ABSTRACT
Background
Despite acute appendicitis is the most common underlying etiology of the acute abdomen, a considerable list of other pathologies should be considered; despite sharing almost the same clinical presentation. This study aimed to re-enhance the importance and sensitivity of CT scan as a solitary imaging tool, in the evaluation of patients with acute right lower abdominal pain.
Patients and methods
It is a retrospective study of the last 1000 patients, referred with acute right lower abdominal pain for CT scan examination. Biphasic CT scan abdomen protocol was applied for all.
Results
Cecal carcinoma was detected in three patients (0.3%), epiploic appendicitis in five (0.5%), omental infarct in two (0.2%), appendicular mucocele in two (0.2%), appendicular NET in one (0.1%), cecal diverticulitis in four (0.4%), Chron’s disease in six (0.6%), intussusception in one (0.1%) and FB in one (0.1%) and appendicular perforation in one (0.1%), acute simple appendicitis 398 (39.8%) and 577 (57.7%) were unremarkable.
Conclusion
Despite acute appendicitis is the most common cause of the acute abdomen, many other surgical and non-surgical etiologies should also be considered, with a higher sensitivity of CT as a solitary diagnostic tool of imaging.
1. Introduction
Acute right iliac fossa pain is undoubtedly the most common cause of acute abdominal presentation to the ER. Despite acute appendicitis is the most common underlying etiology, a considerable list of differential diagnoses should be considered. Other pathologies, which may be presented with similar clinical presentation, include ileocecal inflammatory and infectious conditions, e.g. diverticulitis and epiploic appendagitis. Also, acute omental or mesenteric vascular insults and some neoplastic lesions may have similar presentation. The clinical diagnosis of appendicitis may be challenging even in the most experienced hands, with considerable recorded errors in surgical management decisions, based upon false-positive clinical and/or sonographic diagnosis of appendicitis. [Citation1–Citation3]
Although false-positive ultrasound results of acute appendicitis are not frequently encountered, there were some reports of such error. This may be due to the presence of some other diseases, which may share the sonographic main reliable sign of acute appendicitis. This possible shared sign is the non-compressible tubular structure at the right iliac fossa, which also could be due to regional ileitis or pelvic ureteritis, which also may have similar clinical presentation. Also, regional vasculitis with segmental bowel ischemia or localized right lower ureteric dilatation and inflammation may show nearby sonographic features. [Citation4,Citation5]
Multidetector CT scan had been proven to be an extremely sensitive noninvasive tool of imaging for accurate evaluation of the patients, who are presented with acute right lower abdominal pain. In a relatively newly published study, it was proven that the sensitivity and specificity of CT range between 87% and 100% and 89% and 99%, respectively; as regards the diagnosis of appendicitis. On the contrary, this high sensitivity and specificity records are good indicators for the ability of CT scan to accurately delineate appendicitis mimic diseases. This clear differentiation is very helpful to avoid unnecessary surgical intervention or possibly iatrogenic complications of non-operable cases. [Citation6,Citation7]
2. Aim of the study
This study aimed to re-enhance the importance and sensitivity of CT scan in the evaluation of patients with acute right lower abdominal pain, as regards demonstrating the alternative possible pathological conditions that may clinically simulate acute appendicitis. Many of these similar clinical disorders are non-surgical emergencies, which could be managed conservatively.
3. Patients and methods
3.1. Patients
It is a retrospective study of the last 1000 (571 males and 429 females) patients, who were referred from the ER as an emergency to do an urgent abdominal CT scan. All patients were referred with acute right iliac fossa pain, which was clinically suspected to be acute appendicitis. The study included the examinations done from 1-3-2017 to 30–10-2019, retrieved from the CT scan cases notebook. The patients’ age ranged from 5 years to 76 years. Approval consent was obtained from the hospital medical ethics committee. A signed consent was obtained from all study candidates, including a detailed description of the technique with the rare possible drawbacks.
3.2. Protocol
Our standard urgent CT abdomen protocol was done, first through instructing the patients to be off oral for 2–4 hours prior to the study time. Then, oral preparation was done by drinking 5 cups (1 L) of distilled water 1 h prior to the CT examination time. Another two water cups were given on the table, immediately before the examination. Non-contrast scan was done first, followed by an automated injection of 1.5 ml/kg intravenous nonionic contrast media (Omnipaque 300) as a single bolus with an injection rate of 3–4 ml/sec. Then, CT scan cuts were obtained at both arterial and portal phases, 20–30 and 60–70 seconds, respectively. The CT examinations were done through Philips Brilliance 64 CT Scanner, Philips Medical System, and Nederland. B.V. Veenpulis 4–5, 468 + 4 PC Best, Netherlands.
4. Results
Retrograde checking of CT scan results of the 1000 candidates was: cecal carcinoma in 3 patients (3%), acute epiploic appendagitis in 5 patients (0.5%), omental infarct in 2 patients (0.2%), appendicular mucocele in 2 patients (0.2%), appendicular NET in one patient (0.1%), cecal diverticulitis in 4 patients (0.4%), Chron’s disease in 6 patients (0.6%), ileocecal intussusception, and foreign body in one patient (0.1%) and appendicular perforation in one patient (0.1%). Three hundred and ninety-eight (39.8%) patients were diagnosed as acute simple appendicitis, while the rest 577 studies (57.7%) were unremarkable.
Table 1. The CT scan results.
5. Discussion
Definitely, acute appendicitis is the comments etiology of acute abdomen in the hospitals’ EMS. However, acute appendicitis can clinically simulate a group of different diseases, which could be managed conservatively, with no need for surgical intervention. Reciprocally, many conditions are initially incorrectly diagnosed as appendicitis, with resultant delayed treatment or unnecessary removal of a non-inflamed appendix. Also, appendicitis could be concomitantly presented, in association with one of these mimickers, which may cause failed appendectomy symptoms. So, being alert with these appendicitis mimics will help to attain early prompt and accurate diagnosis, which is essential to minimize the expected morbidity. In our retrieved research, we had confronted with different types of appendicitis mimics alone or in association with acute appendicitis [Citation8,Citation9].
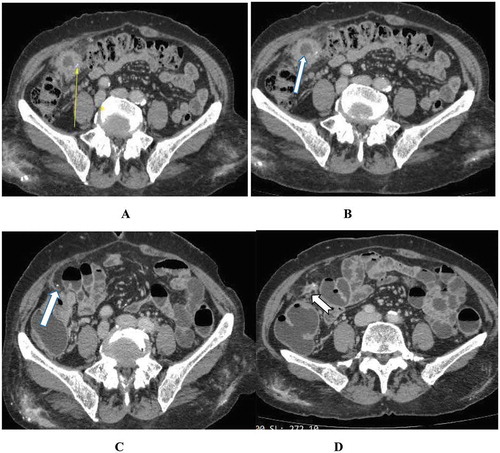
5.1. Cecal carcinoma
Three patients (0.3%) had been presented with chronic right iliac fossa pain, with acute exacerbation. WBC was normal in two patients and elevated in only one patient. They had been diagnosed with CT scan as ileocecal tumors; which were proven pathologically to be adenocarcinoma. The one who had associated high WBC was presented with carcinoma associated with acute appendicitis (). Acute abdomen may be the initial presentation of an ileocecal malignant tumor, commonly at this site adenocarcinoma or lymphoma, gastrointestinal stromal tumor, or metastasis, especially if complicated with perforation or abscess. The differentiation between an appendicular mass and a malignant ileocecal lump may be straightforward at the CT scan; if the appendix could be clearly identified and separated from the ileocecal mass lesion. However, this is not always a simple easy task. [Citation10,Citation11]
Figure 1. Incidental cecal carcinoma discovery in association with acute appendicitis: (A&B) Axial post-contrast (C&D) CMPR showing: An infracecal inflammed appendix (Arrow in A&C), in association with cecal mass (Notched arrow in B&D), together with extensive regional mesenteric fat stranding.
This diagnostic quandary could be explained by the possibly shared CT signs such as abscess formation, fat planes stranding, as well as bowel wall thickening. Considering, as well faced in our study, the usual elderly patient’s presentation in malignancy, a malignant consideration should be always kept in mind in older patients even if presented with clear appendicitis symptoms, with immediate postoperative specimen pathological analysis. This malignant suspicion, even if it got some false-positive results, it is expected to protect against missing and dissemination of these regional neoplastic lesions. [Citation12]
5.2. Acute epiploic appendagitis/Omental infarct
Acute epiploic appendagitis, is one of the infrequently seen causes of acute abdominal pain. It is more commonly found on the left abdomen, in association with left colonic diverticulae. Uncommonly, it may occur on the right lower abdomen giving a clinical picture of acute right lower abdominal pain and tenderness, which may simulate acute appendicitis, as we detected in five patients (0.5%) of our retrieved cases. They had been presented with symptoms similar to acute appendicitis, including the right iliac fossa rebound tenderness, but with no significant leukocytosis. These are multiple peritoneal pouches exiting from the serosal surface of the colon, with a vascular stalk. These pouches are mainly composed of fatty tissues and blood vessels, having a length of 0.5–5 cm. Normally, they are not seen unless there is considerable surrounding ascetic fluid. Once inflamed, they could be typically seen at CT examinations; as an oval lesion 1.5–3.5 cm in diameter, with fatty attenuation and hyperdense central spot of a thrombosed vein. [Citation13,Citation14]
Figure 2. Urgent immediately done CT scan abdomen showing: Acute infracecal appendictis (Arrow in A), while axial (B), coronal reformat (C) and sagittal reformat (D) show infracecal epiploic appendigitis (Notched arrow from B-D).
Despite the central high attenuation spot due to venous thrombosis is a specific character for the diagnosis of acute epiploic appendagitis, it is not always present which may overlap its CT features with the nearby features of the omental infarct. However, omental infarct is reported to more commonly affect younger age groups rather than the adult age group of the epiploic appendagitis, i.e. children and adolescents. Also, omental infarct, as we saw in two patients (0.2%), is usually presented with a larger noncapsulated omental mass of smudged fat (more than 5 cm). It is larger than and lacks the central hyperdense dot of the epiploic appendagitis (). However, distinctive differentiation between omental infarcts and epiploic appendagitis is not so important, as the management of both insults is almost similar [Citation15].
5.3. Appendicular mucocele/low-grade cystic tumor
The mucoceles occur due to abnormal excessive accumulation of mucin within the appendicular lumen, leading to excessive cystic distention of the appendix on top of different pathologies. We had been confronted with two cases (0.2%) of appendicular mucocele () and only one (0.1%) as low grade mucinous cystic tumor (). Both lesions were clinically presented as right iliac fossa distension and dull aching pain, with minimal leukocytosis. Pathologically, the appendicular mucocele could be subdivided into different types; according to the underlying etiology. It could be due to simple inflammatory retention mucocele, which may occur due to appendicular lumen obstruction by a faecolith or mucosal hyperplasia. Also, it may be mucinous cystadenoma, which is the most common or less commonly mucinous cystadenocarcinoma. [Citation16,Citation17]
Figure 4. CT scan abdomen axial (A&B) and CMPR (C&D) showing: cystic mucocele due to distal appendiceal dilatation (Arrow in A,b&D) on top of proximal lumen obstruction (Notched arrow in A&C). There is asymmetrical right pelvic raectional lateral conal fascial thickening (Curved arrow in D), adherent to the chronically inflammed appendix.
Figure 5. CT scan arterial phase: (A&B) axial and (C) CMPR of one patient with appendicular calcific (Notched Arrow) enhancing carcinoid tumor (Arrow). (D,E&F) CMPR of another patient with appendicular tip calcific enhancing carcinoid tumor (Notched Arrow) in association with right adrenal avidly enhancing nodule (Arrow) highly suggestive of pheochromocytoma.
CT is very sensitive imaging modality for diagnosis of the appendicular mucocele, which is seen as a well-encapsulated, hypodense, finger-like or rounded cystic swellings of different sizes. The most important sign is the continuity of the swelling with the base of the cecum at the assumed position of the appendix. A ring-like calcification could be seen in about 50% of cases (), or rarely intraluminal gas or a gas-fluid level, due to superadded infection. Differentiation with mural nodularity and irregular wall thickening are suggestive of a malignant process. It is very important to check for extraluminal mucin, which could be seen at CT scan as extra-appendicular hypodense implants, due to appendicular mucocele perforation. This extraluminal free mucin could be localized periappendiceal space, or it could be disseminated in the peritoneal cavity, e.g. the pouch of Douglas, rectovesical pouch, perihepatic space, and omentum. The severest complication of the appendicular mucocele perforation is the pseudomyxoma peritonei (mucinous ascites), if there is underlying neoplastic etiology. [Citation18,Citation19]
5.4. Appendicular NET (carcinoid tumor)
Appendicular neuroendocrinal tumor (NET), which was previously termed carcinoid tumors, was preoperatively diagnosed in one patient (0.1%). It was clinically presented with chronic, dull aching, nonspecific lower right quadrant abdominal pain, with no leukocytosis. It was seen as an appendicular apical, arterially enhancing soft tissue swelling, with ring-like calcification (). Appendicular NET, less than 1 cm in size, is difficult to be clearly seen at the usual CT abdomen protocols. If located at the base of the appendix, it is usually presented with appendicitis like symptoms, due to obstructed lumen. It is commonly misdiagnosed as inflammatory appendicular mass. [Citation20,Citation21] ()
Figure 6. (A&B) Axial (C &D) Sagittal contrast Ct scan showing anterior cecal diverticulitis (Arrow in A), posterior cecal diverticula (Notched Arrow), and infracecal normal appendix (Curved Arrow).
Figure 7. CT scan abdomen axial (A-C) and CMPR (D) showing a retroileal partly cystic soft tissue swelling (Arrow in A&B) with a fecolith like calcification. (Arrow in C&D) It was diagnosed as appendicular mass; however, it was surgically and pathologically proven to be NET.
Lymphatic or hematogenous metastasis had been reported in works of literature to be seen in less than 10% of patients, with a carcinoid tumor larger than 2 cm. So, if a post-appendectomy NET is incidentally discovered, postoperative CT chest and abdomen with tiphasic technique is highly recommended to exclude distant arterial enhancing carcinoid deposits. Also, the biochemical markers are specific for the diagnosis of the NET, so it can facilitate a more accurate diagnosis. The two biochemical markers, which are confidently used to diagnose and follow up the treatment results of carcinoid tumors, are 24-h urine 5-hydroxyindoleacetic acid (5-HIAA) and serum chromogranin A (CgA)). [Citation22]
5.5. Cecal diverticulitis
Four patients (0.4%) were diagnosed as acute cecal diverticulitis; with average age 52 years. He was provisionally diagnosed clinically as possible acute appendicitis, with repeated acute right lower abdominal pain, with rebound tenderness and leukocytosis. CT scan revealed severe inflammatory changes in the right lower quadrant, with regional pericecal fat stranding. The inflamed cecal diverticulum had been shown as hyperdense ring surrounding relatively thick-walled edematous diverticulum; beside the other non-inflamed other diverticula which lack this hypodense ring. [Citation23]
Figure 8. CT scan abdomen axial (A&B) and coronal (C&D) showing terminal ileum stricture (Arrow in A&C), as well as pelvic abscess (Notched Arrow in B&D). Fat planes comb sign (Chevron in C), entrapment of the right ureter is noted at the pelvic inlet with secondary severe hydronephrosis (Arrow in D) and hydroureter (Curved Arrow in A&D).
The cecal or right-sided colonic diverticulitis are less common than the left-sided ones, representing only 3.6% of all colonic diverticular disease. It has no specific clinical presentation and may resemble acute right lower abdominal pain of appendicitis or epiploic appendagitis. In contrast to the sigmoid pseudo-diverticula, the cecal and the right-sided colonic diverticula are usually true, which is composed of all layers of the colonic wall. CT scan with oral, rectal, and IV contrast is very sensitive for the diagnosis of cecal diverticular disease and superadded diverticulitis, if any, with sensitivity and specificity reaching 100% [Citation24,Citation25].
5.6. Chron’s disease
Crohn’s disease or regional enteritis is an idiopathic chronic inflammatory bowel disease, which may affect any segment of the gastrointestinal tract, from the mouth to the anus. Crohn’s disease usually shows multiple asynchronous skip segmental gastrointestinal involvement with varying degrees of severity. Ileocecal region is the most commonly involved site, with relative long segmental affection of the terminal ileum and the proximal right colon. The revised history of our candidates documented 6 (0.6%) radiologically diagnosed and histopathologically proven Chron’s disease. Patients’ age ranged between the ages of 15 and 25 years, with near similar clinical and laboratory presentation of questionable acute appendicitis. The complaint was acute exacerbated right iliac fossa pain on top of chronic pain. [Citation26]
CT is the imaging modality of choice for diagnosis of Chron’s disease, at most radiology institutions. This due to its characteristic rapid acquisition time with high spatial resolution during a single breath-hold. It showed ileocecal relatively long segmental annular thickening and smooth stricture, giving the target sign. Abnormal post-contrast enhancement of the bowel wall may be seen as a result of increased vascular permeability and angiogenesis. Characteristic mesenteric inflammatory changes are usually seen in Chron’s disease, as fibrofatty proliferating strands, surrounding the engorged mesenteric blood vessels (comb sign). Also, scattered small mesenteric inflammatory lymphadenopathy, mesenteric abscess, enteric fistula, and skip lesions could be seen. The postcontrast intestinal mural contrast enhancement should be taken into consideration as a sign which reflects the degree of active inflammation and could differentiate IBD from the similar long segmental infiltrating neoplastic process, e.g. lymphoma [Citation27,Citation28].
Figure 9. CT scan abdomen axial (A&B) and coronal (C&D) showing terminal ileum stricture (Arrow in A&C), as well as pelvic abscess (Notched Arrow in B&D). Fat planes comb sign (Chevron in C), entrapment of the right ureter is noted at the pelvic inlet with secondary severe hydronephrosis (Arrow in D) and hydroureter (Curved Arrow in A&D).
5.7. Ileocecal intussusception
One 36y male patient of our candidates (0.1%) was referred from ER with acute lower abdominal pain and tenderness, together with no leukocytosis. CT scan showed an ileocecal intussusception extending for 10 cm within the ascending colon. There was a terminal ileal submucosal lipoma, measuring 6.5 × 4.5 cm in dimensions. This lipoma was acting as the lead point of such short segment ileocecal intussusception. Adult ileocecal intussusception is an uncommon etiology of acute right abdominal pain or appendicitis mimics, as it represents only 5% of the intestinal intussusceptions. It is always secondary to or on top of a leading ileocecal selling, in contrast to the more common primary pediatric intussusceptions (95%). Most authors thought to relate this primary pediatric intussusception to the hypertrophic lymphoid tissue following an infection. This etiology could potentially explain the uncommon presentation of intussusception at the first 3 months of life, due to the fundamental passive immunity [Citation29].
5.8. Secondary appendicitis due to foreign body
Another one 67 y male patient (0.1%) was presented with severe acute appendicitis like symptoms and signs. CT scan revealed showed a linear dense foreign body in the mesentery, in close relation to the tip of a pre-ileal inflamed appendix. There was an ileocecal mucosal hyperenhancement and submucosal edema and regional stranding of the right iliac fossa fat planes. This mesenteric foreign body was surrounded with a considerable ring-enhancing collection, which was reported as sealed appendicular perforation with periappendicular abscess ). The patient was first managed conservatively with intense broad-spectrum short antibiotic course, with repeated CT scan after 1 week. The second study revealed a significant resolution of the collection and clearly demonstrated the residual inflamed appendix. ) Operative feedback history documented a sealed appendicular perforation with extra-appendicular fish bone foreign body.
Figure 11. (A&B) showing a right iliac fossa linear dense FB (Arrow in A), with secondary superadded appendicular abscess. (Arrow in B) (C&D) 5 months follow up study revealed the FB (Arrow in C) in close relation to the tip of an inflamed appendix (Notched arrow in D), which is seen originating from the anterior cecal wall.
Development of appendicitis secondary to or on top of a foreign body is truly uncommon but a reported complication of the ingestion of foreign body objects. However, appendicitis itself is definitely a common disease, and this foreign body association could be just coincidental. Some small rounded foreign body objects, such lead shot, paintball BBs, and aggregated barium particles can be lodged in the appendix for a long time, without significant effect. However, other foreign sharp objects such as fish bones, pins, and toothpicks can induce acute appendicular inflammation or perforation. CT is the perfect imaging modality of choice for the demonstration of these appendicular foreign bodies and the possible appendicular or regional inflammatory changes, as well. [Citation30]
6. Conclusion
Despite, acute appendicitis is the most common cause of the acute right lower quadrant pain, a good number of some other surgical and non-surgical pathologies should also be considered. MSCT scan is the sensitive reliable imaging modality of choice, for the investigation of the right lower quadrant pain, to avoid false appendectomy for appendicitis mimics.
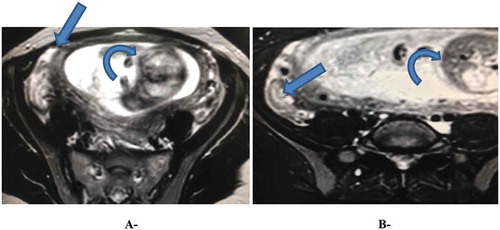
7. Limitations
Regardless of the described sensitivity of CT scan for the accurate diagnosis of the different etiologies of the acute abdomen, it has some limited applications for some patients, e.g. first-trimester pregnancy, as we faced with one patient who was proven to have acute appendicitis by MRI examination (). Also, considering the fact that CT for the acute abdomen should essentially be done with IV contrast, some obstacles will be faced with the patients who are unfit for IV contrast, e.g. patients with compromised renal function and patients with a history of hypersensitivity. So MRI without IV contrast may be a good solution for such limitations. [Citation31].
Authors contribution
Mahmoud Agha: was the editor and supervisor of data collection, editing the manuscript, and corresponding for publication.
Mohammed Eid: Performance of all radiological investigations, as well as revising the edited manuscript draft.
Maha Sallam: Lab consultant doing all necessary lab investigations for the patients; like creatinine clearance; WBC and ESR counts.
Compliance with ethical standards
This study was conducted according to the protocol, good clinical practice, principle, and the declaration of Helsiniki statements. The ethics committee of the administration of the group of Al- Mana General Hospitals had approved the study protocol and all steps, and assigned informed consents were obtained from all participant candidates.
Disclosure statement
The authors declare that they have no conflict of interest.
Additional information
Funding
References
- Falch C, Haeberle H. Kirschniak A and Nissan A. Treatment of acute abdominal pain in the emergency room: a systematic review of the literature. Eur J Pain. 2014;18:902–913.
- Cartwright A, Knudson M. Evaluation of acute abdominal pain in adults. Am Fam Physician. 2008;77(7):971–978.
- Stoker J, Van Randen A, Laméris W, et al. Patients with acute abdominal pain. Radiology. 2009;253(1):31–46.
- Canders C, Brown A, Chiem A. False positive appendicitis on bedside ultrasound. West J Emerg Med. 2014;15:832–833.
- Fox JC, Hunt MJ, Zlidenny AM, et al. A retrospective analysis of emergency department ultrasound for acute appendicitis. Cal J Emerg Med. 2007;8:41–45.
- Schulman H. CT and US in the diagnosis of appendicitis: an argument for CT. Radiology. 2010;255:3–7.
- Sivit CJ. Controversies in emergency radiology: acute appendicitis in children—the case for CT. Emerg Radiol. 2004;10:238–240.
- Petroianu A. Diagnosis of acute appendicitis. Int J Surg. 2012;10(3):115–119.
- Hawkins JD, Thirlby RC. The accuracy and role of cross-sectional imaging in the diagnosis of acute appendicitis. Adv Surg. 2009;43:13–22.
- Fiume I, Napolitano V, Del Genio G, et al. Cecum cancer underlying appendicular abscess. Case report and review of literature. World J Emerg Surg. 2006;1(1):11.
- Khan S, Pawlak SE, Eggenberger JC, et al. Acute colonic perforation associated with colorectal cancer. Am Surg. 2001;67(3):261–264.
- Shine R, Zarifeh A, Frampton C, et al. Appendicitis presenting as the first manifestation of colorectal carcinoma: a 13-year retrospective study. NZ Med J. 2017;130:1459–1468.
- Singh A, Gervais D, Hahn P, et al. Acute epiploic appendagitis and its mimics. RadioGraphics. 2005;25(6):1521–1534.
- Legome EL, Belton AL, Murray RE, et al. Epiploic appendagitis: the emergency department presentation. J Emerg Med. 2002;22(1):9–13.
- Van Breda Vriesman AC, Puylaert JB. Epiploic appendagitis and omental infarction: pitfalls and look-alikes. Abdom Imaging. 2002;27(1):20–28.
- Tirumani S, Fraser-Hill M, Shabana W, et al. Mucinous neoplasms of the appendix: a current comprehensive clinicopathologic and imaging review. Cancer Imaging. 2013;13(1):14–25.
- Pathol AA, Pai RK, Longacre TA. Appendiceal mucinous tumors and pseudomyxoma peritonei: histologic features, diagnostic problems, and proposed classification. Adv Anat Pathol. 2005 Nov;12:291–311.
- Tsokaki P, Misiakos E, Domi V, et al. Low-grade appendiceal mucinous neoplasm presenting as an adnexal mass. Case Rep Obstet Gynecol. 2017;2017:7165321.
- Faure M, Salgado R, Op de Beeck B, et al. Mucocele of the appendix: case report and review of literature. JBR–BTR. 2014;97(4):217–221.
- Pickhardt P, Levy A, Rohrmann C, et al. Neoplasms of the appendix: radiologic spectrum of disease with pathologic correlation. RadioGraphics. 2003;23(3):645–662.
- Ganeshan D, Bhosale P, Yang T, et al. Imaging features of carcinoid tumors of the gastrointestinal tract. AJR. 2013;201(4):773–786.
- Baxi A, Chintapalli K, Katkar A, et al. Multimodality imaging findings in carcinoid tumors: a head-to-toe spectrum. RadioGraphics. 2017;37(2):516–536.
- Ben-Yaacoub I, Boulay-Coletta I, Jullès M, et al. CT findings of misleading features of colonic diverticulitis. Insights Imaging. 2011 Feb;2:69–84.
- Levine CD, Aizenstein O, Lehavi O, et al. Why we miss the diagnosis of appendicitis on abdominal CT: evaluation of imaging features of appendicitis incorrectly diagnosed on CT. AJR Am J Roentgenol. 2005;184(3):855–859.
- Sreenivasan N, Kalyanpur A, Bhat A, et al. CT diagnosis of cecal diverticulitis. Ind J Radiol Imag. 2006;16(4):451–452.
- Thompson J, Selvaraj D, Nicola R. Mimickers of acute appendicitis. J Am Osteopath Coll Radiol. 2014;3:10–21.
- Purysko AS, Remer EM, Filho HM, et al. Beyond appendicitis: common and uncommon gastrointestinal causes of right lower quadrant abdominal pain at multidetector CT. Radiographics. 2011;31(4):927–947.
- Han H, Kim H, Rehman A, et al. Appendiceal Crohn’s disease clinically presenting as acute appendicitis. World J Clin Cases. 2014 Dec;16(2):888–8.
- Kee H, Park J, Yi D, et al. Case of intussusception with acute appendicitis. Pediatr Gastroenterol Hepatol Nutr. 2015 Jun;18:134–137.
- Beh J, Uppaluri A, Koh B, et al. Fishbone perforated appendicitis. J Radiol Case Rep. 2016 Jul;10:14–22.
- Mui LW, Lee HK, Malhotra R. MRI evaluation of acute abdominal pain in the pregnant patient. J Am Osteopath Coll Radiol. 2015;4:12–19.