ABSTRACT
Background
Cardiovascular diseases (CVDs) are on the rise in Sub-Saharan Africa. The management of these CVDs comes at an exorbitant cost to both individuals and health institutions. However, data on the economic impact of the most common CVDs in Ghana are lacking. Our objective was to describe the in-patient cost and outcomes of acute CVD admissions in a leading teaching hospital in Ghana.
Methods
We retrospectively reviewed hospital admissions, cost of hospitalization, length of stay, and CVD outcomes following admissions between January 2018 and December 2019.
Results
A total of 1975 patients with a mean age of 62.2 (±16.1) years were admitted over the study period of which 52.6% were males.The top 3 most prevalent CVDs among admitted patients were stroke(48.5%), hypertensive urgencies/emergencies(42.7%), and heart failure(29.4%). The overall case fatality rate (CFR) was 21.5% (95% CI: 19.7%−23.3%). The CFR for stroke, hypertensive urgencies/emergencies, and heart failure were 28.9%, 17.6%, and 14.1%, respectively. Median (IQR) length of stay and cost of treatment across all CVDs was 5(3–9) days and USD $195.29(137.9–288.9), respectively. The highest median cost for admission was for stroke (USD $211.19).
Conclusion
The average cost of CVD hospitalization is over a hundred times the daily minimum wage of the average Ghanaian. A greater emphasis on primordial and primary prevention is warranted to curtail the economic burden of CVDs in developing economies such as Ghana.
1. Background
The epidemic of cardiovascular diseases (CVDs) continues to ravage humanity as the number one cause of mortality globally. CVDs account for over three quarters the mortality burden in low and middle-income countries [Citation1]. They are projected to double by 2030 [Citation2]. Indeed CVDs will outnumber infectious disease as the number one cause of mortality in developing countries by 2030 [Citation3]. Furthermore, the associated Disability Adjusted Life Years (DALYs) lost to CVDs, as reported by the Global Burden Of Disease group, is also projected to increase by 55% between 1990 and 2020 in adults less than 65 years in developing countries while upper-middle income countries like China are projected to see a 70% increase in DALYs in 2020 [Citation4]. In contrast, developed countries have experienced a 14.3% decrease in DALYs lost to CVDs over the same period [Citation5]. The percentage of heart failure admissions in Ghana predominantly increased by 78% between 2004 and 2014 [Citation6]. Similar trends in stroke and diabetes admissions and mortality rates have been observed spanning three decades in central Ghana [Citation7,Citation8].
In a developing country with very limited resources, the efficient allocation of health resources requires an understanding of costs for CVD health care. Though previous studies in this field have largely analyzed rates and trends in common CVDs such as stroke and heart failure, more attention should be given to the associated cost that impacts affected individuals, health systems, and national economies. This knowledge gap potentially undermines the collective effort to achieve Sustainable Development Goal (SDG) number 3.4, which seeks to reduce by one-third premature mortality from Non-Communicable Diseases (NCDs) through prevention and treatment, and promote mental health and wellbeing [Citation9]. Data on the economic burden CVD admissions impose on society provides valuable information on healthcare resource utilization that could inform cost-effective national policy interventions. Thus, this study aimed to describe the in-patient cost and outcomes of CVD admissions in a leading teaching hospital in Ghana.
2. Methodology
2.1. Study design
A retrospective study of hospital admissions, cost of admissions, length of stay and deaths from January 2018 to December 2019 was performed using a hospital registry.
2.2. Study site
Komfo Anokye Teaching Hospital (KATH), a leading tertiary referral institution in Ashanti Region, Ghana, serves an estimated population of over 12 million from 10 out of the 16 administrative regions of Ghana.
2.3. Study population
All patients admitted to the medical wards during the study period and whose records were documented in the admissions and discharge registers were considered for the study. However, only information and data from patients with at least one CVD diagnosis were extracted upon discharge from the wards. In this study, CVD was defined as a disease that affects the heart and blood vessels. The main blocks of International Classification of Diseases 10th version (ICD−10) [Citation10] were used to sort out the final diagnoses in the register to group them into the various CVDs.
2.4. Study procedure
Trained data research assistants extracted data from the hospital registry using a standardized data extraction form. The extracted patient information in the registers included: Dates of admission and discharge or death, address, age, sex; initial diagnosis (presenting or admission diagnosis), final diagnosis, and duration of hospital stay. In addition, outcome variables like discharge, transfer to other wards, death, and hospital stay time were noted. The data extracted from the patients’ record were entered into a study database. It was then cleaned by double checking with the original source document by a different person.
2.5. Outcomes
In this study, cost was defined as the direct medical cost of treating CVDs and any related complications during hospitalization, including some basic diagnostic laboratory testing (such as full blood count, renal and liver function tests, lipid profile), and prescription drugs covered by the National Health Insurance Scheme (NHIS), physiotherapy and medical supplies. This study did not capture other out-of-pocket expenses for services such as a computerized tomography (CT), magnetic resonance imaging (MRI), electrocardiographs (ECGs), and echocardiograms (Echo). The cost of treatment was first converted from Ghana cedis to US dollars based on the average exchange rate of GHC5.10 to a USD from January 2018 to December 2019. Next, the length of stay was defined as the total number of days spent from admission to discharge or death whichever came first. Finally, the cost difference was defined as the difference in cost of treatment between patients who died and those who survived a particular CVD.
2.6. Data management and statistical analysis
The data was subsequently exported to Stata SE version 15.1 for further validation and analysis. Since many patients had more than one diagnosis, each diagnosis was dichotomized into one variable indicating if the condition is present or absent in the patient. Persons with either hemorrhagic or ischemic strokes were categorized as having stroke. The proportion of eligible patients with the respective CVDs determined the prevalence of the various CVDs. The top seven CVDs were selected based on this prevalence, and the rest were grouped as “Other CVDs.” The lengths of stay and treatment cost for the CVDs were stratified into those who died and survived and summarized using the median and interquartile ranges. The crude differences between the cost of treatment (with their 95%CI) for patients who died and those who survived was determined and plotted for each CVD. To determine the adjusted independent cost difference between patients who died and those that survived each CVD, a multivariate quantile regression model was used where adjustment for patients’ age, presence of lower respiratory infection and other CVDs was done.
2.7. Ethical considerations
The Committee on Human Research Publication and Ethics (CHRPE) of the Komfo Anokye Teaching Hospital (KATH), Kumasi approved this study.
3. Results
3.1. Baseline demographics and mortality of CVDs
A total of 1975 patients were admitted for various CVDs between January 2018 and December 2019. The top 3 causes of CVD admissions were stroke (48.5%), uncontrolled hypertension (42.7%) and heart failure (29.4%) (). The mean (±SD) age for all patients at admission was 62.2(±16.1)years and 52.6% were males. The lowest and highest proportions of males were seen in patients with other CVDs (30.3%) and COPD (68.9%), respectively. The global CVD fatality rate was 21.5% (95%CI: 19.7% − 23.3%). Atrial fibrillation carried the highest case-fatality rate of 33.8% while valvular heart disease had the lowest (5.3%).
Table 1. Demographics and outcomes of patients with CVDs.
3.1.1. Length of stay in hospital
The median (IQR) length of stay in days for all patients was 5 (3–9). For patients who died and survived, their median (IQR) lengths of stay in days were 5 (3–9) and 4 (2–9) respectively. This difference was not statistically significant (p = 0.112). The median (IQR) number of days spent by stroke survivors was 6 (3–10) days compared to 4 (2–9) days for those who died. Heart failure survivors spent fewer days on admission compared to those who died 4(2–8) vs 6(3–11). Patients with Cor-Pulmonale who died spent ten and a half days compared to 5 days for those who survived ()
Table 2. Distribution of length of stay for survivors and non-survivors.
3.1.2. Cost of admissions
The median (IQR) cost per treatment of patients with CVDs was USD $195.29 (137.90–288.90). Those for patients who survived and died, respectively, were USD $193.45 (138.37–277.94) and USD $203.27 (132.76–319.52). The difference in cost was not statistically significant (p = 0.233). Of all CVD cases, the overall median cost of admission for stroke was the highest at USD $211.19, this was higher among survivors compared to those who died. The median cost among patients who died was highest for Cor-Pulmonale patients and lowest for patients with valvular heart disease. Of the top three CVD cases, median cost for a stroke survivor was the highest at USD $215.03 while heart failure patients who died had the highest median cost of admission ( & )
Figure 1. Cost difference (treatment cost for deaths – treatment cost of survivors) for the various CVDs.
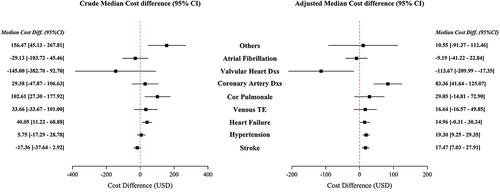
Table 3. Distribution of treatment cost in USD by outcome (died or survived).
3.1.3. Cost difference and CVDs
illustrates the difference in cost of treatment between patients who died and those that survived. The crude difference indicated that the median cost for patients who died was significantly higher than those who survived for COPD, heart failure, and other CVDs. However, after adjusting for each CVD, the presence of lower respiratory tract infections and the patient’s age, it was observed that CAD, uncontrolled hypertension, and stroke were independent predictors of a higher cost of treatment in patients who died compared to those who survive their admission.
4. Discussion
4.1. Summary of results
This is the first attempt to report findings of the cost of treating CVDs in Ghana. We sought to describe the in-patient cost and outcomes of CVD admissions in the second largest teaching hospital in Ghana. Stroke, uncontrolled hypertension (hypertensive urgencies and emergencies) and heart failure constituted the top three most common CVD admissions. On average, stroke survivors and Heart failure non-survivors spent a similar number of days on admission. We found that the median in-patient cost of CVD hospitalization was USD $195.29. Similarly, the median cost for all survivors was USD $193.45 and USD $203.27 for non-survivors. Of all admitted CVD cases, stroke admissions accounted for the highest cost at USD $211.19. Again, of the top 3 CVD admissions, the median cost for a stroke survivor was the highest at USD $215.03 while the median cost for patients who succumbed to heart failure was also the highest at USD $215.48. Compared to survivors, Coronary artery disease, hypertension, and stroke were independent predictors of a higher cost of hospitalization among patients who died than those that survived of these CVDs.
4.2. Comparison with previous research
The global cost of CVD has been estimated to be US $863 billion in 2010, or an average per capita cost of US $125, estimated to rise to US $1044 billion in 2030 [Citation11]. This compares to median cost per patient in this study of US $ 195. Indeed this figure may be an underestimation given this estimate does not capture data on out-of-pocket expenditures for some diagnostic and prescription medications operating on a “cash and carry” basis. Though relatively available in the developed world compared to the developing world, data on cost estimates for CVD admissions shows substantial variation in cost estimates. In developing countries, however, the need for more data and the heterogeneity in the methodology employed makes it even more challenging to compare. One thing, however, remains clear that, as CVD risk factors and hence CVD prevalence increase, its associated cost of care undoubtedly will increase. Again, as developing countries enter the delayed degenerative disease phase sooner than later due to rapid health transition and improved care [Citation12], there is bound to be an increase in the cost of hospitalization.
One central finding of this study was that stroke of all admitted CVD cases cost the highest at a median estimate of USD $ 211.19, while stroke survivors spent the highest per admission among all CVD survivors. This estimate is consistent with the mean cost per case of USD $220 as reported in Tanzania [Citation13]. Despite slight variations in cost categories deployed and the number of patients and duration of follow-up, our results are mainly within range compared to other studies in Sub-Saharan Africa. For instance, the mean cost per stroke patient was USD $157 in Senegal and USD $282 in Congo [Citation14,Citation15]. Higher estimates have been reported in neighboring Nigeria. On average, it requires between USD $600 for government hospitals and USD $4860 for private facilities to access care within the first 36 weeks in the post-stroke affectation period [Citation16]. In this Nigerian study, this cost covered hospitalization, all investigations, physiotherapy and medication cost. This, together with the prolonged study duration of 36 weeks could explain the price variations compared to this current study, where cost covered the hospitalization including consumables, medications covered by the National Health Insurance Scheme (NHIS) that were available, basic laboratory investigations such as full blood count, renal function tests, liver function test, lipid profile. Other investigations or services such as MRI, Head CT scans, ECGs, Echocardiograms, ICU services, out-of-pocket expenses and some medications, which are not NHIS insured were not captured in the cost analysis in this study. The lack of infrastructure, advanced ICU care and such a detailed costing regime may account for the relatively lower cost estimates in the other countries in the Sub-region at the risk of underestimating the cost of treatment.
Heart failure is both a public health emergency and a costly health condition. As the burden of heart failure rises, its attendant management will continue to consume an ever-increasing share of the CVD health cost. The median cost of heart failure hospitalization in this study was USD $182 in keeping with reported studies in Congo, which range between USD $122 and USD $175. Three times this cost expenditure is observed in Nigeria [Citation17]. It sharply contrasts heart failure cost distribution as observed in high-income countries where a detailed costing regime is used in routine practice making it easier to compile comprehensive data on cost. In addition, there is increased utilization of expensive medical equipment and the routine use of highly advanced procedures like right heart catheterization in such high-income centers. In Nigeria notably, only a small proportion of the populace has access to a social health insurance and the out-of-pocket spending balloons the cost of healthcare way outside the remits of the ordinary citizen [Citation18].
It was observed in this study that the cost of treating non-survivors who had coronary artery disease, uncontrolled hypertension and stroke was significantly higher than the cost of admitting and treating those who survived these conditions. This finding has significant implications on efficient resource allocation and utilization. Furthermore, as the epidemic of CVDs continues to rage and more patients succumb to these conditions, the clinical significance of these findings will become even more apparent, thus placing enormous pressure on the limited health care systems to restrain costs.
4.2.1. Strengths and limitations of this study
The main strength of this study was that it is the first of its kind to the best of our knowledge, to attempt to report on the cost of treating CVDs in Ghana. This study brings to sharp focus the potential of conducting comprehensive cost-of-illness studies for stroke and heart failure, particularly as a barometer of the country’s economic strength. However, we did not include the cost of out-of-pocket expenditures, indirect cost by caregivers, transport to and from the hospital and alternative medication use. As a result, the estimated cost in this study may be significantly underestimated.
5. Conclusion
The costs of CVD hospitalization, mainly stroke and heart failure are high, about 100 times the daily minimum wage of the average Ghanaian. Therefore, cost-efficient strategies that combines pragmatic primordial and primary preventive measures with an aggressive CVD risk control program are highly warranted.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Notes on contributors
Lambert Tetteh Appiah
Lambert Tetteh Appiah is a Senior Specialist Physician, a cardiologist, Senior Lecturer and a researcher at the School of Medicine and Dentistry of the Kwame Nkrumah University of Science & Technology (KNUST-SMD), Department of Medicine.
Samuel Blay Nguah
Samuel Blay Nguah is a Senior lecturer at the School of Medicine and Dentistry and an honorary senior specialist affiliated to the Komfo Anokye Teaching Hospital (KATH).
Priscilla Abrafi Opare-Addo
Priscilla Abrafi Opare-Addo Physician specialist, senior registrar in neurology at Komfo Anokye Teaching Hospital , Kumasi, Ghana.
Setri Fugar
Setri Fugar An interventional cardiology fellow at the Medical College of Wisconsin. He has interest in CVD prevention and management among LMICs.
Jessey Mahama Holu
Jessey Mahama Holu is a data management officer with interest in CVD prevention
Yvonne Commodore-Mensah
Yvonne Commodore-Mensah is an associate Professor at Johns Hopkins School of nursing and a cardiovascular nurse epidemiologist whose current program of research seeks to reduce the burden of cardiovascular disease risk among Africans locally (United States) and globally (sub-Saharan Africa) through community-engaged research.
Bernard C. Nkum
Bernard C. Nkum is an Associate Professor at the Department of Medicine, School of Medicine and Dentistry and an Honorary Consultant Cardiologist affiliated to the Komfo Anokye Teaching Hospital (KATH).
Charles Agyemang
Charles Agyemang is a Professor of Global Migration, Ethnicity and Health, and Principal Investigator at Amsterdam University Medical Centres, University of Amsterdam (AMC-UvA). He is also currently the Vice President of the Migrant Health section of the European Public health Association; Scientific Chair of the Global Society of Migration, Ethnicity, Race & Health; and a fellow of the prestigious European Research Council (ERC) under the Consolidation Award program. He is the PI of the RODAM study (www.rod-am.EU) and has published extensively and edited several books.
Fred Stephen Sarfo
Fred Stephen Sarfo is a researcher, a clinician, an educator and a Neurologist who holds 2 doctoral degrees in Epidemiology and Molecular Medicine from Durham University, UK and the Kwame Nkrumah University of Science & Technology respectively. He is the PI of PINGS I and II studies amongst others. To date, he has over 193 peer-reviewed publications in Medical journals.
References
- World Health Organisation, Cardiovascular disease fact sheet [Internet]. [cited 2020 Apr 10]. Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-cvds
- Kariuki JK, Stuart-Shor EM, Leveille SG, et al. Methodological challenges in estimating trends and burden of cardiovascular disease in Sub-Saharan Africa. Cardiol Res Pract. 2015;2015:1–6. doi: 10.1155/2015/921021
- Mathers CD, Loncar D, Samet J. Projections of global mortality and burden of disease from 2002 to 2030. PLOS Med. 3(11): Samet J, editor:e442. 2006 Nov 28. 10.1371/journal.pmed.0030442
- Moran A, Zhao D, Gu D, et al. The future impact of population growth and aging on coronary heart disease in China: projections from the coronary heart disease policy model-China. BMC Public Health. 2008 Nov 27;8(1):394. DOI:10.1186/1471-2458-8-394
- Reddy KS. Cardiovascular diseases in the developing countries: dimensions, determinants, dynamics and directions for public health action. Public Health Nutr. 2002 Feb;5(1A):231–237. DOI:10.1079/PHN2001298.
- Appiah LT, Sarfo FS, Agyemang C, et al. Current trends in admissions and outcomes of cardiac diseases in Ghana. Clin Cardiol. 2017 Oct;40(10):783–788.
- Sarfo FS, Akassi J, Awuah D, et al. Trends in stroke admission and mortality rates from 1983 to 2013 in central Ghana. J Neurol Sci. 2015 Oct 15;357(1–2):240–245. DOI:10.1016/j.jns.2015.07.043
- Sarfo-Kantanka O, Sarfo FS, Oparebea Ansah E, et al. SecUlar trends in admissions and mortality rates from diabetes mellitus in the central belt of Ghana: a 31-year review. PLoS ONE. 2016;11(11):e0165905. DOI:10.1371/journal.pone.0165905
- WHO, Facts sheet. World Health Organisation | SDG 3: ensure healthy lives and promote wellbeing for all at all ages [Internet]. WHO. World Health Organization; [cited 2020 Apr 10]. Available from: http://www.who.int/sdg/targets/en/
- PDF_MI4632_ICD_9-10_Codes_for_Cardio_38365_062915.pdf [Internet]. [cited 2016 Dec 28]. Available from: https://www.questdiagnostics.com/dms/Documents/Other/PDF_MI4632_ICD_9-10_Codes_for_Cardio_38365_062915.pdf
- Bloom DE, Cafiero ET, Jané-Llopis E, et al. 2011. The global economic burden of non-communicable diseases.
- Wang S, Petzold M, Cao Jet al. Direct medical costs of hospitalizations for cardiovascular diseases in Shanghai, China. Medicine (Baltimore). InternetAvailable from2015 May 22[cited 2020 Sep 20]; 94(20): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4602857/e83710.1097/MD.0000000000000837.
- Kabadi GS, Walker R, Donaldson C, et al. The cost of treating stroke in urban and rural Tanzania: a 6-month pilot study. Afr J Neurol Sci. 2013;32(2):45–53.
- Gombet T, Ellenga-Mbolla BF, Ikama MS, et al. [Cost of emergency cardiovascular care at the university hospital center in Brazzaville, Congo]. [Internet]. [cited 2020 Sep 21]. Available from: https://read.qxmd.com/read/19499732/-cost-of-emergency-cardiovascular-care-at-the-university-hospital-center-in-brazzaville-congo
- Touré K, Ndiaye NM, Sène Diouf F, et al. Evaluation of the cost of stroke management in Dakar, Senegal. Med Trop Rev Corps Sante Colon. 2005 Nov;65(5):458–464.
- Birabi BN, Oke KI, Dienye PO, et al. Cost burden of post stroke condition in Nigeria: a pilot study. Glob J Health Sci. 2012 Aug 15;4(6):17. DOI:10.5539/gjhs.v4n6p17
- Ogah OS, Stewart S, Onwujekwe OEet al. Economic burden of heart failure: investigating outpatient and inpatient costs in Abeokuta, Southwest Nigeria. PLoS ONE. InternetAvailable from2014 Nov 21[cited 2020 Sep 21]; 9(11): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4240551/e11303210.1371/journal.pone.0113032.
- Soyibo A, Olaniyan O, Lawanson AO. National health accounts: structure, trends and sustainability of health expenditure in Nigeria. Afr J Econ Policy. 2007;14(1). [[cited 2020 Sep 21]]. InternetAvailable from: https://www.ajol.info/index.php/ajep/article/view/44195
