ABSTRACT
Introduction: Mammography is the most used breast screening tool and was proven to reduce breast-cancer-associated mortality. The estimated sensitivity of mammography varies between 77% and 95%; however, sensitivity could be 26% lower in dense breasts than in entirely fatty breasts. The ability to represent the complex 3D breast architecture and early changes in anatomical structures in a 2D view is the biggest challenge for mammography. In Digital Breast Tomosynthesis (DBT), tomographic images are reconstructed from multiple projections acquired from different angles. This technique allows the generation of 3D data, reduction of tissue overlap and allows better evaluation of masses, architectural distortion, and asymmetries compared with conventional two-dimensional mammographic images.
Objective: To evaluate the impact of Digital Breast Tomosynthesis on BIRADS categorization of mammographic non-mass findings.
Methods: Prospective cohort for 180 women with mammographic non-mass findings who presented to Alexandria University Radio diagnosis Department either for screening or diagnostic purposes between July 2019 and August 2020 with mean age 51.44 ± 10.67 . Digital breast tomosynthesis and ultrasound was done for all patients. Lesions were evaluated on DM; DBT alone then combined DBT & DM. Comparison of results according to changes in BIRADS, diagnostic performance using histopathology as gold standard.
Results: 208 non-mass findings were detected by conventional mammography (104 asymmetry, 35 architectural distortion, 69 micro calcifications), Tomosynthesis reduced the BIRADS 3 count by 32%, upgraded the count of BIRADS 4 lesions by 11.4% while upgraded the BIRADS 2 by 18.9% with consequent improvement of sensitivity and specificity, PPV, NPV and accuracy to 96%, 95%, 94%,97%, and 95.6%.
Conclusion: Combined FFDM and DBT improved the diagnostic performance in evaluation of non-mass findings and proper BIRADS categorization.
1. Introduction
Breast masses are common mammographic findings, it is defined as two-view lesions with complete or partial convex borders. Other non-mass findings including micro calcifications, architectural distortion, and asymmetries (focal, global, asymmetry and developing) are also seen. [Citation1] Strategies for detecting them on screening mammograms include symmetrical comparison of breasts, looking for distortions in parenchymal contour, observation of the retro mammary fat, associated findings, and comparison with previous mammographic studies. [Citation2]
The perception of these findings is crucial to get them diagnosed and treated effectively. Missing or miss-interpreting them can be due to limitations of the diagnostic equipment, fatigue of radiologists during screening programs, or the indistinct features of tumors as they appear on mammography [Citation3]. Accurate diagnosis is essential for proper management and better prognosis [Citation4].
Mammography is still the primary investigating and screening tool, despite of the well-known limited sensitivity due to the misinterpretation of distortions and asymmetries as well as the cancers hidden by superimposed glandular tissue. [Citation5]
Digital breast tomosynthesis (DBT) has been considered as an advancement of mammography with its significant improvements on performance and outcomes. It superpasses supplemental screening tools such as ultrasoundas it significantly increases cancer detection and reducing recall rates. [Citation6]
Although the combined 2D mammography and tomosynthesis radiation dose exceed the 2D mammography alone, the dose of the combined 2D mammography and DBT is still below the FDA radiation dose safety limit of 3 mGy per view and similar to that for screen film mammography. [Citation7]
1.1. Aim of the work
To evaluate the impact of Digital Breast Tomosynthesis on BIRADS categorization of mammographic non-mass findings and correlate its diagnostic performance with final histopathologic diagnosis in comparison with Digital Mammography.
2. Patients and methods
2.1. Patients
Prospective study for 180 patients with mammographic non-mass findings (micro-calcifications, focal asymmetry, and architectural distortion) referred to the mammographic unit of Radio-diagnosis and Intervention Department of Alexandria Main University Hospital and Medical Research Institute between July 2019 and August 2020, with mean age of 51.44 ± 10.67 years.
All patients were subjected to demographic and clinical data which includes patient’s name, age, marital status, lactational history, history of breast diseases, and family history.
2.2. Inclusion criteria
Mammographic non-mass findings including micro-calcifications, asymmetry, and architectural distortion.
2.3. Exclusion criteria
Cases of breast masses evident in two projections were excluded from our study.
2.4. Ethics
The medical ethics were considered. The patient was informed about the details of the examination, patient agreement and informed consent were obtained, the patient has to get use of the examination. This study was approved by the Ethics Committee of the Faculty of Medicine, Alexandria University, IRB no.0007555, FWA no.00018699.
2.5. Equipment and techniques
Mammographic examination was performed using Fujifilm, Amulet Innoviality full-field digital mammography machine with 3D digital breast tomosynthesis. . Low Kilo-voltage Peak (KvP) about 24 to 30 was used. The milli-Ampere-seconds (mAs) are adjusted upon breast tissue density.
2.6. Technique
2.6.1. FFDM
Four projections were obtained, two for each breast, the CC and MLO views. MLO view was done with an angle 45°. All views were taken while the patients were standing. Compression was applied to all breasts.
2.6.2. Digital breast tomosynthesis
Two views (MLO and CC) were obtained. 3D DBT involved the acquisition of 12 to 15 2D projection exposures by a digital detector from a mammographic x-ray source which moves over a limited arc angle. The 3D volume of compressed breast was reconstructed from the 2D projections in the form of series of images (slices) through the entire breast. Images were assessed in the workstation.
2.7. Interpretation and data analysis
Interpretation and data analysis were performed by double peer review of two radiologist expert in breast imaging. One radiologist independently reviewed the FFDM images. Another radiologist independently reviewed the DBT images only. Then, the two radiologists evaluated the combined FFDM and DBT. Each case was assigned three BIRADS categories (one for FFDM, one for DBT and one for combined FFDM & DBT).
A comparison between identical mammographic projections was performed for detection of focal mammographic abnormalities including breast composition, asymmetry, calcifications and distorted mammary architecture of both breasts. No additional views were performed as further contrast and brightness adjustment, zooming was performed on workstation.
The mammographic breast findings were finally assessed and classified according to ACR BIRADS 5th edition.
Mammographic non mass findings were evaluated:
Micro calcifications (were classified according to morphology and distribution.
Asymmetries: Asymmetry, Global asymmetry, Focal asymmetry, and Developing asymmetry).
Architectural distortion
2.8. Statistical analysis
Statistical analysis is performed using SPSS software version 25 (IBM, 2017). Data were presented in tables and figures. Continuous data were presented as mean and standard deviation. Qualitative data were presented as frequencies and proportions. Pearson’s chi-square (χ2) test was used to analyze qualitative data. The diagnostic performance of DM, DBT, and combined DM and DBT was estimated on each case. The receiver operating characteristic (ROC) curve analysis was done to show the areas under the curve (AUCs). A p value of ≤ 0.05 was accepted as statistically significant.
3. Results
3.1. Demographic data
This study included 180 female patients with their ages ranged from 26 to 69 with mean age of 51.44 ± 10.67. The most affected age group was >50 years (48.3%). Young patients were referred for mammography due to suspicious sonographic features with strong positive family history, as suspicious calcifications should be excluded. Positive family history of breast cancer was noted in 73/180 (40.6%). Among the 180 patients; 30 cases (16.7%) presented for screening mammography, while 136 cases (75.6%) came for diagnostic purposes and 14 cases (7.8%) for routine follow up.
3.2. Pathological data
The final diagnosis was reached by histopathological examination in 163 cases, and routine follow up in 17 cases (These cases were related to superimposition of glandular tissue with no underlying lesions and downgraded their BIRADS after Tomosynthesis). Ultrasound guided FNAC was done in 42 cases, core needle biopsy in 117 cases, and excisional biopsy in 4 cases. Ninety-six cases were diagnosed benign (52.5%) and 84 malignant (47.5%). ()
Table 1. Distribution of the studied cases according to final diagnosis of histopathology
3.2.1. Full-field digital mammography (FFDM)
Among the 180 patients, 15 cases (8.3%) were classified as breast density A, 89 (49.4%) ACR B, 69 (38.3%) ACR C and 7 (3.9%) ACR D.
FFDM detected 208 non-mass findings (104 asymmetries (57.8%), 69 micro calcifications (38.3%) and 35 distortions (19.4%)). ()
Table 2. Distribution of to the Non-Mass findings in correlation with histopathology
Out of 104 Asymmetries, focal asymmetry was the most common type, seen in 68/180 cases (37.8%) while the one view asymmetry was seen in 2/180 cases (1.1%). Breast cancer was detected in 44 lesions (51.2%) while 60 asymmetries were related to benign lesions (57.8).
Sixty-nine micro calcifications were classified according to their morphology, with the linear branching was the most common type, seen in 20 cases (11.1%), pleomorphic (n = 13) (7.2%), amorphous (n = 6) (3.3%), coarse heterogeneous in 10 (5.6%), round in 14 (7.8%) and skin calcifications in 3 cases (1.7%). Out of the 69 calcifications, 44 were counted malignant (51.2%) and 25 were benign (26.6%). Their distribution was diffuse, regional, grouped, linear, segmental in 15 (8.9%), 4 (2.8%), 22 (11.7%),8 (4.4%), and 20 (10.6%) cases, respectively.
Thirty-five Architectural distortions (AD) were detected by DBT, this revealed 17 benign and 18 malignant lesions.
Out of the 180 cases, 103 cases were assigned BIRADS 3(58.3%) as probably benign lesions, while BIRADS 2 in 13 cases (7.2%), BIRADS 4 in 64 cases (34.4%), and considered provisionally suspicious. ()
Table 3. Distribution of the studied cases according to FFDM BIRADS category (n = 180)
3.2.2. Digital Breast Tomosynthesis
Tomosynthesis was done for 180 patients. It upgraded the lesion count into 244. DBT detected 52 suspicious masses that were not visualized on FFDM, it clearly detected 5 hidden distortions secondary to tissue overlap. ()
Table 4. Distribution of Tomosynthesis findings and BIRADS categories
17 lesions were secondary to superimposition of glandular tissue and were downgraded to BIRADS 1.
Tomosynthesis reduced the BIRADS 3 count by 32.23% from 103 into 45, upgraded the BIRADS 2 by 18.9% lesions from 13 into 47 and upgraded the count of BIRADS 4 lesions from 64 to 88 lesions. ()
Table 5. Change in individual breast lesion grading on account of digital breast tomosynthesis (DBT) compared to digital mammography (DM)
Significant category changes were noted for both asymmetries and distortions (P value <0.0001). DBT changed the BIRADS category of 65 asymmetries (31 lesions showed increase while 34 showed decrease). As for architectural distortions, seven lesions showed category changes (five increased lesions that were obscured in 2D FFDM and two decreased related to post-operative changes).
No significant category changes were related to micro calcifications (P value 0.99); with 8/69 lesions showed category changes after revising DBT images. (five cases showed category increase and yielded malignant diagnosis (IDC) while the other three were downgraded in benign lesions). ()
Table 6. Significance of category changes after revising DBT according to lesion type
3.3. Agreement of FFDM and DBT as regards histopathology
FFDM succeeded in correct diagnosis of 85/96 benign lesions (true negative for malignancy) and of 54/84 malignant lesions (true positive for malignancy). It misinterpreted 11 benign lesions as malignant (false positive), while it gave false-negative diagnosis of 30 malignant lesions. The overall sensitivity of mammography was 64%, specificity was 88.5%, PPV was 83.1%, NPV was 73.9% and accuracy was 77.2%.
Tomosynthesis improved the sensitivity, specificity, PPV, NPV and accuracy into 96%, 93%, 92%, 97%, and 94%, respectively.
Combined FFDM and DBT with BIRADS further improved the diagnostic performance as regards the sensitivity and specificity into 96 and 95%, positive and negative likelihood of malignancy 18.51 & 0.04, PPV& NPV to 94% and 97% while the accuracy up to 95.6%. ()
Table 7. The diagnostic performance of full-field digital mammography, Digital Breast Tomosynthesis, and combined tomosynthesis and mammography for confident breast cancer diagnosis considered histopathology as the reference standard
The ROC analysis for the diagnostic performance of BI-RADS with DM, BI-RADS with DBT, and BI-RADS with combined DM and DBT for breast cancer revealed that BIRADS with DBT was significantly superior to BIRADS with DM in breast cancer diagnosis (AUC: 94.6 vs. 76.4), and the BI-RADS with combined DM and DBT was significantly superior to BI-RADS with DM or BIRADS with DBT alone (AUC: 95.6 vs 76.4 vs 94.6) . ()
Figure 1. Comparison of the ROC areas of FFDM, DBT and combined FFDM and DBT for breast cancer diagnosis evidenced by histopathology as the reference standard
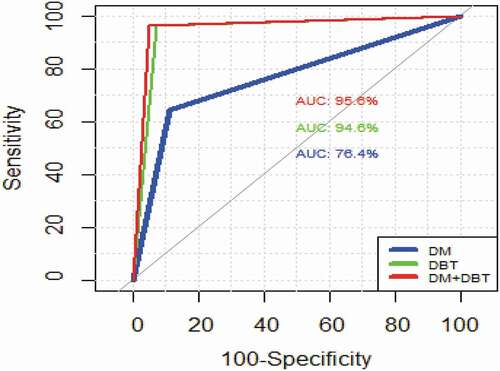
Figure 2. 49 years old case, with positive family history of breast cancer, presented for screening mammography (a) Craniocaudal and (b) Medio lateral oblique DM images of both breasts revealed suspected distortion noted at the inner portion of the left breast. (c) and (d) Craniocaudal and mediolateral oblique Tomosynthesis revealed an area of suspicious architectural distortion.(e) Ultrasound revealed an ill-defined hypo-echoic mass lesion with posterior shadowing. US guided core biopsy was performed and revealed infiltrating ductal carcinoma
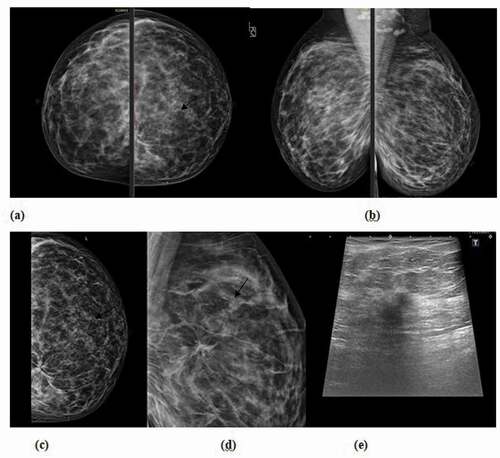
Figure 3. 54 years old patient complaining of left breast lump. (a) Craniocaudal, (b) mediolateral oblique DM images of both breasts revealed an area of focal asymmetry at the left upper inner quadrant, (c) Thin cuts tomosynthesis revealed internal fat density areas with central lucency. (d) Ultrasound showed a small hyper echoic area confined to the pre mammary region, with central cystic changes which was proved to be focal traumatic fat necrosis
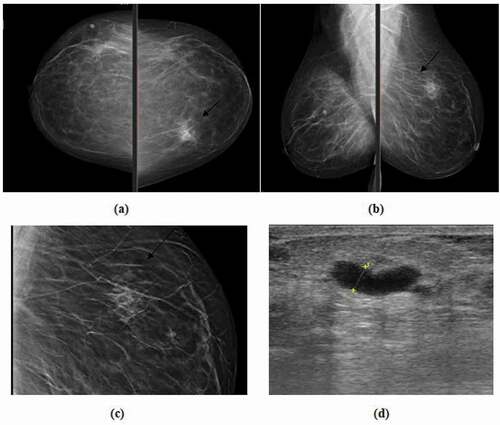
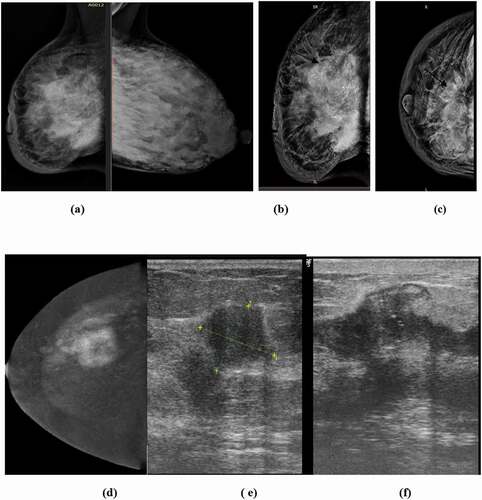
Figure 4. 32 years old lactating patient complaining of fever and right sided inflammation of the breast; (a) Medio-lateral oblique DM images of both breasts revealed right sided diffuse skin and trabecular thickening with suspicious pleomorphic segmental calcifications, (b &c) Cranio-caudal and medio-lateral oblique DBT images of right breast revealed ill-defined sizable heterogeneous mass lesion with focal retraction (tenting) of the posterior retro mammary fat and suspicious segmental calcifications, (d) CESM reveals a heterogeneously enhancing ill-defined mass lesion with related non-mass enhancement surrounding the index lesion, (e&f) Ultrasound revealed multiple ill-defined hypo-echoic masses with overlying calcifications with intervening suspicious dilated ducts. US core biopsy revealed multifocal infiltrating ductal carcinoma
Tomosynthesis raised the sensitivity, specificity, PPV and NPV for asymmetries to 95%, 98%, 98%, and 97% compared to 62%, 93%,87%, and 78% with FFDM.
While for architectural distortions, sensitivity, specificity, PPV and NPV improved from 94%, 71%, 77%, and 92% for FFDM to 94%, 82%, 85%, and 93% by DBT.
As for micro calcifications, the estimated sensitivity, specificity, PPV, NPV for FFDM 93%, 88%, 93%, 88%, respectively, while tomosynthesis reached to 100%, 96%, 98%, and 100%
4. Discussion
The current study focused on the role Digital Breast Tomosynthesis in evaluation of mammographic non-mass findings and displaying its role in changing their BIRADS categorization. Limited studies evaluated this issue and stressed on BIRADS 0 and 3 lesions [Citation8,Citation9].
The clear observation of the study was the increase in the lesions count by DBT compared to FFDM, this increase in lesion count was explained by Andersson [Citation10] who stated that the use of re-constructed images in DBT that are obtained from different angles of the breast allows the assessment of breast parenchyma where lesions may go unnoticed.
Also, the reduction in the number of BIRADS 3 count lesions by 33% (from 103 to 45), which was more significant for asymmetries and distortions is one of the potential advantages of DBT. Similar results were obtained by Basha [Citation11], who reported DBT produced 31.5% upgrading and 35.2% downgrading of BI-RADS scoring of breast lesions. Also DBT reduced number of BI-RADS 3 and 4, compared to FFDM (p < 0.001).
Galati [Citation12] reported that DM+DBT increased the number of negative and benign cases (BI-RADS 1 and 2) and suspicious and malignant cases (BI-RADS 4 and 5), while it reduced the number of BI-RADS 0 and 3.
Regarding asymmetries, DBT reduced the count of true asymmetries from 104 to 87, as 17 asymmetries were overestimated due to tissue overlap with consequent reduction in BIRADS category from 3 to 1. Whereas DBT could detect 18 hidden suspicious lesions thus increasing the count of the BIRADS 4 lesions from 18 to 36 lesions. There were significant category changes for asymmetries by DBT (p < 0.001) with 31 cases showed category increase while 34 cases showed category decrease. This improved the sensitivity and specificity, PPV and NPV for DBT to 95%, 98%, 98%, and 97%, respectively, compared to 62%, 93%, 87%, and 78% for FFDM.
Near results were reported by Mokhtar et al [Citation13], who concluded that DBT enables better depiction of asymmetries and can be used for better lesion detection and accurate description with consequent reduction of BIRADS 3 count, number of biopsies and unnecessary follow up with estimated sensitivity of tomosynthesis was 83.33%, the specificity was 89.74%, the positive predictive value was 78.95%, the negative predictive value was 92.11%, and the accuracy was 87.71% while the sensitivity of mammography was 72.22%, the specificity was 71.79%, the positive predictive value was 54.17%, the negative predictive value was 84.85%, and the accuracy was 71.92%.
The high value of false positives in asymmetry was explained by Sickle [Citation14], who explained this due to high recall patients with abnormal one-view-only findings as they may represent cancers that are either obscured by superimposed glandular tissue or not included in the field. Also, the focal asymmetry is usually managed with short-interval follow-up rather than biopsy.
Architectural distortions are false negatives that typically accompany tissue overlap, so the level of contribution by 3DBT to diagnostic performance is high. [Citation15]
In the current study, 35 architectural distortions were detected by DBT, 30 lesions were evident in 2D mammography while the other five were hidden due to tissue overlap and were counted as false negatives for mammography. There was significant difference in BIRADS category of distortions between FFDM and DBT(P < 0.0001). The reported sensitivity, specificity, PPV and NPV for FFDM were 94%, 71%, 77%, and 92% compared to 94%, 82%, 85%, and 93 by DBT.
Near similar results were obtained by El Bakry [Citation16], who showed that DBT+FFDM had an overall better specificity and sensitivity (94–78%) than stand-alone FFDM (91–65%) respectively.
Partyka [Citation17] suggested that DBT improves the visibility of distortions and eliminates the pseudo-AD effects and with the aid of DBT, ADs that would otherwise remain hidden in DM can be revealed more readily with tomosynthesis than with 2D mammography.
For microcalcifications, 61/69 lesions were assigned to their correct BIRADS by FFDM based on their morphology and distribution. Five cases showed category increase to BIRADS 5 and were proved to be malignant while three were downgraded to BIRADS 2, related to skin calcifications and post-operative fat necrosis. In this study, DBT did not have a significant impact on assessment of microcalcifications compared to FFDM, as most of the lesions were evaluated according to their morphology, distribution in FFDM and assigned to its proper BIRADS category. No significant category changes were noted with DBT. However, it was able to detect concomitant masses, distortions, and confirm multifocality.
Similar observation was noted by Takamoto [Citation18], who reported that calcifications have much higher attenuation compared to normal breast tissue, so it is feasible to detect even in 2DMMG. This explains the low count of false negative lesions in micro calcifications .However, DBT enables stereoscopic recognition of calcification spread. Therefore, it will be a useful modality in the imaging of the extent of resections by surgeons during surgery. The same study concluded that there were significant category changes between DBT and FFDM as regards asymmetry, masses and architectural distortions.
Also, it was found that spatial resolution of micro calcifications is lower at DBT owing to tube motion, greater pixel size, and pixel binning, which affects lesion conspicuity and veils the volumetric distribution of calcifications from individual slices, resulting into a loss in calcification characteristics and morphology. [Citation19]
This study revealed that combined FFDM and DBT significantly improved the diagnostic performance with 95%CI to 96%, 95% as regards the sensitivity and specificity, positive and negative likelihood of malignancy 18.51 & 0.04, PPV& NPV to 94% compared to FFDM or DBT alone.
Similar results were concluded by Sanmugasiva [Citation20] that integrating DBT to FFDM allows good characterization of breast lesions and accurate diagnosis of cancer with sensitivity, specificity, PPV and NPV of mass lesions detected on DBT+ FFDM were 93.8%, 85.1%, 88.8%, and 91.5%, respectively. The PPV for calcification is 61.6% and asymmetry is 60.7% and 81.6%.
Helyie [Citation21] subjectively compared 3D DBT when characterizing known masses, architectural distortions, or asymmetries. They found that combined DM and 3D DBT achievement was better for diagnosis in 50% of cases. They concluded that 3D DBT might be an alternative to the additional mammographic views in most cases mostly in non-calcified concerned lesions.
In a similar study conducted by Basha MA et al, [Citation11] concluded that BIRADS with DBT was significantly superior to BIRADS with DM in breast cancer diagnosis (AUC: 0.883 vs. 0.619; p < 0.0001; 95% CI 0.214 to 0.313), and the BI-RADS with combined DM and DBT was significantly superior to BI-RADS with DM alone or BIRADS with DBT alone (AUC: 0.971; p < 0.0001; 95% CI 0.0565 to 0.120)
Ali et al [Citation22] concluded that 3D DBT significantly reduced the need for additional mammographic views and as well the frequent follow-up studies as it gave better characterization for all BIRADS 3 lesions and reduced the stress levels in women. And that scrolling the three-dimensional images for a particular view eliminates the tissue overlap seen in two-dimensional images and improves the resolution for a better diagnostic capability. In the current study, no additional views were used for evaluation of the lesions to reduce the radiation dose, as further processing was done while viewing the digital images on workstation such as zooming, changing contrast, and brightness to facilitate lesion detection. We believe that the role of additional views was considered being beyond our study.
With the increasingly wide spread of DBT, early detection and management of breast cancer are reached as tomosynthesis may reveal suspicious lesions that were not visible with 2D mammography. Consequently, we recommended the use of combined FFDM and DBT together with BIRADS for the assessment of non-mass findings for better diagnostic performance and lesions evaluation.
5. Conclusions
Digital breast tomosynthesis combined with FFDM are superior to FFDM alone in the assessment and changing BIRADS categorization of distortions and asymmetries. No significant value for DBT in changing BIRADS of microcalcifications.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Burhenne HJ, Burhenne LW, Goldberg F, et al. Interval breast cancers in the screening mammography program of British Columbia: analysis and classification. AJR Am J Roentgenol. 1994;162:1067e71.
- Park JM, Franken EA Jr, Garg M, et al. Breast tomosynthesis: present considerations and future applications. Radiographics. 2007;27:S231–S240.
- Harvey JA, Nicholson BT, Cohen MA. Finding early invasive breast cancers: a practical approach. Radiology. 2008;248(1):74–76.
- Casti P, Mencattini A, Salmeri M, et al. Towards localization of malignant sites of asymmetry across bilateral mammograms. Comput Methods Programs Biomed. 2017;140:11–18.
- Rose SL, Tidwell AL, Bujnoch LJ, et al. Implementation of breast tomosynthesis in a routine screening practice: an observational study. AJR Am J Roentgenol. 2013;200(6):1401–1408.
- Durand MA. Synthesized mammography: clinical evidence, appearance, and implementation. Diagnostics (Basel). 2018;8(2):22. Department of Radiology, Yale University School of Medicine, New Haven, CT 06412, USA.
- Durand MA, Wang S, Hooley RJ, et al. Tomosynthesis-detected architectural distortion: management algorithm with radiologic-pathologic correlation. Radiographics. 2016 Mar;36(2):311–321.
- Stepanek T, Constantinou N, Marshall H, et al. Changes in the utilization of the BI-RADS category 3 assessment in recalled patients before and after the implementation of screening digital breast tomosynthesis. Acad Radiol. 2019;26:1515–1525.
- Bahrs SD, Otto V, Hattermann V, et al. Breast tomosynthesis for the clarification of mammographic BI-RADS 3 lesions can decrease follow-up examinations and enables immediate cancer diagnosis. Acta Radiol. 2018;59:1176–1183.
- Andersson I, Ikeda DM, Zackrisson S, et al. Breast tomosynthesis and digital mammography: a comparison of breast cancer visibility and BIRADS classification in a population of cancers with subtlemammographic findings. Eur Radiol. 2008;18:2817–2825.
- Basha MA, Safwat HK, Eldin AM, et al. The added value of digital breast tomosynthesis in improving diagnostic performance of BI-RADS categorization of mammographically indeterminate breast lesions. Insights Imaging. 2020 Dec;11(1):1–2.
- Galati F, Marzocca F, Bassetti E, et al. Added value of digital breast tomosynthesis combined with digital mammography according to reader agreement: changes in BI-RADS rate and follow-up management. Breast Care. 2017;12(4):218–222.
- Mokhtar O, Gamal G, Naguib E, et al. 3D digital breast tomosynthesis versus US in evaluating breast asymmetries. Egypt J Radiol Nucl Med. 2020 Dec;51(1):1.
- Sickles EA. The spectrum of breast asymmetries: imaging features, work-up, management. Radiol Clin North Am. 2007;45:765–771.
- Mall S, Lewis S, Brennan P, et al. The role of digital breast tomosynthesis in the breast assessment clinic: a review. J Med Radiat Sci. 2017 Sep;64(3):203–211.
- El Bakry RAR. Breast tomosynthesis: a diagnostic addition to screening digital mammography. Egypt J Radiol Nucl Med. 2018;49(2):529–535.
- Partyka L, Lourenco AP, Mainiero MB. Detection of mammographically occult architectural distortion on digital breast tomosynthesis screening: initial clinical experience. Am J Roentgenol. 2014;203:216–222.
- Takamoto Y, Tsunoda H, Kikuchi M, et al. Role of breast tomosynthesis in diagnosis of breast cancer for Japanese women. Asian Pac J Cancer Prev. 2013 Jan 1;14(5):3037–3040.
- Teertstra H, Loo C, van Den Bosch M, et al. Breast tomosynthesis in clinical practice: initial results. EurRadiol. 2010;20(1):16–24.
- Sanmugasiva VV, Hamid MT, Fadzli F, et al. Diagnostic accuracy of digital breast tomosynthesis in combination with 2D mammography for the characterisation of mammographic abnormalities. Sci Rep. 2020 Nov 26;10(1):1.
- Helvie MA. Digital mammography imaging: breast tomosynthesis and advanced applications. Radiol Clin. 2010 Sep 1; 48(5):917–929.
- Ali EA, Adel L. Study of role of digital breast tomosynthesis over digital mammography in the assessment of BIRADS 3 breast lesions. Egypt J Radiol Nucl Med. 2019 Dec 1;50(1):48.
