ABSTRACT
Background: Patient-centered care has been considered the foundation of healthcare quality and the core competency of the doctor-patient relationship.
Aims: To assess the attitudes of medical students toward a patient-centered approach and identify the predictors of patient-centeredness scores.
Methods: A cross-sectional study was carried out in Fayoum Medical School/Egypt using a validated Arabic version of the Patient-Practitioner Orientation Scale (PPOS).
Results: The total PPOS score showed variable score as the grades move up. The total PPOS ranged from 0.05 to 4.39 with an average score of (2.71 ± 0.66) for the entire sample. The sharing and caring subscale score ranged from 0.56 to 4.44 and 0.44 to 5.33 with an average score of (2.33 ± 0.49) and (3.09 ± 0.92) respectively.
Conclusion: Medical students had low patient-centered attitude. Medical curricula should be redesigned, and medical students may also benefit from engagement in patient healthcare service.
1. Introduction
Patient-centered care is considered the foundation of healthcare quality and the core competency of doctor-patient relationship. World Health Organization defines patient-centered care as the degree of orientation of healthcare service toward the health needs and expectations of individuals rather than just managing the disease. The holistic view of patient-centered care embraces the perspectives of individuals, families, and communities, and envisions them as not only beneficiaries but also partners of the healthcare system. Moreover, it provides the patients with the information and support they need to make decisions, foster their engagement, and participate in their own care [Citation1,Citation2]. As a result, the concept of patient-centered care has received increased attention in medical practice [Citation3,Citation4].
Effective interpersonal communication between the healthcare provider and patients was the core component of patient-centered care that fosters shared insights establishing a common ground of trust and understanding [Citation3]. The core elements of patient-centered care are: listening to and respecting patients’ values, preferences, and expressed needs; ensuring coordination and integration of care through flexible policies, procedures, and provider practices; educating patients by sharing complete and unbiased information; providing emotional support; family engagement in health care; strengthening the continuity and ensuring timely access to care [Citation5].
Patient-centered care not only builds caring and compassion between healthcare providers and patients, but also reduces the cost of medical care and creates a positive sustainable healthcare experience [Citation6,Citation7]. Hence, it improves patient satisfaction, patients’ quality of life and reduces anxiety associated with the health state or accessing healthcare facilities [Citation8].
The current study aimed to assess the attitudes of medical students toward a patient-centered approach and elaborate the predictors of patient-centeredness.
2. Subject and methods
2.1. Study design and setting
A cross-sectional study was carried out in Fayoum Medical School/Egypt.
2.2. Study participants and sampling
The study population were medical students from academic years (first, second, and third grades) and clinical years (fourth, fifth, sixth, and interns’ grades). The total number of students at Fayoum Medical School is 1582 in August 2019.
The sample size was calculated by Epi Info 2000 according to number of students attending the medical school in August 2019. With a confidence interval of 99% and a total sample size of 469 students were determined. From each grade we randomly selected students. Students who agreed to participate were included in the study. Thirty-two students refused to participate, so the final sample was 437 with a response rate of 93.2% which minimizes the potential response bias. The academic medical students completed the questionnaire at classrooms after obtaining permission from the instructors before distributing the questionnaire forms. Students at the clinical years completed the questionnaire after finishing their clinical classes. On the other side, the data were collected from interns by disseminating the questionnaire during their practicum time compared to other grades. The aim of the study was explained to participants and confidentiality was assured. Written consent forms were taken from all the students.
2.3. Study tool and data collection
The study data were collected using an Arabic version of the validated Patient-Practitioner Orientation Scale (PPOS). The Patient-Practitioner Orientation Scale [Citation9] consists of 18-items scale with two subscales: (1) Sharing and (2) Caring. The PPOS was considered because it has been widely used in similar studies in different cultures; has been proven to have good psychometric characteristics [Citation10–12]; and its two sub-scales are contemporary elements in medical practice [Citation13]. The sharing sub-scale includes nine items measuring the degree to which the students believe that information should be shared between the health professional and the patient. The caring sub-scale consists of nine items that measure how students see the support, passion, and the holistic approach in doctor-patient relationship. It also reflects the student’s perception about the expectations form and patient’s needs, as an obstacle in the treatment process or not.
The questionnaire is divided into two sections. The first section covered the socio-demographic characteristics, including age, gender, and academic grades of students. The second section included 18 statements that covered the two aspects of PPOS; the caring (nine items) and the sharing (nine items). A six-point Likert scale was used to each statement ranging from 1 (strongly disagree) to 6 (strongly agree). Three statements were phrased in a way that their score does not need to be reversed to match with other items in the same scale. The overall PPOS score calculated as the mean of the scores for the 18 items and were ranked according to the Krupat et al. [9] classification of participants to be more patient centered with a mean score ≥5.00 and more doctor centered with mean score ≤4.75 for doctor centered. The PPOS questionnaire designed in English was translated into Arabic; the validity of the translation was assured by a process of forward and backward translation with personnel who are fluent in both languages.
2.4. Validity and reliability of the Arabic version
The face and content validity of the translated Arabic version of Patient-Practitioner Orientation Scale (PPOS) were examined in a pilot sample of 60 participants (the sample was increased from 10% to 12%, to decrease the response bias) by five experts (statisticians).
A 4-point Likert scale was used including 1 = not relevant, 2 = somewhat relevant, 3 = relevant, and 4 = very relevant. Ratings of 1 and 2 were considered content invalid while ratings of 3 and 4 were considered content valid. A 3-point Likert scale was used for the clarity and essentiality scale. The clarity scale was: 1 = not clear, 2 = need revision; and 3 = clear, and for essentiality: 1 = not essential; 2 = somewhat essential; and 3 = essential. The content validity ratio (CVR) was assessed using Lawshe sheet via this formula (Ne – N/2)/(N/2), where Ne is the number of experts indicating an item as “essential” and N is the total number of experts. A CVR score ≥ 0.62 was considered good. The content validity index (CVI) was calculated by adding all items with I-CVI equal to 1 divided by the total number of items. A CVI score > 0.80 was considered acceptable [Citation14]. Items with highest loadings of 0.30 and above were subjected to a reliability test. Significant factors > 0.30 were tested for internal consistency using Cronbach’s Alpha. Intraclass correlation coefficient (ICC) value > 0.75 was considered excellent [Citation15]. Cronbach’s alpha ≥ 0.70 was chosen to be significant. Bivariate correlations [Citation16] were run to investigate the factor distinctiveness of the final factor solution. A total correlation of an item ≥ 0.4 was considered acceptable
3. Data analysis
Statistical analysis was performed using SPSS (Statistical Package for Social Sciences) Version 21 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp). The mean and standard deviation were calculated for quantitative variables in the form of simple descriptive analysis and one-way ANOVA [Citation17] were used as a test of significance; p-value of ≤0.05 was considered statistically significant. Logistic regression analysis using dichotomous variables was done to test for risk factors associated with PPOS.
4. Results
Female students constituted 57% of the study sample while the academic and clinical students were 133 with a percent of 30.4% and 311 students with a percent of 71.2% respectively. The fourth grade formed most of the participants (158)(35.5%) followed by sixth grade students (79) students (17.2%). While third grade (29) students formed 7.8% of the study sample.
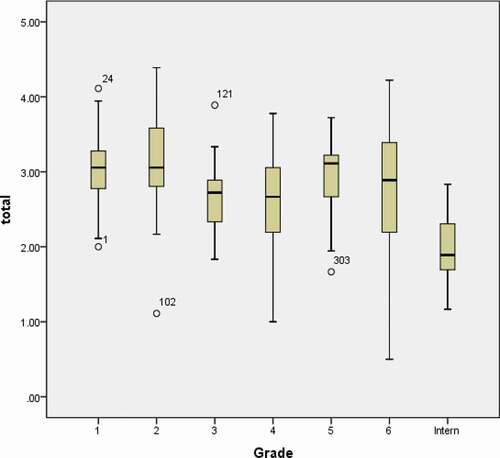
The total PPOS ranged from 0.05 to 4.39 with an average score of (2.71 ± 0.66) for the entire sample. The sharing and caring subscale score were ranged from 0.56 to 4.44 and 0.44 to 5.33 with an average score of (2.33 ± 0.49) and (3.09 ± 0.92) respectively. The total PPOS score did not show a constant increase as the grades moved up, rather it was variable ().
Interns showed the lowest total PPOS score (1.96 ± 0.40), sharing (2.05 ± 0.69) and caring subscales (1.88 ± 0.55) ().
Table 1. Distribution of patient-centeredness scores of participants by grade (N = 437)
There was a significant difference between academic, clinical students, and interns in sharing, caring, and total PPOS, p < 0.05. Regarding gender, there is no significant difference between female and male students (p > 0.05). However, female students showed higher mean scores of total PPOS (7.75 ± 0.69), sharing subscale (2.38 ± 0.71), and caring subscale (3.13 ± 0.95) than male students in total PPOS (2.66 ± 0.63); sharing subscale (2.26 ± 0.66) and caring subscale (3.05 ± 0.87) ().
Table 2. Relationship between PPOS subscales and grade, gender (N = 437)
Logistic regression analysis was performed to show the significant predictors affecting PPOS. Interns were found to be a significant predictor, for low sharing and total PPOS with P < 0.00. The interns are about 1.81 folds risk to develop low PPOS compared to clinical grades and 2.64 folds risk compared to academic ().
Table 3. Multivariate logistic regression analysis for predicting score of total PPOS and subscales (N: 437)
5. Discussion
The main aim of this study was to investigate the patient-centered attitudes and to detect the type of doctor-patient relationship endorsed by medical students using the Patient-Practitioner Orientation Scale (PPOS) and to detect the predictors of patient centered attitude.
The study results have reflected that students endorsed a doctor-centered attitude from the beginning of their medical study as their total PPOS in the first grade was 3.01 and throughout their undergraduate education and it did not increase but it tends to decrease as the students move to higher grades. On the other hand the caring subscale was higher in the same way as the findings reported by Mohamed et al. [Citation18] indicating that students tend to care about the patient emotions and needs rather than involving patient in decisions making. These results reflecting students’ attitude at the beginning of their study could explain the role of cultural elements in creating differences in the doctor patient relationship inter-countries.
The total PPOS score was low (2.71 ± 0.66) with low sharing and caring subscales indicating students with doctor-centered attitude. It was slightly higher than scores of South African medical students (2.25–2.65) [Citation19,Citation20]. But it was lower compared to other parallel studies in Sudan, Mali and Pakistan with total PPOS sores of 3.75, 3.38, and 3.40 respectively [Citation18,Citation21,Citation22]. Furthermore, it was extremely lower compared to the results of medical students in US (4.57) and Brazil (4.66) [Citation10,Citation23].
The low figures of total PPOS score and lower sharing and caring subscales could be due to insufficient training on comprehensive communication skills and decision-making skills in medical schools curricula [Citation24]. Students in their academic and clinical years in the traditional system of medical education were focusing more on gaining biomedical knowledge and technical skills with lack of contact with patients and insufficient courses dealing with communication, ethics and doctor-patient relationship. This could explain the no difference in students attitude as no difference was found in PPOS scores among the different grades, but it tends to decrease, this was in agreement with a Canadian study reported that the PPOS score did not change with student grade or semester [Citation25]. Declining in the total PPOS score and acquiring more doctor-centered attitude was found among medical students with higher academic grades also in Sudan and South Africa [Citation18,Citation19].
On the other hand some studies reported significant increase in the PPOS score with higher grades [Citation10,Citation21]. Also, Wahlqvist et al. [Citation12] reported small steady increase in the total PPOS score especially among female students who already had higher score from the beginning. This is somehow consistent with the current study results as contrary to traditional assumptions, we found no significant difference between males and females but we found females had slightly higher scores. Other studies reported that females had better patient centered and caring oriented behavior related to their best practice for communication [Citation3].
The current study results showed that interns have significant lower total PPOS, sharing and caring scores compared to students in academic or clinical grades. We found that being intern is significant predictor to have more doctor centered attitude and to have lower sharing skills. In Egypt medical students after six years of academic and clinical study have a mandatory year of training as intern before graduation. During this year intern practice the same duties as a physician except prescribing medication. This was consistent with several studies that found involvement in the real clinical practice tends to develop more doctor centered attitude and decrease both the sharing and the caring subscales [Citation3,Citation26]. This could be explained by unpreparedness and pressure felt by interns. Rosewilliam et al. [Citation27] reported that development of a doctor-centered attitude during clinical practice is due to pressure experienced by physicians serving in the health systems. In the contrary of what was assumed in improvement in their attitude once they directly interact with patients and senior physicians that were considered as a role model comparing with the academic years that focus only on biomedical aspects [Citation28].
6. Study strengths and limitations
As far as we know this is the first study dealing with PPOS in our country, covered the entire medical grades with a response rate of 93.2%. Regarding limitations, the responses could be the student’s perceptions rather than the actual status.
The low availability and willingness of students to participate were a big challenge during data collection. The second challenge is decreasing their ability to communicate experiences and opinions in an expressive and reflective manner. Some of the respondents were skeptical of the topic. Some were responding, taken in their considerations, the low abilities of the patients to share in making decision about their health.
Patient-centeredness is important concept that needs special attention, including further research both at undergraduate and postgraduate level. Longitudinal studies are recommended to accurately assess the degree of change in the patient centered attitude.
7. Conclusion and recommendations
The study concluded that medical students had low patient-centered attitude and the total PPOS score did not change by increasing but it tend to decrease in higher grades. Gender did not significantly affect the attitude of the students but being an intern was predicting adapting more doctor-centered attitude. Medical curricula especially communication curricula should be examined and redesigned using more problem-based and situation-based methods of education to change attitude, improve knowledge, and develop skills of patient-centered care. Medical students may also benefit from active participation in patient care. Additionally, real situations and interaction with senior physicians will enhance the acquisition and maintenance of patient-centered care skills through positive role modeling.
Patient-centeredness is important concept that needs special attention, including further research both at undergraduate and postgraduate level. Longitudinal studies are recommended to accurately assess the degree of change in the patient-centered attitude.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- World Health Organization. WHO global strategy on people-centered and integrated health services. Geneva: World Health Organization; 2015. [cited 2020 May 7]. https://www.who.int/servicedeliverysafety/areas/people-centred-care/global-strategy/en/
- Hammerich K, Stuber K, Hogg-Johnson S, et al. Assessing attitudes of patient-centered care among students in international chiropractic educational programs: a cross-sectional survey. Chiropr Man Therap. 2019;27:46.
- Ishikawa H, Son D, Eto M, et al. Changes in patient-centered attitude and confidence in communicating with patients: a longitudinal study of resident physicians. BMC Med Educ. 2018;18:20.
- Donetto S. Medical students and patient-centered clinical practice: the case for more critical work in medical schools. Br J Soc Educ. 2012;33(3):431–449.
- Kitson A, Marshall A, Bassett K, et al. What are the core elements of patient‐centered care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J Adv Nurs. 2013;69:4–15.
- Kidd MO, Bond CH, Bell ML. Patients’ perspectives of patient-centeredness as important in musculoskeletal physiotherapy interactions: a qualitative study. Physiotherapy. 2011;97(2):154–162.
- De Silva D. Helping measure person-centered care: a review of evidence about commonly used approaches and tools used to help measure person centered care. London: The Health Foundation; 2014.
- Archer E, Bitzer EM, Van Heerden BB. Interrogating patient-centeredness in undergraduate medical education using an integrated behavior model. S Afr Family Pract. 2017;59(6):219–223.
- Krupat E, Yeager CM, Putnam S. Patient role orientations, doctor-patient fit, and visit satisfaction. Psychol Health. 2000;15(5):707–719.
- Ribeiro MMF, Krupat E, Amaral CFS. Brazilian medical students’ attitudes towards patient-centered care. Med Teach. 2007;29(6):e204–e208.
- Al-Bawardy R, Blatt B, Al-Shohaib S, et al. Cross-cultural comparison of the patient-centeredness of the hidden curriculum between a Saudi Arabian and 9 US medical schools. Med Educ Online. 2009;14: 19. DOI:https://doi.org/10.3885/meo.2009.T0000144
- Wahlqvist M, Gunnarsson RK, Dahlgren G, et al. Patient-centred attitudes among medical students: gender and work experience in health care make a difference. Med Teach. 2010;32(4):e191–e198.
- McCormack B. A conceptual framework for person‐centered practice with older people. Int J Nurs Pract. 2003;9(3):202–209.
- Lawshe C. A quantitative approach to content validity. Personnel Psychol. 1975;28(4):563–575.
- Koch G. Intraclass correlation coefficient. In: Kotz S, Johnson NL, editors. Encyclopedia of statistical sciences. 4. New York: John Wiley & Sons; 1982. p. 213–217.
- Field, A. (2009) Discovering Statistics using SPSS. 3rd Edition, London: Sage Publication Ltd.
- Fisher R. Studies in crop variation. J Agric Sci, Cambridge. 1921;11: 107–135.
- Mohamed KG, Hunskaar S, Abdelrahman SH, et al. Impact on core values of family medicine from a 2-year Master’s program in Gezira, Sudan: observational study. BMC Fam Pract. 2019;20:145.
- Archer E, Bezuidenhout J, Kidd M, et al. Making use of an existing questionnaire to measure patient-centered attitudes in undergraduate medical students: a case study. Afr J Health Prof Educ. 2014;6(2):150–156.
- Archer E, Van Heerden BB. Undergraduate medical students’ attitudes towards patient-centeredness: a longitudinal study. MedEdPublish. 2017;6:47.
- Hurley EA, Doumbia S, Kennedy CE, et al. Patient centered attitudes among medical students in Mali, West Africa: a cross sectional study. BMJ Open. 2018;(2018(8):e019224.
- Ahmad W, Krupat E, Asmaa Y, et al. Attitudes of medical students in Pakistan toward the doctor-patient relationship. PeerJ PrePrints. 2014;2:e606v1.
- Haidet P, Dains JE, Paterniti DA, et al. Medical student attitudes toward the doctor-patient relationship. Med Educ. 2002;36:568–574.
- Hoffmann TC, Bennett S, Tomsett C, et al. Brief training of student clinicians in shared decision making: a single-blind randomized controlled trial. J Gen Intern Med. 2014;29(6):844–849.
- Dwamena F, Holmes‐Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12:CD003267.
- Grilo AM, Santos MC, Rita JS, et al. Assessment of nursing students and nurses’ orientation towards patient-centeredness. Nurse Educ Today. 2014;34(1):35–39.
- Rosewilliam S, Indramohan V, Breakwel R, et al. Patient centered orientation of students from different healthcare disciplines their understanding of the concept and factors influencing their development as patient centered professionals: a mixed methods study. BMC Med Educ. 2019;19(1):347.
- McNair R, Griffiths L, Reid K, et al. Medical students developing confidence and patient centeredness in diverse clinical settings: a longitudinal survey study. BMC Med Educ. 2011;201(16):176.