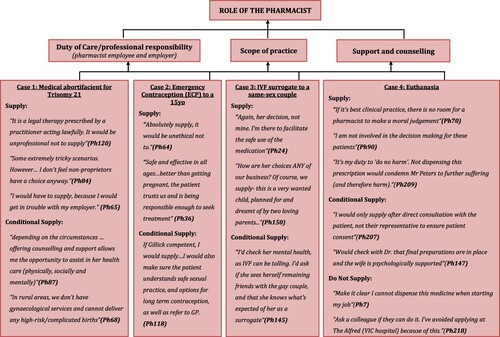
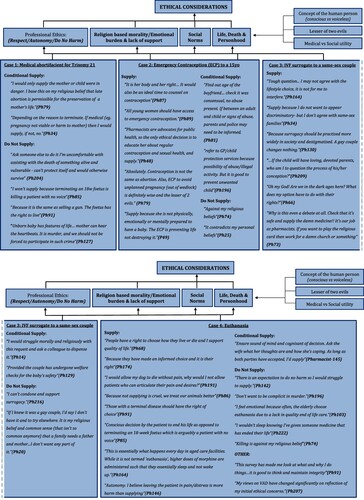
provide the evidence in quotes for each driver in .
Case 1 – medical abortifacient
Supply:
For Case-1, 74% opted to supply ()
It is a legal therapy, prescribed by a practitioner acting lawfully. It’d be unprofessional not to supply (Ph120)
I’m sure pharmacy-owners would object if you refused a sale based on CO. Non-proprietors don’t have a choice. (Ph84)
Some (12%) were concerned about safety and patient support around termination, therefore, would only provide conditional supply. These concerns underpinned the secondary driver of ‘patient support” in the driver scheme.
My hesitation would be that in the rural area, we don’t have services to deliver high-risk/complicated births (Ph68)
I would only supply the medication if there was a clinical danger to the mother or child. (Ph79)
For Case 1, 14% chose not to supply. Religiosity was not the only reason for their response. Some indicated their objection was based on the concept ‘do no harm’. This was the foundation of the secondary driver: ‘professional ethics (respect/autonomy/do no harm)' as well as the sub-driver of ‘concept of the human person'.
I won’t supply because terminating an 18w foetus is arguably killing a patient with no voice (Ph85)
I don’t feel I know enough about the drug and the bigger picture of the situation. It’s almost beyond my scope (Ph3)
Case 2 – emergency contraception (ECP)
Supply:
ECP has been available for legal supply since 1999 (Munro et al., Citation2015), yet still posed some ethical challenges for some. Most participants chose to supply. They highlighted the importance of respect for autonomy in women’s health, which was coded in the secondary driver of ‘Professional Ethics (Respect/Autonomy/Do no harm)'.
It is her body and her right to make an informed decision. It’d also be an ideal time to counsel on contraception (Ph87)
Absolutely supply, it would be unethical not to. (Ph64)
I do not see the morning-after pill as destroying life, it’s preventing life. (Ph49)
Despite being a regular ‘Pharmacist Only’ product, the ECP had the highest level of conditional supply (22%). Most had safety concerns for the patient who was a minor. This was primarily based on the legal age of consent (Australian Government Institute of Family Studies, updated June Citation2017). This underpinned the secondary driver of ‘Professional Ethics (Respect/Autonomy/do no harm)' and ‘support and counselling’.
Check first for consent and no abuse present. If between an adult and child, or signs of abuse, parents and police need to be informed. (Ph196)
By law, a patient needs to be 16 for supply. But depending on situation and availability, common sense prevails. (Ph100)
… follow-up would be difficult due to her age. So, refer. (Ph129)
A minority chose not to supply ECP, indicating it violated their religious beliefs. This further supported the secondary driver of ‘religion-based morality/emotional burden and lack of support' and ‘Professional Ethics: (Respect/Autonomy/Do No Harm)'.
Against my religious beliefs (Ph74)
It’s unknown whether the intercourse was consensual or not. (Ph205)
Case3 – IVF
Supply:
Most pharmacists felt this was the least ethically concerning case, citing the autonomy of the surrogate woman and the same-sex couple’s rights. This was coded to secondary drivers of ‘Professional Ethics: (Respect/Autonomy/Do No Harm)' and ‘scope of practice’.
Again, her decision, not mine. I’m there to facilitate the safe use of the medication (Ph24)
While I may not agree with the lifestyle choice, it is not for me to interfere. (Ph164)
Society now recognises families of all shapes and sizes. Who am I to question the process of his/her conception? (Ph209)
Not many participants had conditions to supply of Clomifene. The main condition stemmed from religion, which would lead to a referral for access. This shaped the secondary-driver of ‘religion-based morality/emotional burden and lack of support'.
I would struggle morally and religiously with this request. I might ask a colleague to dispense the medications. (Ph14)
Provided the couple has had welfare checks to ensure the baby will be raised in a healthy environment (Ph129)
Do Not Supply:
Few participants had any strong objections for which they would deny supply (3%). Only one held a moral objection to the notion of surrogacy.
I can't condone and support surrogacy. (Ph216)
It is my religious belief … that a family needs a father and mother. If they wish to differ, they can go elsewhere, I don't want any part of it. (Ph20)
Case 4 – voluntary assisted dying (VAD)
Supply:
Majority of participants reported they favoured dispensing a prescription for VAD for stage 4 pancreatic cancer. The primary reason for supply was respect for patient autonomy, which encompasses the secondary driver of ‘Professional Ethics: (Respect/Autonomy/Do No Harm)'.
Because they have made an informed choice, and it is their legal right (Ph174)
Not supplying is cruel. We treat our animals better than our brothers and sisters (Ph86)
I believe those with a terminal disease should have the right of choice (Ph91)
As a pharmacist, it is my duty to ‘do no harm’. Not dispensing this prescription would condemn Mr Peters to further suffering (and therefore harm). (Ph209)
If it’s best clinical practice, there is no room for a pharmacist to make a moral judgement (Ph70)
Conditional Supply:
Those who chose to provide conditional supply (17%), did so to preserve patient autonomy and ascertain their intentions, highlighting the recurrent secondary driver of ‘Professional Ethics: (Respect/Autonomy/Do No Harm)'.
I would only supply after direct consultation with the patient, not their representative, otherwise you cannot ascertain patient consent (Ph207)
I’d ensure he’s still sound of mind and cognisant of his decision. I’d ask the wife what her thoughts are and how she’s dealing with it (Ph145)
Do Not Supply:
The second-largest proportion (12%) of ‘do not supply’ responses was in this scenario. Reasons not to supply were consistent with existing literature (Isaac et al., Citation2019), and encompassed the secondary-drivers of ‘Professional Ethics: (Respect/Autonomy/Do No Harm)' and “Religion based morality/Emotional burden and lack of support'.
There is an expectation to do no harm, so I would struggle to supply something that does harm. (Ph142)
I won’t be able to sleep knowing I’ve given someone a medicine that has ended their life (Ph222)
Against my religious belief, killing a person (Ph74)
Make it clear I cannot dispense this medicine when starting my job (Ph7)
I don't know enough about it to comfortably supply … (Ph3)
This questionnaire has made me look at what and why I do what I do … it is good to maintain integrity (Ph91)
My views on VAD have changed significantly on reflection of my initial ethical concerns. (Ph207)
Discussion
Statement of principal findings and comparison to existing literature
This exploratory study identified that most pharmacist participants, when presented with controversial and ethically challenging clinical situations, would supply medicines, or do so irrespective of their personal beliefs. However, findings also indicated that there remained significant minorities who reported they would conscientiously object in several contexts, at times regardless of implications to patients. Principal findings of this study were three primary-drivers () that shed light on the salient concerns of participating pharmacists around CO. These drivers were: the need to clarify the role of the pharmacists, consider the ethical challenges they may face, and provide clear guidelines on how CO can be managed safely.
DRIVER 1: the role of the pharmacist
An interesting perspective expressed by some, was regarding the relationship between employer and employee pharmacists, and the issue of practicing with professional autonomy (Blanks Hindman, Citation1999). This was also mirrored in a 2020 study, which identified the difference in agency between junior doctors and their senior counterparts, where there may be a compromise in moral integrity by participating/accepting, or compromise career-trajectory by objecting (McDougall et al., Citation2022). Having clear professional protocols/guidelines to follow would enable CO to be enacted safely, without discrimination to the objector.
There is also a professional responsibility/accountability for patient care. There is an innate power imbalance associated with being a healthcare professional, who has an expert level of health literacy and education. According to Shanawani H, the challenge of CO amongst healthcare professionals is the ‘ monopoly of knowledge, skills, and resources' (Shanawani, Citation2016) that may impact patient care. The most reasonable solution could be by providing an extension of the conscience clause with a step-by-step protocol, which according to Hanlon et al. would allow for ‘the efficient provision of the pharmaceutical service, whilst at the same time respecting the personal beliefs of those who object' (Hanlon et al., Citation2000).
Driver 2: ethical considerations
For some, the vignettes/cases generated a multitude of difficult ethical dilemmas between principles of ‘respect for patient autonomy’, ‘beneficence’, ‘justice' and ‘do no harm’. These dilemmas would possibly be best resolved with clear guidelines and standards of practice.
Non-denominational religiosity was a key ethical challenge that had a significant influence on participants’ decision-making against supply of the abortifacient, Clomiphene and VAD, as indicated in the findings. This is similar to existing literature (Davidson et al., Citation2010), indicating certain religious affiliations significantly predicted pharmacists’ willingness to dispense medicines that evoke CO. This study, however, was more robust with more focus on the influence of religiosity on professional practice rather than identifying the views of individuals from specific religious denominations. This point highlighted the need to manage the general impact of religiosity on professional reasoning and potentially on patient care.
Religion-based reasoning was also influenced by the degree of harm perceived to be associated with dispensing CO-evoking medicines. Findings indicated a greater proportion of refusal-to-supply was for the abortifacient and VAD, both of which were deemed too consequential, resulting in the death of a human entity. These findings shaped the secondary drivers: life and death, human personhood, the lesser of two evils and medical versus social utility. Ethically and medico-legally, the definition of when the human person begins to exist is not without contention, with varying termination laws between countries and states. In Australia, abortions are legal; however, each state and territory has set different thresholds for termination, with a maximum of 24 weeks gestation or, in some circumstances, more if approved by two physicians (Willis, Citation2019). For many participants who chose not to supply, abortion remained a topic of great contention and moral discomfort. These issues highlighted that despite the conundrum of life and death that will always baffle human beings, they also indicated the need for professional guidance/protocol relating to duties of healthcare providers towards patient care and safety in the case of CO.
Interestingly, findings indicated greater objection to supplying the abortifacient (Case 1) than for the euthanistic (Case 4). Some pharmacists changed their CO between the two cases, with the reasoning that euthanasia is a conscious decision by an adult patient – as opposed to terminating an 18-week foetus, considered a person with no voice. Intriguingly the same participants who objected to the cases of life and death were not as objecting in other scenarios, which may be attributed to the power of social norms and relativity. For example, the acceptance from most participants for IVF surrogacy for a same-sex couple was at least in part influenced by a shift in social norms. This same social acceptance and shift in societal norms may also gradually evolve for bioethical issues concerning life and death in the future, especially as practices of VAD increase around the world. However, there still remains the issue of patient care which may be compromised without firm, clear guidelines for professional practice.
Driver 3: training and guidance
The most significant emergent theme and primary-driver from this study was the need for training and guidance about CO for pharmacist-employers and employees. There was also the misguided understanding of current legislation and/or principles of Codes of Ethics. For example, the provision of the ECP had the highest levels of conditional supply, because of misguided understanding of legal requirements around supply. This was previously demonstrated in an Australian simulation-study, where some pharmacists’ were over-reliant on outdated, non-mandatory, patient-checklists (Schneider et al., Citation2013; Scully, Citation2020) Some pharmacies in Canada and Switzerland were also found to rely on outdated patient-checklists for provision of non-prescription emergency contraception (Arnet et al., Citation2009; Soon et al., Citation2004). Updating knowledge was clearly indicated.
While the request for training and guidance for emerging practices/services like VAD (Isaac et al., Citation2019) was clear, protocols and guidance around what should be done at a time when one chooses to enact CO are non-existent, consequently placing not only the consumer at risk of lack of access, but also places the objector at risk of moral conflict, moral injury, workplace pressures and ostracisation. A clear validated framework also has the potential capacity to simultaneously address the other two drivers of ‘the role of the pharmacists' and ‘ethical considerations’.
Strengths and limitations
Limitations
Given this was a cross sectional questionnaire, a number of limitations may have affected the generalisability of the results. First, common to all questionnaires’ methodology, completion of the study may be subject to respondent bias, where only motivated eligible participants respond. Thus, the results may have been influenced by limited responses from dis-engaged participants. Additionally, the COVID-19 pandemic impacted recruiting pharmacists and restricted access to the questionnaire solely to an online format. This recruitment strategy may have also biased results by appealing to younger pharmacists who were technologically adept. We attempted to address this by advertising the questionnaire on a range of different platforms and when compared with studies conducted of other healthcare professionals (Blaschke et al., Citation2019; Card, Citation2012; Chavkin et al., Citation2013; Combs et al., Citation2011; Darzé & Barroso-Júnior, Citation2018; Dobrowolska et al., Citation2020; Fujioka et al., Citation2018; Hagen et al., Citation2011; Keogh et al., Citation2019; Lamb et al., Citation2019; Lawrence, Citation2009; Lawrence & Curlin, Citation2009; Nordstrand et al., Citation2014; Strickland, Citation2012), our findings were meaningful and not in stark contrast or variability.
Although the sample size for this study met above the calculated target sample size of 195, the results of this study remain exploratory and are by no means generalisable to the entire Australia pharmacy profession. During the Covid pandemic pharmacists were under considerable stress with rapidly changing and evolving roles, which may have affected the potential number of participants recruited.
Strengths
This is the first vignette-based study exploring a relatively large number of Australian pharmacists’ perspectives on CO. The study revealed valuable insight into the perspectives and rationale underpinning decision-making in the domain of CO in healthcare, which can inform future research.
This study also provided valuable insight into the nature of individual pharmacists’ responses which can have direct impact on patient care and the future of pharmacy practice. Therefore, each response, irrespective of its generalisability, was meaningful in that its patient-related impact, would be significant for each individual patient. This aligns with findings from US studies (French et al., Citation2016; Green & Thorogood, Citation2018; Holt et al., Citation2017; Homaifar et al., Citation2017), and a recent paper on CO in women’s health in Australia (Keogh et al., Citation2019).
Conclusion and future research
This study investigated Australian pharmacists’ perspectives regarding CO. Although most participants would not exercise CO in most cases, for the minority who chose to exercise CO, their reasons and approaches varied. For some, it was for religious values; for others, it was mostly due to the ethical tension between principles of ‘do no harm’ and ‘respect for patient autonomy’. These findings highlighted the need for further research and development of a professional framework to guide pharmacists who conscientiously object and their employers, about the processes needed to ensure patient safety, access, and continuity of care.
With a plethora of new technologies and healthcare legislations emerging around the world, it is important that professional organisations consider a universally formulated guideline that can be readily adapted to manage CO in practice. Findings of this study can provide a platform for future, more expanded research into CO in pharmacy. They may also help inform the development of new healthcare standard operating procedures around CO to guide pharmacists and their employers in navigating ethically challenging scenarios relating to CO.
Supplemental Material
Download Zip (278 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Sami Isaac
Dr. Sami Isaac is both a registered medical practitioner (GP registrar) and a registered pharmacist working in community health, having graduated with a MD, BPharm (Hons). He is also a PhD Graduate of the Sydney Pharmacy School, faculty of Medicine and Health, University of Sydney with a thesis on conscientious objection in healthcare and publications in bioethics, voluntary assisted dying and medicinal cannabis. His experience has also included academic work as a tutor with the university and involvement in the International Pharmaceutical Federation (FIP) as a speaker and member of various ethics committees.
Ardalan Mirzaei
Dr. Ardalan Mirzaei is a registered pharmacist and data scientist. He completed his PhD in the School of Pharmacy, developing a dynamic model of patients' health information-seeking behaviour. Ardi has worked in community pharmacy for over 15 years and he has a background in education, working as a training coordinator for pharmacy internships and teaching at the University of Sydney on subjects in business, pharmacy, and machine learning. His interests have led to his involvement in the International Pharmaceutical Federation (FIP) Technology Advisory Group.
Andrew J. McLachlan
Prof. Andrew J. McLachlan is the Head of School and Dean of Pharmacy in the Sydney Pharmacy School and a Member of the Order of Australia. He is the former Program Director of the NHMRC Centre for Research Excellence in Medicines and Ageing and previously Professor of Pharmacy (Aged Care) (2006-2018) in the then Faculty of Pharmacy and at Concord Hospital's Centre for Education and Research on Ageing. He is a pharmacist, academic and researcher experienced in clinical pharmacology and research on the quality use of medicines. His research focuses on understanding the variability in response to medicines and how this can be managed to optimise patient care, particularly in special patient populations such as older people, the very young and the critically ill. He is interested in translating clinical pharmacology research and high quality clinical trial evidence into real-world practice.
Betty B. Chaar
Dr. Betty B. Chaar is a pharmacist and Associate Professor in professionalism in pharmacy. She holds a master's degree in Health Law and her PhD is about developing moral reasoning capabilities and ethical decision-making in pharmacy practice. Betty has been working in the field of pharmacy for many years, with experience in community pharmacy ownership, hospital pharmacy, pharmaceutical industry, academia and research.
References
- Alele, F., & Malau-Aduli, B. (2023). 5.6 Triangulation of data. An introduction to research methods for undergraduate health profession students.
- Arnet, I., Frey Tirri, B., Zemp Stutz, E., Bitzer, J., & Hersberger, K. E. (2009). Emergency hormonal contraception in Switzerland: A comparison of the user profile before and three years after deregulation. The European Journal of Contraception & Reproductive Health Care, 14(5), 349–356. https://doi.org/10.3109/13625180903147765
- Australian Government Institute of Family Studies. (2017, updated June). Child Family Community Australia (CFCA) Resource Sheet - Age of consent laws. The Australian Institute of Family Studies. https://aifs.gov.au/cfca/publications/age-consent-laws.
- Australian Health Practitioner Regulation Agency (AHPRA) & National Boards. (2022). Shared Code of conduct Australia2022. https://www.ahpra.gov.au/Resources/Code-of-conduct/Shared-Code-of-conduct.aspx.
- Bawa, Z., Saini, B., McCartney, D., Bedoya-Pérez, M., McLachlan, A. J., & McGregor, I. S. (2022). A cross-sectional survey exploring the knowledge, experiences and attitudes of Australian pharmacists toward medicinal cannabis. International Journal of Clinical Pharmacy, 45, 375–386. https://doi.org/10.1007/s11096-022-01519-z
- Beauchamp, T. L., & Childress, J. F. (2019). Principles of biomedical ethics (8th ed). Oxford University Press.
- Benson, M. J., Abelev, S. V., Connor, S. J., Corte, C. J., Martin, L. J., Gold, L. K., … McGregor, I. S. (2020). Medicinal cannabis for inflammatory bowel disease: A survey of perspectives, experiences, and current use in Australian patients. Crohn's & Colitis 360, 2(2), otaa015.
- Blanks Hindman, E. (1999). Divergence of duty: Differences in legal and ethical responsibilities. Journal of Mass Media Ethics, 14(4), 213–230. https://doi.org/10.1207/S15327728JMME1404_2
- Blaschke, S.-M., Schofield, P., Taylor, K., & Ugalde, A. (2019). Common dedication to facilitating good dying experiences: Qualitative study of end-of-life care professionals’ attitudes towards voluntary assisted dying. Palliative Medicine, 33(6), 562–569. https://doi.org/10.1177/0269216318824276
- Callaghan, K., & Vella, T. (2023). Voluntary assisted dying (VAD) substance management - NSW health - south eastern Sydney local health district New South Wales NSW health - South Eastern Sydney Local Health District. https://www.seslhd.health.nsw.gov.au/sites/default/files/documents/SESLHDPR%20764%20-%20Voluntary%20Assisted%20Dying%20%28VAD%29%20Substance%20Management.pdf.
- Cantor, J. D. (2009). Conscientious objection gone awry–restoring selfless professionalism in medicine. New England Journal of Medicine, 360(15), 1484–1485. https://doi.org/10.1056/NEJMp0902019
- Card, R. F. (2012). Is there no alternative? Conscientious objection by medical students. Journal of Medical Ethics, 38(10), 602–604. https://doi.org/10.1136/medethics-2011-100190
- Chavkin, W., Leitman, L., & Polin, K. (2013). Conscientious objection and refusal to provide reproductive healthcare: A White Paper examining prevalence, health consequences, and policy responses. International Journal of Gynecology & Obstetrics, 123(S3), S41–S56.
- Combs, M. P., Antiel, R. M., Tilburt, J. C., Mueller, P. S., & Curlin, F. A. (2011). Conscientious refusals to refer: findings from a national physician survey. Journal of Medical Ethics, 37(7), 397–401. https://doi.org/10.1136/jme.2010.041194
- Creswell, J. W., & Clark, V. L. P. (2017). Designing and conducting mixed methods research - Chapter 3: Choosing a mixed methods design. Sage publications.
- Darzé, O., & Barroso-Júnior, U. (2018). Attitudes, and factors motivating conscientious objection toward reproductive health among medical students. Revista Brasileira de Ginecologia e Obstetrícia / RBGO Gynecology and Obstetrics, 40(10), 599–605. https://doi.org/10.1055/s-0038-1673367
- Davidson, L. A., Pettis, C. T., Joiner, A. J., Cook, D. M., & Klugman, C. M. (2010). Religion and conscientious objection: A survey of pharmacists’ willingness to dispense medications. Social Science & Medicine, 71(1), 161–165. https://doi.org/10.1016/j.socscimed.2010.03.027
- Dobrowolska, B., McGonagle, I., Pilewska-Kozak, A., & Kane, R. (2020). Conscientious object in nursing: Regulations and practice in two European countries. Nursing Ethics, 27(1), 168–183. https://doi.org/10.1177/0969733019845136
- French, V. A., Anthony, R. S., Berrios, S. E., Crockett, L. D., & Steinauer, J. E. (2016). A Sense of obligation: Attitudes and referral practices for abortion services among women’s health providers in a rural US state. Clinical Obstetrics, Gynecology and Reproductive Medicine, 2(4), 204–210. https://doi.org/10.15761/COGRM.1000151.
- Fujioka, J. K., Mirza, R. M., McDonald, P. L., & Klinger, C. A. (2018). Implementation of medical assistance in dying: A scoping review of health care providers’ perspectives. Journal of Pain and Symptom Management, 55(6), 1564–76.e9. https://doi.org/10.1016/j.jpainsymman.2018.02.011
- Glaser, B., & Straus, A. (1967). The discovery of grounded theory: Strategies for qualitative research. Adline.
- Green, J., & Thorogood, N. (2018). Qualitative methods for health. SAGE Publications.
- Griggs, S. K., & Brown, C. M. (2007). Texas community pharmacists’ willingness to participate in pharmacist-initiated emergency contraception. Journal of the American Pharmacists Association, 47(1), 48–57. doi:10.1331/1544-3191.47.1.48.Griggs
- Hagen, G. H., Hage, C., Magelssen, M., & Nortvedt, P. (2011). [Medisinstudenters holdninger til selvbestemt abort]. Tidsskrift for Den Norske Legeforening, 131(18), 1768–1771. https://doi.org/10.4045/tidsskr.10.1161
- Haining, C. M., Keogh, L. A., & Gillam, L. H. (2021). Understanding the reasons behind healthcare providers’ conscientious objection to voluntary assisted dying in Victoria, Australia. Journal of Bioethical Inquiry, 18(2), 277–289. https://doi.org/10.1007/s11673-021-10096-1
- Hanlon, T. R., Weiss, M. C., & Rees, J. (2000a). British community pharmacists’ views of physician-assisted suicide (PAS). Journal of Medical Ethics, 26(5), 363–369. https://doi.org/10.1136/jme.26.5.363
- Holt, K., Janiak, E., McCormick, M. C., Lieberman, E., Dehlendorf, C., Kajeepeta, S., … Langer, A. (2017). Pregnancy options counseling and abortion referrals among US primary care physicians. Family Medicine, 49(7), 527–536.
- Homaifar, N., Freedman, L., & French, V. (2017). “She's on her own”: A thematic analysis of clinicians' comments on abortion referral. Contraception, 95(5), 470–476. https://doi.org/10.1016/j.contraception.2017.01.007
- International Pharmaceutical Federation (FIP). (2019). Abu Dhabi 2019 Congress Session: C8 - The Ethics Forum – what does it mean to exercise conscientious objection? https://abudhabi2019.fip.org/programme-session/the-ethics-forum-what-does-it-mean-to-exercise-conscientious-objection-c8/.
- Isaac, S., McLachlan, A., & Chaar, B. (2019). Australian pharmacists’ perspectives on physician-assisted suicide (PAS): Thematic analysis of semistructured interviews. BMJ Open, 9(10), e028868. doi:10.1136/bmjopen-2018-028868
- Isaac, S., Mirzaei, A., McLachlan, A., & Chaar, B. (2023). Conscientious objection – a vignette-based, pilot study of international pharmacists’ perspectives. Pharmacy Education, 23(1), 383–406. https://doi.org/10.46542/pe.2023.231.383406
- Karanges, E. A., Suraev, A., Elias, N., Manocha, R., & McGregor, I. S. (2018). Knowledge and attitudes of Australian general practitioners towards medicinal cannabis: A cross-sectional survey. BMJ Open, 8(7), e022101. doi:10.1136/bmjopen-2018-022101
- Keogh, L. A., Gillam, L., Bismark, M., McNamee, K., Webster, A., Bayly, C., … Newton, D. (2019). Conscientious objection to abortion, the law and its implementation in Victoria, Australia: Perspectives of abortion service providers. BMC Medical Ethics, 20(1), 11. https://doi.org/10.1186/s12910-019-0346-1
- Lakens, D. (2022). Sample size justification. Psychology, 8(1). https://doi.org/10.1525/collabra.33267
- Lamb, C., Evans, M., Babenko-Mould, Y., Wong, C., & Kirkwood, K. (2019). Nurses’ use of conscientious objection and the implications for conscience. Journal of Advanced Nursing, 75(3), 594–602. https://doi.org/10.1111/jan.13869
- Lawrence, C. (2009). Autonomy, religion and clinical decisions: Findings from a national physician survey. Journal of Medical Ethics, 35(4), 214–218. https://doi.org/10.1136/jme.2008.027565
- Lawrence, R., & Curlin, F. (2009). Physicians’ beliefs about conscience in medicine: A national survey. Academic Medicine, 84(9), 1276–1282. https://doi.org/10.1097/ACM.0b013e3181b18dc5
- Lee, R. Y., Moles, R., & Chaar, B. (2015). Mifepristone (RU486) in Australian pharmacies: The ethical and practical challenges. Contraception, 91(1), 25–30. https://doi.org/10.1016/j.contraception.2014.08.003
- Maple Tech International LLC. (2023). Calculator.net Sample Size Calculator: Maple Tech International LLC https://www.calculator.net/sample-size-calculator.html?type=1&cl=95&ci=7&pp=50&ps=32777&x=Calculate.
- McDougall, R. J., White, B. P., Ko, D., Keogh, L., & Willmott, L. (2022). Junior doctors and conscientious objection to voluntary assisted dying: Ethical complexity in practice. Journal of Medical Ethics, 48(8), 517–521. https://doi.org/10.1136/medethics-2020-107125
- Munro, M. L., Dulin, A. C., & Kuzma, E. (2015). History, policy and nursing practice implications of the plan B® emergency contraceptive. Nursing for Women's Health, 19(2), 142–153. https://doi.org/10.1111/1751-486X.12186
- New South Wales Parliament Legislative Council Standing Committee on Law and Justice Report no 79. (2021). Voluntary Assisted Dying Bill 2021 2022. https://www.parliament.nsw.gov.au/tp/files/81572/Report%20No%2079%20-%20Provisions%20of%20the%20Voluntary%20Assisted%20Dying%20Bill%202021.pdf.
- Nordstrand, S. J., Nordstrand, M. A., Nortvedt, P., & Magelssen, M. (2014a). Medical students’ attitudes towards conscientious objection: A survey. Journal of Medical Ethics, 40(9), 609–612. https://doi.org/10.1136/medethics-2013-101482
- O'Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A., & Cook, D. A. (2014). Standards for reporting qualitative research. Academic Medicine, 89(9), 1245–1251. https://doi.org/10.1097/ACM.0000000000000388
- Pharmaceutical Society of Australia. (2017). Code of ethics for pharmacists Australia: Pharmaceutical Society of Australia [Available from: https://www.psa.org.au/downloads/codes/PSA-Code-of-Ethics-2017.pdf.
- Pharmacy Board of Australia AHPRA. (2020). Pharmacy Board of Australia - Registrant data (Reporting period: 01 January 2020 to 31 March 2020) [Available from: https://www.pharmacyboard.gov.au/About/Statistics.aspx.
- Piecuch, A., Gryka, M., & Kozłowska-Wojciechowska, M. (2014a). Attitudes towards conscientious objection among community pharmacists in Poland. International Journal of Clinical Pharmacy, 36(2), 310–315. https://doi.org/10.1007/s11096-013-9878-5
- Schneider, C. R., Gudka, S., Fleischer, L., & Clifford, R. M. (2013). The use of a written assessment checklist for the provision of emergency contraception via community pharmacies: A simulated patient study. Pharmacy Practice (Internet), 11(3), 127. https://doi.org/10.4321/S1886-36552013000300001
- Scully, R. P. (2020). The Guardian - Some chemists wrongly telling women they must fill in form to access emergency contraception 2020. https://www.theguardian.com/society/2020/apr/09/some-chemists-wrongly-telling-women-they-must-fill-in-form-to-access-emergency-contraception.
- Shanawani, H. (2016). The challenges of conscientious objection in health care. Journal of Religion and Health, 55(2), 384–393. https://doi.org/10.1007/s10943-016-0200-4
- Sharma, A., Minh Duc, N. T., Luu Lam Thang, T., Nam, N. H., Ng, S. J., Abbas, K. S., … Karamouzian, M. (2021). A consensus-based checklist for reporting of survey studies (CROSS). Journal of General Internal Medicine, 36(10), 3179–3187. https://doi.org/10.1007/s11606-021-06737-1
- Smith, V. P. (2006). Conscientious objection in medicine: Doctors’ freedom of conscience. British Journal of Medicine, 332(7538), 425.
- Soon, J. A., Levine, M., Osmond, B. L., Ensom, M. H., & Fielding, D. W. (2004). Provision of emergency contraceptives by pharmacists: British Columbia experience a template for other provinces. Canadian Pharmacists Journal / Revue des Pharmaciens du Canada, 137(6), 23–29. https://doi.org/10.1177/171516350413700605
- Strickland, S. L. (2012). Conscientious objection in medical students: A questionnaire survey. Journal of Medical Ethics, 38(1), 22–25. https://doi.org/10.1136/jme.2011.042770
- Verweel, L., Rosenberg-Yunger, Z. R. S., Movahedi, T., & Malek, A. H. (2018). Medical assistance in dying: Examining Canadian pharmacy perspectives using a mixed-methods approach. Canadian Pharmacists Journal / Revue des Pharmaciens du Canada, 151(2), 121–132. https://doi.org/10.1177/1715163518754917
- Willis, O. (2019). ABC health & wellbeing - is abortion legal in Australia? It's Complicated [News Article]. ABC NEWS; 2018 [updated 10 September 2019. Health. https://www.abc.net.au/news/health/2018-05-26/is-abortion-legal-in-australia/9795188.
- Yin, R. K. (2015). Qualitative research from start to finish: Guilford publications.