ABSTRACT
Introduction
The prevalence of Diabetes Mellitus (DM) is currently reported to be on the increase in the school environment among teachers and students in Africa. This review highlighted the current state of DM in primary and secondary schools in Africa.
Methods
The review assessed critical literature on African Journals Online, Google Scholar search, PubMed, Medline, and Science Direct as well as information available about DM in the Africa continent. Relevant search terms included prevalence of DM in primary schools, the prevalence of DM in secondary schools, prevalence of DM among teachers and students, knowledge of DM among teachers and students, risk factors of DM among teachers and students in Africa.
Results
The review highlighted the prevalence of T2DM among teachers, while prediabetes and T1DM were reported among students. Furthermore, only two studies were identified to assessing knowledge of DM among teachers while few studies reported poor knowledge of DM among students.
Conclusion
The issue of DM in both primary and secondary schools should be given the needed attention by the concerned stakeholders. This is because of the possible escalation of T1DM and T2DM within the school environment in Africa in the nearest future.
1. Introduction
Diabetes is a chronic, progressive disease characterized by elevated levels of blood glucose usually resulting in both microvascular and macrovascular complications [Citation1]. Diabetes Mellitus (DM) is one of the four conditions causing premature death and disability in lower and middle-income countries [Citation2]. According to the WHO estimates an estimated 422 million adults were living with diabetes in 2014, compared to 108 million in 1980 representing a rising prevalence from 4.7% to 8.5% in the adult population [Citation1]. The rising prevalence of DM is also reflected in Africa as an estimated 15.5 million adults aged 20–79 years have diabetes in Africa in the year 2017 and the number is expected to increase to 162.5% in the year 2045 [Citation3]. This increase has been attributed to an associated increase in risk factors such as obesity, overweight, alcohol, smoking, and physical inactivity.
The school is a place of learning and educating children to empower them with knowledge. However, while teachers are responsible for empowering students with knowledge based on well-defined objectives, students, on the other hand, need to assimilate and process the information to prevent contracting diseases. Diseases like DM are a threat to achieving health-promoting schools across Africa because as in the general population the problem of DM has been reported among teachers and students in primary and secondary schools across Africa. The implication of this development is students who were asymptomatic to DM are now adding to the burden of DM in the school environment which was already struggling with the burden of DM among teachers. Thus, this exploratory review was designed to highlight the problem of DM in schools across Africa as a way of creating awareness and stimulating increased research activities on DM in African schools.
2. Objectives of the review
1. To underline the prevalence of DM among teachers and students
2. To assess the knowledge of DM among teachers and students
3. To highlight the risk factors promoting DM among teachers and students
3. Materials and methods
Google search engine was used to access Google Scholar, African Journal Online, PubMed, Medline, and Science Direct related materials on prevalence and knowledge of DM in primary and secondary schools in Africa. In all 35 articles were accessed after exclusion of articles that were not in line with the study objectives. Only school-based studies among teachers and students that were carried out in Africa, knowledge of DM was determined and in which Fasting Blood Sugar (FBS) and Random Blood Sugar (RBS) were used to diagnose DM were included in the review. Furthermore, included studies were prospective or cross-sectional studies, and interventional studies published in the English language. Diabetes was diagnosed as fasting blood glucose (FBG)>7.0 mmol/l or >126 mg/dl, or a random blood glucose (RBG)>11.0 mmol/l or >200 mg/dl Classification [Citation4]. Search themes were developed from the study objectives to serve as guides to extract relevant information on prevalence and knowledge of DM in Africa. Information searched were prevalence of DM in primary schools, the prevalence of DM in secondary schools, prevalence of DM among teachers and students, knowledge of DM among teachers and students, risk factors of DM among teachers and students in Africa. The information collected was subjected to thematic analysis based on the objectives of the study. The findings were presented as critical prose highlighting the prevalence and knowledge of DM among teachers and students.
4. Prevalence of diabetes mellitus among teachers
Teachers occupy the role of teaching and caring for children in the school environment. This role by the teachers could be affected if the teachers were diagnosed with DM. This is because DM is a chronic disease that presents with numerous signs and symptoms and requires multi-facets daily and livelong management practices [Citation5–7]. Furthermore, the prevalence of DM has been projected to be on the increase in Africa with an estimated 15.5 million adults aged 20–79 years living with diabetes in the IDF Africa Region in 2017, representing a regional prevalence of 3.3% [Citation3]. The prevalence of DM has also been shown to be on the increase among teachers in schools in Africa who are subsets of the larger population. A cohort study among teachers in South Africa reported the prevalence of DM to be 10.10% [Citation8]. Similarly, another study in South-West Nigeria reported prevalence of DM to be 2.80% [Citation9] while another study in Tanzania East Africa reported the prevalence of DM among teachers to be 8.30% [Citation10] and a further study in Nigeria reported prevalence of DM among teachers to be 1.20% [Citation11]. Other studies in Africa that reported prevalence of DM among teachers were two studies in South Africa which detailed the prevalence of DM to be 13.50% [Citation12] and 2.0% respectively [Citation13].
5. Prevalence of diabetes mellitus among students
In Africa, the incidence and prevalence of DM are shown to be on the increase among children and teenagers. The estimated number of children < 20 years with T1DM in the African region was 50,200 [Citation3]. Nigeria, Algeria, and Morocco have been listed among the 10 highest number of countries with the number of new cases of T1DM (children and adolescents <20 years), per year in the world. The current trend suggests a possible escalation of DM among children and adolescents in Africa shortly. Children and adolescents <19 years are part of the population of secondary schools in Africa. Various studies have reported the prevalence of T1DM among secondary school students in Africa. For instance, a cross-sectional study in Cameroon reported the prevalence of TIDM to be 1.8% among students [Citation14], while a study in Nigeria reported the prevalence of Impaired Fasting Glucose to be 17.30% [Citation15] and a further study in Nigeria detailed the prevalence of T1DM among students to be 0.3% [Citation16]. Also, another study among girls in selected boarding secondary schools in the Wakiso district of Uganda showed a prevalence of pre-diabetes to be 6.40% [Citation17] and a cross-sectional study in Nigeria reported the prevalence of T1DM among students to be 0.6% and 28.70% for prediabetes [Citation18]. Also, a study investigating the prevalence of T1DM among school-age children in the Menoufia governorate in Egypt found the overall prevalence of T1DM to be 3.75/1000 [Citation19]. Besides, few studies have reported the prevalence of T2DM among adolescents in the general population in Africa [Citation20]. However, as at the time of putting this review together, there was the paucity of studies of T2DM carried out among primary and secondary school students in Africa.
6. Knowledge of diabetes mellitus among teachers
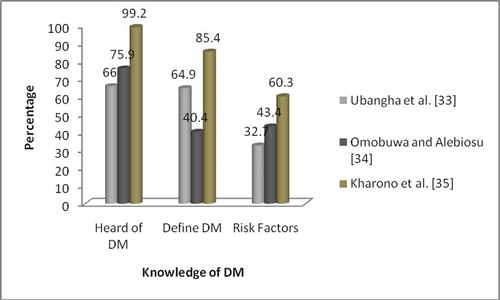
Knowledge of DM is crucial in prevention, management, and control of the disease. Various population-based studies in Africa have reported inadequate knowledge of DM among adults [Citation21–27]. However, there is a paucity of studies assessing the knowledge of DM among teachers in Africa. A study in Ghana by Amissah et al [Citation28] is as shown in . Also, another study that assessed the knowledge and practice of preventive measures against diabetes mellitus amongst Secondary School Teachers showed poor knowledge of DM with a mean knowledge score of the respondents was 31.76 ± 12.02% [Citation29]. Inadequate knowledge of DM remains a challenge in achieving optimum management outcomes of the disease in Africa [Citation30].
Figure 1. Knowledge of DM among teachers by Amissah et al [Citation28]
![Figure 1. Knowledge of DM among teachers by Amissah et al [Citation28]](/cms/asset/b443648a-d0f8-4822-a317-c26a29a2fab1/tajm_a_1833278_f0001_oc.jpg)
7. Knowledge of diabetes mellitus among students
The role of knowledge as a key factor in the prevention and management of DM cannot be overemphasized. This is so considering the increasing prevalence of the disease among children and adolescents [Citation31–35]. The knowledge of DM among students is shown in below.
In the same vein a comparative study that assessed the awareness and knowledge about DM and hypertension amongst adolescents in secondary schools in Oyo State shows that health club members who were aware of diabetes 95.0% were higher than those of none members 81.7%, 83.1% of health club members stated that obesity is a risk factor for diabetes mellitus as compared to 71.2% of non-club members, 81.40% health club members affirmed family history to be a risk factor for diabetes mellitus as compared to 68.40% of non-club members, 68.6% and 58.7% for decreased physical activity, and 35.1% and 31.7% for stress respectively. Furthermore, 85.5% of club members stated that diabetes can cause complications in other organs of the body as opposed to 66.0% of non-club members while 91.0% of club members stated that diabetes can be prevented as opposed to 79.5% of non-club members [Citation36]. Furthermore, another cross-sectional study carried out among in-school adolescents in Nigeria showed high awareness of diabetes among the students, less than half knew that diabetes meant an abnormally high blood glucose level, but only 2(0.2%) were aware that it was due to deficiency of insulin. Most of those who knew that diabetes was associated with raised blood glucose thought that the cause was an excessive intake of sugar and 37% could name at least two symptoms [Citation37]. An interventional study among students also showed inadequate knowledge of DM pre-intervention and improved knowledge of DM post-intervention [Citation38,Citation39].
8. Risk factors of Type-2 DM among teachers and students in Africa
8.1. Family history
Diabetes Mellitus is a hereditary disease that could be inherited by offspring from their maternal and paternal parents. Thus one of the major factors promoting the increasing prevalence of T2DM within the school environment is a family history of the disease. A review study in Nigeria showed one of the risks factors for the pooled prevalence of DM was a family history of DM (4.6%; 95% CI 3.5–5.6) [Citation40]. Other studies reported a family history of DM as a risk factor for contracting DM [Citation41,Citation42].
8.2. Increasing age
Another factor identified to be driving the prevalence of T2DM is increasing age especially among teachers. Life expectancy in Africa is gradually increasing as more people are growing older. This has been attributed probably because aging is often accompanied by a decline in lean body mass and an increase in body fat, particularly visceral adiposity which may contribute to the development of insulin resistance [Citation43]. Also, aging has been shown to induce a decrease in insulin sensitivity and inadequate response of β-cell functional mass and is also associated with a decrease of β-cell proliferative capacity [Citation44,Citation45]. Besides, studies in Africa have shown the association between increasing age and prevalence of DM [Citation40,Citation41,Citation46–48].
8.3. Physical inactivity
Lack of physical inactivity due to a sedentary lifestyle is fueling the increasing prevalence of DM in Africa. This is a characteristic of urban populations that have been exposed to westernization [Citation49]. Studies in Africa have reported physical inactivity as a risk factor for the increasing prevalence of DM [Citation9,Citation40,Citation46–52].
8.4. Obesity
Obesity defined by the World Health Organization as Body Mass Index >30 Kg/m2 [Citation53] is considered a major risk factor for type 2 diabetes [Citation54]. This is because the likelihood of the incidence of diabetes increases by a 2-3-fold factor in obese individuals [Citation55]. Obesity leads to insulin resistance by increasing the production of adipokines/cytokines, including tumor necrosis factor-α, resistin, and retinol-binding protein 4 [Citation56] and mitochondrial dysfunction by decreasing insulin sensitivity and by compromising β-cell function [Citation57]. Studies have highlighted obesity as a risk factor for the prevalence of DM [Citation41,Citation46,Citation55,Citation58–60].
8.5. Alcohol and smoking
It has been projected that developing countries like Africa will bear 77% of the global burden of the DM epidemic in the 21st century. This projected increase has been attributed mainly to unhealthy lifestyle habits such as smoking and alcohol [Citation61]. Studies have reported the association between alcohol and smoking as risk factors for DM prevalence [Citation40,Citation41,Citation46,Citation60,Citation62–64].
8.6. Unhealthy dietary habits
Consumption of unhealthy diets such as fatty foods, soft drinks, red meat, sweets, and fried foods has been highlighted to be contributing to the increasing prevalence of DM [Citation65–67]. The underlying risk factor prompting the onset of DM due to diet is nutritional imbalance due to high energy, fat, and cholesterol [Citation68]. Higher fat intake, intake of red meat, and higher intake of dairy products have all been associated with increased risk of DM [Citation69,Citation70]. On the other hand, fiber-rich diets, wholegrain, fruits, and vegetable consumption, and consumption of diets high in plant-based protein and fat were all associated with a lower risk of DM [Citation71,Citation72].
8.7. Problem of starvation
Starvation due to wars, famine, and poverty is prevalent in African countries. In some countries in Africa, about 50–60% of the population lives below 1 dollar per day making it difficult for them to afford three square meals. This state of undernutrition has been shown to have a relationship with the development of DM in adulthood as it causes morphological and functional changes in the key organs involved in the regulation of metabolic processes such as the pancreas [Citation73,Citation74]. Furthermore, during pregnancy unbalanced nutrition during fetal life may cause adipose tissue accumulation and pancreatic beta-cell dysfunction in the developing fetus [Citation75]. All these processes could allow adaptation to poor nutritional conditions by decreasing insulin production and establishing insulin resistance.
8.8. The way forward in the prevention of DM in schools
The increasing prevalence of both T1DM and T2DM among pupils/students and teachers in primary and secondary schools in Africa should be a source of concern to all stakeholders. This is because DM a disease thought to be prevalent in the developed world has now become a reality in the continent today, even among adolescents, youths, and young adults. The school environment is not spared of DM scourge as both teachers and students have been diagnosed with prediabetes, T1DM, and T2DM. Although, very little could be done in the prevention of T1DM because of its autoimmune response; much more could be done to prevent the onset of T2DM. Since the school is a place of learning, it seems to be the ideal place for the implementation of DM prevention programmes. Firstly, the creation of awareness about the DM remains one of the sure ways of preventing its prevalence in communities around Africa. More awareness of DM including its definition, signs and symptoms, risk factors, complications, and prevention must be carried out across primary and secondary schools. This would enable the correction of any myth associated with the disease and change the negative perception of the disease among students and teachers. Secondly, the curriculum of primary and secondary schools should be reviewed to include prevention of non-communicable diseases where it does not exist and in detail where it exists minimally. This would ensure knowledge of DM and other non-communicable diseases at an early stage and adoption of preventive measures thereby reducing the prevalence of DM either at the adolescent stage or in adulthood. The curriculum should highlight the benefits of healthy eating and physical activity options for both teachers and students. The importance of consuming healthy diets and engaging in physical activity should be taught through seminars for students and teachers in both primary and secondary schools. Teachers could engage in sports activities weekly, while sports activities could be organized for students regularly. For diets, a variety of healthy diets could be made into posters displayed in classrooms and staff rooms to encourage healthy eating among staff and students. Besides, a project like the Kids and Diabetes in Schools Project which was developed by the International Diabetes Federation could be redesigned and implemented in schools in Africa to foster a safe and supportive environment that creates a better understanding of diabetes and supports children with the condition. The availability of health insurance for both staff and students would ensure prompt and regular medical checkup and affordability of medications for those already diagnosed with the disease.
9. Limitation
This review is limited because only relevant materials that were available on online search engines were used in writing the review.
10. Conclusion
The review highlighted the prevalence of DM in the school environment. T2DM was reported among teachers while both prediabetes and T1DM were reported among students. Inadequate knowledge of DM was also reported among teachers and students as well as the proposed factors predisposing teachers and students to DM in the school environment. Therefore, all stakeholders from the Ministry of Education and Health at all levels of governance, including the primary and post-primary education boards, teachers union and parents association must come together to support the implementation of DM preventive programmes within the school environment to promote a healthy school environment and helping Africa to achieve the Sustainable Goal 3.
Disclosure statement
The authors report no conflict of interest
Additional information
Funding
Notes on contributors
Agofure Otovwe
Agofure Otovwe is a public health specialist with focus on Health Promotion and Education. He is an MPH holder and currently running his PhD program in the University of Ibadan. He is a member of professional academic bodies and has publications in both local and international journals.
Efegbere Henry Akpojubaro
Efegbere Henry Akpojubaro is a medical consultant with specialization in Public Health and Community Medicine. He has various certifications and as well as membership of various medical, management, social sciences professional bodies both within and outside Nigeria.
References
- World Health Organisation. Global report on diabetes. Geneva 27, Switzerland; 2016. http://www.who.int
- World Health Organization. Global health observatory. Non-communicable diseases country profile. Nigeria; 2010. http://www.who.int/nmh/ countries/nga_en pdf
- International Diabetes Federation. 2017. Diabetes Atlas 8th Edition. http://www.diabetesatlas.org.
- World Health Organization. Report of a WHO consultation: definition, diagnosis, and classification of diabetes mellitus and its complication. Part 1 diagnosis and classification of diabetes mellitus. Department of noncommunicable disease surveillance. Geneva: WHO; 2011.
- Agofure O, Oyewole OE, Igumbor EO, et al. Diabetes care in Delta State of Nigeria: an expository review. Diabetes Updates. 2018;1(1):1–8.
- Oyewole EO, Agofure O. Patterns of adherence to management among patients with type 2 diabetes mellitus in the South-South Region of Nigeria. J Soc Health Diabet. 2015;3:115–119.
- Fasanmade OA, Dagogo-Jack S. Diabetes care in Nigeria. Ann Glob Health. 2015;81:821–829.
- Laurence EC, Volmink J, Esterhuizen TM, et al. Risk of cardiovascular diseases among teachers in Cape Town: findings of the South African PaCT pilot study. SAMJ. 2016;106(10):996–1001.
- Ilesanmi OS, Ojo OA, Omotoso B, et al. Prevalence of diabetes mellitus and the associated behavioral risk factors among the staff of three secondary schools in Owo, Ondo State, Nigeria. Res J Health Sci. 2017;5(3).
- Chiwanga FS, Njelekela MA, Diamond MB, et al. Urban and rural prevalence of diabetes and pre-diabetes and risk factors associated with diabetes in Tanzania and Uganda. Glob Health Action. 2016;9:31440.
- Akintunde AA, Oloyede TW. Metabolic syndrome and occupation: any association? Prevalence among auto technicians and school teachers in southwest Nigeria. Diabetes Metab Syndr. 2017;11(Suppl 1):S223–S227.
- Dalal S, Holmes MD, Laurence C, et al. Feasibility of a large cohort study in sub-Saharan Africa assessed through a four-country study. Glob Health Action. 2015;8(1):27422.
- Senekal M, Seme Z, de Villiers A, et al. Health status of primary school educators in low socio-economic areas in South Africa. BMC Public Health. 2015;15:Article number:186.
- Kamdema F, Lemogoumb D, Jingic AM, et al. Prevalence and determinants of abnormal glucose metabolism in urban and rural secondary schools in Cameroon: A cross-sectional study in a sub-Saharan Africa setting. Prim Care Diabetes. 2019. DOI:10.1016/j.pcd.2019.02.006.
- Jaja T, Yarhere IE. Risk factors for type 2 diabetes mellitus in adolescents secondary school students in Port Harcourt, Nigeria. Niger J Paediatr. 2015;42(2):137–141.
- Okpere AN, Anochie IC, Eke FU. Prevalence of Microalbuminuria among secondary school children. Afr Health Sci. 2012;12(2):140–147.
- Nakiriba R, Mayega RW, Piloya T, et al. Prevalence and factors associated with dysglycemia among girls in selected boarding secondary schools in Wakiso District, Uganda. Adolesce Health Med Therapeutics. 2018;9:167–176.
- Oluwayemi IO, Brink SJ, Oyenusi EE, et al. Fasting Blood Glucose Profile among Secondary School Adolescents in Ado-Ekiti, Nigeria. J Nutr Metab. 2015;Article ID 417859:4.
- Hassan FM, Khatab AA, Abo El-Fotoh WM, et al. Prevalence of diabetes mellitus among school-age children. Menoufia Med J. 2019;32:305–310.
- Oluwayemi IO, Airemionkhale A. Type 2 diabetes in a Nigerian adolescent: diagnostic and management challenges in a resource poor setting. Int J Pediatrics Neonatal Health. 2017;1(3):74–76.
- Mufunda E, Ernersson A, Hjelm K. Limited knowledge of diabetes in patients attending an outpatient diabetes clinic at a referral hospital in Zimbabwe: a cross-sectional study. Pan Afr Med J. 2018;29:144.
- Mufunda E, Wikby K, Björn A, et al. Level and determinants of diabetes knowledge in patients with diabetes in Zimbabwe: a cross-sectional study. Pan Afr Med J. 2012;13:78.
- Gebremichael LG, Abdurahman AA, Periasamy G. Assessment on knowledge of diabetic patients on their disease and therapeutic goal at ayder referral Hospital, Mekelle, Ethiopia. J Drug Deliv Therap. 2014;4(3):164–170.
- Ben Abdelaziz A, Thabet H, Soltane I, et al. Knowledge of patients with type 2 diabetes about their condition in Sousse, Tunisia. East Mediterr Health J. 2007;13(3):505–514.
- Mabaso RG, Oduntan OA. Knowledge and practices related to diabetes mellitus among adults with diabetes in the Mopani District, Limpopo Province, South Africa. Afr Vision Eye Health. 2016;75(1):a324.
- Agofure O, Efegbere AH, Odje AE. Knowledge of dietary and medical management of type-2 diabetes in an urban and rural community of Delta State Nigeria. AfrJ Diabetes Med. 2018;26(1).
- Oguoma VM, Nwose EU, Bwititi PT. Cardiovascular disease risk prevention: a preliminary survey of baseline knowledge, attitude, and practices of a Nigerian rural community. North Am J Med Sci. 2014;6:466–471.
- Amissah I, Barnes NA, Craymah JP, et al. Knowledge of diabetes mellitus and management practices among senior high school teachers in Ghana. Int J Sci Res. 2017;6(1).
- Ubajaka CF, Okafor CO, Adogu POU, et al. Knowledge and practice of preventive measures against diabetes mellitus amongst secondary school teachers in Awka South LGA of Anambra State, Nigeria. Int J Diabet Res. 2019;2(1):50–56.
- Oguejiofor O, Odenigbo C, Onwukwe C. Diabetes in Nigeria: impact, challenges, future directions. Endocrinol Metabolic Syndrome. 2014;3:130.
- John C, Abok II, Yilgwan C. Clinical profile of childhood type 1 diabetes mellitus in Jos, Nigeria. Afr J Diabete Med. 2013;11:11–13.
- Chuang LM, Wei JN, Sung FC, et al. Incidence and prevalence of childhood diabetes in Taiwan: an experience with nationwide mass screening. Diabetes Res Clin Pract. 2006;86:S165.
- Ubangha LO, Odugbemi TO, Abiola AO. Diabetes mellitus: identifying the knowledge gaps and risk factors among adolescents attending a public school in Lagos State. J Clin Sci. 2016;13:193–198.
- Omobuwa O, Alebiosu OC. Awareness of diabetes amongst undergraduates in a Nigerian University, South-West Nigeria. Sahel Med J. 2014;17(1):29–33.
- Kharono B, Nabisere R, Persis NK, et al. Knowledge, attitudes, and perceived risks related to diabetes mellitus among university students in Uganda: a cross-sectional study. East Afr Health Res J. 2017;1(2):105–112.
- Omisore AG, Alebiosu CO, Abe OS, et al. Awareness and knowledge about diabetes mellitus and hypertension amongst adolescents in secondary schools, Oyo State, Nigeria– an interventional Study by the +SIDCAIN Research Group. Res J Health Sci. 2014;2(2).
- Okoh BA, Jaja T. Knowledge and awareness of diabetes among adolescents in Port Harcourt, Nigeria. AfrJ Diabetes Med. 2014;22:18–20.
- Mhlongo M, Marara P, Bradshaw K, et al. Health education on diabetes at a South African national science festival. Afr J Health Professions Educ. 2018;10(1):26–30.
- Srinivas SC, Wrench WM, Bradshaw K, et al. Diabetes mellitus: preliminary health-promotion activity based on service-learning principles at a South African national science festival. JEMDSA. 2011;16(2):101–106.
- Uloko AE, Musa BM, Ramalan MA, et al. Prevalence and risk factors for diabetes mellitus in Nigeria: a systematic review and meta-analysis. Diabetes Therapy. 2018;9(3):1307–1316.
- Asiimwe D, Mauti GO, Kiconco R. Prevalence and risk factors associated with Type 2 diabetes in elderly patients aged 45-80 years at Kanungu District. J Diabetes Res. 2020. DOI:10.1155/2020/5152146 |Article ID 5152146 × 5 pages |
- Amarasinghe S, Balakumar S, Arasaratnam V. Prevalence and risk factors of diabetes mellitus among adults in Jaffna District. Ceylon Med J. 2015;60:107–110.
- Björntorp P. Metabolic implications of body fat distribution. Diabetes Care. 1991;14:1132–1143.
- Maedler K, Schumann DM, Schulthess F, et al. Aging correlates with decreased beta-cell proliferative capacity and enhanced sensitivity to apoptosis: A potential role for Fas and pancreatic duodenal homeobox-1. Diabetes. 2006;55:2455–2462.
- Meneilly GS, Elliott T. Metabolic alterations in middle-aged and elderly obese patients with type 2 diabetes. Diabetes Care. 1999;22:112–118.
- Arugu GM, Maduka O. Risk factors for diabetes mellitus among adult residents of a rural District in Southern Nigeria: implications for prevention and control. Niger J Clin Pract. 2017;20:1544–1549.
- Sabir AA, Balarabe S, Sani AA, et al. Prevalence of diabetes mellitus and its risk factors among the suburban population of Northwest Nigeria. Sahel Med J. 2017;20(4):168–172.
- Omar SM, Musa IR, ElSouli A, et al. Prevalence, risk factors, and glycaemic control of type 2 diabetes mellitus in eastern Sudan: a community-based study. Ther Adv Endocrinol Metab. 2019;10:1–8.
- Gatimu SM, Milimo BW, Sebastian MS. Prevalence, and determinants of diabetes among older adults in Ghana. BMC Public Health. 2016;16:1174.
- Lachat C, Otchere S, Roberfroid D, et al. Diet and physical activity for the prevention of non-communicable diseases in low- and middle-income countries: a systematic policy review. PLoS Med. 2013;10(6):e1001465.
- Sobngwi E, Mbanya JCN, Unwin NC, et al. Physical activity and its relationship with obesity, hypertension, and diabetes in urban and rural Cameroon. Int J Obes. 2002;26(7):1009–1016.
- Longo-Mbenza B, Kasiam Lasi On’kin JB, Nge Okwe A, et al. Metabolic syndrome, aging, physical inactivity, and incidence of type 2 diabetes in general African population. Diab Vasc Dis Res. 2010;7(1):28–39.
- WHO. Physical status: the use of and interpretation of anthropometry. Geneva, Switzerland: Report of a WHO Expert Committee, World Health Organization; 1995.
- WHO. Obesity: preventing and managing the global epidemic. Geneva, Switzerland: World Health Organization; 2000.
- Mugharbel KM, Al-Mansouri MA. Prevalence of obesity among type 2 diabetic patients in Al-Khobar primary health care centers. J Family Community Med. 2003;10(2):49–53.
- Deng Y, Scherer PE. Adipokines as novel biomarkers and regulators of the metabolic syndrome. Ann New York Academic Sci. 2010;1212:E1–19.
- Bournat JC, Brown CW. Mitochondrial dysfunction in obesity. Curr Opin Endocrinol Diabetes Obes. 2010;17:446–452.
- Sabir AA, Isezuo SA, Ohwovoriole AE. Dysglycaemia and its risk factors in an urban Fulani population of Northern Nigeria. West Afr J Med. 2011;30:325–330.
- Ekpenyong CE, Akpan UP, Nyebuk ED, et al. Gender and age-specific prevalence and associated risk factors of type 2 diabetes mellitus in Uyo metropolis, South Eastern Nigeria. Diabetol Croat. 2012;41:17–28.
- Tuei VC, Maiyoh GK, Ha CE. Type 2 diabetes mellitus and obesity in sub-Saharan Africa. Diabet Metabolism Res Rev. 2010.
- Chi-Shing Cho W, Kin-Man Yue K, Wing-Nang LA. An outline of diabetes mellitus and its treatment by traditional Chinese medicine & acupuncture. J Chinese Med. 2005;1:78.
- Ogbera AO, Ekpebegh C. Diabetes mellitus in Nigeria: the past, present, and future. World J Diabetes. 2014;5:905–911.
- Ruhembe CC, Mosha TC, Nyaruhucha CN. Prevalence and awareness of type 2 diabetes mellitus among the adult population in Mwanza city, Tanzania. Tanzanian J Health Res. 2014;16:89–97.
- Abebe SM, Berhane Y, Worku A, et al. Diabetes mellitus in North West Ethiopia: A community-based study. BMC Public Health. 2014;14:97.
- Nseir W, Nassar F, Assy N. Soft drinks consumption and nonalcoholic fatty liver disease. World J Gastroenterol. 2010;16:2579–2588.
- Assy N, Nasser G, Kamayse I, et al. Soft drink consumption linked with fatty liver in the absence of traditional risk factors. Can J Gastroenterol. 2008;22:811–816.
- Amin TT, Al-Sultan AI, Ali A. Overweight and obesity and their association with dietary habits, and socio-demographic characteristics among male primary school children in Al-Hassa, Kingdom of Saudi Arabia. Indian J Community Med. 2008;33:172–181.
- Dario G, Ceriello A, Esposito K. The effects of diet on inflammation. J Am Coll Cardiol. 2006;48(4):677–685.
- Tong X, Dong JY, Wu ZW, et al. Dairy consumption and risk of type 2 diabetes mellitus: A meta-analysis of cohort studies. Eur J Clin Nutr. 2011;65(9):1027–1031.
- Pan AN, et al. Red meat consumption and risk of type 2 diabetes: 3 Cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94(4):1088–1096.
- Mohan V, Radhika G, Sathya RM, et al. Dietary carbohydrates, glycaemic load, food groups, and newly detected type 2 diabetes among the urban Asian Indian population in Chennai, India (Chennai Urban Rural Epidemiology Study 59). Br J Nutr. 2009;9:1–9.
- Aune D, Norat T, Romundstad P, et al. Whole-grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidemiol. 2013;28(11):845–858.
- Kim JB. Dynamic cross talk between metabolic organs in obesity and metabolic diseases. Exp Mol Med. 2016;48(3).
- Zabuga OG, Vaiserman AM. Malnutrition in early life and risk of type 2 diabetes: theoretical framework and epidemiological evidence. Moscow Univ Biol Sci Bull. 2017;72(2):37–46.
- Nielsen JH, Haase TN, Jaksch C, et al. Impact of fetal and neonatal environment on beta cell function and development of diabetes. Acta Obstet Gynecol Scand. 2014;93(11):1109–1122.