ABSTRACT
Introduction: The ideal lip repair is characterized by; the symmetrical shape of nasolabial folds and both alae of the nose with a natural-looking philtrum and Cupid’s bow in both static and dynamic states, in addition to a hidden scar.
Objective: to compare between Fisher anatomical subunit approximation technique and Millard rotational advancement technique in unilateral cleft lip repair.
Methods: Prospective study for 40 patients presented to Alexandria Main University hospital with unilateral cleft lip deformity between March 2019 and October 2020. Twenty patients with unilateral cleft lip deformity were repaired by Fisher anatomical subunit approximation technique, while the other twenty were repaired by Millard rotational-advancement technique. The postoperative photographs of the patients were captured and processed in computer photogrammetry software through which anthropometric parameters including (lip height, lip width, vermilion height, and alar base width) were compared between the normal side and the repaired side. In this software, each anthropometric parameter length on the normal side is taken as a control with a fixed value of (1) then the same parameter on the repaired side was measured as a ratio of this value to avoid bias. Comparison between both groups for assessment of the quality of cleft lip repair was also done based on Steffensen grading criteria.
Results: Comparison between both techniques in unilateral cleft lip repair showed that there was no significant difference between them in the anthropometric measurements. While the comparison between the two groups using Steffensen grading criteria showed that Fisher’s technique surpassed Millard’s technique.
Conclusion: We recommend the use of the Fisher anatomical subunit approximation technique in unilateral cleft lip repair for its superior results over the Millard rotational advancement technique.
KEYWORDS:
1. Introduction
A cleft lip is one of the most common congenital malformations, with a mean incidence of 1/1000 live births worldwide [Citation1].
Plenty of techniques were described for cleft lip repair. The main idea of all these techniques is the precise dissection of the orbicularis oris pathological muscle insertions around the cleft, and their reinsertion into the correct anatomical position, in order to reconstruct the normal nasolabial anatomy [Citation2].
Many techniques were described for the repair of the cleft lip over time, denoting that there is no single best one [Citation3–5].
The proper management of cleft lip is now accomplished through many protocols depending on multidisciplinary approaches in specialized centers. The aim of the surgical repair is not only to provide an appropriate anatomical reconstruction but also to improve the function and the esthetic appearance of the lip [Citation6].
The ideal lip repair is characterized by; the symmetrical shape of nasolabial folds and alae of the nose on both sides with a natural-looking philtrum and Cupid’s bow in both static and dynamic states, in addition to a hidden scar [Citation7].
In 1964, Millard [Citation8] introduced the rotational advancement technique which entails the advancement of a lateral flap into the upper part of the lip, with the rotation of the medial part downward. The advantages of this technique are: reconstructing the philtrum and the Cupid’s bow, transferring the tension of the wound beneath the base of the ala, decreasing nasal flare and directing the normal growth of the alveolar process.
Afterward, Wynn [Citation10] and Davies [Citation11] described variations of the triangular flaps introduced into the upper lip. Nevertheless, Millard’s repair [Citation9] has withstood the test of time and remains the most popular method for closure of the unilateral cleft lip. Skoog [Citation12] and Trauner [Citation13] independently described procedures that involve a combination of flaps in the upper and lower portions [Citation14].
In 2005 Fisher introduced the anatomical subunit approximation technique which is derived from a previously described techniques and stick to the concept of anatomical subunits of the lip [Citation15].
Fisher’s technique gained the idea of using sloped incisions to increase the length of the lip from Rose-Thompson technique, which allowed him to design a smaller triangular flap above the cutaneous roll which was described by Noordhoff [Citation16], with the incisions respecting the anatomical subunits of the lip [Citation15].
Millard’s technique remained the standard method for unilateral cleft lip repair in the Alexandria Plastic Surgery department for a long period of time. The use of Fisher’s anatomic subunit approximation technique in cleft lip repair has increased over the last decade. So we conducted this study aiming to find accordingly which technique gives a better outcome.
2. Patients and methods
A prospective study was conducted for 40 patients with unilateral cleft lip deformity with or without cleft palate in the Alexandria Main University hospital. All cases were operated by the authors M.E, N.G, A.F, and M.A.
All the patients/patients’ guardians were aware of the procedure and informed consents were taken from them. The study was registered and approved from the Medical Ethics Committee with IRB no.: 00012098 and FWA no.: 00018699.
The study included two randomly assigned groups:
I. The first group included (20) patients with unilateral cleft lip deformity which was repaired by Fisher’s anatomical subunit approximation technique.
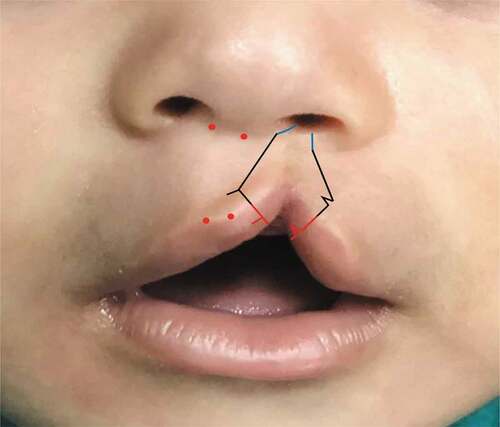
The incisions are made to cross the cutaneous roll perpendicularly on the peak of the cupid’s bow at the cleft side (medial lip) and the base of philtral column at the lateral lip. Then the incision is extended upward to be on a line that is symmetrical to the noncleft side philtral column and continued superolaterally along the lipo-columellar crease to the final closure point in the nostril sill [Citation15].
A Rose-Thompson lengthening effect is achieved above the level of the cutaneous roll with a small triangle placed just above it, is usually used. The central vermilion deficiency is compensated by a triangular vermilion flap from the lateral lip element. [Citation15] ()
II. The second group included (20) patients with unilateral cleft lip deformity which were repaired by Millard rotational-advancement technique.
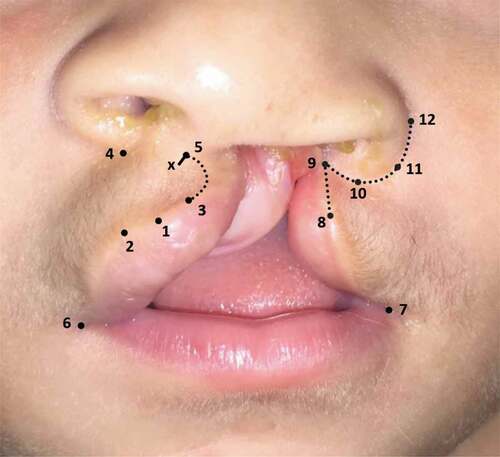
Medial lip markings: point (1) is the center of the cupid’s bow, point (2) is the peak of the cupid’s bow on the noncleft side, point (3) is the peak of the cupid’s bow on the cleft side, point (4) is the alar base on the noncleft side, point (5) is the mid-point of columellar-labial angle and X is back cut point and point (6) is the oral commissure on the noncleft side ()
Lateral lip markings: point (7) is the oral commissure on the cleft side, point (8) is the new peak of the cupid’s bow on the cleft side, point (9) is the superior tip of the advancement flap, point (10) is the midpoint of alar base cleft side, point (11) is the lateral base of cleft side and point (12) is the extent of lateral alar base incision ().
In both groups the nasal deformities were repaired by; centralization of the columellar base and septum, release of the attachments of the lower lateral cartilage from the lateral piriform rim, symmetrical alar base repositioning at the same level, and equalization of the nostrils’ circumference.
2.1. Post-operative care
The wounds were cleaned with normal saline and antibiotic ointment was applied 3 times daily. Sutures were removed after 5–7 days and anti-tension adhesive strips were applied.
2.2. Clinical follow-up and assessment of the results
Postoperative follow-up was planned every week for 1 month then monthly for 6 months during which photographs were captured in both frontal and sub-mental views.
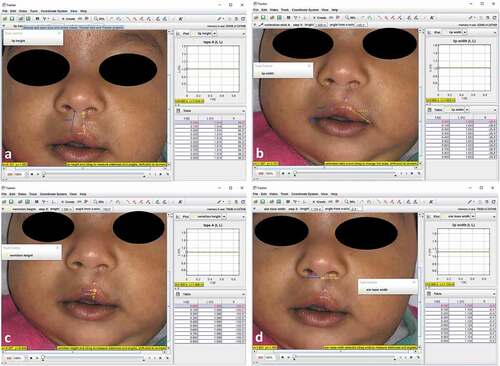
These postoperative photographs are processed in computer photogrammetry software (tracker 5.1.5 copyright (c) 2020 Douglas Brown https://physlets.org/tracker) through which anthropometric parameters including (lip height, lip width, vermilion height, and alar base width) were measured and compared between the normal side and the repaired side. In this software, each anthropometric parameter length on the normal side is taken as a control with a fixed value of (1) then the same parameter on the repaired side was measured as a ratio of this value to avoid bias ().
Figure 3. Anthropometric measurements on the patient (a: lip height), (b: lip width), (c: vermilion height), and (d: alar base width)
Comparison between both groups for assessment of the quality of cleft lip repair was also done based on Steffensen grading criteria.
3. Results
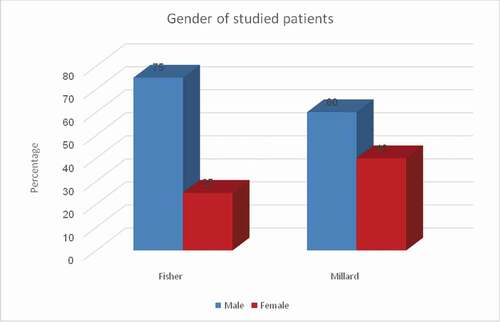
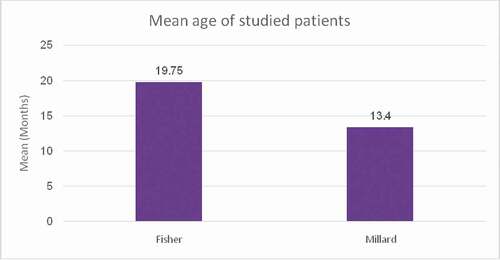
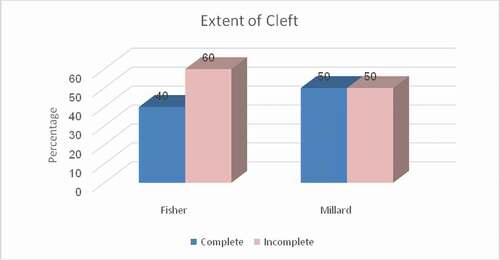
Forty patients were included in this study, 20 operated on by the Fisher’s technique, and the other 20 by modified Millard’s technique. The distribution of patients according to their demographic data, the extent of the cleft, and surgical intervention is shown in ().
Among the 40 patients, 19 patients had a cleft on the right side (7 of them were repaired by Fisher’s technique, while 12 patients were repaired by Millard’s technique). The other 21 patients had clefts on the left side (13 of them were repaired by Fisher’s technique, while 8 patients were repaired by Millard’s technique) ().
Table 1. Distribution of studied patients based on affected side, extent, and surgical technique
The extent of the cleft lip was complete in 18 patients (8 of them were repaired by Fisher’s technique, while 10 patients were repaired by Millard’s technique). The other 22 patients had incomplete clefts (12 of them were repaired by Fisher’s technique, while 10 patients were repaired by Millard’s technique) ().
Four anthropometric measurements were obtained from the postoperative photographs for each patient (on the cleft side taking the normal side as a perfect ratio of 1.00) and compared according to repair technique as shown in ().
Table 2. Comparison between two groups according to anthropometric parameters
Table 3. Comparison between two groups according to the cleft extent and anthropometric measurements
Comparison between 2 groups according to Steffensen grading criteria showed that the scar appearance was “good” in 90% of the cases in Fisher’s group and 65% in Millard’s group ().
Table 4. Comparison between two groups according to Steffensen grading criteria
Clinical cases: ).
Figure 7. A case of Fisher’s group; 4-month-old male, with left-sided unilateral incomplete cleft lip. (a and b) Preoperative frontal and submental views and (c and d) 2 months’ postoperative frontal and submental views

Figure 8. A case of Fisher’s group; 4-month-old male, with left-sided unilateral incomplete cleft lip. (a and b) Preoperative frontal and submental views and (c and d) 3 months’ postoperative frontal and submental views

Figure 9. A case of Fisher’s group; 3-month-old female, with left-sided unilateral incomplete cleft lip. (a and b) Preoperative frontal and submental views and (c and d) 6 months’ postoperative frontal and submental views

Figure 10. A case of Fisher’s group; 6-month-old male, with right-sided unilateral complete cleft lip. (a and b) Preoperative frontal and submental views and (c and d) 5 months’ postoperative frontal and submental views

Figure 11. A case of Millard’s group; 5-month-old male, with left-sided unilateral complete cleft lip. (a and b) Preoperative frontal and submental views and (c and d) 12 months’ postoperative frontal and submental views

Figure 12. A case of Millard’s group; 4-month-old male, with left-sided unilateral incomplete cleft lip. (a and c) Preoperative frontal and submental views and (b and d) 3 months’ postoperative frontal and submental views

4. Discussion
In 1964, the rotation advancement technique was introduced by Millard for the repair of unilateral cleft lip, which gained popularity very rapidly and became the most widely used technique until now [Citation17].
Millard’s technique was designed to preserve the natural landmarks of the philtrum and the Cupid’s bow and to rotate them into normal position. Maintenance of this rotation is achieved by the advancement of the lateral lip medially which also reduces the alar flare and width of the nostril floor. The strategic positioning of the scars manages to place most of the oblique scar along the natural line of a philtrum column while the interdigitations are hidden in the shadow of the nostril sill and nasal floor [Citation17–19].
The rotation-advancement technique advantages over earlier procedures are that it allows modifications and manipulations while maintaining the main anatomical and surgical goals, the minimal discard of tissue, and the ease of secondary correction [Citation20,Citation21].
Further on, this technique was modified by Millard himself and other surgeons to be tailored according to patients’ variations aiming to improve the outcome and avoid any faults [Citation20,Citation21].
In 2005 Fisher introduced a new technique for unilateral cleft lip repair (anatomical subunit approximation). That allows approximation of the lateral and medial lip elements almost entirely along the junctions of the anatomical subunits of the lip and nose avoiding the rotation incision which crosses the philtral column on the cleft side [Citation15].
The advantage of the anatomic subunit approximation repair is that it is reliable as it is based on previously described repairs; Rose-Thompson lengthening occurs by the sloped incisions crossing the cutaneous roll of the medial and lateral lip elements which allows for a smaller inferior triangle than usually required. This inferior triangle is positioned according to Noordhoff’s description, above the cutaneous roll, to allow for better continuity of the roll. [Citation15]
This technique results in an ideal line of repair which starts from the cleft-side peak of “Cupid’s bow” to the base of the nose along a line typically symmetrical to the noncleft-side philtral column and then continues superolaterally along the lip-columellar crease to end in the nostril sill so the cutaneous scar on the nose is minimized and limited to the cleft-side nostril sill and respecting the anatomical subunits of the lip and nose. [Citation15]
In 2017 Musanzayi et al. performed 101 unilateral cleft lip cases by fisher’s technique; they evaluated their results using both Asher McDade esthetic index and Steffensen’s grading criteria, and concluded that the anatomical subunit approximation technique significantly improves the length of the medial and lateral lip and leaves an acceptable scar [Citation22].
In our study we excluded the Asher-McDade Esthetic Index, because it has some limitations, as it does not provide enough detail on some important parameters such as scar characteristics.
Kwong et al. in 2019 performed a comparative study between Fisher, Millard, and Mohler techniques of cleft lip repair surgery and assessed the results using eye-tracking technology; and concluded that Fisher repairs were the best esthetically, then Mohler repairs and finally Millard repairs [Citation23].
Patel et al. in 2019 performed a comparative study between the Fisher and Millard cleft lip repairs including 24 cases of unilateral cleft lip based on both anthropometric measurements and Steffensen Criteria. There were no significant differences in the qualitative findings between the techniques. Though quantitative results suggest that the Fisher anatomical subunit technique may have more reliable outcomes despite the degree of severity of the cleft. [Citation3]
Fujimoto et al in 2020 studied the surface area of the part sacrificed from lateral lip during primary repair of a “unilateral cleft lip” using three-dimensional measurements comparing the design of incisions of three different techniques (Millard, Onizuka, and Fisher) [Citation24].
The Millard repair study showed that; it had the least sacrifaction ratio while Fisher repair ratio exceeded 20%. Although sacrifice ratio is not the best way for evaluation of “unilateral cleft lip” repair techniques, but the more sacrification of the lateral lip tissue would make the secondary lip correction difficult [Citation24].
Suchyta et al. in 2020 compared the esthetic results of 21 children with unilateral cleft lip deformity who had undergone surgery by 3 different techniques (Millard, Fisher, and Mohler) through an online crowdsourcing platform named mechanical turk; scar severity was lowest for Fisher and higher for Millard and Mohler. The other parameters were more or less equal in the three techniques [Citation25].
In our study comparison between both techniques in unilateral cleft lip repair showed that there was no significant difference in the anthropometric measurements of lip height, lip width, vermilion height, and alar base length. While the comparison between the two groups using Steffensen grading criteria showed that the Fisher’s group surpassed the Millard’s group especially in its scar appearance as the scar on the nose is limited to the cleft-side nostril sill and respecting the anatomical subunits of the lip and nose (cleft side philtral column).
5. Conclusions
We recommend the use of the Fisher anatomical subunit approximation technique in unilateral cleft lip repair for its superior results regarding the scar appearance compared to the Millard rotational advancement technique.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Notes on contributors
Mohamed F. ElMaghraby
Mohamed F. ElMaghraby Assistant Lecturer in Department of Plastic and Reconstructive Surgery, Faculty of Medicine, University of port said, port said, Egypt.
Nasser A. Ghozlan
Nasser A. Ghozlan Prof. Dr. in Department of Plastic and Reconstructive Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt.
Mona H. Ashry
Mona H. Ashry A. Prof. Dr. Depatment of public health and community medicine, Faculty of Medicine, University of Alexandria, Alexandria, Egypt.
Mohamed H. Abouarab
Mohamed H. Abouara Lecturer in Department of Plastic and Reconstructive Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt.
Adham Farouk
Adham Farouk A. prof. Dr. Department of Plastic and Reconstructive Surgery, Faculty of Medicine, University of Alexandria, Alexandria, Egypt.
References
- Farouk A. Critical choices in cleft surgery: 18-year single-surgeon retrospective review of 900 cases. Eur J Plast Surg. 2016;39(1):11–22.
- Iliopoulos C, Mitsimponas K, Lazaridou D, et al. A retrospective evaluation of the aesthetics of the nasolabial complex after unilateral cleft lip repair using the tennison-randall technique: a study of 44 cases treated in a single cleft center. J Craniomaxillofac Surg. 2014;42(8):1679–1683.
- Patel TA, Patel KG. Comparison of the fisher anatomical subunit and modified millard rotation-advancement cleft lip repairs. Plast Reconstr Surg. 2019;144(2):238e–245e.
- Mc NC. Orthodontic procedures in the treatment of congenital cleft palate. Dent Rec (London). 1950;70(5):126–132.
- Marston AP, Costello MS, Farhood Z, et al. Association of pediatric patient demographic factors and scar anatomic features with scar outcomes after surgical repair of cleft lip. JAMA Facial Plast Surg. 2019;21(5):452-7.
- Gkantidis N, Papamanou DA, Karamolegkou M, et al. Esthetic, functional, and everyday life assessment of individuals with cleft lip and/or palate. Biomed Res Int. 2015;2015:510395.
- Vyas RM, Warren SM. Unilateral cleft lip repair. Clin Plast Surg. 2014;41(2):165–177.
- Millard D. A primary camouflage in the unilateral harelbok, from trans of first international congress de plastic surgeons. Baltimore: Williams and Wilkins; 1957.
- Millard DR Jr. Cleft Craft: the evolution of its surgery. I. the unilateral deformity. Vol. 105. Boston: Little, Brown; 1976. p. 3.
- Wynn SK. Lateral flap cleft lip surgery technique. Plast Reconstr Surg. 1960;26(5):509–520.
- Davies D. The one-stage repair of unilateral cleft lip and palate: a preliminary report. Plast Reconstr Surg. 1966;38(2):129–136.
- Skoog T. A design for the repair of unilateral cleft lips. Am J Surg. 1958;95(2):223–226.
- Trauner R, Trauner M. Results of cleft lip operations. Plast Reconstr Surg. 1967;40(3):209–219.
- Roberts JM, Jacobs A, Morrow B, et al. Current trends in unilateral cleft lip care: a 10-year update on practice patterns. Ann Plast Surg. 2020; 84(5):595-601.
- Fisher DM. Unilateral cleft lip repair: an anatomical subunit approximation technique. Plast Reconstr Surg. 2005;116(1):61–71.
- Noordhoff MS The surgical technique for the unilateral cleft lip-nasal deformity: Noordhoff Craniofacial Foundation; 1997.
- Millard DR Jr. Rotation-advancement principle in cleft lip closure. Cleft Palate J. 1964;12:246–252.
- Millard DR. Anatomy in multiple dimensions. In: Millard DR, editor. Cleft craft: the evolution of its surgery I the unilateral deformity. Boston: Little, Brown; 1976. p. 19–40.
- Bhattacharya S, Khanna V, Kohli R. Cleft lip: the historical perspective. Indian J Plast Surg. 2009;42(Suppl):S4–8.
- Costello BJ, Ruiz RL. Unilateral cleft lip and nasal repair: the rotation-advancement flap technique. Atlas Oral Maxillofac Surg Clin North Am. 2009;17(2):103–116.
- Stal S, Brown RH, Higuera S, et al. Fifty years of the millard rotation-advancement: looking back and moving forward. Plast Reconstr Surg. 2009;123(4):1364–1377.
- Mbuyi-Musanzayi S, Tshilombo Katombe F, Lukusa Tshilobo P, et al. Anthropometric and aesthetic outcomes for the nasolabial region in 101 consecutive African children with unilateral cleft lip one year after repair using the anatomical subunit approximation technique. Int J Oral Maxillofac Surg. 2017;46(10):1338–1345.
- Kwong JW, Cai LZ, Azad AD, et al. Assessing the fisher, mohler, and millard techniques of cleft lip repair surgery with eye-tracking technology. Ann Plast Surg. 2019;82(5S Suppl 4):S313–s9.
- Fujimoto H, Morioka D, Akamine S, et al. Three-dimensional measurement of the lateral lip element sacrificed in primary repair of a unilateral cleft lip. Ann Plast Surg. 2020;85(2):180–184.
- Suchyta M, Azad A, Patel AA, et al. Applied online crowdsourcing in plastic and reconstructive surgery: a comparison of aesthetic outcomes in unilateral cleft lip repair techniques. Ann Plast Surg. 2020;84(5S Suppl 4):S307–s10.