Abstract
Background: South Africa has 7.06 million people who are HIV-positive, with those having a low CD4 count being susceptible to cryptococcal meningitis (CCM), which has an estimated mortality of 30–50%. This study aimed to establish the outcome of patients admitted with CCM to a regional hospital in Durban between June 2015 and May 2016, and the extent to which the National Department of Health (NDoH) protocol was adhered to in managing their condition.
Method: This retrospective observational descriptive study reviewed the records of patients ≥ 12 years old admitted with CCM between June 2015 and May 2016, from which their demographic and medical data were extracted.
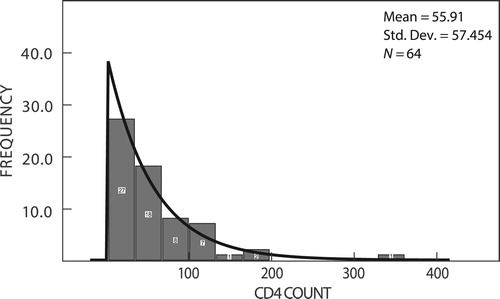
Results: Seventy-six complete records were found of which 49 were men and 27 were women. The average CD4 count was 55.9 cells/mm3, 85.5% were treated with intravenous amphotericin B and high-dose oral fluconazole, 6.7% received only amphotericin B and 5.2% received only fluconazole. There was an in-hospital mortality of 31.6%, and the NDoH protocol was adhered to in 72.4% (55/76) of patients. There was, however, no significant difference in outcome between those who were and were not managed as per the protocol (p = 0.177).
Discussion and conclusion: In-hospital mortality for CCM continues to be significant despite high rates of adherence to the NDoH protocol in the majority of patients. For this to be addressed, early diagnosis of HIV and initiation of ART to prevent the profound immunosuppression is essential.
Keywords::
Introduction
By the end of 2016, 36.7 million people were living with HIV/AIDS worldwide, of whom almost 52% (19 million) resided in sub-Saharan Africa (SSA).Citation1,Citation2 South Africa (SA) has the largest HIV epidemic in the world, with an estimated 7.06 million people who are HIV-positive (+ve)Citation3 and a national HIV prevalence rate of approximately 12.6%.Citation3 KwaZulu-Natal province, with the country’s second highest population, is the epicentre of the South African HIV epidemic. HIV preventative programmes and the extensive roll-out of antiretroviral therapy (ART) has resulted in a decrease in the rate of new HIV infections in SA, down from 3.4 million in 2001 to 960 000 in 2015,Citation1,Citation2 and a reduction in the number of patients presenting with Kaposi’s sarcoma and other Stage 4 AIDS-defining conditions.Citation4 However, among HIV + ve patients with a low CD4 count, cryptococcal meningitis (CCM) continues to have a significant mortality, estimated at between 30% and 50% of all patients admitted with CCM.Citation5–7
A number of strategies have been introduced in SA that could have an impact on the mortality associated with CCM. These include the UNAIDS 90–90–90 initiativeCitation8 (90% of the population to know their status, 90% of those who are HIV + ve to be on treatment and 90% of those on treatment to be virally suppressed by 2020); proactively screening all patients with a CD4 count ≤ 100 cells/mm3 for cryptococcal antigens (CrAg); carefully assessing those who are CrAg + ve for CCM; and adding high-dose fluconazole to the treatment regimen for patients admitted with CCM.
The UNAIDS 90–90–90 strategy promotes proactive HIV testing in facilities, while in communities, community campaigns and public awareness about the importance of testing and knowing one’s status are supplemented by healthcare provider initiated testing.Citation8 It was anticipated that an aggressive proactive strategy to ensure that everyone was aware of their HIV status would lead to a diagnosis prior to the onset of symptoms for many people. This would enable those who were diagnosed with HIV to start treatment at a higher CD4 count, which would make them less susceptible to opportunistic infections (OIs), such as CCM. With the target of 90% of those who are HIV + ve being on antiretroviral treatment (ART), it was anticipated that their immune status would improve, which would help to prevent OIs such as CCM, and that having 90% virally suppressed would allow for immune recovery and prevention of OIs. The 90–90–90 strategy has shown promising progress in SA, with 86% of the population being aware of their HIV status by mid-2015, and 56% of those who were HIV + ve being on ARTs, of whom 45% were virally suppressed.Citation9 Despite these national figures, a recent study from Prince Mshiyeni Memorial hospital (PMMH) in Durban, KwaZulu-Natal province, reported that between June 2015 and May 2016, 3702 HIV + ve patients (age between 12 and 86 years) with a CD4 count ≤ 100 cells/mm3 (range 1–100 cells/mm3) presented for care at its referral clinics. These figures suggest that there is still a long way to go in Durban in the early identification of patients who are HIV infected.Citation10
In 2015, the National Department of Health (NDoH) introduced a screening programme for all patients with a CD4 ≤ 100 cell/mm3 and updated the national protocol on managing patients admitted with CCM,Citation11 based on WHO recommendations.Citation12,Citation13 The protocol stipulates that all HIV + ve patients with a CD4 ≤ 100 cells/mm3 must be proactively screened for CrAgs, and those who are Cr Ag + ve must be carefully assessed for signs and symptoms suggestive of CCM. In keeping with the protocol, those with such signs and/or symptoms must have a lumbar puncture (LP) to facilitate early diagnosis and management of CCM, which would hopefully reduce the associated mortality. Those HIV + ve patients with a CD4 ≤ 100 cells/mm3 who are CrAg + ve, but who have no signs or symptoms suggestive of CCM, must be started on oral fluconazole for the primary prevention of CCM.
Concerning the early detection of CCM by screening HIV + ve patients with CD4 counts ≤100 cells/mm3, the results have been mixed. A 2014 study in Gauteng province reported that 41% (99/244) of patients who were CrAg + ve were symptomatic, of whom 57% (56) had an LP and 59% (33/56) were diagnosed with CCM.Citation14 However, a study at PMMH in 2016 reported that only 5.1% (190/3702) of HIV + ve patients seen between June 2015 and May 2016 with a CD4 count ≤ 100 cell/mmCitation3 were CrAg + ve, of whom only 2.6% (5/190) had an LP. The authors reported that none of the patients referred to PMMH from the clinics for suspected CCM were diagnosed with CCM, but that 20% (38/190) of those previously seen at the referral clinics who were CrAg + ve had self-presented to the hospital with CCM.Citation10 The authors concluded that early/subclinical CCM may be difficult to detect in a busy clinical environment, and that there might be a place for doing routine LPs in all patients with a CD4 count ≤ 100 cells/mm3 to detect early onset of CCM.Citation15 The aim of this study was to establish the outcome of patients admitted with CCM to a regional referral hospital in Durban between June 2015 and May 2016, and to establish to what extent the NDoH protocols were adhered to in the management of CCM.
Methods
Prince Mshiyeni Memorial Hospital (PMMH) is a 1200-bed regional referral hospital situated on the outskirts of Umlazi Township, Durban, and serves a population of approximately two million people with an estimated HIV prevalence of 16.9%.Citation16 This was an observational descriptive study in which medical records of patients admitted to PMMH with CCM were retrospectively reviewed. All the ward admission books from the adult medical wards at PMMH were reviewed by the principal investigator, and the records of all patients (≥ 12 years) admitted for suspected meningitis between June 2015 and May 2016 were retrieved and reviewed in detail. Only the files of those who had an LP-confirmed diagnosis of CCM based on the CSF results were included in the study.
A standardised data collection sheet was used to record the following: (A) demographic details; (B) medical details (patient symptoms, CD4 count, previous TB, ARTs duration (if on ARTs), CSF results, complications, outcome (death, discharge) and length of stay (recorded in days); and (C) adherence to the NDoH management protocol (duration and dosages of amphotericin B and fluconazole, appropriate monitoring and therapeutic LPs when necessary). Patients given the correct doses of amphotericin B and fluconazole, and who had monitoring bloods taken on three occasions, were assessed to have been managed according to the NDoH protocol. If the patient died before day 14 but had received the correct doses of amphotericin B and high-dose fluconazole, and had been monitored appropriately, they were assessed as having been managed according to the protocol. The data were analysed to establish whether there were any differences between patients who died from CCM and those who were discharged after treatment. The Microsoft Excel software package was used (Microsoft Corp, Redmond, WA, USA) and the data analysed descriptively using the IBM SPSS Statistical Software, version 25 (IBM Corp, Armonk, NY, USA). Fisher’s exact test was used for categorical data and the independent sample t-test for the numerical data, with the level of significance being set at 0.05. Permission to conduct this study was given by the Biomedical Research Ethic Committee (BREC REF No: BE402/16) of University of KwaZulu-Natal (UKZN), the KwaZulu-Natal Department of Health and PMMH management.
Results
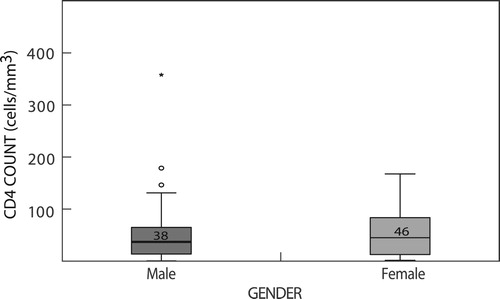
Seventy-six complete records were found of patients admitted and treated at PMMH with CCM between June 2015 and May 2016, of whom 49 (64.5%) were men and 27 (35.5%) were women. The average age of the men was 36 ± 6.9 years and the women was 32 years ± 6.5years, their combined average age being 34.4 (± 6.9 years). Only 64 patients had their CD4 count recorded in their files and/or were traceable on the National Health Laboratory services (NHLS) lab-track, and the average CD4 count was 55.9 cells/mm3 ± 57.4 (range 2–365 cells/mm3) (). Thirty-six (57.8%) of the 64 patients whose CD4 counts were available had a CD4 < 50 cells/mm3; 17 (26.6%) had a CD4 of 50–100 cells/mm3 and 10 (15.6%) had a CD4 > 100cells/mm3 ().
Figure 1: Box diagram of the CD4 count distribution of male and female patients admitted to PMMH with confirmed CCM.
Although not all patient complaints were documented, headache was the commonest symptom (90.8%, 69/76) in those presenting with CCM, with other common symptoms including photophobia (52.6%) and confusion (32/75; 42.6%). A large percentage of patients (60%; 45/75) either had active TB or a history of previous TB. Thirty-eight (50.6%) of the patients were ART naive and nine (12%) had been on ARTs for less than one month ().
Table 1: Profile of patients admitted for CCM at PMMH 2015/2016
The CSF finding of patients admitted with CCM are presented in , which shows that there was no statistically significant difference in the results between those discharged and those who died in terms of CSF chemistry, CSF globulin or cell count. In addition, there was no statistical difference in mortality when scanty, moderate and numerous yeast cells were seen in the CSF.
Table 2: CSF variables for patients admitted for CCM at PMMH 2015/2016
The majority of patients (65/76, 85.5%) were treated with intravenous (IV) amphotericin B and high-dose oral fluconazole (). Five patients (6.7%) received only amphotericin B; four (5.2%) received fluconazole only (two had renal impairment; one died before amphotericin B was given; no reason could be found for the last patient), and two were not treated with antifungals (one died before LP results were available; no reasons were given as to why the other patient was not treated with antifungal agents). There was a statistically significant difference in the mortality between those who received amphotericin B and fluconazole, amphotericin B only and fluconazole only (p = 0.011). The average dose of amphotericin B was 0.85 mg/kg, which is in keeping with recommendation of 0.7–1.5 mg/kg provided in the NDoH protocol. Similarly, 90.8% (69/76) were started on high-dose fluconazole; two were started on 400 mg, while one was given 200 mg only during the entire stay in the hospital.
Table 3: Treatment given and outcome of patients admitted with cryptococcal meningitis
Fourteen days of amphotericin B was completed in only 51.4% (36/70) of patients, for whom a urea and electrolytes (U&E) sample was taken on average 3.38 times. Of the 65 (85.5%) patients who were treated with amphotericin B and fluconazole combination, 44 had at least one electrolytes complication that needed to be managed in the ward. Overall, there were no statistically significant differences in terms of outcome, whether they had one, two or three complications during the treatment (p = 0.264), nor between complications and outcome (p = 0.538). Therapeutic LPs and opening pressure measurements were not common, with the latter never being recorded in the ward, possibly due to a lack of equipment. Notwithstanding the treatment duration, only 19 (25.7%) patients received one therapeutic LP, while four (5.4%) received two. The low number of therapeutic LPs may be due to the large number of patients each clinician is expected to manage.
Of the 76 patients admitted, 24 died (32%) and 52 (68%) were discharge after treatment, with those who survived spending an average of 19.5 days in hospital. The NDoH protocol for managing CCM was adhered to in 72.4% (55/76) of patients, with no statistically significant difference in outcome between those patients who were managed as per the protocol and those who were not (p = 0.177).
Discussion
The profile of patients presenting with CCM were young (average age of 34.4 years) and male (64.5%), which is similar to the 65% male predominance reported by Adeyemi from Northdale Hospital in 2015,Citation17 and highlights the challenge of HIV testing and treating this cohort. In this study, the males were slightly older (mean age = 36 ± 6.9 years) than the females (mean age = 32 ± 6.5 years) (p = 0.046), which is consistent with the findings of other studies, suggesting that women are contracting HIV at a younger age.Citation18–20 Research has shown that young women are at a higher risk for HIV acquisition due to a complex combination of biological, behavioural, structural and sociocultural factors.Citation18,Citation21 The age group most affected in this study was 20–48 years, with a mean of 34.4 ± 6.9 years.
The males had a slightly lower CD4 (cells/mm3) count (mean = 55.74 ± 64.7) than the females (mean = 56.16 ± 45) (p = 0.978), which is similar to the gender difference reported in a number of other studies.Citation19,Citation20 The very low CD4 count in the majority of patients in this study suggests long-standing HIV infection and profound immunosuppression. There have been numerous HIV campaigns in SA, and it may be that many (young) people have become immune to the HIV prevention messages and are no longer receptive to the ABC (abstain, be faithful and condomize) approach to HIV prevention. New thinking and strategies need to be developed to encourage people to test and treat if we are to achieve the 90–90–90 targets and an AIDS-free generation by 2020.Citation8
In this study, 45 of the 76 (59.2%) patients who were admitted and 13 of the 24 (54.2%) who later died had either a previous history of previous tuberculosis (TB) or were on TB treatment at the time of admission. The literature suggests a link between TB, pulmonary fungal survival and the development of CCM in HIV-infected patients.Citation29,Citation30 There is a particularly strong epidemiological link between TB and HIV infection,Citation22,Citation23 with HIV infection known to be an important risk factor for reactivation of latent Mycobacterium TB infection, its rapid progression and re-infection.Citation24 Likewise, TB has been shown to be the commonest cause of morbidity and mortality in HIV-infected persons.Citation25–27 The synergic interaction that exists between TB and HIV requires both diseases to be understood within the same epidemiological boundary, as their management is closely linked, and the outcomes depend on pre-emptive suspicion, diagnosis and management of the other. Similarly, in order to understand the role of the lung in cryptococcal infection, the primary pulmonary infection by C. neoformans is suspected to be the basis of fungal survival, latency and systemic dissemination to the central nervous system.Citation28 In addition, it is thought that TB contributes in some way to disseminating the cryptococcal fungi;Citation29 however, the link between CCM and TB infection needs further study.
While some studies have linked acute mortality in CCM to confusion at presentation and a low CSF white cell count, Citation30–32 this study showed no significant statistically difference in mortality with regard to confusion (p = 0.597) and a CSF white cell count (p = 0.353). This lack of relationship between acute mortality and low bodyweight and CSF white cell count is consistent with other studies that have shown no link between these factors.Citation33,Citation34 It has been reported that cryptococcal fungi, identified by Indian ink staining at diagnosis, is directly linked to high mortality in HIV-positive patients.Citation35 However, due to the small sample in this study, mortality was not strongly related to a positive Indian ink result (p = 0.223).
In SA, CCM in HIV-infected patients is managed according to the 2011 WHO guidelines,Citation12 which were adopted and included in the South African HIV protocol for managing CCM in 2015.Citation13,Citation36 Of the 65 (63%) patients who were treated with amphotericin B and fluconazole, as per the NDoH protocol,Citation36 44 developed electrolyte abnormalities that needed to be managed in the ward. These finding are higher than a phase II randomised trial conducted in Thailand and the USA between 2005 and 2007, in which only 30% of patients on a combination of amphotericin B and fluconazole developed toxicity leading to hypomagnesemia, hypokalaemia, anaemia, decreased renal function or psychosis.Citation37 Although there was no association between developing complications and mortality, the findings of this study highlight the need for careful monitoring of all patients treated for CCM to detect and manage problems associated with treatment.
In-hospital mortality from CCM was 31.6%, despite the use of IV amphotericin B and high-dose fluconazole in the majority of those who died. Although there was no statistical association between following the protocol and discharge (p = 0.177), in slightly over one-quarter of patients the NDoH protocol for managing CCM was not followed, highlighting the importance of audits and ongoing training in the management of patients with CCM. Despite the high adherence to the NDoH protocol in the majority of patients, it would appear that the in-hospital management mortality for CCM can only be addressed by earlier diagnosis of HIV and initiation of ARTs to prevent the profound immunosuppression that is associated with CCM.
Limitations
The small sample size may have affected the study results, which must therefore be treated with caution.
Conclusions and recommendations
Although there is room to improve the in-hospital management of CCM, its associated high mortality is unlikely to change substantially without new thinking about testing and treating HIV-infected individuals. In addition, based on the findings of Ndayishimiye,Citation10 a more proactive approach to patients who are CrAg + ve should be considered, which could include an LP on all HIV + ve patients with low CD4 counts who were CrAg + ve. This approach has been shown to detect a high rate of patients with CCM in other studies and could lead to a reduction in mortality associated with CCM.Citation38,Citation39 However, this practice will add additional health costs and increase the already heavy workload of healthcare workers in SA, and such a policy change must be carefully considered and done in collaboration with other stakeholders to enable timeous and cost-effective assessment and treatment measures to be put in place.
Disclosure statement
No potential conflict of interest was reported by the authors.
ORCID
Egide Ndayishimiye http://orcid.org/0000-0003-2287-5724
References
- AIDS update 2016. Geneva, Switzerland: Joint United Nations programme on HIV/AIDS 2017.
- WHO. Global Report: UNAIDS Report on the AIDS epidemic, 2016. In: HIV/Aids. JUNPo, editor. Geneva: UNAIDS; 2016.
- Lehohla P. Mid-year population estimates, 2017. In: Stats SA, Pretoria: Government printer; 2017;1–20.
- Sengayi MM, Kielkowski D, Egger M, et al. Survival of patients with Kaposi's sarcoma in the South African antiretroviral treatment era: A retrospective cohort study. S Afr Med J. 2017;107(10):871–6.
- Harrison TS. The burden of HIV-associated cryptococcal disease. AIDS. 2009;23(4):531–2.
- Lessells RJ, Mutevedzi PC, Newell ML, et al. Poor long-term outcomes for cryptococcal meningitis in rural South Africa. S Afr Med J. 2011;101(4):251–2.
- Adeyemi BO, Ross A. Management of cryptococcal meningitis in a district hospital in KwaZulu-Natal: a clinical audit. Afr J Prim Health Care Fam Med. 2014;6(1):1–6.
- Organisation WH. Ambitious treatment targets: Writing the final chapter of the AIDS epidemic In: UNAIDS, editor. Geneva: UNAIDS; 2014.
- Johnson LF, Moolla H, Dorrington RE. Progress towards the 2020 targets for HIV diagnosis and antiretroviral treatment in South Africa. South Afr J HIV Med. 2017;18(1):1–8.
- Ndayishimiye E, Ross AJ. An audit of the screen-and-treat intervention to reduce cryptococcal meningitis in HIV-positive patients with low CD4 count. African Journal of Primary Health Care & Family Medicine. 2018;10(1):1–7.
- National consolidated guidelines for the prevention of mother-to-child transmission of HIV (PMTCT) and the management of HIV in children, adolescents and adults. In: Health NDo, editor. Pretoria: National Department of Health; 2014. p. 119.
- Nagalingeswaran Kumarasamy PC, Nelesh PG, Lut Lynen, et al. Rapid advice: diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents and children: December 2011. WHO. 2011;1–44.
- Govender N, Meintjes G, Bicanic T, et al. Guideline for the prevention, diagnosis and management of cryptococcal meningitis among HIV-infected persons: 2013 update. S Afr J HIV Med. 2013;14(2):76–86.
- Walaza S. Cryptococcal screen-and-treat in Gauteng province, South Africa: Update from the first two years of implementation, 2012–2014. In: Health GDo, editor. Pretoria: Department of Health; 2014.
- Pongsai P, Atamasirikul K, Sungkanuparph S. The role of serum cryptococcal antigen screening for the early diagnosis of cryptococcosis in HIV-infected patients with different ranges of CD4 cell counts. Journal of Infection. 2010;60(6):474–7.
- KZN. UNIVERSAL TEST AND TREAT “A Game Changer in HIV Prevention”. In: Health, editor. KwaZulu-Natal: KZNonline; 2016.
- Adeyemi BO, Ross A. Profile and acute mortality outcome of patients admitted with cryptococcal meningitis to an urban district hospital in KwaZulu-Natal, South Africa. S Afr Fam Pract. 2015;57(2):1–5.
- Shisana O, Rehle T, Simbayi LC, et al. South African national HIV prevalence, incidence and behaviour survey, 2012. 2014.
- Mosha F, Muchunguzi V, Matee M, et al. Gender differences in HIV disease progression and treatment outcomes among HIV patients one year after starting antiretroviral treatment (ART) in Dar es Salaam, Tanzania. BMC public health. 2013;13(1):1–7.
- Hawkins C, Chalamilla G, Okuma J, et al. Sex differences in antiretroviral treatment outcomes among HIV-infected adults in an urban Tanzanian setting. Aids. 2011;25(9):1189–97.
- Pettifor AE, Rees HV, Kleinschmidt I, et al. Young people's sexual health in South Africa: HIV prevalence and sexual behaviors from a nationally representative household survey. Aids. 2005;19(14):1525–34.
- Corbett L, Raviglione M. Global burden of tuberculosis: past, present, and future. Tuberculosis and the Tubercle Bacillus: American Society of Microbiology; 2005. p. 3–12.
- Sharma S, Mohan A, Kadhiravan T. HIV-TB co-infection: epidemiology, diagnosis & management. Indian J Med Res. 2005;121(4):550–67.
- Bucher HC, Griffith LE, Guyatt GH, et al. Isoniazid prophylaxis for tuberculosis in HIV infection: a meta-analysis of randomized controlled trials. Aids. 1999;13(4):501–7.
- Del Amo J, Malin AS, Pozniak A, et al. Does tuberculosis accelerate the progression of HIV disease? Evidence from basic science and epidemiology. Aids. 1999;13(10):1151–8.
- Badri M, Ehrlich R, Wood R, et al. Association between tuberculosis and HIV disease progression in a high tuberculosis prevalence area. Int J Tuberc Lung Dis. 2001;5(3):225–32.
- Lopez-Gatell H, Cole S, Hessol N, et al. Effect of tuberculosis on the survival of women infected with human immunodeficiency virus. Am J Epidemiol. 2007;165(10):1134–42.
- Zaragoza O, Nielsen K. Titan cells in Cryptococcus neoformans: cells with a giant impact. Curr Opin Microbiol. 2013;16(4):409–13.
- Singh U, Aditi AP, Kapoor B, et al. Cryptococcal meningitis associated with tuberculosis in HIV infected patients. Indian J Tuberc. 2013;60(3):180–3.
- Jarvis JN, Bicanic T, Loyse A, et al. Determinants of mortality in a combined cohort of 501 patients with HIV-associated cryptococcal meningitis: implications for improving outcomes. Clin Infect Dis. 2014;58(5):736–45.
- Boulware DR, Meya DB, Muzoora C, et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N Engl J Med. 2014;370(26):2487–98.
- Kambugu A, Meya DB, Rhein J, et al. Outcomes of cryptococcal meningitis in Uganda before and after the availability of highly active antiretroviral therapy. Clin Infect Dis. 2008;46(11):1694–701.
- Rolfes MA, Hullsiek KH, Rhein J, et al. The effect of therapeutic lumbar punctures on acute mortality from cryptococcal meningitis. Clin Infect Dis. 2014;59(11):1607–14.
- Bicanic T, Muzoora C, Brouwer AE, et al. Independent association between rate of clearance of infection and clinical outcome of HIV-associated cryptococcal meningitis: analysis of a combined cohort of 262 patients. Clin Infect Dis. 2009;49(5):702–9.
- Zuger A, Louie E, Holzman RS, et al. Cryptococcal disease in patients with the acquired immunodeficiency syndrome: diagnostic features and outcome of treatment. Ann Intern Med. 1986;104(2):234–40.
- DoH. National consolidated guidelines for the prevention of mother-to-child transmission of HIV (PMTCT) and the management of HIV in children, adolescents and adults. In: Health, editor. Pretoria: South African Department of Health 2014;1–136.
- Pappas PG, Chetchotisakd P, Larsen RA, et al. A phase II randomized trial of amphotericin B alone or combined with fluconazole in the treatment of HIV-associated cryptococcal meningitis. Clin Infect Dis. 2009;48(12):1775–83.
- Micol R, Lortholary O, Sar B, et al. Prevalence, determinants of positivity, and clinical utility of cryptococcal antigenemia in Cambodian HIV-infected patients. J Acquir Immune Defic Syndr. 2007;45(5):555–9.
- Pongsai P, Atamasirikul K, Sungkanuparph S. The role of serum cryptococcal antigen screening for the early diagnosis of cryptococcosis in HIV-infected patients with different ranges of CD4 cell counts. Journal of Infection. 2010;60(6):474–7.