 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Introduction
Heart failure (HF) is a chronic condition associated with substantial mortality and hospitalisation, resulting in costly inpatient visits. The healthcare systems of several countries, including Vietnam, experience considerable difficulty in dealing with the enormous fiscal burden presented by HF. This study aims to analyse the direct medical costs associated with HF inpatient treatment from the hospital perspective.
Materials and methods
This study retrospectively analysed the electronic medical records of patients diagnosed with HF from 2018 to 2021 at Military Hospital 175 in Vietnam. The sample consisted of 906 hospitalised patients (mean age: 71.2 ± 14.1 years). The financial impact of HF was assessed by examining the direct medical expenses incurred by the healthcare system, and the costs of pharmaceutical categories used in treatment were explored.
Results
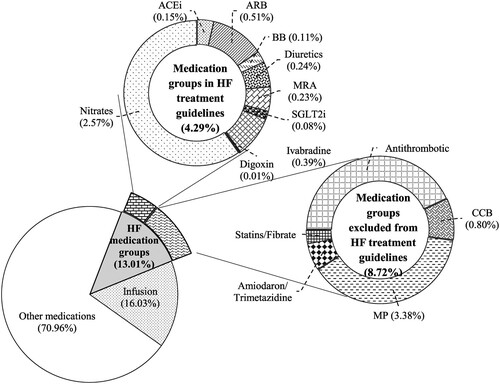
The cumulative economic burden of HF from 2018 to 2021 was US$1,068,870, with annual costs ranging from US$201,670 to US$443,831. Health insurance covered 72.7% of these costs. Medications and infusions, and medical supplies accounted for the largest expenses, at 29.8% and 22.1%, respectively. The medication HF group accounted for 13.01% of these expenses, of which the costliest medications included nitrates (2.57%), angiotensin II receptor blockers (0.51%), ivabradine (0.39%), diuretics (0.24%), and mineralocorticoid receptor antagonists (0.23%). Comorbidities and the length of hospital stay significantly influenced annual treatment costs.
Conclusion
The study reveals that HF significantly impacts Vietnam’s healthcare system and citizens, requiring a comprehensive understanding of its financial implications and efficient management of medical resources for those diagnosed. This study highlights the substantial economic burden of HF on Vietnam’s healthcare system, with medication costs, particularly antithrombotic drugs, representing the largest expense. Most healthcare costs were covered by health insurance, and expenses were significantly influenced by comorbidity and length of hospital stay. These findings can inform healthcare policy, resource allocation and optimise management strategies in Vietnam.
Introduction
On a global scale, cardiovascular disease (CVD) is the primary cause of mortality, resulting in about 17.9 million deaths annually (World Health Organization, Citation2022). As a consequence of CVD, heart failure (HF) is also a life-threatening illness characterised by elevated rates of morbidity and mortality, imposing significant burdens on patients, caregivers, and healthcare systems (Zannad, Citation2018). A study on 23,047 patients from all major geographic regions of the world showed that the morbidity rates of HF with reduced ejection fraction, HF with mid-range ejection fraction, and HF with preserved ejection fraction are 53.6%, 20.6%, and 24.2%, respectively (Joseph et al., Citation2020). In the United States, 924,000 individuals were diagnosed with HF in 2017 (Agarwal et al., Citation2021). That same year, its prevalence in North Africa, Central Europe, and the Middle East ranged from 1,133 to 1,196 per 100,000 individuals, while its prevalence in Eastern Europe and Southeast Asia was 498 to 595 per 100,000 individuals (Bragazzi et al., Citation2021). Additionally, Koudstaal et al. proposed that persons suffering from advanced HF had a bleak prognosis, as shown by a survival rate of less than 50% during a five-year period (Koudstaal et al., Citation2017). There is currently insufficient epidemiological data on HF in Vietnam; however, prevalence has also been rising, with the disease contributing 15% of total hospital admissions (Do et al., Citation2019).
The annual expenditure for treating patients with HF in the United State is around US$108 billion, of which direct medical expenses account for approximately 60% (Lesyuk et al., Citation2018). Each patient diagnosed with the illness is estimated to incur a lifetime expenditure of US$83,980 for inpatient treatment (Dunlay et al., Citation2011). The economic burden of HF in the country is attributed mostly to direct medical expenditures, with a special emphasis on hospitalisation expenses. The cost of hospitalisation for each HF patient ranges from US$13,418 to US$15,879, corresponding to 44% to 96% of total healthcare expenditure (Urbich et al., Citation2020). In Denmark, the mean expenditure per HF patient was €17,094, 70% of which was direct medical expenses with €11,926 per patient (Bundgaard et al., Citation2019). In several Asian countries, the average cost of HF hospitalisation per patient is as follows: US$8,887 in South Korea, US$2,916 to US$4,860 in Hong Kong, US$3,606 in Thailand, US$2,388 in Taiwan, and US$800 in Indonesia (Reyes et al., Citation2016). Medical expenditures per patient in South Korea from 2011 to 2012 consisted of those linked to investigations (US$2,852.05), treatments and procedures (US$1,481.59), hospital beds (US$1,026.32), medications (US$455.57), consultations (US$150.42), and blood supply (US$84.04) (Kim et al., Citation2018). In Vietnam, the average total treatment cost per case of HF was US$394.7, based on the payer perspective, according to health insurance data from 2017 to 2018 (Thuy et al., Citation2020). A study conducted on HF outpatients and inpatients covered by health insurance for the period 2020–2022 in cardiovascular specialised hospitals, found that the direct medical cost of heart failure treatment was valued at US$62.2 for one outpatient visit and US$714 for one inpatient visit (Pham et al., Citation2023). These figures show a significant economic burden on Vietnam’s healthcare system and patients; however, they might not capture the full economic burden. Findings from the health insurance data exclude out-of-pocket expenses or expenses for uninsured individuals (Thuy et al., Citation2020). On the other hand, the estimated cost in tertiary specialist hospitals might reflect the burdens of patients with the majority at severe levels (Pham et al., Citation2023). Consequently, these highlight a critical gap in understanding the comprehensive economic impact of HF across all patient demographics.
Vietnam’s healthcare system comprises the public and private sectors, organised into a four-tiered hierarchical structure comprising the central, provincial, district, and commune levels (Quan & Taylor-Robinson, Citation2023). Social health insurance (SHI) is a crucial component of Vietnam's healthcare financing, covering a significant portion of the population (Le et al., Citation2020). SHI provides coverage for healthcare costs primarily in public health facilities, with limited coverage for services obtained in private facilities. Despite its extensive coverage, there are challenges related to the adequacy of the benefits and financial protection offered to patients, especially those seeking care outside the public system or uninsured patients. The cost data derived from actual clinical practice offer significant insights into the socioeconomic impact of HF and serve as crucial primary data for health technology assessment (HTA) (Lesyuk et al., Citation2018). HTA is critical in enabling the objective evaluation and prioritisation of healthcare provision and the allocation of resources, including payment for new interventions, such as novel medications, preventive programmes, surgical operations, and more (Drummond et al., Citation2008). Accordingly, cost-of-illness studies have gained global recognition as reliable sources of evidence on whose basis medical decisions can be made (Lesyuk et al., Citation2018).
The objective of this study was to examine the treatment cost of HF incurred from 2018 to 2021 at Military Hospital 175 in Ho Chi Minh City, Vietnam, from the perspective of the hospital and to investigate factors associated with the economic burden of HF.
Materials and methods
Study design and population
This study was a prevalence-based cost-of-illness analysis. A retrospective bottom-up analysis of electronic medical records was conducted to estimate the direct medical expenses spent on HF inpatients from 2018 to 2021. This process included identifying all resources used for HF treatment and documenting the amount and unit price of each item (Choi & Lee, Citation2019; Jo, Citation2014). This study involved adult patients hospitalised in the Military Hospital 175, recognised as the central-level hospital and military medical centre in southern Vietnam, in the period 2018–2021. This hospital has an extensive database that covers information on its HF patients, hence facilitating the identification of individuals who have been treated for this condition. The eligible population was identified using the International Classification of Diseases 10th Revision (ICD-10) with specific ICD-10 codes related to heart failure (HF): I11.0 for hypertensive heart disease with congestive HF, I13.0 for hypertensive heart and renal disease with congestive HF, I13.2 for hypertensive heart and renal disease with both congestive HF and renal failure, and I50.x for HF as the primary diagnosis (Lee et al., Citation2016; World Health Organization, Citation2019). However, patients with a secondary diagnosis of HF were excluded to ensure the specificity of this cost-of-illness analysis. Including these patients could introduce variability due to the costs associated with their primary diagnoses and comorbidity, which might skew the results. Focusing solely on primary HF diagnoses provides a more accurate and consistent estimate of the direct medical costs attributable to HF treatment.
Cost calculations
To analyse the consumption of healthcare resources by patients, this study concentrated specifically on the assessment of direct medical expenses related to HF treatment during hospitalisation. The expenses examined in this research included those related to the number of bed days required for inpatient care, consultations with physicians, medications, infusions, laboratory tests, diagnostic imaging, surgical operations, and medical supplies, as well as costs associated with blood, blood products, and other treatments administered over the course of illness. The discount factor for medications and services was not considered. The cost of each component was determined by multiplying its unit price by the amount used. The total annual cost of HF therapy is calculated by summing up the costs of all the components used in HF management over a year. The healthcare expenditures associated with HF per patient per year (PPPY) and per hospitalisation per year (PHPY) were also assessed. The mean yearly expense per patient or hospitalisation was determined using the following equations:
and
This research likewise delved into the expenses associated with the primary categories of medications that are often administered to manage HF, with the aim of exhaustively explaining the pharmaceutical use patterns at Military Hospital 175. The medicines were categorised into those included and excluded from HF treatment guidelines (Ministry of Health, Citation2022). Finally, the financial burden imposed on patients in terms of out-of-pocket expenses and extent of health insurance coverage was investigated.
The consumer price index was used to convert the unit prices applicable in the period 2018–2021 into valid costs for the reference year (i.e. 2022) (Riewpaiboon, Citation2018):
All costs were expressed in US dollars for 2022 on the basis of the average exchange rate of US$ to VND provided by the State Bank of Vietnam (i.e. US$1 = VND23,271) (The State Bank of Vietnam, Citation2022).
Statistical analyses
The medical electronic data examined in this work comprised demographic information, including case identification, patient age, gender, insurance code (which was used to determine discounts [in percentage] from total costs), medical admission and discharge details, comorbidities, the quantities of drugs administered to each patient, and the frequency of testing conducted for each of them. Descriptive statistics were used to summarise the results. The categorical variables were the number of observations, percentage, and median, along with the 25th and 75th percentiles, and the continuous variables were measured as mean ± standard deviation (SD). Missing values were excluded from the answer percentages pertaining to each category.
A generalised linear model (GLM) with a log-link function and gamma distribution was used to probe into the influence of demographic variables (age group, gender, comorbidities, and duration of hospital stay) on overall medical expenditures. The statistical significance threshold was determined to be p < 0.05, which was regarded as indicative of high confidence.
One-way sensitivity analysis was carried out to assess the effects of altering each parameter while holding all other factors constant. Two specific cost components – primary pharmaceutical categories and therapeutic medical devices – were analysed within the direct medical cost structure for HF. These analyses were performed to inform decision-making on budgeting for the healthcare system (Briggs & Gray, Citation1999; Taylor, Citation2009). The statistical analyses were run on Microsoft Excel 365® and the Statistical Package for the Social Sciences® version 26.0.
Ethical approval
This research was granted ethical clearance by the Research Ethics Board at Pham Ngoc Thach University of Medicine (Approval No. 847/TĐHYKPNT-HĐĐĐ) and Military Hospital 175 (Approval No. 1371/GCN-HĐĐĐ). The research strategy and methods employed were approved by the hospital’s ethics committee, which afforded the researchers access to the requisite resources. Given the use of hospital records, which contained personal information, appropriate measures were taken to anonymise sensitive data and uphold patient confidentiality. Due to the utilisation of available anonymised data for retrospective analysis, without involving any direct interactions with patients, and with approval from the ethics committee, formal informed consent from the patients was not required. The data was intended only for research and accessible only to the researchers and their colleagues.
Results
Patient characteristics
presents the characteristics of patients diagnosed with HF from 2018 to 2021 at Military Hospital 175. The research involved a cohort of 906 eligible patients, corresponding to 1027 hospitalisations. The incidence of readmission fluctuated, decreasing from 11.4% in 2018 to 5.6% in 2019 before increasing to 9.1% in 2021. Most of the patients (54.1%) were male, and 69.5% were aged 65 years or older. The patients covered fully by health insurance accounted for the highest percentage of the sample (46.6%). In terms of comorbidities, 38.6% had hypertensive illnesses, followed by diabetes mellitus (19.7%), ischemic heart diseases (18.9%), pneumonia (13.3%), renal diseases (10.0%), atrial fibrillation (5.9%), dyslipidemia (1.8%), and other cardiovascular conditions (3.6%). The hospital recorded 481 emergency admissions attributable to HF, representing 46.7% of the total.
Table 1. Baseline characteristics of HF inpatients (2018–2021).
Direct medical cost components
presents data on the yearly costs per patient and per hospitalisation associated with healthcare services for HF from 2018 to 2021. The cumulative expenditure for HF therapy over four years amounted to US$1,068,870, of which the majority comprised expenses on medications and infusion services (i.e. US$318,314 of 29.8%). Expenses related to medical supplies, laboratory tests, bed days, and surgical operations amounted to US$236,137, US$175,460, US$160,977, and US$118,409, respectively, representing a significant proportion of overall medical expenses. The total average cost PHPY ranged from US$858.36 (2021) to US$1,212.63 (2019), and the total average cost PPPY ranged from US$964.19 (2021) to US$1,318.08 (2019).
Table 2. Annual healthcare expenditures PHPY/PPPY on HF treatment (2018–2021) (US$ 2022).
Sources of payment for HF treatment
shows the out-of-pocket expenditures borne by the patients and health insurance payments. During the four-year period, most of the healthcare costs were covered by health insurance, except for medical supplies, which accounted for 54.1% (US$127,809.1) of out-of-pocket expenses. The average health insurance payments accounted for more than 70% of healthcare expenditures on HF each year.
Table 3. Annual healthcare expenditures by patient and health insurance (2018–2021) [US$ (%)].
Distribution of pharmaceutical costs during HF treatment
presents the expenditures of patients and health insurance companies associated with each pharmaceutical category and infusions for the management of HF over the period studied. The combined expenditure on medications and infusion services was US$318,314, and the percentage of health insurance payments for pharmaceuticals and infusions was more than 85% each year. The drug groups used to manage HF were priced differently depending on the type of payer. Out-of-pocket payments ranged from US$6.9 for digoxin to US$1,646.9 for nitrates, while health insurance payments ranged from US$36.9 for digoxin to US$10,415.2 for antithrombotic. For infusions, patient payments reached US$7,944.0 (15.6%), whereas health insurance coverage amounted to US$43,074.3 (84.4%).
Table 4. Cost of pharmaceuticals and infusions by patient and health insurance (2018–2021) [US$ (%)].
illustrates the proportion spent by Military Hospital 175 on pharmaceuticals and infusions. The medication HF group accounted for 13.01% of these expenses, infusions accounted for 16.03%, and other medications made up 70.96%. The two groups of medications for HF patients, inside (4.29%) and outside (8.72%) recommended guidelines, were clarified. For drugs included in the HF guidelines, most of the expenses were devoted to nitrates (2.57%), followed by angiotensin II receptor blockers (ARBs) (0.51%), ivabradine (0.39%), diuretics (0.24%), and mineralocorticoid receptor antagonists (MRAs) (0.23%). For medications outside the treatment guidelines, the majority of spending was allocated to antithrombotic (3.75%), magnesium and potassium aspartate (MP) (3.38%), calcium channel blockers (CCBs) (0.80%), amiodaron or trimetazidine (0.52%), and statins or fibrates (0.27%).
Figure 1. Proportions of medication group expenses in the costs of pharmaceuticals and infusions (2018–2021). ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin II receptor blocker; BB: beta-blocker; CCB: calcium channel blocker; CV: cardiovascular; NOACs: novel oral anticoagulants; VKAs: vitamin K antagonists; MP: magnesium aspartate and potassium aspartate; MRA: mineralocorticoid receptor antagonist; SGLT2i: sodium-glucose co-transporter 2 inhibitors.
presents the factors influencing the expenses associated with HF therapy, as determined via GLM. Pneumonia comorbidities and lengthy hospital stays were associated with higher costs of HF treatment in all the four years examined. A statistically significant difference in expenses was found between patients with hypertensive diseases, ischemic heart diseases, and diabetes mellitus and healthy individuals, with expenses increasing by 24.4% in 2021, 30.3% in 2020, and 30.8% in 2021, respectively (p < 0.05).
Sensitivity analysis
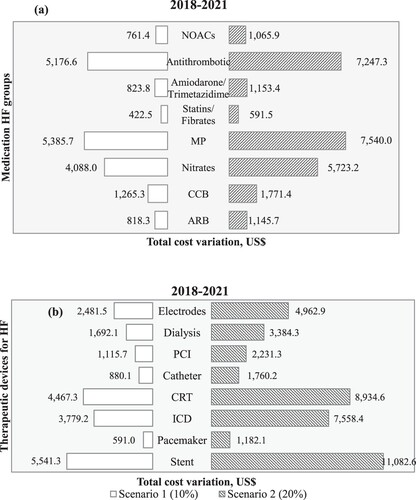
The tornado diagram in shows the effects of variations in expenses associated with drug groups and medical supplies on the overall healthcare-related cost of hospitalisation. Two scenarios featuring changes of 50% and 70% were used to look into the costs of medicines for the HF groups. MP (US$5385.7–US$7540.0) and antithrombotic (US$5176.6–US$7247.3) exhibited the most significant variations in terms of cost ((a)). The principal types of devices used in HF treatment were analysed under two scenarios featuring 10% and 15% variations. The cost of stent and cardiac resynchronisation therapy (CRT) had a notable effect on the overall cost of HF treatment, resulting in a range of US$5,541.3 to US$11,082.6 and US$4,467.3 to US$8,934.6, respectively ((b)).
Figure 2. Tornado diagram: (a) Impact of medication groups on total HF cost (2018–2021) and (b) impact of the main types of device therapy on total HF cost (2018–2021). *The central baseline value is US$0, corresponding to the total cost of HF for the period 2018–2021; ARB: angiotensin II receptor blocker; CCB: calcium channel blocker; CRT: cardiac resynchronisation therapy; ICD: implantable cardioverter defibrillator; MP: magnesium aspartate and potassium aspartate; NOACs: novel oral anticoagulants; PCI: percutaneous coronary intervention.
Discussion
This study derived evidence on the economic burden of HF in Vietnam. The observed fluctuations may be attributed to the decrease in the number of individuals requiring hospitalisation because of the COVID-19 pandemic in 2019–2021. Consequently, government authorities implemented a series of restrictive measures, often referred to as lockdown regulations, to mitigate the transmission of the viral infection. The findings indicated that the five-year readmission rates for HF varied from 5.6% to 11.4%, which are lower than those observed in Taiwan (21.5%) and Malaysia (22.1%) but greater than those documented in Korea (4.0%) and Thailand (9.0%) (Yingchoncharoen et al., Citation2021). Research on the economic impact on HF patients enrolled in Medicare found readmission rates of 8.4%, 13.4%, and 16.7% within 30, 60, and 90 days, respectively (Kilgore et al., Citation2017). The current investigation observed a range of 1.09–1.16 in the mean number of hospital admissions PPPY, with the five-year average being 1.13. More frequent hospitalisations were observed in South Korea (1.4 ± 0.9), Taiwan (1.3 ± 0.6), Thailand (1.2 ± 0.5), and Malaysia (1.4 ± 0.7) (Yingchoncharoen et al., Citation2021), but a study in Korea reported a rate similar (1.14) to that found in the current work (Cho et al., Citation2018). The present study observed a mean length of stay of 9.6 days, which is longer than that found by Kilgore et al. (7.07 days) (Kilgore et al., Citation2017) but shorter than that discovered by Kim et al. (9.95 days) (Kim et al., Citation2018).
HF poses a burden on the overall well-being of the worldwide population, particularly among those in advanced age (Ambrosy et al., Citation2014). Most of the HF patients in the present research were 65 years old and above, consistent with studies conducted in Asian nations, such as Korea (64.6%), Thailand (66.0%), China (69.0%), and Taiwan (82.5%) (Cho et al., Citation2018; Huang et al., Citation2017; Yingchoncharoen et al., Citation2021). The findings indicated that the most prevalent comorbidities in individuals with HF were hypertension and diabetes. A study in Japan found that 52% of individuals with HF had hypertension, and 26% had diabetes mellitus (Kanaoka et al., Citation2019). Explorations in Malaysia, Denmark, the Czech Republic, and the United States reported comparable rates of hypertension and diabetes mellitus among individuals with HF (Bundgaard et al., Citation2019; Kilgore et al., Citation2017; Ong et al., Citation2022; Pavlušová et al., Citation2018). From 2018 to 2021, a significant hospitalisation rate of 46.7% was found for emergency HF patients, which notably diverges from the results on certain countries, such as Korea (15%), Thailand (27%), and Malaysia (22.1%) but lower in comparison with Taiwan (64%) (Yingchoncharoen et al., Citation2021). This heterogeneity may be attributed to differences in demographics among studies conducted in various countries.
Table 5. Generalised linear regression model with log link and gamma distribution (2018–2021).
The estimates of the various components of medical costs PPPY were considerably higher than those reported in a prior study in Vietnam (Thuy et al., Citation2020). However, the average total medical cost per patient ranged from US$964.19 to US$1,318.08, which is much lower than those reported in other countries. The total annual medical costs for each patient in South Korea (Kim et al., Citation2018) amounted to US$6,199, but those in Saudi Arabia reached US$9,563 (Alghamdi et al., Citation2021). The findings indicated a notable disparity from research conducted in other nations, but it is important to view this comparison with caution given potential variations in unit costs, study durations, exchange rates, and annual inflation rates across different countries. Furthermore, the present analysis identified medications and infusions as the largest cost components, accounting for 29.8% and 22.1% of the total, respectively. An earlier study reported that the cost of examination constituted the majority of expenses (44.8%), while pharmaceutical expenditure accounted for 7.6% (Kim et al., Citation2018). Another study reported pharmaceutical prices of 12.0% (Ong et al., Citation2022), 11% (Alghamdi et al., Citation2021), and 15% (Ogah et al., Citation2014). Medication costs (42.0%) and procedure costs (40.8%) accounted for the largest proportions (42.0%) of outpatient and inpatient costs in Malaysia (Ong et al., Citation2022). The observed discrepancy may be ascribed to the unique medical cost components and the classification of economic situations in different research locations or the use of diverse treatment regimens across various organisations for the management of HF. The higher cost of medications and infusions for heart failure treatment in Vietnam, compared to other countries in the region, can be attributed to several factors. Inflated medicine prices significantly impact access to essential medicines (T. A. Nguyen et al., Citation2017). The excessive prices of generic drugs are due to financial inducements paid to prescribers and procurement officers, which constitute a major cost component. Additionally, poor market intelligence, failure to achieve economies of scale, and multiple layers in the supply chain further contribute to high prices. Unregulated retail markups exacerbate the situation. In the public sector, medicines are generally expensive and low in availability and affordability, increasing the overall cost burden on patients (A. T. Nguyen et al., Citation2009). Physician consultations comprised the smallest proportion (0.1%) of expenses, consistent with the finding of Kim et al. (Citation2018) (1.13%) (Kim et al., Citation2018). Physician consultation fees might be standardised or regulated to keep them relatively low compared with other components of treatment, thereby ensuring accessibility, affordability, and fairness in healthcare delivery.
Health insurance covered most of the annual medical expenditures incurred by patients with HF, with the average being 72.7%. This finding indicates a higher insurance coverage rate in Vietnam than in Asian regions, such as Malaysia (65.4%), South Korea (67.4%), and Thailand (70.1%), but a lower coverage than Taiwan (86.8%) (Yingchoncharoen et al., Citation2021). The HF patients in this research were of advanced ages (mean age: 71.2 ± 14.1 years) and beyond the typical age for employment, resulting in limited or nonexistent financial resources. According to Vietnam Social Insurance, more than 10.8 million out of 11.3 million elderly individuals had health insurance in 2019, accounting for nearly 96% of the population that year (Vietnam Social Insurance, Citation2019). A study confirmed that health insurance helps patients reduce out-of-pocket spending by about 23% at each hospitalisation (C. V. Nguyen, Citation2012). Consequently, patients often rely on health insurance to reduce expensive treatment costs for noncommunicable diseases in general and CVDs in particular, especially HF (Kankeu et al., Citation2013). However, note that more than half of medical supplies were paid out of pocket, which is a significant burden on HF patients.
A comprehensive analysis was directed to expenses associated with pharmaceuticals and infusions, after which the insights derived were assessed and integrated to categorise the pharmaceutical classes used in the management of HF. The findings indicated fluctuations in the overall expenditure on medicines and infusion services. Specifically, there was a significant drop in prices from 2018 to 2020, with a decline from US$125,144 to US$53,816. The observed fluctuations may be attributed to the fluctuating number of patients on an annual basis, resulting in varying levels of medicine usage.
Notably, certain medications within this group, including antithrombotics (3.75%), MP (3.38%), and nitrates (2.57%), accounted for substantial expenses on medications and infusions, thus underscoring the financial burden associated with these drugs in HF management. However, antithrombotics and MP are outside HF treatment guidelines in Vietnam. This phenomenon might be due to differences in clinical practice, local preferences, or a lack of strong evidence supporting their use in the HF context. It is essential to assess whether the clinical benefits of these medications justify their expense and whether their inclusion in treatment protocols should be reevaluated. In accordance with the findings of Ong et al., the highest mean cost PPPY for different medication groups was that related to angiotensin receptor-neprilysin inhibitors, followed by ARB, angiotensin-converting enzyme inhibitors (ACEis), beta-blockers (BB), and MRA (Ong et al., Citation2022). The variations in medication costs may reflect differences in healthcare practices and drug availability between Vietnam and other countries.
The regression model showed that age affected medical expenses, which is similar to the findings of Alghamdi et al., who reported that the older a patient, the higher the average annual direct medical costs (Alghamdi et al., Citation2021). However, this contrasts with the results of Kim et al (Kim et al., Citation2018). Older individuals with HF often have additional health conditions, such as hypertension, diabetes, and chronic kidney disease (Bekmurodovna et al., Citation2020). Comorbidities are associated with the HF costs incurred by patients with additional health conditions (Urbich et al., Citation2020). Managing HF in adults often involves multiple medications to address both HF and comorbid conditions, which not only increases medication costs but also raises the risk of medication-related adverse events. These outcomes can lead to even more healthcare expenses. In the present work, costs were largely driven by the length of hospital stay. Lahewala et al. determined that the average cost of care per patient with HF is US$15,732 and that the mean duration of stay per patient is 6.1 days (Lahewala et al., Citation2019). For patients with HF, the related mean cost of care is estimated at US$25,879, and the mean length of hospital stay is 7.5 days.
The one-way sensitivity analysis revealed that the most significant impact occurred amid changes in expenses associated with medications and medical supplies. According to research conducted on chronic HF in the Philippines, the overall expenses associated with hospitalisation for chronic HF are highly influenced by the costs of diagnostic tests. Conversely, the effects of pharmaceutical costs on total expenditure is nonsignificant (Tumanan-Mendoza et al., Citation2018). The research found that a 50% to 70% increase in the cost of MP medication leads to a significant rise in the four-year medical cost of HF, ranging from US$6,996.0 to US$9,794.4. Similarly, a 10% to 15% increase in the cost of implanted cardioverter defibrillators increases the four-year medical cost of HF from US$6,913.2 to US$10,369.7. These findings have the potential to assist medical institutions in optimising resource allocation, namely, in the areas of pharmaceutical groups and therapeutic devices for HF, and efficiently achieving cost savings.
The predominance of HF among older age groups and the prevalence of comorbidities like hypertension and diabetes highlight the complex nature of HF management, particularly in aging populations. Policy discussions may focus on targeted interventions for managing comorbidities and promoting healthy aging strategies to reduce the overall burden of HF. The substantial coverage of medical costs by health insurance in Vietnam indicates a positive aspect of healthcare accessibility. However, the out-of-pocket burden for medical supplies underscores potential areas for policy improvement, such as expanding insurance coverage or implementing cost-reduction strategies for essential medical supplies. The findings highlight the significant impact of medication and medical supply costs on total expenditures. Policy initiatives aimed at cost-effective medication use and rational treatment protocols have the potential to improve outcomes and reduce economic burdens on patients and healthcare systems.
The present study has several notable strengths. It offered a comprehensive and meticulous cost analysis of HF treatment and derived cost estimates on the basis of out-of-pocket and health insurance payments. It elucidated the correlation between certain common characteristics and treatment expenses during the period studied. The research can be considered an accurate and reliable economic evaluation of HF-related interventions. Nevertheless, it was also encumbered by certain limitations. The population investigated does not encompass the entirety of the Vietnamese HF community but is centred on HF patients receiving treatment at a military hospital. This introduces potential selection bias as the sample may not fully represent the broader HF population in Vietnam. Patients treated at military hospitals might have different health profiles or access to healthcare resources compared to the general population. Furthermore, the data was obtained from medical records and only direct medical expenses were quantified. Consequently, an analysis of the nonmedical expenses and indirect costs associated with HF was not conducted, thereby constraining the reflection of the complete societal impact of HF. This limitation may result in an underestimation of the total economic burden of HF. A few factors were analysed in the regression model because several determinants were excluded, given the considerable proportion of missing data. This exclusion may have led to omitted variable bias, affecting the accuracy of the model's predictions. Finally, the sensitivity analysis was directed only at pharmaceutical and medical supply expenditures, potentially missing other components such as hospitalisation costs, diagnostic tests, and outpatient visits. This narrow focus limits the comprehensiveness of the cost analysis. Future research should investigate the direct nonmedical expenses and indirect costs associated with HF, as these factors significantly contribute to treatment and economic burdens. Multiple centres should be involved, and evaluations should be conducted nationally to compare hospitals in several regions. Economic evaluation is essential to identify the most cost-effective interventions, while longitudinal studies tracking patients over several years can provide valuable insights into the long-term benefits of early interventions. Additionally, research into health equity can reveal disparities in HF management and outcomes, guiding improvements to ensure equitable care across socioeconomic and ethnic groups. Overall, these findings underscore the importance of continued research and policy development to enhance HF management and mitigate its economic impact on healthcare systems. Policymakers could use the study’s findings to strengthen health insurance schemes, ensuring adequate coverage for HF treatments, thereby lessening the financial strain on affected individuals. The study’s findings support the current trend towards personalised medicine in heart failure management, highlighting the need for tailored treatment plans. By demonstrating the economic burden of heart failure, the study underscores the importance of preventative measures and early intervention strategies in national healthcare policies.
Conclusion
This study highlights the significant economic burden of HF on healthcare systems while filling a crucial gap by considering previously overlooked factors such as uninsured individuals and out-of-pocket expenses. Identifying medication costs as a major expense, the study highlights challenges to optimising drug procurement and medication use according to treatment guidelines. Moreover, the significant role of health insurance in mitigating costs suggests that enhancing insurance coverage and reducing out-of-pocket expenses could substantially alleviate the financial burden on patients. These insights can inform targeted interventions to improve resource allocation, ultimately enhancing the quality and sustainability of HF care.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Agarwal, M. A., Fonarow, G. C., & Ziaeian, B. (2021). National trends in heart failure hospitalizations and readmissions from 2010 to 2017. JAMA Cardiology, 6(8), 952–956. https://doi.org/10.1001/jamacardio.2020.7472
- Alghamdi, A., Algarni, E., Balkhi, B., Altowaijri, A., & Alhossan, A. (2021). Healthcare expenditures associated with heart failure in Saudi Arabia: A cost of illness study. Healthcare, 9(8), 988. https://doi.org/10.3390/healthcare9080988
- Ambrosy, A. P., Fonarow, G. C., Butler, J., Chioncel, O., Greene, S. J., Vaduganathan, M., Nodari, S., Lam, C. S., Sato, N., & Shah, A. N. (2014). The global health and economic burden of hospitalizations for heart failure: Lessons learned from hospitalized heart failure registries. Journal of the American College of Cardiology, 63(12), 1123–1133. https://doi.org/10.1016/j.jacc.2013.11.053
- Bekmurodovna, T. K., Erkinovna, E. N., Gadaevich, G. A., Oripovna, D. N., & Abdujalolovna, K. F. (2020). Comorbid states in patients with chronic heart failure. Regional level of the problem (preliminary study). Journal of Cardiovascular Disease Research, 11(2), 59–65.
- Bragazzi, N. L., Zhong, W., Shu, J., Abu Much, A., Lotan, D., Grupper, A., Younis, A., & Dai, H. (2021). Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017. European Journal of Preventive Cardiology, 28(15), 1682–1690. https://doi.org/10.1093/eurjpc/zwaa147
- Briggs, A. H., & Gray, A. M. (1999). Handling uncertainty in economic evaluations of healthcare interventions. BMJ, 319(7210), 635–638. https://doi.org/10.1136/bmj.319.7210.635
- Bundgaard, J. S., Mogensen, U. M., Christensen, S., Ploug, U., Rørth, R., Ibsen, R., Kjellberg, J., & Køber, L. (2019). The economic burden of heart failure in Denmark from 1998 to 2016. European Journal of Heart Failure, 21(12), 1526–1531. https://doi.org/10.1002/ejhf.1577
- Cho, H., Oh, S.-H., Lee, H., Cho, H.-J., & Kang, H.-Y. (2018). The incremental economic burden of heart failure: A population-based investigation from South Korea. PLoS One, 13(12), e0208731.
- Choi, H.-J., & Lee, E.-W. (2019). Methodology of estimating socioeconomic burden of disease using national health insurance (NHI) data. In S. Reddy & A. I. Tavares (Eds.), Evaluation of health services. IntechOpen.
- Do, T. N. P., Do, Q. H., Cowie, M. R., Ha, N. B., Do, T. H., Nguyen, T. T. H., Tran, T. L., Nguyen, T. N. O., Nguyen, T. M. H., & Chau, T. T. Q. (2019). Effect of the optimize heart failure care program on clinical and patient outcomes – The pilot implementation in Vietnam. IJC Heart & Vasculature, 22, 169–173. https://doi.org/10.1016/j.ijcha.2019.02.010
- Drummond, M. F., Schwartz, J. S., Jönsson, B., Luce, B. R., Neumann, P. J., Siebert, U., & Sullivan, S. D. (2008). Key principles for the improved conduct of health technology assessments for resource allocation decisions. International Journal of Technology Assessment in Health Care, 24(3), 244–258. https://doi.org/10.1017/S0266462308080343
- Dunlay, S. M., Shah, N. D., Shi, Q., Morlan, B., VanHouten, H., Hall Long, K., & Roger, V. L. (2011). Lifetime costs of medical care after heart failure diagnosis. Circulation: Cardiovascular Quality and Outcomes, 4(1), 68–75. https://doi.org/10.1161/CIRCOUTCOMES.110.957225
- Huang, J., Yin, H., Zhang, M., Ni, Q., & Xuan, J. (2017). Understanding the economic burden of heart failure in China: Impact on disease management and resource utilization. Journal of Medical Economics, 20(5), 549–553. https://doi.org/10.1080/13696998.2017.1297309
- Jo, C. (2014). Cost-of-illness studies: Concepts, scopes, and methods. Clinical and Molecular Hepatology, 20(4), 327. https://doi.org/10.3350/cmh.2014.20.4.327
- Joseph, P., Dokainish, H., McCready, T., Budaj, A., Roy, A., Ertl, G., Gomez-Mesa, J. E., Leong, D., Ezekowitz, J., & Hage, C. (2020). A multinational registry to study the characteristics and outcomes of heart failure patients: The global congestive heart failure (G-CHF) registry. American Heart Journal, 227, 56–63. https://doi.org/10.1016/j.ahj.2020.06.002
- Kanaoka, K., Okayama, S., Nakai, M., Sumita, Y., Nishimura, K., Kawakami, R., Okura, H., Miyamoto, Y., Yasuda, S., & Tsutsui, H. (2019). Hospitalization costs for patients with acute congestive heart failure in Japan. Circulation Journal, 83(5), 1025–1031. https://doi.org/10.1253/circj.CJ-18-1212
- Kankeu, H. T., Saksena, P., Xu, K., & Evans, D. B. (2013). The financial burden from non-communicable diseases in low- and middle-income countries: A literature review. Health Research Policy and Systems, 11(1). https://doi.org/10.1186/1478-4505-11-31
- Kilgore, M., Patel, H. K., Kielhorn, A., Maya, J. F., & Sharma, P. (2017). Economic burden of hospitalizations of Medicare beneficiaries with heart failure. Risk Management and Healthcare Policy, 10, 63–70. https://doi.org/10.2147/RMHP.S130341
- Kim, E., Kwon, H.-Y., Baek, S. H., Lee, H., Yoo, B.-S., Kang, S.-M., Ahn, Y., & Yang, B.-M. (2018). Medical costs in patients with heart failure after acute heart failure events: One-year follow-up study. Journal of Medical Economics, 21(3), 288–293. https://doi.org/10.1080/13696998.2017.1403922
- Koudstaal, S., Pujades-Rodriguez, M., Denaxas, S., Gho, J. M., Shah, A. D., Yu, N., Patel, R. S., Gale, C. P., Hoes, A. W., & Cleland, J. G. (2017). Prognostic burden of heart failure recorded in primary care, acute hospital admissions, or both: A population-based linked electronic health record cohort study in 2.1 million people. European Journal of Heart Failure, 19(9), 1119–1127. https://doi.org/10.1002/ejhf.709
- Lahewala, S., Arora, S., Tripathi, B., Panaich, S., Kumar, V., Patel, N., Savani, S., Dave, M., Varma, Y., & Badheka, A. (2019). Heart failure: Same-hospital vs. different-hospital readmission outcomes. International Journal of Cardiology, 278, 186–191. https://doi.org/10.1016/j.ijcard.2018.12.043
- Le, Q. N., Blizzard, L., Si, L., Giang, L. T., & Neil, A. L. (2020). The evolution of social health insurance in Vietnam and its role towards achieving universal health coverage. Health Policy OPEN, 1, Article 100011. https://doi.org/10.1016/j.hpopen.2020.100011
- Lee, H., Oh, S.-H., Cho, H., Cho, H.-J., & Kang, H.-Y. (2016). Prevalence and socio-economic burden of heart failure in an aging society of South Korea. BMC Cardiovascular Disorders, 16(1), 1–9. https://doi.org/10.1186/s12872-015-0179-x
- Lesyuk, W., Kriza, C., & Kolominsky-Rabas, P. (2018). Cost-of-illness studies in heart failure: A systematic review 2004–2016. BMC Cardiovascular Disorders, 18(1), 1–11. https://doi.org/10.1186/s12872-018-0815-3
- Ministry of Health. (2022). Guidelines for the diagnosis and treatment of acute and chronic heart failure.
- Nguyen, C. V. (2012). The impact of voluntary health insurance on health care utilization and out-of-pocket payments: New evidence for Vietnam. Health Economics, 21(8), 946–966. https://doi.org/10.1002/hec.1768
- Nguyen, A. T., Knight, R., Mant, A., Cao, Q. M., & Auton, M. (2009). Medicine prices, availability, and affordability in Vietnam. Southern Med Review, 2(2), 2–9.
- Nguyen, T. A., Knight, R., Mant, A., Razee, H., Brooks, G., Dang, T. H., & Roughead, E. E. (2017). Inflated medicine prices in Vietnam: A qualitative study. Health Policy and Planning, 32(5), 647–656. https://doi.org/10.1093/heapol/czw174
- Ogah, O. S., Stewart, S., Onwujekwe, O. E., Falase, A. O., Adebayo, S. O., Olunuga, T., & Sliwa, K. (2014). Economic burden of heart failure: Investigating outpatient and inpatient costs in Abeokuta, Southwest Nigeria. PLoS One, 9(11), e113032. https://doi.org/10.1371/journal.pone.0113032
- Ong, S. C., Low, J. Z., Yew, W. Y., Yen, C. H., Kader, M. A. S. A., Liew, H. B., … Ghapar, A. K. A. (2022). Cost analysis of chronic heart failure management in Malaysia: A multi-centred retrospective study. Frontiers in Cardiovascular Medicine, 9, 1–18. https://doi.org/10.3389/fcvm.2022.971592
- Pavlušová, M., Klimes, J., Špinar, J., Zeman, K., Jarkovský, J., Benešová, K., Miklik, R., Pohludková, L., Felšöci, M., & Veselá, V. (2018). Chronic heart failure – impact of the condition on patients and the healthcare system in the Czech Republic: A retrospective cost-of-illness analysis. Cor et Vasa, 60(3), e224–e233. https://doi.org/10.1016/j.crvasa.2018.03.002
- Pham, M. H., Bui, M. T., Vo, N. Y. N., Mai, T. H., Nguyen, C. T., Nguyen, T. T. T., … Nguyen, T. T. T. (2023). Analysis of direct medical costs in heart failure treatment at some specialized hospitals in the period of 2020–2022. Vietnam Medical Journal, 527(1B), 46–50. https://doi.org/10.51298/vmj.v527i1B.5734.
- Quan, N. K., & Taylor-Robinson, A. W. (2023). Vietnam’s evolving healthcare system: Notable successes and significant challenges. Cureus, 15(6), e40414.
- Reyes, E. B., Ha, J. W., Firdaus, I., Ghazi, A. M., Phrommintikul, A., Sim, D., Vu, Q. N., Siu, C. W., Yin, W. H., & Cowie, M. R. (2016). Heart failure across Asia: Same healthcare burden but differences in organization of care. International Journal of Cardiology, 223, 163–167. https://doi.org/10.1016/j.ijcard.2016.07.256
- Riewpaiboon, D. A. (2018). Hospital cost analysis in developing countries: A methodological comparison in Vietnam. Asian Journal of Pharmaceutics (AJP), 12(1), S8–S18. https://doi.org/10.22377/ajp.v12i01.2341.
- The State Bank of Vietnam. (2022). Exchange rate. Retrieved July 6, 2022, from https://www.sbv.gov.vn/TyGia/faces/TyGiaTrungTam.jspx?_afrLoop = 59041398703480224&_afrWindowMode = 0&_adf.ctrl-state = tmprikc3a_149
- Taylor, M. (2009). What is sensitivity analysis. Consortium YHE: University of York, 1–8.
- Thuy, T. T. N., Dong, C. T., & Hung, T. T. (2020). Analyze direct treatment cost of hospitalized case for heart failure from health insurance database in Vietnam in 2017–2018. Vietnam Medical Journal, 491(1), 93–96.
- Tumanan-Mendoza, B. A., Mendoza, V. L., Santos, A. A. A. B.-D., Punzalan, F. E. R., Pestano, N. S., Natividad, R. B., … Lam, H. Y. (2018). Economic burden of hospitalisation for congestive heart failure among adults in the Philippines. Heart Asia, 10(2), e011039. https://doi.org/10.1136/heartasia-2018-011039.
- Urbich, M., Globe, G., Pantiri, K., Heisen, M., Bennison, C., Wirtz, H. S., & Di Tanna, G. L. (2020). A systematic review of medical costs associated with heart failure in the USA (2014–2020). Pharmacoeconomics, 38(11), 1219–1236. https://doi.org/10.1007/s40273-020-00952-0
- Vietnam Social Insurance. (2019). Strive for 100% of the elderly covered by health insurance cards before 2020. Electronic Magazine of Social Insurance. Retrieved April 30, from https://tapchibaohiemxahoi.gov.vn/phan-dau-100-nguoi-cao-tuoi-co-the-bhyt-truoc-nam-2020-48762.html
- World Health Organization. (2019). International classification of diseases 10 version: 2019. Retrieved July 3, 2022, from https://icd.who.int/browse10/2019/en#/I30-I52
- World Health Organization. (2022). Cardiovascular diseases. Retrieved August 9, 2022, from https://www.who.int/health-topics/cardiovascular-diseases#tab = tab_1
- Yingchoncharoen, T., Wu, T.-C., Choi, D.-J., Ong, T. K., Liew, H. B., & Cho, M.-C. (2021). Economic burden of heart failure in Asian countries with different healthcare systems. Korean Circulation Journal, 51(8), 681–693. https://doi.org/10.4070/kcj.2021.0029
- Zannad, F. (2018). Rising incidence of heart failure demands action. The Lancet, 391(10120), 518–519. https://doi.org/10.1016/S0140-6736(17)32873-8
