Abstract
Introduction: Typhoid ileal perforation is a very serious complication of typhoid fever and remains a significant surgical problem in developing countries like Nigeria, where it is associated with higher mortality and morbidity, due to lack of adequate clean drinking water, poor sanitation and lack of access to health facilities in remote areas and delays in hospital presentation.
Materials and methods: This was a retrospective study; all patients treated for typhoid ileal perforation at the centre in the period from January to December 2016 were included.
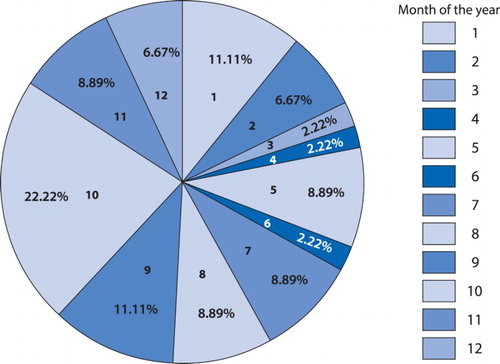
Results: There were 22 (59.5%) males and 15 (40.5%) females, with a male to female ratio of 1.5: 1. The ages ranged from 5 to 49 years with mean of 16.5± 9.2 years. The month of October recorded the highest cases of typhoid ileal perforation. Abdominal pain, anorexia, fever and abdominal swelling were the most common symptoms reported by the subjects. The number of ileal perforations was from 1 to 7 with mean of 2.0 ± 1.3; however, the majority had a single perforation. In addition, excision and simple closure was the most common surgery performed in these cases. Operation site infection was the most common complication in this study. Furthermore, the majority of cases were successfully discharged while eight deaths were recorded.
Conclusion: Typhoid ileal perforation was most common among males; abdominal pain, swelling and fever were common findings; single site perforation was the most common intra-operative findings and excision and simple closure was the most common operative procedure. Therefore early presentation, adequate resuscitation and lower number of ileal perforations are associated with better prognosis.
Introduction
Typhoid fever, a severe febrile illness caused primarily by the gram-negative bacillus Salmonella typhi, has continued to be a public health problem in many developing countries.Citation1 Typhoid infection is generally transmitted by faeco-oral route and may occasionally lead to an epidemic, particularly in areas with poor sanitation and limited availability of clean, potable water.Citation2
Intestinal perforation is a common cause of peritonitis necessitating emergency surgical intervention. Perforation of the bowel is a serious abdominal complication of typhoid fever. Although intestinal haemorrhage is the most common complication of typhoid fever, ileal perforation continues to be the most frequent cause of its high morbidity and mortality.Citation3 Despite global scientific development typhoid fever and its complications continue to be a great health problem, especially in developing countries.Citation4 It is a global health problem that can have a devastating impact on the resources of poor countries and it is estimated that more than 33 million cases of typhoid fever occur annually causing more than 500,000 deaths.Citation2,Citation5
Regions of the world like West Africa, lacking clean and potable water supplies and with inadequate waste-disposal systems, have a high incidence of typhoid fever. One of the most fatal complications of typhoid fever is ileal perforation.Citation6 In the West African environment the incidence of typhoid ileal perforation varies from 15% to 33%.Citation7 This complication was almost invariably fatal, but with the availability of potent broad-spectrum antibiotics, improved methods of resuscitation, and modern and safe anaesthesia, surgery is now routinely used to manage ileal perforation and offers the best hope of survival.Citation6
Ileal perforation is a very serious complication of typhoid fever and remains a significant surgical problem in developing countries like Nigeria, where it is associated with higher morbidity and mortality, due to lack of adequate clean drinking water, poor sanitation and lack of access to health facilities in remote areas and delay in hospital presentation.Citation8 The rates of perforation have been reported in the literature to vary between 0.8% and 18%.Citation9–11 The high incidence of perforation in most developing countries has been attributed to late diagnosis and the emergence of multi-drug resistant and virulent strains of Salmonella typhi.Citation11 The disease affects mostly young adults who contribute enormously to the economy of third world countries.Citation12 It also affects children and it is most common in people in the low socio-economic strata.Citation11
The incidence and endemicity of typhoid fever is not known in all the local regions of Nigeria due to a poor infectious disease database and the poor health-seeking attitudes of the people, who may prefer to patronise unorthodox practitioners with resultant low usage of orthodox medical healthcare facilities. The prevalence of typhoid ileal perforation, which cannot be managed at the primary and secondary healthcare facilities or by unorthodox means, may be accepted as a reflection of the endemicity of the disease in a locality.Citation13
The preoperative management of typhoid ileal perforation is very important. Aggressive but not rapid correction of dehydration was the policy adopted. Urethral catheters were always passed to monitor urine output, since most patients were dehydrated and had impaired renal function. Electrolyte replacement, mainly potassium, was done only when there was urine output of at least 30 ml/min. Nasogastric tubes were always passed to decompress the bowel and prevent aspiration. Patients had surgery as soon as they were adequately resuscitated (correction of dehydration, good urine output, normal urea and electrolytes).Citation14
Immediate surgery is accepted as definitive treatment. Various operative procedures are:
simple closure of the perforation;
resection and anastomosis;
ileostomy.
Postoperative complications of typhoid ileal perforation include wound infection, wound dehiscence, faecal fistula, peritonitis, septicaemia, ileostomy-related complications and intestinal obstruction.Citation15 Among all the postoperative complications faecal fistula is associated with significant morbidity and mortality.
Aim of the study
To provide an overview of the spectrum of typhoid ileal perforation cases and their outcome that were managed in a semi-urban tertiary care hospital in Nguru, Yobe State, north-east Nigeria.
Definition of terms
Fever was defined as axillary temperature of ≥ 37.5°C.Citation16
Bradycardia was defined as pulse rate of less than 60/min while tachycardia was pulse rate greater than 100/min in adults,Citation17 while age-specific ranges were used for childrenCitation18
Tachypnoea was respiratory rate greater than 25/min in adults,Citation19 while age-specific ranges were used for children.Citation20
Materials and methods
The Federal Medical Centre is a tertiary hospital located in Nguru Local Government Area. Nguru is a Local Government Area in Yobe State, in the north-eastern geopolitical zone of Nigeria. Its headquarters is in the town of Nguru near the Hadejia River at 12°52′45″ N 10°27′09″ E. It has an area of 916 km² and a population of 150 632 according to the 2006 census.Citation21 It serves as a referral hospital to neighbouring local government areas of Yobe, Jigawa states and border towns of the Niger Republic.
This retrospective study was based on hospital records of all patients admitted with the diagnosis and treatment for typhoid ileal perforation at the centre in the period from January 2016 to December 2016. Case notes and folders of all patients with the diagnosis of typhoid ileal perforation were retrieved from hospital entry points such as the Accident and Emergency Unit (A&E) and Emergency Paediatric Unit (EPU), and surgical wards and records from the operating theatre. The total number of surgical admissions and surgical operations performed during the period under review were also obtained from the hospital records.
All relevant information was retrieved from the patient record; this included the socio-demographic characteristics, clinical history on admission, admission–operation time, number of perforations, type of ileal repair, outcome of surgery, preoperative mortality, postoperative complications. Other information obtained from the records was the total number of general surgical/paediatric surgeries during the period under review.
Ethical considerations
Ethical approval was obtained from the Medical Research Ethics Committee of the Federal Medical Centre, Nguru Yobe State. Confidentiality was ensured by not writing the names of patients on questionnaires.
Data analysis
Data obtained from the case notes were entered and analysed using the Statistical Package for the Social Sciences® version 20 (IBM Corp, Armonk, NY, USA). Absolute numbers and simple percentages were used to describe categorical variables. Similarly, quantitative variables were described using measures of central tendency mean and measures of dispersion such as range or standard deviation as appropriate. Fisher’s exact test was used in assessing the significance of associations between categorical groups. A p-value < 0.05 was considered statistically significant.
Results
A total of 471 surgeries were done during the period under review. Forty-six of these were for typhoid ileal perforation (9.8%); however, nine were excluded in most of the analysis due to incomplete data. Therefore there were 22 (59.5%) males and 15 (40.5%) females, with a male to female ratio of 1.5: 1. Thirty (81.1%) of the cases were single while seven (18.9%) were married; five (13.5%) were Kanuris, 16 (43.2%) were Hausas, 11 (29.7%) were Fulanis, while five (13.5%) were from the minority tribes.
The ages ranged from 5 to 49 years with a mean of 16.5± 9.2 years. Most of the cases were in the paediatric age group 10–19 years (43.2%); the majority had no formal education (43.2%) while 51.3% were still at school at the time of the illness (). Thirty-five (94.6%) of them earned less than 150 Naira per day; only two (5.4%) earned more than 150 Naira per day. Twenty-seven (73.0%) of the cases were self-referrals while 10 (27%) were referred from other health facilities. Similarly, 27 (73.0%) had used orthodox medications before presentation to a health facility, while 10 (27.0%) had used traditional medications. Most cases (24, 64.9%) were admitted through the Accident and Emergency Department, whereas 13 (35.1%) cases were admitted through the Emergency Paediatric Unit.
Table 1: Sociodemographic characteristic of subjects with typhoid ileal perforation
Abdominal pain, anorexia, fever and abdominal swelling were the most common symptoms reported by the subjects. Common signs elicited were abnormality in the pulses, among these 26 (78.8%) had tachycardia while 7 (21.2%) had bradycardia. Tachypnoea was the next most common abnormal sign elicited, while jaundice and hepatomegaly were the least () reported.
Table 2: Common symptoms and signs associated with typhoid ileal perforation reported by the subjects
The majority of cases had fever for between 6 and 10 days before presentation; the duration of illness before admission was from 4 days to 36 days with a mean of 12.1 ± 7.0. The duration of admission ranged from 1 to 38 days with a mean of 14.7 days ± 9.0 days; most were ill for between 1 and 2 weeks (59.5%) and the majority spent more than 2 weeks (43.3%) in hospital following admission ().
Table 3: Duration of fever, illness before presentation and total duration of admission of cases with typhoid ileal perforation
Four (10.8%) cases did not have surgery; however, among the 33 cases that were operated on, most had surgery with 13–24 hours (51.5%) of admission; the number of perforations was from 1 to 7 with a mean of 2.0 ± 1.3. The majority had a single perforation, and the distance between perforation site to the ileo-caecal valves ranged between 6 and 42 cm with a mean of 16.8 ± 8.0 cm; most perforations were closer to the ileo-caecal valves (5–10 cm, 30.3%). In addition, excision and simple closure was the most common surgery performed in these cases ().
Table 4. Time lapse before surgery and intraoperative findings observed in cases with typhoid ileal perforation
Operation site infection was the most common complication observed in this study, while enterocutaneous fistula and septic shock were the least common; furthermore, the majority of cases were successfully discharged but eight deaths were recorded (). Among the deaths, four (50%) occurred before surgery and four (50%) died post-operatively; two (50%) of the cases had wedge resection while each had excision and simple closure (25%) and ileal resection (25%) respectively. The interval between operation and death ranged from one day to five days with a mean of 2.8 ± 2.1.
Table 5: Postoperative complications and outcome of cases
shows that the majority of cases irrespective of the duration of illness before presentation, their use of any medication or number of perforations observed intra-operation were successfully discharged; however, these observations was not statistically significant (Fisher’s exact test = 4.581, p = 0.390; Fisher’s exact test = 1.088, p = 0.75; and Fisher’s exact test = 10.305, p = 0.077, respectively).
Table 6: Comparing the outcome with: the duration of illness; use and type of medication before presentation; and number of perforations
shows the distribution of cases of typhoid perforation according to months The month of October recorded the highest number of cases of typhoid perforation.
Discussion
Enteric fever remains a scourge in most developing countries; this is attributable to the limited availability of potable water supply, poor personal hygiene and food handling, and indiscriminate disposal of human waste, all of which form a formidable cocktail for transmission of the infective agent Salmonella enterica var Typhi. Therefore poverty and low socioeconomic status are common associated factors. About 95% of the cases in this study lacked significant earnings; this could influence their health-seeking behaviours, especially in a setting without social security, hence they may prefer patronising drug vendors and unorthodox traditional healers who are thought to be cheaper. This was observed in this study because all the cases had started unsuccessful self-medication (orthodox and traditional) before presentation. This attitude may result in heightened complications and increased mortality.
Our study showed a male preponderance of ileal perforation; this observation was similar to previous reports by Beniwal et al.Citation22 and Ugochukwu et al.Citation6 but this was at variance with the report of Edino et al.Citation7 who reported more female predominance. The reason for this difference is not completely understood but Beniwal et al.Citation22 reported that males are more exposed to risk and genetic predisposition also heightens the risk of infection. Again, the majority of the cases were within the paediatric age range (first and second decade of life); this was similarly reported by Ugochukwu et al.Citation6 Edino et al.Citation7 and Ahmed et al.Citation23
The month of October witnessed the highest caseload of typhoid ileal perforation in our study; this observation was comparable to those of Ugochukwu et al.Citation6 Gupta et al.Citation24 and Anyanwu et al.Citation25 but it differed from that of Ugwu et al.Citation11 who documented more cases between November and March.
Abdominal pain and swelling, fever, anorexia, and nausea and vomiting were common complaints reported in this study; this was similar to those of Ugochukwu et al.Citation6 and Gupta et al.Citation24 but Gupta et al.Citation24 also reported diarrhoea in 75% of their cases, while only 21.6% of our cases had diarrhoea. The disparity may be because their study involved only children, while adults were also included in our study; this was similar to the findings of Channh et al.Citation26 who also reported 25% of cases with diarrhoea; similarly, fewer cases of headache, jaundice, hepatomegaly and splenomegaly were observed in their study.
Typhoid ileal perforation occurs by the end of the second week or early in the third week,Citation9 but in developing countries with greater disease burden it tends to occur earlier in the second week of illness; Chalya et al.Citation27 suggested depressed immunity, virulent isolates different from those from developed countries, hypersensitivity to Peyer’s patches due to reported infection and ileal bacteria burden as possible reasons for this difference. The majority of the cases in our study presented within the second week of illness, which corresponded to the timing of ileal perforation reported in other studies.Citation6,Citation7,Citation24 Most cases spent more than two weeks in hospital following admission, with a mean duration of 14.7 days. This observation was similar to that of Edino et al.Citation7 who reported a mean of 16.1 days, and that of Mogasale et al.Citation28 who reported a mean of 18.4 days. However, this was shorter than the 21.56 days reported by Shrivastava et al.Citation29 This disparity could be because most of their cases had postoperative complications requiring longer hospital stay.
Surgery remains the mainstay of treatment for typhoid ileal perforation; however, this will require efficient resuscitation and correction of deficits such as electrolyte derangements and shock before surgery. Early surgery may determine the outcome, especially following effective resuscitation. About 52% of our cases were operated on within 13–24 hours post-admission. Gupta et al.Citation24 reported that early surgical intervention improves the prognosis. The choice of surgical technique is influenced by the severity of illness such as the number of perforations and the expertise of the surgeon. In our study, excision and simple closure was the most common procedure done; this observation was similar to that of Ugochukwu et al.Citation6 Edino et al.Citation7 This procedure is easy and less time-consuming, though the risk of postoperative fistula is higher;Citation29 however, we reported only a single case (5.6%). The number of perforations in our study ranged from one to seven, which was similar to the one to eight reported by Anyanwu et al.Citation25 Single perforation was the most common intraoperative observation in our study; this was similar to other reports.Citation6,Citation7,Citation25,Citation27,Citation30
The mortality rate of typhoid ileal perforation ranged from 9% to 43%;Citation31 22% mortality was recorded in this study; this figure was similar to those of Adesunkanmi and AjaoCitation31 but higher than those of Edino et al.Citation7 and the 10.9% reported by Anyanwu et al.Citation25 Easy access to health facilities and late presentation to hospital might have contributed to this disparity. Our study involved predominantly a rural population with a limited health infrastructure; some patients had to travel for days before accessing a secondary or tertiary healthcare facility.
Conclusion
Typhoid ileal perforation is still a disease of great public health concern; early surgical intervention remains the mainstay of treatment. Though single perforation was most commonly observed, the high mortality rate observed in this study might be related to late presentation to the health facility because 50% of the deaths occurred preoperatively. Therefore early presentation, adequate resuscitation and lower number of ileal perforations are associated with a better prognosis. The choice of surgical technique in our protocol was dependent on the severity of the typhoid ileal perforation and morbidity, therefore simple surgical excision was chosen in most cases because most had fewer perforations.
Recommendations
Prevention is the key to eliminating typhoid ileal perforation. Our observation in this study calls for a concerted effort through advocacy by engaging policy-makers to make potable water available; ensuring easy accessibility by rural dwellers; similarly proper disposal of human waste through provision of toilets, and prohibition of open defecation should be enforced; however, improving public awareness through enlightenment on the risk factors for typhoid ileal perforation and its complications and the hazards associated with indiscriminate self-medication and patronising unorthodox healers should be done routinely. Furthermore, the surgical expertise for managing typhoid ileal perforation should also be available in secondary healthcare facilities; this will reduce the time spent before accessing quality care.
ORCID
BA Grema http://orcid.org/0000-0002-2316-6455
I Aliyu http://orcid.org/0000-0003-0018-1828
GC Michael http://orcid.org/0000-0003-4008-4483
A Musa http://orcid.org/0000-0002-5172-6405
BM Abubakar http://orcid.org/0000-0001-6965-0325
References
- Crum NF. Current trends in typhoid fever. Current Gastroenterol Rep. 2003;5:279–86. doi: 10.1007/s11894-003-0064-0
- Ukwenya AY, Ahmed A, Garba ES. Progress in management of typhoid perforation. Ann Afr Med. 2011;10:259–65. doi: 10.4103/1596-3519.87040
- Sumer A, Kemik O, Dulger AC, Olmez A, Hasirci I, Kisli E, et al. Outcome of surgical treatment of intestinal perforation in typhoid fever. World J Gastroenterol. 2010;16:4164–8. doi: 10.3748/wjg.v16.i33.4164
- Sharma AK, Sharma RK, Sharma SK, Sharma A, Soni D. Typhoid Intestinal Perforation: 24 Perforations in One Patient. Ann Med Health Sci Res. 2013;3(Suppl 1):S41–S43. doi: 10.4103/2141-9248.121220
- Perera N, Geary C, Wiselka M, Rajakumar K, Andrew SR. Mixed Salmonella infection: case report and review of the literature. J Travel Med. 2007;14:134–5. doi: 10.1111/j.1708-8305.2007.00111.x
- Ugochukwu AI, Amub OC, Nzegwu MA. Ileal perforation due to typhoid fever – review of operative management and outcome in an urban centre in Nigeria. International Journal of Surgery. 2013;11:218–22. doi: 10.1016/j.ijsu.2013.01.014
- Edino ST, Yakubu AA, Mohammed AZ, Abubakar IS. Prognostic factors in typhoid ileal perforation, a prospective study of 53 cases. J Natl Med Assoc. 2007;99:1042–5.
- Bhutta ZA. Current concepts in the diagnosis and treatment of typhoid fever. Br Med J. 2006;333:78–82. doi: 10.1136/bmj.333.7558.78
- Atamanalp SS, Aydinli B, Ozturk G, Oren D, Basoglu M, Yildirgan MI. Typhoid intestinal perforations: twenty-six year experience. World J Surg. 2007;31:1883–8. doi: 10.1007/s00268-007-9141-0
- Otegbayo JA, Daramola OO, Onyegbatulem HC, Balogun WF, Oguntoye OO. Retrospective analysis of typhoid fever in a tropical tertiary health facility. Trop Gastroenterol. 2002;23:9–12.
- Ugwu BT, Yiltok SJ, Kidmas AT, Opalawa AS. Typhoid intestinal perforation in North Central Nigeria. West Afr J Med. 2005;24:1–6.
- Saxe JM, Crospey R. Is operative management effective in treatment of perforated typhoid? Am J Surg. 2005;189:342–4. doi: 10.1016/j.amjsurg.2004.11.032
- Osifo OD, Ogiemwonyi SO. Typhoid ileal perforation in children in Benin city. Afr J Paediatr Surg. 2010;7:96–100. doi: 10.4103/0189-6725.62843
- Archampong EQ, Tandoh JFK, Nwako FA, et al. Small and large intestines (including rectum and anus). In: Badoe EA, Archampong EQ, da Rocha-Afodu JT, editors. Principles and practice of surgery including pathology in the tropics. 3rd edn. Accra: UGMS, 2000. p. 603–84.
- Zarappa S, Suggaiah L, Vamangiri S, Shankarappa U, Raj P, Krishnarajesh RC, et al. Typhoid ileal perforation-a retrospective study. J Evolution Med Dent Sci. 2016;5:229–32. doi: 10.14260/jemds/2016/49
- Elechi HA, Rabasa AI, Muhammad FB, Garba MA, Abubakar GF, Umoru MA. Prevalence and pattern of malaria parasitaemia among under-five febrile children attending Paediatric out-patient clinic at university of Maiduguri teaching hospital, Maiduguri. Niger J Paed. 2015;42:319–24. doi: 10.4314/njp.v42i4.7
- Spodick DH, Raju P, Bishop RL, Rifkin RD. Operational definition of normal sinus heart rate. Am J Cardiol. 1992;69:1245–6. doi: 10.1016/0002-9149(92)90947-W
- Hanash CR, Crosson JE. Emergency diagnosis and management of pediatric arrhythmias. J Emerg Trauma Shock. 2010;3:251–60. doi: 10.4103/0974-2700.66525
- Ray P, Birolleau S, Lefort Y, Becquemin MH, Beigelman C, Isnard R, et al. Acute respiratory failure in the elderly: etiology, emergency diagnosis and prognosis. Crit Care. 2006;10(3):R82. [ cited 2015 January 20]. Available from: https://www.ncbi.nlm.nih.gov/pubmed?term=16723034
- Shann F. WHO definition of tachypnoea in children. Lancet. 1992; 339:176–7. doi: 10.1016/0140-6736(92)90237-W
- Report of Nigeria’s National Population Commission on the 2006 Census Population and Development Review 2007;33:206–10.
- Beniwal US, Jindal D, Sharma J, et al. Comparative study of operative procedures in typhoid perforation. Indian J Surg. 2003;65:172–7.
- Amed HN, Niaz MP, Amin MA, khan MH, Parhar AB. Typhoid perforation still a common problem: situation in Pakistan in comparison to other countries of low human development. J Pak Med Assoc. 2006;56:230e2.
- Gupta V, Gupta SK, Shuklal VK, Gupta S. Perforated typhoid enteritis in children. Postgrad Med J. 1994;70:19–22. doi: 10.1136/pgmj.70.819.19
- Anyanwu L-J, Mohammed A, Abdullahi L, Farinyaro A, Obaro S. Determinants of postoperative morbidity and mortality in children managed for typhoid intestinal perforation in Kano Nigeria. J Pediatr Surg. 2017 (article in press). [cited 2018 March 16]. Available from: https://doi.org/10.1016/j.jpedsurg.2017.11.058
- Chanh NQ, Everest P, Khoa TT, House D, Murch S, Parry C, et al. A clinical, microbiological, and pathological study of intestinal perforation associated with typhoid fever. Clin Infect Dis. 2004;39:61–7.
- Chalya PL, Mabula JB, Koy M, Kataraihya JB, Jaka H, Mshana SE. Typhoid intestinal perforations at a University teaching hospital in Northwestern Tanzania: a surgical experience of 104 cases in a resource-limited setting. World J Emerg Surg. 2012;7:4. http://www.wjes.org/content/7/1/4 doi: 10.1186/1749-7922-7-4
- Mogasale V, Desai SN, Mogasale VV, Park JK, Ochiai RL, et al. Case fatality rate and length of hospital stay among patients with typhoid intestinal perforation in developing countries: a systematic literature review. PLoS ONE. 2014;9:e93784. doi: 10.1371/journal.pone.0093784
- Shrivastava D, Kumar JA, Pankaj G, Bala SD, Sewak VR. Typhoid intestinal perforation in Central India – a surgical experience of 155 cases in resource limited setting. IJBAR. 2014;5:600–4.
- Nuhu A, Gali B, Dawha S. Postoperative complications of typhoid ileal perforation in children in Azare, Nigeria. Int J Surg. 2008;21(1). [ cited 2018 March 16]. Available from: https://print.ispub.com/api/0/ispub-article/9305
- Adesunkanmi ARK, Ajao OG. Prognostic factors in typhoid ileal perforation: a prospective study in 50 patients. J R Coll Surg Edinb. 1997;42:395–399.