ABSTRACT
Background
Pediatric ocular trauma may be a major source of lifelong visual morbidity and disability.
Objective
To report on the different types of ocular injury in children in a tertiary referral center.
Participants and settings
Children presenting with ocular trauma to the casualty department of the pediatric ophthalmology unit of Alexandria Main University Hospital in Alexandria, Egypt.
Methods
The study was conducted from June to December 2018. Upon admission, thorough history was obtained from the attending person(s), and thorough ophthalmic examination was performed. Appropriate treatment was subsequently provided to every case (though not the scope of the current study).
Results
A total of 146 children (from a total of 436 patients, 33.5%) (103 males, 70.5%) presented with various types of ocular injuries. The mean age ± standard deviation of the injured children was 98.1 ± 56.4 months. Study participants were almost equally distributed between within and outside of the city of the study locale, with a predominance of patients from urban areas in Alexandria (30%) and from rural areas outside of Alexandria (35.6%). Seventy percent of the care providers of the study children were manual workers. The places of the incidents were almost equally distributed between household (40%) and external environment with a slight predominance of the later (50%).
Conclusions
Ocular injuries represent one-third of all ocular injuries in the study locale. Ocular injuries in children occur with an almost equal distribution in both urban and rural areas and in both household and external environments. Mechanical trauma was the most common cause of trauma.
1. Introduction
Trauma is a significant cause of ocular morbidity and potentially lifelong disability, especially in children [Citation1,Citation2]. Ocular trauma has a reported incidence of 3.7%[Citation3]; pediatric ocular trauma is reported to represent about 22.6% of all eye trauma [Citation4] and is reported to be responsible for about 9 per 100,000 of hospital admissions [Citation5] and 16% of permanent visual impairment [Citation6]. Ocular trauma in children presents a special case in which the consequences may be devastating, both on the personal and community levels. Child abuse may well manifest in the form of ocular trauma [Citation7] with potential social and legislative consequences. Moreover, many of the childhood ocular trauma are potentially preventable, posing responsibility on care providers, as well as on policymakers. The reported incidence of pediatric ocular trauma is highly variable among different countries, being higher in developing countries (ranging between 11%[Citation1] – 36%[Citation2]) than developed countries (25%[Citation8]). The aim of the current study was to report on the different types (and whenever possible, the mechanisms) of ocular injury in children in a tertiary referral center in a developing country.
2. Patients and methods
The study was conducted in the casualty department of pediatric ophthalmology unit of Alexandria Main University Hospital in the period from the beginning of June 2018 to the end of December 2018. All children (individuals below 18 years of age) presenting with ocular trauma were included in the study. The study adhered to the guidelines of the Declaration of Helsinki and was approved by the ethical committee of Alexandria Faculty of Medicine. Written informed consent was provided by all the care providers of the study participants. Upon admission to the casualty department, thorough history was obtained from the attending person(s) regarding the socio-demographics of the injured child and the circumstances of the injury. A thorough ophthalmic examination was performed in the casualty department (office examination) and was complemented by examination under anesthesia (EUA) if this was deemed necessary. When the surgical intervention was considered, EUA was conducted as the initial part of the surgical intervention. Ocular injuries afflicting every part of both eyes were stratified by the mechanism and shape of the injury into injuries inflicted by sharp trauma (open injuries) and blunt trauma (both closed and open injuries) as well as by detailed description according to the nature of the injury. Appropriate treatment was subsequently provided to every case, though not the scope of the current study.
3. Results
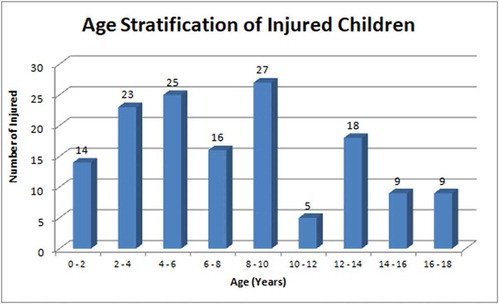
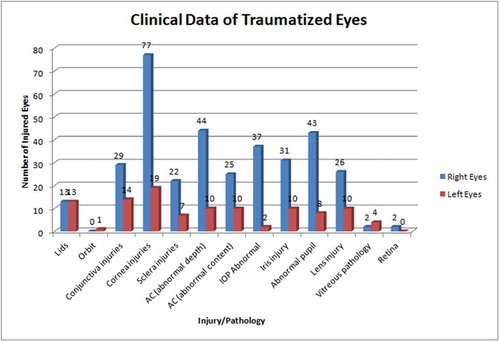
The study was conducted in the period from the beginning of June 2018 to the end of December 2018. During the study period a total of 146 children (from a total of 436 patients, 33.5%) presented with various types of ocular injuries to Alexandria Main University Hospital. The demographic characteristics of the study children are presented in . Almost two-thirds of the injured children were males (70.5%) and the mean age of the injured children was around 8 years. Age stratification of the study children population into biannual strata revealed a predominance of injuries in the age group of 2–10 years, almost equally distributed between the age groups with another peak at 12–14 years (). More than three quarters of the injured eyes were right eyes (77.6%). Study participants were almost equally distributed between within and outside of the city of the study locale, Alexandria, Egypt, with a predominance of patients from urban areas in Alexandria (30%) and from rural areas outside of Alexandria (35.6%). Almost 70% of the care providers of the study children were manual workers. presents the circumstances of the injury in the study children population. The places of the incidents were almost equally distributed between household (40%) and external environment with a slight predominance of the later (50%). One-tenth of the children sustained injuries which care providers could not locate, the children were not attended to by any adult or care provider. Physical trauma was the predominant mode of injury (92.5%), with mechanical trauma (88.3%), both blunt and sharp, being the most common. One child sustained an alkali injury and there was one case of suspected child abuse that could not be confirmed. Almost all study children were fully conscious (96.6%), except for 4 children with impaired consciousness and one comatose child. The clinical data of the injured eyes are presented in and . Corneal injuries represented the most common injuries in both right and left eyes, with abnormalities of the anterior chambers, intraocular pressure, and pupils subsequently.
Table 1. Study patients’ demographics.
Table 2. Circumstances of injury.
Table 3. Clinical data of traumatized eyes.
4. Discussion
This study was conducted to report on ocular injuries in children in a tertiary referral center. The study was conducted over a 7-month period and included 147 children, representing one-third of all ocular trauma cases referred to Alexandria Main University Hospital during the study period. The study was originally designed to cover half of a calendar year (6 months). However, within the study period, a local feast of about 2 weeks interrupted the study duration in which the authors feared would introduce a sampling error due to obvious change in the daily habits and life activities of the target population. In an attempt to dilute this effect, the authors extended the recruitment period for one extra month and hence the 7-month study duration. The fact that pediatric ocular injuries represent almost one-third of all ocular injuries reflects how much children are a vulnerable population to ocular injuries, especially in such underprivileged communities in developing countries, which is in accordance with the findings reported by Al Wadeai et al. [Citation9], by Khan et al. [Citation10] and by Wagle et al. [Citation2] in developing countries, and is much higher than that reported by Sii et al. [Citation11] in developed countries. Within the study cohort, it is obvious that younger age groups are more vulnerable than older age groups. Younger are more prone to an irresponsible behavior and lack of appreciation of potential hazards and areas of harm. This is in accordance with other published reports [Citation9,Citation11,Citation12]. Being more active and more exposed to outdoor activities and sometimes even involved in childhood labor especially in developing countries and rural communities, it is not surprising that more than 70% of the injured children were males as already highlighted [Citation2,Citation4,Citation9,Citation13,Citation14]. A striking finding in this study, unlike other reports [Citation4,Citation11], is the predominance of right eye injuries over left eyes. Although no obvious cause could be attributed to this finding in the study, yet the authors hypothesize that, at least theoretically, trauma may be self-inflicted, in which case the predominance of right-handedness may make the right eyes more vulnerable than left eyes, though this could never be confirmed.
Studying the geographic locale of the study participants reveals that almost half of the cases came from outside of Alexandria, the city where the referral center of the study is located. This reflects the advantageous location of the Alexandria Main University Hospital lying in the heart of its coverage area with better delivery of services to beneficiaries. The importance of the proximity of health services to beneficiaries cannot be overemphasized and is stressed upon in different studies [Citation9,Citation12,Citation15]. Rural areas outside of Alexandria represented the major input of the injured children, almost one-third, reflecting the more trauma-prone relatively hazardous practices, common to rural areas and agricultural communities, as already reported from other areas of the World [Citation4,Citation16]. A rather related issue is the care-provider profession, with manual laborers taking the major share. In the local community of the study coverage area, it is a common practice for manual laborers to be escorted by their youngsters, either as bystanders for entertainment or for actual participation in the job. This may expose their children to their work environment with its antecedent risks. To the best of the authors’ knowledge, this is the first study to report on the relation of the care-providers profession to childhood trauma.
Scrutiny of the circumstances of injury provides important insights. There was an almost equal incidence of occurrence of injuries in the household and external environments, reflecting the potential hazard of household environments, and especially so that the majority of injuries occurred in rural areas. Lack of adequate parental supervision might have been an additional factor, which might have contributed to the household environment being equally hazardous as the outdoor play areas and schools. More attention must be paid to ensure a child-friendly home environment or at least a hazard-free home setting for children, especially younger age group children. Closer attention must be paid to children at home by the care providers. Collaboration of the household is a potential source of care, though absolute safety can never be guaranteed. The significance of a hazardous environment in relation to childhood ocular injuries has already been emphasized [Citation11,Citation13]. Mechanical trauma, and especially blunt trauma, was the cause of the injuries in the majority of the injured children, in accordance with other studies [Citation12,Citation13,Citation17]. Although only one child sustained an alkali injury in this study, yet this case warrants significant attention due to the potentially blinding nature of such severe injuries.
Review of the clinical findings of the injured children demonstrates that corneal injuries represent the major injury sustained in the study cohort. Children are generally less careful on dealing with hazardous objects and activities than adults (and more so in younger than older children), and hence have a greater propensity for “relatively sudden” insults to the face with a high chance of injury to the cornea, the eyes occupying a larger surface area of the child’s face. Moreover, being the major refractive surface of the eye, it is not surprising that ocular injuries have poor visual prognosis in children. This relatively high prevalence of corneal injuries has been emphasized by other reports [Citation9,Citation12]. On the other hand, the remainder of the outer wall of the eye, namely the sclera, is less exposed (being relatively protected in the bony orbit), and is mechanically more robust than the cornea, hence less vulnerable to injury. Related to the outer wall of the eye and the occurrence of open injuries are the anterior chamber depth and IOP. The few eyes in which a ruptured globe was diagnosed yet the anterior chamber depth was normal represented cases of self-sealed corneal injuries. The difficulty of measuring the IOP in children is clearly reflected in a number of eyes in which it was not possible to assess the IOP and the reliance on the digital method rather than formal Goldmann applanation Tonometry (GAT) for the assessment of the vast majority of the injured eyes. The delicate structure of the iris and the pupil renders it vulnerable to injury with the majority of ocular injuries. The natural crystalline lens is another very delicate intraocular structure that is very vulnerable in children's eyes, as obvious in one-fourth of the eyes presenting with an abnormality in the natural crystalline lens. The lids, being the first anatomical structure and the first line of defense to the eyes, are commonly injured. Additionally, the delicate skin of children contributes to the higher incidence of open lid injuries (cuts and lacerations) than closed injuries (hematoma), even with blunt trauma. Although children bone is more brittle than adult bones, yet, orbital fracture still mandate significant force, hence were fortunately not common. This pattern of ocular injuries parallels that published in other studies [Citation4,Citation9]. The importance of imaging investigative tools in the setting of ocular trauma cannot be overemphasized, and especially so in cases of opaque media. Nevertheless, the need for relative patient cooperation and the occasional hazard of some tools, namely B-scan ultrasonography, were responsible for the relative scant resort to these investigative tools in this study.
This study has a number of limitations. The study covered a relatively short period and not covering a complete calendar year. This does not permit studying the effects of different social circumstances around the year, such as school environment injuries for instance. The study as well did not report on the interventions done for the treatment of the injured children or the final outcome of the injury and the treatment measures provided.
In conclusion, ocular injuries represent one-third of all ocular injuries in the study locale. Ocular injuries in children occur in both urban and rural areas with an almost equal distribution and in both household and external environments. Mechanical trauma, both blunt and sharp, is the most common cause of trauma in the current study.
Data availability
The corresponding author had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis as well as the decision to submit for publication. The study was not funded by any institution or body.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes on contributors
Nader Hussein Lotfy Bayoumi
Nader Bayoumi is a professor of Ophthalmology at the ophthalmology department, Faculty of Medicine, Alexandria University. He is specialized in glaucoma diagnosis and treatment especially pediatric glaucoma and has many published papers.
Rania AbdElFattah Hussein Mahmoud Eldakhs
Rania El Dakhs is an assistant lecturer of Ophthalmology at the ophthalmology department, Faculty of Medicine, Alexandria University. She is interested in scientific research and currently doing a fellowship in cornea and external eye diseases.
Monsef Ibrahim Kharboush
Monsef Kharboush is an assistant lecturer of Ophthalmology at the ophthalmology department, Faculty of Medicine, Alexandria University. She is interested in scientific research and currently doing a vitreoretinal surgery fellowship.
Noureldin Doaa Fathi Elsamman
Noureldin ElSamman is a 5th-year resident at the ophthalmology department, Faculty of Medicine, Alexandria University. He is interested in scientific research and vitreoretinal surgery.
Shahira Mahmoud
Shahira Mahmoud is a lecturer of Ophthalmology at the ophthalmology department, Faculty of Medicine, Alexandria University. She is specialized in anterior segment disease especially corneal diseases.
References
- Gupta P, Gupta V. Ocular morbidities in pediatric outpatient population at a tertiary care ophthalmic centre: a descriptive study. Int J Contemp Pediatr. 2018 Jul;5(4):1195–1198.
- Wagle N, Usgaonkar U, Naik P. Pediatric ocular morbidity profile in the inpatient department of a tertiary health care hospital in Goa. IOSR-JDMS. 2018;17(3):7–9.
- El-Sebaity DM, Soliman W, Soliman A, et al. Pediatric eye injuries in upper Egypt. Clin Ophthalmol. 2011;5:1417–1423.
- Wang W, Zhou Y, Zeng J, et al. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in South-Central China. Acta Ophthalmol. 2017 Sep;95(6):e503–e510. Epub 2017 Mar 30
- Brophy M, Sinclair SA, Hostetler SG, et al. Pediatric eye – related hospitalizations in the United States. Pediatrics. 2006;117(6):e1263-e1271.
- Al-Mahdi H, Bener A, Hashim S. Clinical pattern of pediatric ocular trauma in fast developing country. Int Emerg Nurs. 2011;19(4):186–191.
- Emerson MV, Jakobs E, Green WR. Ocular autopsy and histopathologic features of child abuse. Ophthalmology. 2007 Jul;114(7):1384–1394.
- Thompson CG, Kumar N, Billson FA, et al. The aetiology of perforating ocular injuries in children. Br J Ophthalmol. 2002;86(8):920–922.
- Al Wadeai EAY, Osman AA, Macky TA, et al. Epidemiological features of pediatric ocular trauma in Egypt. J Ophthalmology Article ID 7874084. 2016;2016:6.
- Khan MD, Kundi N, Mohammed Z, et al. A 6 1/2-years survey of intraocular and intraorbital foreign bodies in the North-west Frontier Province, Pakistan. Br J Ophthalmol. 1987;71(9):716e719.
- Sii F, Barry RJ, Abbott J, et al. The UK paediatric ocular trauma study 2 (POTS2): demographics and mechanisms of injuries. Clin Ophthalmol. 2018;12:105–111. cited 2018 Jan 9.
- Qayum S, Anjum R, Rather S. Epidemiological profile of pediatric ocular trauma in a tertiary hospital of northern India. Chin J Traumatol. 2018 Apr;21(2):100–103. cited 2018 Mar 3. .
- MacEwen CJ, Baines PS, Desai P. Eye injuries in children: the current picture. Br J Ophthalmol. 1999;83:933–936.
- Cao H, Li L, Zhang M, et al. Epidemiology of pediatric ocular trauma in the Chaoshan region, China, 2001–2010. PLoS ONE. 2013;8(4):e60844.
- Omolase CO, Omolade EO, Ogunleye OT, et al. Pattern of Ocular Injuries in Owo, Nigeria. J Ophthalmic Vis Res. 2011 Apr;6(2):114–118.
- Khatry SK, Lewis AE, Schein OD, et al. The epidemiology of ocular trauma in rural Nepal. Br J Ophthalmol. 2004 Apr;88(4):456–460.
- Puodžiuvienė E, Jokūbauskienė G, Vieversytė M, et al. A five-year retrospective study of the epidemiological characteristics and visual outcomes of pediatric ocular trauma. BMC Ophthalmol. 2018 Jan 18;18(1):10.