ABSTRACT
Background
Sepsis-associated encephalopathy (SAE) refers to multifactorial syndrome manifested by generalized cerebral dysfunction induced by systemic response to infections with no clinical or laboratory evidence of directly cerebral infections or other forms of encephalopathy. The electroencephalogram (EEG) is one of the methods that allow physicians to continuously monitor the cerebrum and help management decisions. We studied the EEG changes in predicting morbidity and mortality of SAE in critically ill cases suffering sepsis or septic shock.
Patients and Methods
In this prospective observational study, 80 cases with sepsis or septic shock were subjected to EEG recording to assess EEG changes in critically ill patients with SAE and its correlation with their morbidity and mortality.
Results
There was a statistically significant difference in prognostic performance for EEG grading between survivors and non survivors to predict mortality. The area under the curve (AUC) was 0.887, cut off was > 2#, sensitivity was 87.50 and specificity was 81.25 and accuracy was 83.75 as the higher the score was associated with higher mortality. There was statistically significant association between EEG grading and 28-day mortality (p-value ˂0.001). Also, there was statistically significant association between EEG grading and the need for mechanical ventilation and vasopressors (p-value ˂0.001). There was a significant association between EEG within 72 hours of admission and length of ICU stay (p-value ˂ 0.017).
Conclusion
Early EEG changes have a positive correlation with morbidity and mortality and can be used as a good predictor in cases suffering sepsis or septic shock presenting with SAE.
1. Introduction
Sepsis refers to a clinical syndrome that is manifested by physiological, biological, and biochemical changes as a result of an unbalanced host response to infections [Citation1].
Septic shock, a type of distributive shock, represents the commonest type of shock among cases admitted to intensive care unit (ICU) [Citation1].
Sepsis-associated encephalopathy (SAE) is described as multifactorial syndrome manifested by generalized cerebral dysfunction promoted via systemic responses to infections with no detected clinical or laboratory evidence of direct cerebral infections or other forms of encephalopathy (for example, hepatic or renal encephalopathy) or evidence of structural abnormality [Citation2].
The incidence of SAE is approximately fifty percent. It ranges between eight percent to seventy percent or more of cases with sepsis, based on the sepsis severity, patient’ profile, and SAE diagnostic features [Citation3].
Degree of encephalopathy is accompanied by increased mortality on grading using the Glasgow Coma Score (GCS) [Citation2].
Electroencephalogram (EEG) is a test used to detect electrical activity in the brain via the use of small, metal discs (electrodes) attached to the scalp. Neurons communicate via electrical impulses and are active all the time. The neurons’ activity appears in the form of wavy lines on recording the EEG [Citation4].
EEG changes determined in septic cases might denote the neurotoxic processes. Distinct EEG pattern that appears during sepsis includes absence of reactivity, excess theta and delta activity, electrographic seizure in addition to periodic discharge [Citation5].
The goal of our study was to investigate early EEG abnormalities in cases admitted to ICU with diagnosis of sepsis or septic shock presenting with SAE and its correlation with morbidity and mortality.
2. Patients and methods
The study included eighty adult patients of both sex who were in sepsis or septic shock based on sepsis surviving campaign 2021 [Citation6], with disturbed conscious level with GCS less than 15 admitted to Critical Care Medicine Department in Alexandria Main University Hospital according to sample size calculation. We excluded patients who were less than 18 years old, cases suffering neurological, hepatic, or renal diseases, patients receiving muscle relaxants, or who were post cardiac arrest not retaining their baseline conscious level. Approval of the Medical Ethics Committee of Alexandria Faculty of Medicine was obtained and written informed consent was taken from the next of kin prior to conducting the study as well.
3. Data collection
Patients included in our study were classified as survivors and non-survivors based on 28-day mortality. Demographic data (age, gender) as well as complete history taking, complete clinical examination including patients’ vital signs, laboratory investigations (including procalcitonin level, ABG and CRP) were done, neurological assessment was done via Glasgow coma score (GCS) and Richmond agitation Sedation Scale (RASS). Severity of the critical illness was evaluated by Acute physiology and chronic health evaluation (APACHEII score) [Citation7].
4. EEG recording and analysis
EEG recordings and analysis according to the guidelines of the International Federation of Clinical Neurophysiology for the usage of EEG inside the ICU [Citation8].
EEG was recorded within the first 72 hours of ICU admission, Standard EEG was carried out at the bedside via the use of a Nicolet v32 portable digital EEGsystem, twenty-one electrodes were placed depending upon the international10–20system’s instructions. EEG recording remained for30min.
Standardized EEG analysis included a description of basic parameters [Citation9]:
Predominant frequency (Alpha is 8-12 Hertz, beta >12 Hertz, theta4–8 Hertz or delta <4 Hertz).
EEG voltage was estimated from the peak to bottom, in longitudinal bipolar montage using standard ten-twenty electrodes (normal voltage equal twenty microvolt (μV); whereas low voltage less than twenty μV).
EEG reactivity was assessed via potent sound stimuli (like slapping hands, callingthe first name of the patient loudly) and painful stimulus (such as strong pinching of the arm of the patient, or the sternum). EEG reactivity includes changed intensity or frequency after applying these stimuli.
EEG findings in acute encephalopathy changes According to The EEG classification developed by Synek scale Includes [Citation5]: 1. Grade 0: normal EEG. 2. Grade 1: predominant alpha activity with or without some delta-theta activity. 3. Grade 2: predominant theta or delta activity with some alpha activity still detectable. 4. Grade 3: predominant theta or delta activity, no alpha activity. 5. Grade 4: low-voltage delta activity, burst suppression, alpha coma, theta coma, Periodic Discharges (Generalized periodic discharges occurring in short trains at about 1 Hz frequency). 6. Grade 5: electro-cerebral silence.
Outcome
Primary Outcomes: 28-day mortality rate was calculated.
Secondary Outcomes: Need for vasopressors, need for mechanical ventilation, and length of ICU stay.
Neurological outcome: was assessed 1 month after doing EEG using cerebral performance category score scale (CPC) [Citation10].
5. Statistical analysis of the data
Mean differences of age, APACHE II score, CRP, Procalcitonin, GCS on admission, and RASS of ventilated patients between survivors and non survivors were analyzed using Mann Whitney test. Mean arterial blood pressure (MAP), heartrate (HR), temperature, respiratory rate (RR), Paco2, Pao2, and Hco3 were analyzed using the Student t-test. The Chi-square test was used to compare between need for mechanical ventilation, need for vasopressors, EEG grading scale (synek scale), gender and past history in both groups. The correlation between EEG grading scale with length of ICU stay in total patients and CPC score in survivor patients was evaluated using spearman coefficient. The univariate logistic regression analysis was used to assess the effect of covariates on mortality. Agreement (sensitivity, specificity) for APACHE II score, procalcitonin, MAP, EEG and age where calculated to predict mortality. The results were analyzed using the IBM SPSS software package (version 20.0). Sample size was calculated using power analysis and sample size software (PASS2020) “NCSS, LLC. Kaysville, Utah, USA, ncss.com/soft ware/pass.” The minimum sample size required to achieve 80% study power and 95%confidence limits was 80 patients.
6. Results
Patients were classified into two groups, survivors (48 patients, 60%) and non-survivors (32 patients, 40%) according to 28-day mortality. Regarding the demographic data cases were selected randomly either males or females with no concern to specific gender, there were more males (53.8%) than females (46.3%) in the study population. Among males, 30 patients were survivors and 13 patients were non-survivors, while among females, 18 patients were survivors and 19 patients were non-survivors and this was not statistically significant. The mean age was not similar for survivors and non-survivors, the results showed statistically significant difference (p-value ˂0.001) as the higher the age the higher the mortality.There was statistically significant difference between the two groups regarding past medical and drug history (p-value ˂0.001). The mean arterial blood pressure (MAP) showed statistically significant difference between two groups regarding MAP (p-value <0.009) as lower MAP was associated with higher mortality. Temperature and respiratory rate (RR) showed no significant difference between both groups (p-value <0.225 and p-value <0.144 respectively). There was statistically significant difference between the two groups regarding heart rate (HR) (p-value <0.030) as higher HR was associated with higher mortality. There was statistically significant difference between the two groups regarding the APACHE II score as higher score was associated with higher mortality (P-value <0.012). However, there was no statistically significant difference between the two studied groups as regard GCS on admission and RASS of ventilated patients, Also, no statistically significant difference between the two studied groups as regard arterial lactate, CRP but when compared based on procalcitonin there was statistically significant difference. (P-value <0.010). There was a significant association between EEG grading score and 28-day mortality. Comparing between the two studied groups based on EEG grading (Synek scale)
6.1. EEG grading and number of cases accordingly
Grade 0 > 3 / Grade 1 > 20 / Grade 2 > 20 / Grade 3 > 15 / Grade 4 > 11 / Grade 5 > 11
The type of abnormalities was mentioned in synek scale according to grading all cases in grades 4 and 5 suffered seizures.
(P-value <0.001) ().
Table 1. Comparison between survivors and non-survivors regarding baseline characteristics.
There was a significant association between EEG grading score and length of ICU stay (p-value <0.017), the higher the EEG grade the longer the ICU stay.
Also shows that there is a significant association between EEG within 72 hours of admission and Need for mechanical ventilation (p-value <0.001), as the higher EEG score was positively associated with need for mechanical ventilation. There is also a significant association between EEG within 72 hours of admission and Need for vasopressors (p-value <0.001), as the higher EEGgrading the higher the need of vasopressors.
This table shows that: No statistically significant differences were determined with negative correlation between EEG within 72 hours of admission with CPC score in Survivors group after 1 month of ICU admission ().
Table 2. Correlation between EEG grading with length of ICU stay, need for mechanical ventilation, need for vasopressors and CPC score in total patients (n = 80).
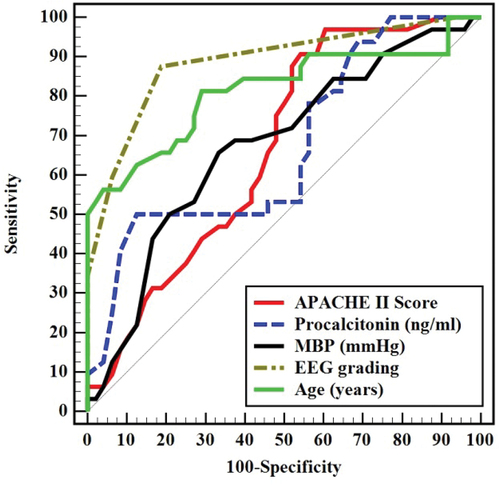
and how that there are multiple parameters that predict 28-day mortality in ICU patients, each of them can be used in predication of mortality by itself. Five univariate parameters affect 28-day mortality with different sensitivity and specificity. From , we figure out that EEG grading has the highest sensitivity and accuracy and procalcitonin has the highest specificity. EEG grading has the highest accuracy compared with the rest of the parameters affecting mortality.
Table 3. Univariate logistic regression analysis for the parameters affecting 28-day mortality (n = 32 vs. 48): (fig.1).
Table 4. Prognostic performance for different parameters to predict 28-day mortality (n = 32 vs. 48).
7. Discussion
Regarding demographic data of the patients, we found statistically significant differences between the two studied groups regarding age, and no statistically significant difference between the two studied groups regarding gender which was similar to the study by Orhun et al. who studied sepsis and acute brain dysfunction [Citation11].
In the current study, statistically significant differences between the two studied groups regarding past medical history and drug history were observed which was similar to the study by Peng et al. who studied prediction of mortality in cases suffering SAE [Citation12].
In the current study, statistically significant differences were demonstrated between the two studied groups regarding MAP and HR which was similar to a study by Peng et al. who studied prediction of mortality in cases suffering SAE [Citation12].
In the current study, statistically significant differences were demonstrated between the two studied groups regarding the APACHE II Score on admission. This comes in correlation with a study by Berisavac et al., who studied APACHE II score as an indicator of mortality [Citation13].
In the current study, statistically significant differences were demonstrated between the two studied groups regarding the Procalcitonin, which was similar to a study by Assicot et al. who studied procalcitonin concentration in patients with sepsis [Citation14].
In the current study, no statistically significant differences were demonstrated between the two studied groups as regard Arterial blood gases. On the contrary, in Peng et al., study revealed statistically significant differences between the two studied groups regarding Arterial blood gases. Cases that died had lower pH, lower bicarbonate, lower PaO2. This may be due to smaller sample size of our study [Citation12].
In the present study, nostatistically significant differences were demonstrated between the two studied groups and GCS on admission and RASS ofventilated patients. In a study by Nguyen et al. and another study by Berisavac et al. both showed significant difference regarding GCS, which may be explained in the studies by larger sample size and no exclusion of normal GCS [Citation13,Citation15].
In the current study, we found that there was statistically significant association between EEG grading within 72 hours of admission and length of ICU stay. Also a study by Chen et al. revealed significant differences in the duration of hospitalization, indicating that encephalopathy caused by sepsis might have a high effect on the long-term outcome [Citation16].
There was statistically significant association between EEG within 72 hours of admission and need for mechanical ventilation,also there was statistically significant association between EEG within 72 hours of admission and need for vasopressors, which comes in parallel with a study by Peng et al. who studied prediction of mortality in cases suffering SAE [Citation12].
In our study there was no statistically significant difference between EEG within the 72 hours and CPC score with negative correlation. Also a study by Urbano V et al. showed similar results [Citation17].
We found that there was a statistically significant association between EEG grading and 28-day mortality. Also Willems LM et al. found that EEG changes was correlating significantly with mortality [Citation18].
Five univariate logistic regression analysis for the parameters affecting 28-day Mortality was done and performance for different parameters to predict 28-day Mortality.
We figured out that EEG grading has the highest sensitivity and accuracy in comparison with the rest of the parameters affecting mortality and procalcitonin has the highest specificity. Also a study by Saito et al. showed similar results [Citation19].
8. Limitation of our study
The shortcomings of the present study are:
❑ Conducting EEG in the first 72 hours of ICU admission (only one time).
❑ conducting the study on critical patients in one center (AMUH).
❑ Larger number of patients for a longer period are required and correlating themwith the outcome.
9. Conclusion
High APACHE II score, procalcitonin, age and lower MAP were associated with higher mortality in patients with sepsis or septic shock presenting with SAE.
EEG changes (higher EEG grading) were associated with higher 28- day mortality
EEG grading has the highest sensitivity and accuracy and procalcitonin has the highest specificity to predict 28-day mortality
Availability of data and materials
All data generated or analyzed during the current study are included in this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Tamer A. Helmy
Prof. dr Tamer A. Helmy Professor of critical care department alexandria university.
Amr H. Dahroug
Ass. prof. dr Amr H. Dahroug Assistant professor of critical care department alexandria university.
Ahmed Taha
Dr. Ahmed Taha Lecturer of critical care department alexandria university.
Abdelrahman E. Soudy
Dr Abdelrahman E. soudy Specialist of critical care department alexandria university.
References
- Cecconi M, Evans L, Levy M, et al. Sepsis and septic shock. Lancet. 2018 Jul;392(10141):75–87.
- Tauber SC, Djukic M, Gossner J, et al. Sepsis-associated encephalopathy and septic encephalitis: an update. Exp Rev Anti-Infective Ther. 2020 Sep 14;19(2):215–231.
- Chen J, Shi X, Diao M, et al. A retrospective study of sepsis-associated encephalopathy: epidemiology, clinical features and adverse outcomes. BMC Emerg Med Internet. 2020 Oct 6;20(1):77. [cited 2022 Dec 4]. doi: 10.1186/s12873-020-00374-3
- Rubinos C, Alkhachroum A, Der-Nigoghossian C, et al. Electroencephalogram monitoring in critical care. Semin Neurol. 2020 Nov 11;40(6):675–680. doi: 10.1055/s-0040-1719073
- Young GB, McLachlan RS, Kreeft JH, et al. An electroencephalographic classification for coma. Can J Neurol Sci. 1997;24(4):320–5. doi: 10.1017/S0317167100032996
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–247. doi: 10.1007/s00134-021-06506-y
- Akavipat P. Acute physiology and chronic health evaluation (APACHE) II score – the clinical predictor in neurosurgical intensive care unit. ACC. 2019. doi: 10.20471/acc.2019.58.01.07
- Babiloni C, Barry RJ, Başar E, et al. International Federation of Clinical Neurophysiology (IFCN) – EEG research workgroup: recommendations on frequency and topographic analysis of resting state EEG rhythms. Part 1: applications in clinical research studies. Clin Neurophysiol. 2020 Jan;131(1):285–307.
- Tatum WO, Selioutski O, Ochoa JG, et al. American clinical neurophysiology society guideline 7: guidelines for EEG reporting. Neurodiagn J Internet. 2016;56(4):285–293. [cited 2019 Dec 24]. doi: 10.1080/21646821.2016.1245576
- Benghanem S, Paul M, Charpentier J, et al. Value of EEG reactivity for prediction of neurologic outcome after cardiac arrest: insights from the parisian registry. Resuscitation. 2019;142:168–74. doi: 10.1016/j.resuscitation.2019.06.009
- Orhun G, Esen F, Özcan PE, et al. Neuroimaging findings in sepsis-induced brain dysfunction: association with clinical and laboratory findings. Neurocrit Care Internet. 2019 Feb 1;30(1):106–117. doi:10.1007/s12028-018-0581-1.
- Peng L, Peng C, Yang F, et al. Machine learning approach for the prediction of 30-day mortality in patients with sepsis-associated encephalopathy. BMC Med Res Methodol. 2022 Jul 4;22(1). doi: 10.1186/s12874-022-01664-z
- Berisavac II, Padjen VV, Ercegovac MD, et al. Focal epileptic seizures, electroencephalography and outcome of sepsis associated encephalopathy-A pilot study. Clin Neurol Neurosur. 2016;148:60–66. doi: 10.1016/j.clineuro.2016.06.013
- Assicot M, Gendrel D, Carsin H, et al. High serum procalcitonin concentration in patients with sepsis and infection. Lancet. 1993;341(8844):515–518. doi: 10.1016/0140-6736(93)90277-N
- Nguyen DN, Huyghens L, Zhang H, et al. Cortisol is an associated-risk factor of brain dysfunction in patients with severe sepsis and septic shock. Bio Med Res Int. 2014;2014:1–7. doi: 10.1155/2014/712742
- Yuan J, Zhang Y, Zhou L, et al. Single-junction organic solar cell with over 15% efficiency using fused-ring acceptor with electron-deficient core. Joule. 2019;3(4):1140–1151. doi: 10.1016/j.joule.2019.01.004
- Urbano V, Novy J, Alvarez V, et al. EEG recording latency in critically ill patients: impact on outcome. An analysis of a randomized controlled trial (CRETA). Clin Neurophysiol. 2022 Jul;139:23–27. doi: 10.1016/j.clinph.2022.04.003
- Willems LM, Trienekens F, Knake S, et al. EEG patterns and their correlations with short-and long –termmortality in patients with hypoxic encephalopathy. Clinical Neuropysiolo. 2021 Nov;132(11):2851–2860.
- Saito T, Malicoat JR, Leyden LR, et al. Mortality prediction by bispectral electroencephalography among 502 patients: its role in dementia. Brain Comm. 2021;3(2). doi: 10.1093/braincomms/fcab037