ABSTRACT
Introduction: Hypotension is the most frequent consequence of spinal anesthesia in cesarean section. It results in harmful effects on mother and newborn.
Aim: This study aim was to evaluate the correlation of positional changes in hemodynamic (heart rate and blood pressure) measured before spinal anesthesia in anticipation of occurrence of hypotension throughout cesarean delivery.
Methods: 100 ASA grade I parturient were selected for this prospective observational study. Preoperative sociodemographic data, parity, and hemodynamic parameters were recorded including changes in systolic, diastolic, mean arterial blood pressure, and heart rate after positional shift from supine to lateral and sitting positions. Intraoperative, occurrence of hypotension was noted.
Results: With hypotension as the dependent variable, the age, parity, heart rate at supine position, and changes in (heart rate, systolic, diastolic and mean arterial blood pressure) from supine to lateral position, and from supine to sitting position had high statistical significant negative correlation with blood pressure as P value <.05. Multivariate logistic analysis to assess predictors of hypotension concluded that changes in hemodynamic variable from supine to lateral position only significant predictor were (∆ heart rate, ∆ diastolic and ∆ mean blood pressure), and changes in hemodynamic variable from supine to sitting position only significant predictor were (∆heart rate and ∆ diastolic blood pressure).
Discussion: Elevated sympathetic activity before neuraxial anesthesia was associated with higher risk for post-spinal hypotension. The great variability in hemodynamic after positional change indicates higher sympathetic activity to blood vessels. The high rise in the autonomic activity, the higher the risk for post-spinal hypotension
Conclusion: Age, parity, and positional changes in hemodynamic were correlated with blood pressure reading after spinal anesthesia during cesarean delivery.
1. Introduction
Globally, the percentage of cesarean sections continues to rise especially in high- and middle-income societies. [Citation1] It should be performed when vaginal delivery has a risk to the mother or baby. Many factors have increased the number of cesarean section as amniotic membrane premature rupture, breech presentation, maternal preference, previous cesarean delivery, and cephalo-pelvic discrepancy. [Citation2–4] When medically indicated, cesarean delivery can prevent maternal and perinatal adverse effects. [Citation5] Obstetric anaesthetists have to deliver care for both the mother and the unborn baby. A team approach is important to ensure optimal outcome while ensuring that the labor process is a safe and happy experience for the parturient.
The percentage of cesarean deliveries carried out under spinal anesthesia has greatly increased over the last 20 years. [Citation6] Neuraxial anesthesia is the preferred choice for cesarean delivery in most countries unless contraindicated, due to the decrease in maternal mortality as shown by the UK Confidential Enquiry into Maternal Death (CEMD and its successors) which demonstrates the link between falling maternal mortality and rising rates of spinal anesthesia for cesarean section and in general lower rates of morbidity and mortality for neuraxial anesthesia in cesarean section. [Citation7] Complications of spinal anesthesia for cesarean delivery include the following, increase the risk of hypotension, intrapartum nausea and vomiting, possibility of post-dural puncture headache, and limited duration of action. Various efforts for prediction of maternal hypotension to modify the plan of its management
Increased sympathetic activity before spinal anesthesia is aligned with intraoperative hypotension. [Citation8] The higher blood pressure when changing position means higher sympathetic activity. [Citation9] This great variation in blood pressure can be taken as an estimation of sympathetic activity and so that can anticipate post-spinal hypotension
It was hypothesized that the occurrence of hypotension during cesarean delivery after neuraxial anesthesia was correlated with autonomic nervous system function, so this study aim was to assess the correlation of the positional changes in hemodynamic (heart rate and blood pressure) measured before spinal anesthesia in anticipation of post-spinal hypotension throughout cesarean delivery.
2. Materials & methods
After approval of the Local Ethical Research Committee and having written informed consent from all patients, 100 pregnant women scheduled for cesarean delivery with neuraxial anesthesia were enrolled in this prospective observational study from May 2019 till May 2020 in El Shatby University Hospital, Alexandria University, Egypt. Inclusion criteria were (ASA) status I, single baby, all subjects were at a gestation of 39 weak pregnancy or above, grade IV elective cesarean delivery. [Citation10] Exclusion criteria were history to allergy to any study medication, contraindication to spinal anesthesia, BMI ≥ 35 kg/m2, height less than 150 cm or more than 180 cm.
The sample size was approved to be sufficient by the Department of Statistics, Medical Research Institute, Alexandria University, Egypt.
In order to fulfill selection criteria, every patient was subjected to a careful pre-anesthetic assessment. Patients were given routine antacid prophylaxis in the form of 30 mL of sodium citrate. Upon arrival in the operating room, patients were positioned on an operating table in supine position with left lateral tilt 15 to 30 degree and allowed to rest and calm down for 5 minutes. An 18-gauge intravenous cannula was inserted under local anesthesia. Routine monitors were attached. Baseline hemodynamic measurements were made by averaging three consecutive measurements. Heart rate was recorded using pulse oximetry and electrocardiography. Systolic, diastolic, and mean blood pressure was assessed using an automated noninvasive device (Biolight M69, Biolight Meditech®, Zhuhai, China).
After taking baseline parameters in supine position with left lateral tilt 15 to 30 degree, patients were placed in left lateral position 90 degree and blood pressure and heart rate were noted immediately after changing position. Then, the patients were returned to supine position with left lateral tilt 15 to 30 degree. After that the patients were placed in sitting and hemodynamic parameters were noted again in this sitting position immediately after changing position.
In the sitting position spinal anesthesia was delivered under full sterilization. After skin local anesthetic injection with lidocaine 2%, a 25-gauge Quincke spinal needle was inserted at the L4-L5 vertebral interspace. After free flow of cerebrospinal fluid, 2.2 ml (11 mg) of hyperbaric bupivacaine 0.5% and 25 μg (0.5 ml) fentanyl was given, and the patient was returned back to the baseline position. At the start of local anesthetic injection, coload of lactated Ringer’s solution was started for the first 1 L, by fully opening the IV fluid set with the bag suspended at a height of approximately 1 m above the midpoint of the operating table. Then, maintenance fluids were limited to 10 ml/kg/hour. Block height was assessed using ice swap and considered adequate if at the T4 level or above. Also motor block was assessed using bromage score and considered adequate if grade IV unable to move legs or feet. If sensory or motor block were not adequate, the patient was excluded from the study. Surgery was started after the block adequacy was considered by anesthesiologist. After the delivery of baby, 3 IU oxytocin was administered as a slow bolus injection, and 7 IU was added to a second bag of Ringer’s lactate and infused over the remainder of the operation. Patients were monitored for (Systolic, diastolic and mean) blood pressure and heart rate every 2 min till the delivery of baby and every 3 min thereafter. No prophylactic ephedrine was administered.
The most common definitions of hypotension used in research studies were either systolic blood pressure “< 80% baseline”, or ‘< 100 mmHg. [Citation11] Hypotension was defined as a decrease of >20% from basal systolic blood pressure. Although definition of hypotension depends on systolic blood pressure, treatment with intravenous 10 mg ephedrine when mean blood pressure below 60 mm Hg, as perfusion depends on mean arterial blood pressure.
Bradycardia was defined as a heart rate below 60 beat per minute, and 0.5 mg atropine was given intravenous.
Oxygen was given via face mask oxygen 4 liters per minute if needed, to keep the SpO2 values above 95%.
2.1. Statistical analysis
Data were coded and entered using the statistical package for the Social Sciences (SPSS) version 22. Data were summarized by mean as measure of central tendency& Standard deviation, range as measures of dispersion for quantitative variables. Categorical variables are described by frequencies and percentages.
Correlation between variables was tested by calculating the Pearson correlation coefficient and testing its significance except parity which was tested by Spearman correlation.
To test relation between number of hypotensive episodes and age Kruskal–Wallis test was used. For significant results, pair wise comparison was done.
Multivariate logistic analysis was performed to detect the independent contribution of different factors affecting occurrence of hypotension.
3. Results
Sociodemographic variables including parity are displayed in .
Table 1. Socio-demographic characteristics& gestational history
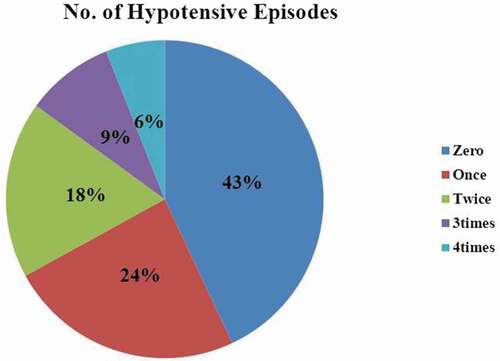
Hypotension occurred in 57% of cases of which 42% had only one, 32% two and 26% three or more episodes of hypotension. &
Table 2. Number of hypotensive episodes
Of the sociodemographic variables age showed a negative correlation with intraoperative systolic blood pressure as (r = −.651, p = .0001), while weight and height had no significant correlation with intraoperative systolic blood pressure as {(r = −.088, p = .38), (r = .09, p = .42) respectively}.As regards parity there was statistical significant negative correlation with intraoperative systolic blood pressure as (r = −.756, p = .0001).
Table 3. Correlation between Socio-demographic characteristics and intraoperative systolic blood pressure (SBP) readings
Of hemodynamic variables at supine position heart rate had statistical significant negative correlation with intraoperative systolic blood pressure as (r = −.793, p = .0001) ) while, other measurements (systolic, diastolic, and mean) blood pressure had no statistical significant correlation with intraoperative systolic blood pressure.
Table 4. Correlation between hemodynamic measurements at supine position with intraoperative systolic blood pressure (SBP)
Figure 2. Correlation between heart rate at supine position and intraoperative systolic blood pressure (SBP) readings
Changes from supine to lateral position in heart rate and (systolic, diastolic, and mean) blood pressure had statistical significant negative correlation with intraoperative systolic blood pressure as P value <.05. & –]
Table 5. Correlation between Changes in hemodynamic (heart rate and blood pressure) from supine to lateral position and intraoperative systolic blood pressure (SBP) readings
Figure 3. Correlation between ∆HR in lateral position and intraoperative systolic blood pressure (SBP) readings
Figure 4. Correlation between ∆DBP in lateral position and intraoperative systolic blood pressure (SBP) readings
Figure 5. Correlation between ∆MABP in lateral position and intraoperative systolic blood pressure (SBP) readings
Changes from supine to sitting position in heart rate and (systolic, diastolic, and mean) blood pressure had statistical significant negative correlation with intraoperative systolic blood pressure as P value <.05. & , )
Table 6. Correlation between Changes in hemodynamic (heart rate and blood pressure) from supine to sitting position and intraoperative systolic blood pressure (SBP) readings
Figure 6. Correlation between ∆HR in sitting position and intraoperative systolic blood pressure (SBP) readings
Figure 7. Correlation between ∆DBP in sitting position and intraoperative systolic blood pressure (SBP) readings
shows that overall model including changes from supine to lateral position (heart rate, systolic, diastolic, and mean blood pressure) was statistically significant in prediction of occurrence of hypotension. The significant predictors were (∆ heart rate, ∆diastolic and ∆ mean blood pressure)
Table 7. Model 1 to assess factors affecting occurrence of intraoperative systolic blood pressure (SBP) hypotension as regards hemodynamic changes from supine to lateral position
shows that overall model including changes from supine to sitting position (heart rate, systolic, diastolic, and mean blood pressure) was statistically significant in prediction of occurrence of hypotension. The significant predictors were (∆heart rate and ∆diastolic blood pressure).
Table 8. Model 2 to assess factors affecting occurrence of intraoperative systolic blood pressure (SBP) hypotension as regards hemodynamic changes from supine to sitting position
4. Discussion
There was no accepted single definition of hypotension in the scientific literature. The incidence rate of hypotension differs according to the selected definition. [Citation12] S. Klohr et al, [Citation11] found 15 variable definitions of hypotension in 63 studies following spinal anesthesia or combined spinal-epidural anesthesia for cesarian section, carried out from 1999 to 2009. Hypotension was defined as a decrease of systolic blood pressure below 80% of the baseline value. This was the same definition of 13 studies (20.6%) of total (63)Sixty-three qualified publications (7120 patients) were rectified, releasing 15 variable definitions of hypotension. [Citation13–15]
As regards the incidence rate of hypotensive cases, 57% of females were hypotensive. This percent falls in the same range of hypotension due to the sympathectomy resulting from spinal anesthesia which is enhanced by the physiological changes during the last trimester, in as much as 55%-90%. [Citation16,Citation17] As regards the age there was significant negative correlation with the intraoperative systolic blood pressure. Similar results were reported by Brenk, et al. who found lower incidence of hypotension in younger parturient than in older ones. [Citation18] DG, Bishop. found that preoperative maternal age was predictive of hypotension in cesarean delivery. [Citation19] The explanation of this could be related to reduction in cardiac reserve and changes in baroreceptor and sympathetic nervous system responses in older patients. [Citation20–22]As regards the parity there was significant negative correlation with intraoperative systolic blood pressure. In agreement with this result Ghaem, et al. found pregnant with gravidity ≥4 has higher risk of developing hypotension. [Citation23]The explanation of this result could be related to decrease in peripheral vascular tone during pregnancy. The extent of the reduction in systemic vascular resistance in pregnancy was higher in multiparous when compared to nulliparous. [Citation24] Hence, sympathectomy as a result of spinal anesthesia in multiparous has been associated with further spinal hypotension. [Citation22]
Of hemodynamic variables at supine position heart rate had a significant negative correlation with intraoperative systolic blood pressure. In agreement with this result Yokose, et al. found that a higher pre-anesthetic heart rate was associated with the occurrence of post-spinal hypotension during cesarean delivery. [Citation25] Furthermore DG, Bishop. found that preoperative basal heart rate has good prediction of post spinal hypotension during cesarean delivery. [Citation19] Finally, Gaem, et al. found basal heart rate was a risk factor for prediction of hypotensive cases after spinal anesthesia in cesarean section. [Citation23] This could be explained by higher basal heart rate generally reflects enhanced activity of the sympathetic nervous system. Therefore, parturient with higher basal heart rates more liable to post-spinal hypotension. On the other hand Zifeng, et al. demonstrated that pre-anesthetic heart rate was not predictive factor with the incidence of postspinal hypotension during cesarean delivery. [Citation26] The explanation of this difference with our result may be due to Zifeng heart rate measurement was done in supine position without lateral tilt, the patient was supine all through the operation, and finally, Zifeng used different dose and different drug of local anesthesia.
As regards baseline blood pressure (systolic, mean, and diastolic) not significant correlated with intraoperative systolic blood pressure. In agreement with this result Toyama, et al. failed to demonstrate baseline hemodynamic parameters as a good predictor of spinal anesthesia induced hypotension. [Citation22] On the other hand DG, Bishop. found that basal mean blood pressure was predictive of hypotension in cesarean delivery. [Citation19] Also Ghaem, et al. [Citation23] revealed that baseline systolic blood pressure <120 mmHg was aligned with elevated risk of developing hypotension. This difference may be due to that our parturient were ASA I, gestation of 39 weak or more pregnancy, and grade IV elective cesarean delivery so that not expected to have significant changes in basal blood pressure. Furthermore, the method of measurement of basal blood pressure by three measurements after rest of 5 min that allowed stress effect and anxiety to be released. Finally, the difference of local anesthetic dose, fluid load, and definition of hypotension may contribute to this difference.
Changes from supine to lateral position and from supine to sitting position in (heart rate, systolic, diastolic, and mean blood pressure) had significant negative correlation with intraoperative systolic blood pressure. In agreement with this result Jeon, et al. concluded that the higher the orthostatic changes in blood pressure and heart rate from supine to lateral positions, the greater the reduction of blood pressure in patients. [Citation27] Also Hans, et al concluded that higher sympathetic tone before anesthesia would be associated with further reduction of blood pressure after anesthesia. [Citation9] Finally, Sun and Huang reported that hypotension after spinal anesthesia was affected by preoperative sympathetic activity and effective circulating blood volume. [Citation28] On the other hand, Kinslow et al. couldn’t find any correlation between the blood pressure and heart rate changes due to position and the occurrence of post-spinal hypotension. [Citation29] Also Froelich and Caton, [Citation30] couldn’t find a correlation between hemodynamic changes due to position and the occurrence of hypotension. The explanation for this difference may be related to the use of different methods of measurement. In this study, the orthostatic blood pressure measured just after changing position, but Froelich and Caton took the average of five blood pressure readings one every minute after changing position. The peak positional blood pressure change takes place by around 1 minute after changing position, [Citation31,Citation32] assessment based on delayed values may produce variable outcome.
Multivariate logistic analysis to assess factors affecting occurrence of hypotension found that changes in hemodynamic variable from supine to lateral position only significant predictor were (∆ heart rate, ∆ diastolic and ∆ mean blood pressure), and changes in hemodynamic variable from supine to sitting position only significant predictor were (∆heart rate and ∆ diastolic blood pressure). In agreement with two models Ragi Jain, found moderate degree of correlation for changes in diastolic and mean blood pressure between supine and lateral positions with occurrence of intraoperative hypotension. However, correlation of difference between sitting from the supine position showed only mild association with occurrence of intraoperative hypotension. [Citation33] The explanation for this analysis may be due to the difference in sympathetic and parasympathetic response to changes in position. Sympathetic function test was assessed by changes of systolic blood pressure from supine to sitting or standing, while parasympathetic function was assessed by testing heart rate changes after standing up from supine position. It was very difficult to the patient to assume standing position from supine; we measured the variation in orthostatic blood pressure and heart rate by permitting patient to change position from supine to lateral and sitting positions. A pilot study by Hyun Kim, et al suggested that the parasympathetic function tests may be useful methods for predicting the occurrence of post-spinal hypotension throughout cesarean delivery. There was no correlation between sympathetic dysfunction and hypotension. [Citation34]
Higher sympathetic activity before neuraxial anesthesia was associated with increased risk for post-spinal hypotension. The great variability in hemodynamic after positional change indicates higher sympathetic activity to blood vessels. [Citation27] The higher autonomic activity, the higher the risk for post-spinal hypotension.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- World Health Organization (WHO). Statement on caesarean section rates. Geneva, Switzerland: WHO; 2015.
- Al-Rifai R. Rising cesarean deliveries among apparently low-risk mothers at University teaching hospitals in Jordan: analysis of population survey data, 2002-2012. Glob Health Sci Pract. 2014;2(2):195–209.
- Panditrao S. Intraoperative difficulties in repeat cesarean section. J Obstet Gynecol India. 2008;58:507–510.
- World Health organization (WHO). Monitoring emergency obstetric care: a handbook. Geneva, Switzerland: WHO; 2009.
- Hannah ME, Hannah WJ, Hewson SA, et al. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomisedmulticentre trial. Term Breech trial collaborative group. Lancet. 2000;356(9239):1375–1383.
- Guo S. Delievery settings and caesarean section rates in China. B World Health Organ. 2007;85(10):755–762.
- Lamon AM, Habib AS. Managing anesthesia for cesarean section in obese patients: current perspectives. Local Reg Anesth. 2016;9:45–57.
- Slagt C, Malagon I, Groeneveld AB. Systematic review of uncalibrated arterial pressure waveform analysis to determine cardiac output and stroke volume variation. Br J Anaesth. 2016;9(4):626–637.
- Hanss R, Ohnesorge H, Kaufmann M, et al. Changes in heart rate variability may reflect sympatholysis during spinal anaesthesia. Acta Anaesthesiol Scand. 2007;51(10):1297–1304. .
- Lucas DN, Yentis SM, Kinsella SM, et al. Urgency of caesarean section: a new classification. J R Soc Med. 2000;93(7):346–350. .
- Kl€ohr S, Roth R, Hofmann T, et al. Definitions of hypotension after spinal anaesthesia for caesarean section: literature search and application to parturients. Acta Anaesthesiol Scand. 2010;54(8):909–921.
- Seeling M, Papkalla N, Radtke F, et al. Incidence of intraoperative hypotension during anaesthesia varies greatly with the chosen definition. Eur J Anaesthesiol. 2008;25(Sup44):8.
- Zhou ZQ, Shao Q, Zeng Q, et al. Lumbar wedge versus pelvic wedge in preventing hypotension following combined spinal epidural anaesthesia for caesarean delivery. Anaesth Intensive Care. 2008;36(6):835–839.
- Ngan Kee WD, Lee A, Khaw KS, et al. A randomized double-blinded comparison of phenylephrine and ephedrine infusion combinations to maintain blood pressure during spinal anesthesia for cesarean delivery: the effects on fetal acid-base status and hemodynamic control. Anesth Analg. 2008;107(4):1295–1302.
- Cesur M, Alici HA, Erdem AF, et al. Spinal anesthesia with sequential administration of plain and hyperbaric bupivacaine provides satisfactory analgesia with hemodynamic stability in cesarean section. Int J Obstet Anesth. 2008;17(3):217–222.
- Orbach-Zinger S, Ginosar Y, Elliston J, et al. Influence of preoperative anxiety on hypotension after spinal anaesthesia in women undergoing caesarean section. Br J Anaesth. 2012;109(6):943–949. .
- Kee WD, Khaw KS. Vasopressors in obstetrics: what should we be using? Curr Opin Anaesthesiol. 2006;19(3):238–243.
- Brenck F, Hartmann B, Katzer C, et al. Hypotension after spinal anesthesia for cesarean section: identification of risk factors using an anesthesia information management system. J Clin Monit Comput. 2009;23(2):85–92. .
- Bishop DG, Cairns C, Grobbelaar M, et al. Obstetric spinal hypotension: preoperative risk factors and the development of a preliminary risk score - the PRAM score. S Afr Med J. 2017;107(12):1127–1131.
- Pereira ID, Grando MM, Vianna PT, et al. Retrospective analysis of risk factors and predictors of intraoperative complications in neuraxial blocks at faculdade de medicina de botucatu-UNESP. Rev Bras Anestesiol. 2011;61(5):568–581. .
- Chinachoti T, Saetia S, Chaisiri P, et al. Incidence and risk factors of hypotension and bradycardia during spinal anaesthesia. Siriraj Med J. 2006;58:696–701.
- Toyama S, Kakumoto M, Morioka M, et al. Perfusion index derived from a pulse oximeter can predict the incidence of hypotension during spinal anaesthesia for Caesarean delivery. Br J Anaesth. 2013;111(2):235–241. .
- Ghaem H, Fakherpour A, Fattahi Z, et al. Maternal and anaesthesia-related risk factors and incidence of spinal anaesthesia-induced hypotension in elective caesarean section: a multinomial logistic regression. Indian J Anaesth. 2018;62(1):36.
- Clapp JF, Capeless E. Cardiovascular function before, during, and after the first and subsequent pregnancies. Am J Cardiol. 1997;80(11):1469–1473.
- Yokose M, Mihara T, Sugawara Y, et al. The predictive ability of non-invasive haemodynamic parameters for hypotension during caesarean section: a prospective observational study. Anaesthesia. 2015;70(5):555–562.
- Xu Z, Xu T, Zhao P, et al. Differential roles of the right and left toe perfusion index in predicting the incidence of postspinal hypotension during cesarean delivery. Anesth Analg. 2017;125(5):1560–1566.
- Jeon Y, Hwang J, Kim M, et al. Positional blood pressure change and the risk of hypotension during spinal anesthesia for cesarean delivery. Anesth Analg. 2010;111(3):712–715. .
- Sun S, Huang SQ. Role of pleth variability index for predicting hypotension after spinal anesthesia for cesarean section. Int J Obstet Anesth. 2014;23(4):324–329.
- Kinsella SM, Norris MC. Advance prediction of hypotention at cesarean delivery under spinal anesthesia. Int J ObstetAnesth. 1996;5:3–7.
- Frölich M, Caton D. Baseline heart rate may predict hypotension after spinal anesthesia in prehydrated obstetrical patients. Can J Anaesth. 2002;49(2):185–189.
- Nardo CJ, Chambless LE, Light KC, et al. Descriptive epidemiology of blood pressure response to change in body position. ARIC study. Hyperten. 1999;33(5):1123–1129.
- Borst C, van Brederode JF, Wieling W, et al. Mechanisms of initial blood pressure response to postural change. Clin Sci. 1984;67(3):321–327.
- Jain R, Agarwal A, Yadav S. Prediction of hypotension during caesarean section with positional changes in the blood pressure and heart rate. 2015;1(3):150–154. Int J Med Res Prof.
- Kim H, An J, Kim E, et al. A pilot study on the role of autonomic function testing in predicting hypotension in patients undergoing cesarean section under spinal anesthesia. Anesth Pain Med. 2019;14(3):259–265. .