Abstract
Bleomycin, an antibiotic agent with antitumour activity, is an important drug in the management of many oncological malignancies such as lymphoma and germ cell tumours. These tumours are potentially curable and mostly affect young people. The potential side effects and long-term toxicities should be considered. The major limitation of bleomycin therapy is pulmonary toxicity and may be life threatening in about 10% of cases. This article reports a case of an ovarian mixed germ cell tumour, which presented with bleomycin-associated pulmonary toxicity.
Introduction
Bleomycin, an antibiotic agent with antitumour activity, is an important drug in the management of many oncological malignancies such as lymphoma and germ cell tumours. These tumours are potentially curable and mostly affect young people. The potential side effects and long-term toxicities should be considered. The major limitation of bleomycin therapy is pulmonary toxicity and may be life threatening in about 10% of cases.Citation1–3 This article reports a case of an ovarian mixed germ cell tumour, who received bleomycin-containing chemotherapy and presented with bleomycin-associated pulmonary toxicity.
Ethics
The Human Research Ethics Committee (HREC) of Stellenbosch University approved the present report.
Case study
A 27-year-old woman, gravida 0, presented post-laparotomy for a right ovarian mass when a right ovarectomy and omentum biopsy was performed. Histology of the right ovary confirmed a mixed germ cell tumour consisting of dysgerminoma (70%), yolk sac tumour (25%) and immature teratoma (5%) that also involved the omentum. Systemic evaluation for metastases was negative and according to the International Federation of Gynecology and Obstetrics classification (FIGO) was staged as a FIGO stage IIIB nonseminomatous germ cell tumour and standard chemotherapy with the BEP regime (bleomycin 30 IU day 1, 8 and 15; etoposide 100 mg/m2 days 1 to 5, and cisplatin 20 mg/m2 days 1 to 5 every 3 weeks) was initiated. Pending her biomarker response, tolerability and toxicity, four to six cycles of BEP were planned.
Cycle 2 was delayed due to an episode of neutropenic sepsis; this resolved and Cycle 2 was completed. Again she was readmitted with neutropenic sepsis and signs of an acute renal injury syndrome (ARI). With a creatinine value of 284 µmol/l (49–90 µmol/l) and a creatinine clearance of 30.5 ml/min (Cockcroft–Gault formula), a nephrology consult and conservative management the renal output improved and possible proximal tubule damage was attributed to cisplatin administration and sepsis. Nephrology advised against any chemotherapy administration for at least a six-month period.
After extensive consultation with the patient and family she opted for an alternative, less nephrotoxic regime, carboplatin 300 mg/m2 on day 1, etoposide 135 mg/m2 on days 1 to day 3 and bleomycin 30 IU on day 1 (CEB) with granulocyte colony-stimulating factor (G-CSF) support from days 5 to 10, post-chemotherapy to maintain dose intensity in a potentially curable cancer. She completed three cycles of CEB. Bleomycin was administered on D1, D8 and D15 of cycle 1 and 2 but only on day 1 of cycles 3–5 due to the underlying concern regarding potential toxicity. The cumulative bleomycin dose was 270 mg, well within the maximum allowed lifetime amount of 400–450 mg.
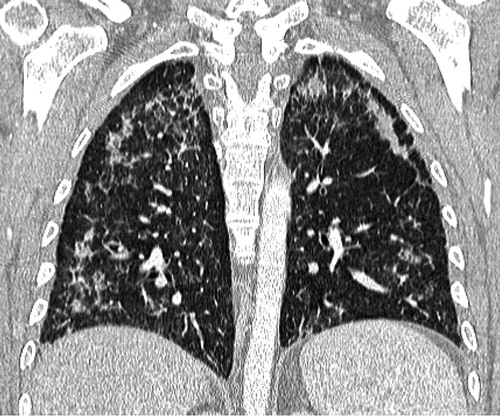
Initial preoperative biochemical markers included a raised alpha-fetoprotein (AFP) 19 016 μg/l (0.0–7.0 μg/l), human chorionic gonadotropin (HCG) 892 IU/l (< 5 IU/l) and lactate dehydrogenase (LDH) 4 741 U/l (100–190 U/l). At the onset of chemotherapy, the marker values decreased to AFP 733 μg/l, HCG 39 IU/l and LDH 275 U/l. Her biochemical markers normalised at cycle 3 (). At the completion of cycle 5 a lung-abdominopelvic computer tomography scan (CT scan) revealed no signs of metastatic disease in either the abdomen or chest but peripheral reticular changes in the lung fields and areas of airspace opacifications confirmed the radiological appearance of active interstitial fibrosis of both lungs (a).
Figure 1: Biochemical marker response. AFP = alpha-fetoprotein; HCG = human chorionic gonadotropin; LDH = lactate dehydrogenase.
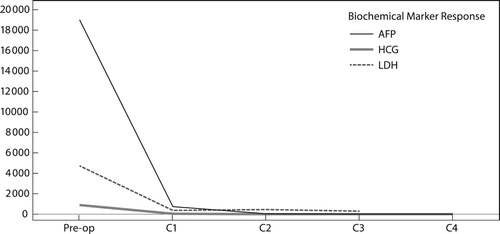
Figure 2: (a) Initial and (b) follow-up CT scan: upper lungs axial CT slices (lung windows): (a) There is intra- and inter-lobular septal thickening with associated ground-glass opacification and an incidental small-volume pneumomediastinum, the aetiology of which is not clear, possibly related to an air leak from the adjacent lung pathology. The lung changes are consistent with an NSIP pattern of lung injury or an organising pneumonia. (b) Interval progression is noted in terms of severity as well as area of the lung involved. There is now diffuse ground-glass opacification of the lungs as well as established fibrosis with regions of honeycombing. The large ground-glass component suggests an active cellular component to the disease and the radiological picture favours a mixed cellular fibrotic NSIP pattern of lung injury. The pneumomediastinum progressed and there is a left-sided pneumothorax.
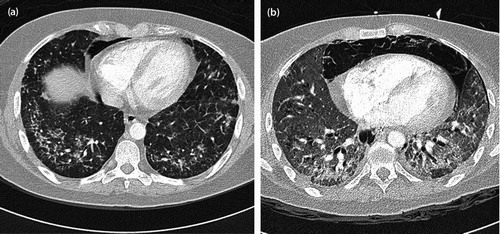
However, four weeks post-completion of chemotherapy she was admitted with signs and symptoms of severe anaemia – haemoglobin 4 gm/dl (12.0–15.0 gm/dl) – and associated increase in shortness of breath (SOB). Supportive care included a red blood cell transfusion, oxygen and prednisone, but progressive worsening in SOB with oxygen dependency necessitated intubation and a follow-up lung CT scan to exclude the possibility of a pulmonary embolism. The fibrotic changes in the lung had undergone progression and together with bilateral ground-glass opacification were consistent with a non-specific interstitial pneumonitis (NSIP) pattern of lung disease. A significant pneumomediastinum and left pneumothorax was observed and compared with the initial CT scan had progressed ( and ). No pulmonary emboli were demonstrated. A GeneXpert sputum test was negative for pulmonary tuberculosis as was an immune-fluorescent assay for Pneumocystis jirovecci.
Discussion
Ovarian germ cell neoplasms arise in women between the ages of 10 and 30 years, derived from primordial germ cells of the ovary, and may be either benign or malignant but account for only 5% of all malignant ovarian neoplasms. Ovarian mixed germ cell tumours consist of two or more types of germ cell neoplasms and often secrete tumour markers, such as alpha-fetoprotein (AFP), human chorionic gonadotropin (HCG), or lactate dehydrogenase (LDH).Citation4
The staging procedure for women with ovarian germ cell tumours is the same as for epithelial ovarian cancer. The majority of women undergo surgical cytoreduction before the start of chemotherapy and this is in direct contrast to testicular cancer, where surgery is reserved for residual masses post-chemotherapy. Post-surgery most women will receive adjuvant platinum-based chemotherapy with curative intent. Cisplatin-based chemotherapy for 3–6 cycles is considered the standard of care. Long-term cure rates are > 90% for early-stage and up to 80% for advanced disease.Citation4–7
Drugs may produce a variety of respiratory tract disorders. Pulmonary infiltrates with fibrosis may result from the use of cytotoxic drugs used in the treatment of cancer and the most common cause of these reactions is bleomycin. The mechanism for the development of bleomycin pulmonary-induced injury is not clear but appears to involve the induction of free radicals and cytokines that result in endothelial damage. Bleomycin directly activates alveolar macrophages that subsequently produce cytokines and free radicals resulting in fibroblast activation with accompanying deposits of collagen. Other components might include a deficiency in the bleomycin hydrolase enzyme and a possible genetic susceptibility.Citation2,Citation3
There is an increased risk of lung injury associated with the administration of > 400 mg of bleomycin, although injury can occur at doses as low as 50 mg. The risk appears higher in the older patient (> 40 years) and in patients with renal insufficiency. These patients should be spared exposure to bleomycin unless equally effective alternative regimens are not available. Thoracic irradiation and concurrent high-dose cisplatin administration increase the risk of bleomycin lung toxicity and in animal studies concomitant administration of granulocyte colony-stimulating factor (G-CSF) was identified as a possible risk factor for bleomycin-induced lung injury.Citation1–3
Clinical manifestations occur between one and six months post-bleomycin administration, but even occur during the administration of bleomycin. Symptoms and signs include a non-productive cough, dyspnoea, pleuritic or substernal chest pain, fever, tachypnoea, lung restriction and hypoxemia. The use of pulmonary function tests (PFTs), particularly the diffusing capacity of the lung for carbon monoxide (DLCO) to screen for evidence of pulmonary toxicity, has been controversial. The assessment of PFTs, including spirometry and a DLCO, at baseline and prior to each new treatment cycle is recommended for most patients with germ cell tumours who receive a bleomycin-containing regimen. It is recommended to discontinue bleomycin therapy if an asymptomatic ≥ 25% decrease in the DLCO is observed. Routine chest radiographs in asymptomatic people are not recommended.Citation2,Citation3,Citation8
Four types of lung toxicity are associated with the administration of bleomycin: (1) subacute progressive pulmonary fibrosis, (2) hypersensitivity pneumonitis, (3) organising pneumonia, and (4) an acute chest pain syndrome that can occur during rapid infusion. The classic chest radiological pattern of bleomycin-induced fibrosis includes bibasilar sub-pleural opacities with volume loss and blunting of the costophrenic angles; however, fine nodular densities may be seen. Honeycombing may develop as fibrosis progresses. Pneumomediastinum and pneumothorax might be rare complications of bleomycin-related lung fibrosis.Citation2,Citation3,Citation9–11 The differential diagnosis includes infection, venous thromboembolism and, depending on age, assessment for cardiac failure or a myocardial infarction and pulmonary hypertension, metastatic disease and radiation-induced lung fibrosis should be undertaken. Management of suspected bleomycin lung-induced toxicity includes discontinuation of bleomycin therapy and for symptomatic patients a trial course of prednisone is recommended for 4–6 weeks; if there is a response to this, then the prednisone dose should gradually be tapered.Citation2,Citation3,Citation12,Citation13
During the management of this case, we observed several treatment-related complications and toxicities that required urgent medical intervention: the patient experienced neutropenic sepsis on two occasions that was treated and prevented in successive cycles by the administration of prophylactic G-CSF. She developed a severe acute renal injury syndrome (creatinine clearance of 30 ml/min) secondary to sepsis and cisplatin administration and was managed with conservative treatment. A nephrology consult suggested a six-month ban on further chemotherapy administration but dealing with a curable disease made for serious ethical consideration and discussion with both the patient and her family. When she presented with severe anaemia (Hb 4 gm/dl), the lung injury was diagnosed on clinical symptoms that she experienced and the radiological signs that confirmed the lung fibrosis (diffuse ground-glass opacification of both lungs as well as established fibrosis with regions of honeycombing). She also experienced the rare complication of a pneumothorax and pneumomediastinum as a result of the related lung fibrosis.
Eventually, our patient was admitted into the high care facility and managed on a respirator, as she was unable to maintain her oxygen saturation levels. The outcome was dismal when she decompensated and developed an asystole.
Conclusion
Ovarian germ cell tumours generally have a good prognosis and even in advanced disease almost 80% of patients will have long-term survival. The chemotherapy regimens used to treat these tumours are platinum based and BEP is the recommended standard of care. However, these drugs are not without short- and long-term toxicities and, although rare, the consequences can be fatal. Here we described a case that experienced fatal bleomycin-induced pulmonary fibrosis. The practical approach to prevent bleomycin-induced lung toxicity is to perform routine PFTs in patients with germ cell tumours undergoing a bleomycin-containing regime.
Competing interests
The authors declare no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors’ contributions – PB was the project leader and responsible for the design, concept and preparation of the manuscript. SG made conceptual contributions and was involved in the manuscript preparation and final editing.
ORCID
P Barhardt http://orcid.org/0000-0002-3888-0571
S Griffith-Richards http://orcid.org/0000-0002-7031-8108
Additional information
Funding
References
- O’Sullivan JM, Huddart RA, Norman AR, et al. Predicting the risk of bleomycin lung toxicity in patients with germ-cell tumours. Ann Oncol. 2003;14:91–96. doi:10.1093/annonc/mdg020.
- Reinert T, Baldotto CS, Nunes FAP, et al. Bleomycin-Induced Lung Injury. J Can Research. 2013;1–7. doi:10.1155/2013/480608.
- Sleiifer S. Bleomycin-Induced Pneumonitis. Chest. 2001;120(2):617–624. doi:10.1378/chest.120.2.617.
- Simone CG, Markham MJ, Dizon DS. Chemotherapy in ovarian germ cell tumours: a systematic review. Gynecol Oncol. 2016;17(8):44. doi:10.1007/s11864-016-0416-2.
- Bafna UD, Umadevi K, Kumaran C, et al. Germ cell tumours of the ovary: Is there a role for aggressive cytoreductive surgery for nondysgerminomatous tumours? Int J Gynecol Cancer. 2001;11:300–304. doi: 10.1046/j.1525-1438.2001.011004300.x
- Murugaesu N, Schmid P, Dancey G, et al. Malignant ovarian germ cell tumours: identification of novel prognostic markers and long-term outcome after multimodality treatment. J Clin Oncol. 2006;24:4862–4866. doi:10.1200/JCO.2006.06.2489.
- Hurteau JA, Febbraro T. Germ cell tumours: treatment consensus across all age groups through MAGIC [Malignant Germ Cell International Collaborative]. Cancer 2016;122(2):181–183. doi:10.1002/cncr.29729.
- Lauritsen J, Kier MG, Bandak M, et al. Pulmonary function in patients with germ cell cancer treated with bleomycin, etoposide, and cisplatin. J Clin Oncol. 2016;34:1492–1499. doi:10.1200/JCO.2015.64.8451.
- Sikar T, Macvicar D, Husband JE. Pneumomediastinum complicating bleomycin related lung damage. Br J Radiol. 1998;71:1202–1204. doi: 10.1259/bjr.71.851.10434917
- Kuhlman JE. The role of chest computed tomography in the diagnosis of drug-related reactions. J Thorac Imaging. 1991; 6(1): 52–61. doi: 10.1097/00005382-199101000-00008
- Mills P, Husband JE. Computed tomography of pulmonary bleomycin toxicity. Semin Ultrasound CT MR. 1990;11(5):417–422.
- Maher J, Daly PA. Severe bleomycin lung toxicity: reversal with high dose corticosteroids. Thorax 1993;48:92–94. doi:10.1136/thx.48.1.92.
- Kozielski J. Reversal of bleomycin toxicity with corticosteroids. Thorax 1994: 49(2):290. doi: 10.1136/thx.49.3.290-a