ABSTRACT
Background: The quality of soft tissue reconstruction in upper and lower extremities caused by trauma, infection, burns, and tumor resection affects the patient function and esthetic outcome. Many flaps have been described in the literature to reconstruct such defects. Medial sural artery perforator flap is one of the options for reconstruction of upper and lower extremities.
Patients and methods: Starting from July 2019 through August 2020, 20 pedicled and free MSAP flaps were used for reconstruction of upper and lower limbs soft tissue defects.
Results: total flap loss occurred in two cases, partial flap loss occurred in two cases and the flap was abandoned in two cases. Otherwise, all flaps survived well.
Conclusion: MSAP flap is an excellent option in the reconstruction of soft tissue defects in upper and lower extremities.
1. Introduction
Reconstruction of upper and lower extremities requires a thin flap [Citation1]. The radial forearm flap had gained popularity in the past but with the disadvantage of significant donor site morbidity. The medial sural artery perforator flap can be used in soft tissue reconstruction of the head and neck, upper, and lower extremities. MSAP was first described by Cavadas et al. in 2001 [Citation2]. It was first used for lower limb reconstruction and then the clinical application was increased to include reconstruction of upper extremity, head, and neck [Citation3].
The advantages of MSAP are: its perforator allows an elevation of the skin leaving the medial gastrocnemius muscle intact preserving function. It can also be elevated with the muscle to fill the defect with low donor site morbidity. It has a long pedicle that allows an elevation of the island flap to reconstruct soft tissue defect around the knee and lower thigh. In case of free flap reconstruction around the knee the surgeon can use its pedicle as a recipient's vessel to avoid deeper dissection and the use of vein graft. It is also a thin flap even in obese patients [Citation4].
The main disadvantages of MSAP are: the scar in the donor site especially for women would be unaccepted, late congestion, and sometimes it is not available to harvest the flap as the perforator may be diminutive or originate from the medial sural artery [Citation5].
The versatility of MSAP comes from its ability to be elevated as a thin fasiocutaneous flap or elevated with the underlying gastrocnemius muscle to fill the deep defect or it can also be elevated as a chimeric flap. The sural nerve, the lesser saphenous vein, or the plantaris tendon can also harvest within the flap [Citation6,Citation7].
2. Aim of the work
The aim of the work was to evaluate the feasibility of the medial sural artery perforator flap either pedicle or free in the reconstruction of soft tissue defect in upper and lower extremities regarding etiology, defect area, flap size, color, thickness, and recipient vessels in free flaps, donor site closure, and morbidity.
3. Patients
This study was carried out for 20 patients with soft tissue defects in upper and lower extremities due to trauma, surgical release of post-burn contractures, or oncological resection in Alexandria University hospitals.
3.1. Exclusion criteria
Defects can be managed by simpler methods of reconstruction such as skin grafts.
A large defect that cannot be managed by MSAP flap.
Contraindication to free flap
The medical status that precludes an extended operative procedure.
History of coagulopathy resulting in a hypercoagulable state like polycythemia.
4. Methods
All patients were subjected to the following:
4.1. Clinical study
History taking including the present history of the mechanism of injury, past history of (trauma, fracture, infection, etc.), and any medical problems.
Physical examination and accurate assessment of the defect including length, width, and template design of the defect.
Routine laboratory investigations with special interest on bleeding and coagulation profile.
Informed consent was obtained fro each patient (guardian in pediatric patients) after a thorough explanation of the procedure.
4.2. Radiological examination
Duplex ultrasound:
Assessment of the perforators regarding their course, diameter, and continuity before the operation with marking using high resolution superficial 7–10 MHZ probe.
4.3. Surgical procedure
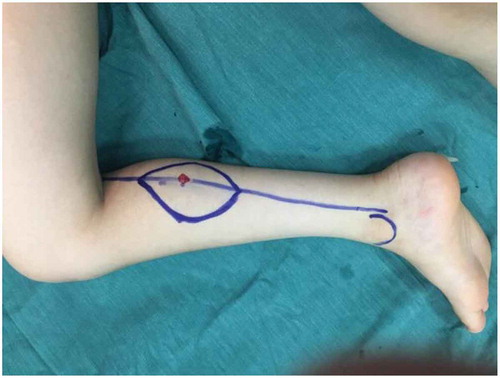
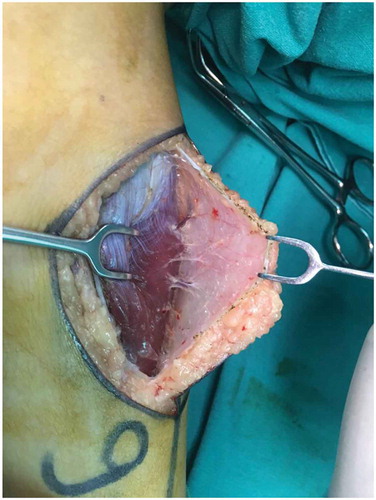
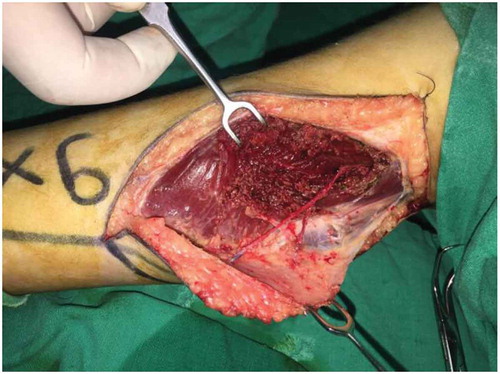
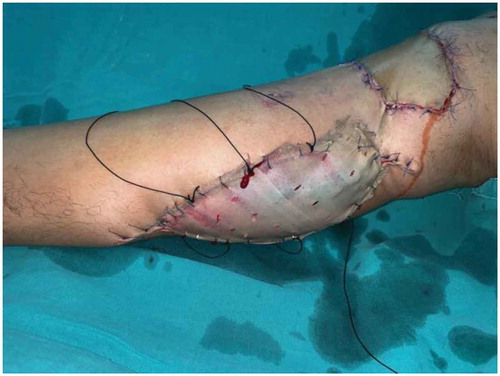
The patient was usually placed in a supine position with the hip abducted and knee flexed in a frog-like position. The main sizable perforator is usually located 8 cm distal to the popliteal crease located on a line from the middle of the popliteal crease to the medial calcaneus as demonstrated in . If more than one perforator was present, they are usually located further distally up to 15 cm distal to the popliteal crease. The medial border of the flap was elevated first to confirm the location and size of the perforators as demonstrated in . When one or two sizable perforators were identified, the opposite border was then incised and the flap elevated. The pedicle was then freed from the medial head of the gastrocnemius muscle through an intramuscular dissection as demonstrated in . Hemostasis was meticulously carried out using bipolar cautery. Basically, the course of the main trunk of the vascular pedicle is parallel to the gastrocnemius muscle fibers and can be exposed by splitting the muscle rather than cutting through it. The pedicle may be dissected 9 to 16 cm in length, and if possible, we harvest a superficial vein to secure venous outflow. In the case of pedicle flap transfer is through direct transposition to cover the defect which was either on the popliteal fossa, knee, or upper third of the leg. In cases of free flaps, the pedicle was cut and the flap transferred to the recipient site through the microvascular anastomosis. Donor site closure through direct closure or skin graft [Citation8] as demonstrated in .
5. Results
From July 2019 to August 2020 twenty MSAP flaps were performed for upper and lower extremities soft tissue defects: 10 pedicles and 10 free, six for upper limb and 14 for lower limb, six females and 14 males. The ages range from 6 to 56 years old.
The flap lengths range from 8 to 14 cm, the widths from 5 to 8 cm, the artery diameters from 1 to 2 mm, the veins diameters from 1.5 to 2.5 mm, and the pedicle lengths from 10 to 12 cm.
In our study, 14 patients (70%) passed and in six patients (30%) flaps failed: two had total flap loss, two had partial flap loss, and two with unreliable perforators during the operations and we changed the plan.
5.1. Case 1
Male patient 9 years old with crushed right hand treated by free MSAP as demonstrated in .
Figure 6. Case 1. a: Palmer surface of right hand showing soft tissue defect. b: Dorsal surface of right hand showing soft tissue defect. c: Flap marking. d: Anastomosis site. e: Dissection of the perforator. f: Dissection of the pedicel. g: Flap in-setting Palmer surface. h: Flap in-setting dorsal surface. i: Donor side closure. j: Patient after 1 week. k: Patient after 1 month. l: Patient after 3 months. m: Patient after separation of index finger. n: Patient during separation of middle and ring fingers showing the perforator. o: Patient after 6 months. p: Patient after 6 months. q: Patient after 6 months. r: Patient after 8 months

The data of the patients included in this study, as well as the criteria of the flaps, are summarized in
Table 1. Summary of the data of the patients included in this study
5.2. Case 2
Male patient 9 years old with post-traumatic contracture and recurrent ulceration of the right ankle treated by free MSAP as demonstrated in . The sural nerve was harvested with the flap and anastomosed to the posterior tibial nerve to provide sensation to the flap.
Figure 7. Case 2. a: Pre-operative photo showing the defect. b: Intraoperative photo showing the defect. c: Flap marking. d: Perforator dissection. e: Flap elevation. f: Flap insetting. g: Patient after 2 weeks. h: Patient after 2 months with good color match and thickness. i: Patient after 3 months. j: Donor side hypertrophic scar

5.3. Case 3
Female patient 7 years old with post-burn contracture of the left knee treated by pedicle MSAP as demonstrated in
Figure 8. Case 3. a: The defect in the left knee. b: Marking of the flap. c: Excision of the defect. d: Dissection of the perforator. e: Flap elevation. f: Flap insetting. g: Patient after 1 week. h: Patient after 1 month. i: Patient after 5 months. j: Patient after 11 months with good color match and thickness

6. Discussion
In our study, 12 patients have a single perforator and eight patients have double perforators and this is different from other researches which proved that most patients had more than a single perforator except the study made by Chen et al. [Citation9] which said that most patients had a single perforator.
The causes of the defects were post-traumatic in 13 patients, one case post tumor excision, and sex cases post-burn contractures.
Regarding other researches, Kao et al. [Citation10] said that the total perforators’ number was from 1 to 5 but the number of sizable was from 1 to 3 and the main pedicle length was 12.7 cm. Okamoto et al. [Citation11] proved that there were 1 to 5 perforators no one was higher than 5 cm and no one was lower than 17.5 cm. In 16 patients 36% there were 2 perforators the proximal one was found at a mean of 9,6 cm from the popliteal crease and the distal one at 12 8 cm. Nugent et al. [Citation12] said that the pedicle length was between 11 and 18 cm, arterial diameter was between 1 and 2 mm and venous diameter was between 2 and 6 mm. Toyseskani et al. [Citation8] said that the flap lengths were between 7 and 14 cm with a mean of 10 cm, widths between 3.5 and 8 cm with a mean of 5 cm, and the pedicle lengths were between 8 and 12 cm with a mean of 10 cm. Cavadas et al. [Citation2] described that the total number of perforators was between 1 and 4 with a mean of 2.2 and in most patients, there were 2 perforators at a mean of 11.8 cm and 17 cm from the popliteal crease. Balan et al. [Citation13] described that the mean flap size was 14.29 × 6.6 cm and the mean pedicle length was 9.71 cm.
According to the size of perforators, we had 18 patients (90%) with good size perforators and 2 patients (10%) with unreliable perforators and we changed the plan intraoperative. The first patient had soft-tissue defect post-marjolin ulcer in the upper third of the left lower limb, and after excision with a safety margin during the elevation of the flap we found a small-caliber perforator and we changed the plan intraoperative. The second patient is a child with a crush left hand and after debridement and elevation of the flap we found during microvascular anastomosis a small-caliber artery and we changed the plan intraoperative. In comparison with other research made by Toyserkani et al. [Citation8], we found the same result but the research was made on 10 patients and in 9 patients (90%) the perforators were reliable and in one patient (10%) the perforator was very small so the plan was changed.
In our study, 14 patients (70%) passed and in six patients 30% flaps failed: two had total flap loss, two had partial flap loss, and two with unreliable perforators during the operations and we changed the plan.
The first total flap loss was a male patient with a soft tissue defect in the lower third in the left lower limb due to a road traffic accident. He was admitted to Alexandria Main University Hospital in the Emergency Department. The first aid and stay suture of multiple traumatic flaps were done. Flap necrosis and exposure of tendon-Achilles occurred. We decided to cover the defect with an MSAP flap. The flap was elevated with a dimension of 6 × 9 cm, a single perforator at 10 cm from the popliteal crease, and with an elevation of the short saphenous vein. In the setting of the flap was done and the flap was in a good condition intraoperative. During the first day post-operative we observed a hematoma under the flap and a change in the color. Urgent re-exploration was done and we found slippage of the micro clip of the distal runoff. Evacuation of the hematoma and good hemostasis was done and the flap was in a good condition. Despite a regular follow-up and venous drainage through a saphenous vein, during the third post-operative day we observed venous congestion of the flap, and although efforts to salvage the flap it was lost.
The second patient complained of a soft tissue defect in the lower third in the left lower limb post-RTA. He was admitted to Alexandria Main University Hospital. MSAP-free flap was elevated with a dimension of 5 × 8 cm, double perforator at 10 and 12 cm from the popliteal crease. A good microvascular anastomosis was done with a single artery and vein to posterior interosseous artery and vena-comitant. During the second day follow up we found venous congestion of the flap and although major efforts to salvage the flap it was lost.
We had two patients with soft tissue defects reconstructed with pedicle MSAP flaps were subjected to partial flap necrosis. The first case suffered from the hematoma and venous congestion and the second from venous congestion only. Evacuation of hematoma in the first case and trials to deal with venous congestion with topical therapy, negative pressure therapy, and leach therapy failed to completely salvage the flaps and partial flap necrosis occurred. The first case after debridement healed by secondary intention and the second case needed a skin graft.
The results of flap success in other studies were: Kao et al. [Citation10] had one failed case from 29 patients, Agrawal et al. [Citation14] worked on 10 patients with one failed case, Toyserkani et al. [Citation8] had worked on 10 patients with 6 uncomplicated cases, 2 total flap losses due to venous congestion, one case had a venous problem that was salvaged and one the flap was changed intraoperative, Chen et al. [Citation9] worked on 11 patients with one flap failed, Shun et al. [Citation15,Citation16] worked on 31 patients with one flap failed due to pressure on the pedicle and Balan et al. [Citation13] worked on seven patients with one flap has a partial loss.
The sural nerve was harvested with the flap in two cases to render it a sensate one. Both patients suffered the paraesthesia encountered with sural nerve harvest (Outer part of the dorsum of the foot). Otherwise, the remaining 18 patients did not suffer any sensory deficit in the donor limb as a result of flap harvest.
Regarding the complications of the flap, we had two patients with hematoma and venous congestion, two patients with venous congestion, and one patient with an infection. Dealing with patients with hematoma was done through evacuation and hemostasis. In patients with venous congestion, we tried to conserve the flaps with topical therapy, negative pressure wound therapy, and leach therapy. In patients with an infection, we managed with frequent dressing and intravenous antibiotics.
The risk of venous congestion was the most common cause of flap failure and had been decreased by harvesting the short saphenous vein and enhancing the venous drainage through supercharging technique by double venous anastomosis or phlebotomy technique to aid in venous drainage. Toyserkani et al. [Citation8] recommended harvesting superficial veins in order to secure venous drainage. Venous congestion is the most common cause of flap loss as described by other literature. In our study donor site closure was performed primarily in 11 patients and skin grafts were needed in 9 patients. In comparison, with other researches Agrawal et al. [Citation14] said that all donor sites in 10 patients were closed primary and Nugent et al. [Citation12] said that the donor site in 6 patients was closed primary in 5 patients and a skin graft was needed in one patient.
Regarding donor site complications we had two patients (10%) with hypertrophic scars. One case was suffered from infection, wound dehiscence and healing occurred by secondary infection after frequent dressing and prompt antibiotic therapy. Toyserkani et al. [Citation8] had no donor site complications. Balan et al. [Citation13] had 2 donor sites' morbidity in the form of wound dehiscence.
MSAP has a relatively long pedicle so can reach as an island flap to cover the knee without microvascular anastomosis with the advantage to preserve the gastrocnemius muscle [18].
Our study includes patients with post-burn contractures in the hand and knee regions. Patients with contractures in the knee region were treated by surgical release and reconstruction using a pedicle MSAP flap with the advantage of good color and texture and alleviate the risk of contracture of skin graft.
In our study, we used preoperative duplex to locate the perforator and intraoperative hand-held Doppler and they were sufficient.
7. Conclusion
The MSAP is an easy, reliable flap, with low morbidity at the donor site. It can utilizedbe for the reconstruction of small-sized defects either in the upper or lower limbs. The sensate variant provides both soft tissue and nerve reconstruction.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Notes on contributors
Shereif Ibrahim Salah Eldin Hegazy
Shereif Ibrahim Salah Eldin hegazy Assistant lecturer of Plastic and Reconstructive Surgery, Faculty of Medicine, Port Said University.
Nasser Ahmed Gozlan
Nasser Ahmed Gozlan Professor of Plastic and Reconstructive Surgery, Faculty of Medicine, Alexandria University. Fellow of Vienna University, Austeria.
Hossam Yehia Elkafrawi
Hossam Yehia Elkafrawi Assistant Professor of Plastic and Reconstructive Surgery, Faculty of Medicine, Alexandria University. Fellow of UZ Gent, Belgium.
Mohamed Mahmoud Elshafei
Mohamed Mahmoud Elshafei Assistant Professor of Radiodiagnosis and Intervention, Faculty of Medicine, Alexandria University. Consultant in ICC Radiology center , Alexandria. Consultant in Almadina Scan Radiology center, Alexandria.Consultant in Elsafwa Scan Radiology center, Alexandria.
Hassan Mahmoud Kholosy
Hassan Mahmoud Kholosy Assistant Professor of Plastic and Reconstructive Surgery, Faculty of Medicine, Alexandria University, Egypt. Fellow of the European Board of Plastic, Reconstructive, and Aesthetic Surgery (EBOPRAS). Fellow of Barmherzige Brueder Hospital, Salzburg, Austria.
References
- Levin LS, Erdmann D. Primary and secondary microvascular reconstruction of the upper extremity. Hand Clin. 2001;17(3):447–455. https://pubmed.ncbi.nih.gov/11599212/
- Cavadas PC, Sanz-Gimenez-Rico JR, Gutierrez-de la Camara A, et al. The medial sural artery perforator free flap. Plast Reconstr Surg. 2001;108(6):1609–1615.
- Jandali Z, Lam MC, Aganloo K, et al. The free medial sural artery perforator flap: versatile option for soft tissue reconstruction in small-to-moderate size defects of the foot and ankle. Microsurgery. 2018;38(1):34–45.
- Kim KN, Kim SI, Ha W, et al. Popliteal fossa reconstruction with a medial sural artery perforator free flap using the medial sural vessel as the recipient. J Plast Surg Hand Surg. 2017;51(6):387–392.
- Hallock GG. Medial sural artery perforator free flap: legitimate use as a solution for the ipsilateral distal lower extremity defect. J Reconstr Microsurg. 2014;30(3):187–192.
- Sano K, Hallock GG, Hamazaki M, et al. The perforator-based conjoint (chimeric) medial Sural (medial gastrocnemius) free flap. Ann Plast Surg. 2004;53(6):588–592.
- Hwang MK, Chu SC, Hwang SM, et al. The usability of medial sural artery perforator flap for reconstruction of the finger defects. J Korean Soc Surg Hand. 2015;20(4):153–160.
- Toyserkani NM, Sørensen JA. Medial sural artery perforator flap: a challenging free flap. Eur J Plast Surg. 2015;38(5):391–396.
- Chen SL, Chen TM, Lee CH. Free medial sural artery perforator flap for resurfacing distal limb defects. J Trauma. 2005;58(2):323–327.
- Kao HK, Chang KP, Chen YA, et al. Anatomical basis and versatile application of the free medial sural artery perforator flap for head and neck reconstruction. PlastReconstrSurg. 2010;125(4):1135–1145.
- Okamoto H, Sekiya I, Mizutani J, et al. Anatomical basis of the medial sural artery perforator flap in Asians. Scand J Plast Reconstr Surg Hand Surg. 2007;41(3):125–129.
- Nugent M, Endersby S, Kennedy M, et al. Early experience with the medial sural artery perforator flap as an alternative to the radial forearm flap for reconstruction in the head and neck. Br J Oral Maxillofac Surg. 2015;53(5):461–463.
- Balan JR. Medial sural artery perforator free flap for the reconstruction of leg, foot and ankle defect: an excellent option. ANZ J Surg. 2018;88(3):E132–e6.
- Agrawal G, Gupta A, Chaudhary V, et al. Medial sural artery perforator flap for head and neck reconstruction. Ann Maxillofac Surg. 2018;8(1):61–65.
- Hsiang-Shun S, Kokkoli E, Jeng S-F. Medial sural artery perforator flap a practical way of optimizing the harvesting procedure. Plast Reconstr Surg. 2015;136(4S):167.
- Hallock G. The medial sural artery perforator island flap as a simpler alternative for prophylactic skin augmentation prior to total knee arthroplasty. Int J Ortho Surg. 2019;2(1):1–4.