ABSTRACT
Objective: To address the question of whether antibiotic therapy can obviate the need for prostate biopsy (PBx) in patients presenting with high prostate-specific antigen (PSA) levels.
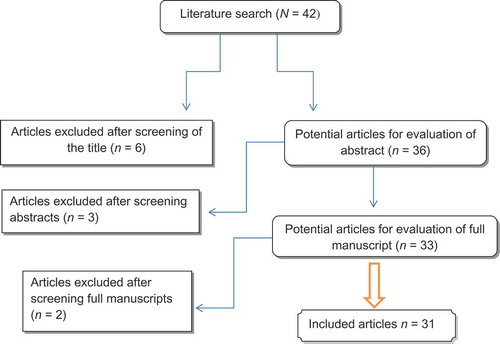
Methods: With the increase in unnecessary PBx in men with high PSA levels, a systematic review was performed according to the Cochrane Reviews guidelines and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.
Results: The literature search yielded 42 studies, of which 11 were excluded due to irrelevance of data. Most of the studies were retrospective, nine studies were randomised controlled trials, and there were seven prospective non-randomised trials. The age range of the patients was 51–95 years. Antibiotics, predominantly ofloxacin or ciprofloxacin, combined with a non-steroidal anti-inflammatory drug (NSAID) or not, were prescribed for 2–8 weeks. All studies focussed on PSA levels ranging from ≤ 4 to ≥ 10 ng/mL. Furthermore, antibiotic therapy normalised PSA levels by a wide variety of percentages (16–59%), and the PSA level decrease also varied widely and ranged from 17% to 80%. For patients who had unchanged or decreased PSA, carcinoma was found in 40–52% and 7.7–20.3%, respectively. No cancer was detected if the PSA level decreased to < 4 ng/mL.
Conclusion: Antibiotic therapy is clinically beneficial in patients with high PSA levels. PSA reduction or normalisation after medical therapy, either antibiotic and/or NSAID, for ≥ 2 weeks can avoid unnecessary PBx. Antibiotic therapy is more beneficial when the PSA level is < 20 ng/mL.
Abbreviations: EPS: expressed prostatic secretion; PBx: prostate biopsy; (%f)(f/t)(t)PSA, (percentage free) (free/total) (total) serum PSA; PSAD: PSA density; RCT: randomised controlled trial; VB3: voided bladder urine 3
Introduction
In daily practice, some urologists often prescribe antibiotics before prostate biopsy (PBx) to men with a newly increased PSA to decrease inflammation-induced PSA elevation and help to reduce unnecessary PBx. However, others have reported that antibiotic treatment has no significant effect on the PSA level and that a lowered level of PSA after antibiotic treatment does not mean a decreased risk of prostate cancer [Citation1].
PBx is a potentially morbid procedure. Prostatitis is commonly reported on needle biopsies and 65–70% of patients with abnormal PSA levels do not have cancer on prostate needle biopsy. After a 2-year clinical and biochemical follow-up of symptomatic men who had a high PSA level and a normal DRE, and normal repeat PSA level, PBx can be safely avoided [Citation2].
In the present review we aimed to address the controversy of whether antibiotic treatment can exclude inflammation in the differential diagnosis of PSA elevation and thus can avoid unnecessary PBx. We considered patients with LUTS, normal DRE and normal urine analysis, and elevated PSA levels.
Methods
Search strategy and study selection
The systematic review was performed according to the Cochrane Reviews guidelines and in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [Citation3].
The search strategy was conducted to find relevant studies from the Medical Literature Analysis and Retrieval System Online (MEDLINE; 1966–2018), Excerpta Medica dataBASE (EMBASE; 1980–2018), Google Scholar, and individual urological journals. The search was conducted in January 2018.
Terms used included: ‘prostate’, ‘biopsy’, ‘high PSA’, and ‘antibiotic therapy’.
Mesh phrases included:
(‘high PSA’[Mesh]) AND ‘unnecessary prostate biopsy’[Mesh])
((‘high PSA’[Mesh]) AND ‘antibiotic therapy’[Mesh]) AND ‘unnecessary prostate biopsy’[Mesh])
(((‘high PSA’[Mesh]) AND ‘antibiotic therapy’[Mesh]) AND ‘ unnecessary prostate biopsy’[Mesh]) AND ‘NSAID’[Mesh])
All language papers were considered if reporting on PSA reduction after antibiotic therapy. References of searched papers were evaluated for potential inclusion. Authors of the included studies were contacted whenever the data were not available or not clear.
Inclusion criteria
All studies reporting on antibiotic therapy in patients with high PSA levels.
Studies published in the English language over the period 1980–2018.
Exclusion criteria
Animal studies and case reports.
Studies on patients with high PSA levels without documented antibiotic therapy.
Two reviewers (D.T. and O.M.A.) identified all studies that adhered to the inclusion criteria for full review. Each reviewer independently selected studies for inclusion. Disagreement between the extracting authors was resolved by consensus or referred to a third author (A.A.S.).
Data extraction and analysis
The objectives were to evaluate the efficacy and safety of using antibiotic therapy in PSA reduction resulting in the avoidance of unnecessary PBx. The variables extracted from each study were: patient demographics, antibiotic type, antibiotic duration, NSAID use with antibiotic or not, PSA reduction level after antibiotic therapy, and rate of PBx after antibiotic therapy.
Results
The literature search yielded 42 studies, of which 11 were excluded due to irrelevance of data (). The majority of studies were retrospective and nine studies were randomised controlled trials (RCTs) [Citation4–Citation12]. Furthermore, there were seven prospective non-randomised trials [Citation13–Citation19]. All studies reported on the variables indicated in the data extraction section and are listed in [Citation4–Citation32, Citation34, Citation35].
Table 1. The detailed features of the studies included in the review.
Characteristics of the included studies
The 31 included studies were published between 1995 and 2018, and included 4682 patients with an age range between 51 and 95 years.
The type and duration of antibiotic use
Concerning the duration of antibiotic use, some studies prescribed antibiotics for 2–4 weeks [Citation8–Citation28], whilst others prescribed for 6–8 weeks [Citation4,Citation7,Citation28–Citation30].
Six studies used ofloxacin [Citation4,Citation8,Citation10,Citation13,Citation15,Citation16], six studies used 500 mg ciprofloxacin [Citation5,Citation9,Citation17,Citation19,Citation21,Citation23], and five used levofloxacin [Citation6,Citation9,Citation12,Citation28]. Six studies combined the antibiotic therapy with NSAIDs [Citation4,Citation5,Citation18,Citation20,Citation23,Citation25]. Huang et al. [Citation21] added the plant extracts, Ningbitai and Yunnan Baiyao capsule, to the antibiotic therapy. Magri et al. [Citation29] combined 500 mg/day ciprofloxacin and 500 mg/day azithromycin.
Effect of antibiotic use
There was no significant difference in the mean change in PSA level between the levofloxacin and ciprofloxacin groups [Citation9].
Shtricker et al. [Citation10] compared 135 patients who received antibiotics (65) with those who did not (70). The PSA levels decreased by 60% in both groups and at PBx prostate cancer was found in 25% of patients in both groups. In both groups, 40% of the patients had no decrease in PSA levels; however, prostate cancer was found in only two patients (12%) who received antibiotics, and in eight (42%) who did not receive antibiotic. PSA levels tend to fall when measurement is repeated after 45 days, regardless of antibiotic use [Citation6].
In the Lee et al. [Citation7] study of 413 patients, 215 (52%) patients had positive findings on expressed prostatic secretion (EPS) or voided bladder urine 3 (VB3) tests. After 8 weeks of quinolone antibiotic therapy, 53 of these 215 men avoided PBx due to of normalisation of their PSA levels.
No effect of antibiotic on PSA level
Inflammation had no significant influence on total serum PSA (tPSA) level or the percentage free PSA (%fPSA) [Citation26]. The tPSA, %fPSA, and free/total PSA ratio (f/tPSA) alterations before and after antibiotic therapy did not show any statistically significant difference (P > 0.05) [Citation22]. There is no advantage in administering antibacterial therapy with initial PSA levels of 4–10 ng/mL, without overt evidence of inflammation [Citation10].
The studied level of PSA
All studies focussed on PSA levels ranging from 4 to 10 ng/mL. Some studies assessed PSA levels <4 ng/mL [Citation6,Citation18] and others assessed levels >10 ng/mL [Citation9,Citation16,Citation19,Citation21].
The majority of studies addressed the effect of antibiotics on the acutely inflamed prostate, whilst some of the other studies reported on documented chronic inflamed type [Citation4,Citation7,Citation9,Citation18,Citation20,Citation21,Citation25,Citation29].
Morote et al. [Citation26] assessed benign tissue without inflammation in association with chronic prostatitis or acute prostatitis, whilst other studies focussed on patients presenting with LUTs only with normal urine analysis [Citation6,Citation13,Citation19,Citation23,Citation24,Citation27,Citation31,Citation32].
Three studies did not use antibiotics but assessed the degree of inflammation after prostatectomy [Citation33–Citation35].
The degree of PSA decline
The PSA level was normalised by a wide variety of percentages and varied across the studies from 16% to 59% [Citation7,Citation8,Citation20,Citation25,Citation29,Citation30]. The PSA level decrease also varied widely and ranged from 17% to 80% [Citation4,Citation13,Citation15,Citation18,Citation20,Citation23,Citation24,Citation29,Citation32].
In the Dirim et al. [Citation28] study, PSA levels decreased after antibiotic treatment in 47 of 85 patients. The f/tPSA ratio decreased or remained unchanged in 21 of these 47 cases and increased in 26. There were 38 patients who had increased PSA levels after antibiotic therapy. The f/tPSA ratios decreased or remained unchanged in 20 of these 38 cases and increased in 18. In the Toktas et al. [Citation12] study, there were significant changes in the values of PSA and its derivatives in the antibiotic treatment group, from 5.31 to 4.69 and 4.58 ng/mL, consecutively. In the Kyung et al. [Citation30] study, the PSA density (PSAD) after antibiotic treatment was normalised (< 0.15 ng/mL/mL) in 23 of the 40 patients with a high PSAD before treatment.
Significantly, the mean (range) PSA level decreased by 33.8% from 8.12 (4.02–24.8) to 5.37 (1.35–12.94) ng/mL after treatment (P = 0.001) [Citation18], and by 36.4% from 8.48 ng/mL before to 5.39 ng/mL after treatment (P < 0.001) [Citation25]. Similarly, in the Wang et al. [Citation20] study, the mean PSA decreased from 6.24 ng/mL before treatment to 4.58 ng/mL 4 weeks after treatment (P < 0.05). In the Toktas et al. [Citation12] study, there were significant changes in the values of PSA and its derivatives in the treatment group (from 5.31 to 4.69 and 4.58 ng/mL, consecutively).
Rate of carcinoma and pbx avoidance
As regard patients who had unchanged or decreased PSA levels, carcinoma was found in 40–52% and 7.7–20.3%, respectively. No cancer was detected if the PSA level decreased to < 4 ng/mL or by > 70% [Citation10,Citation17,Citation27,Citation28]. However, the possibility of prostate cancer in patients with a PSA level of < 2.5 ng/mL is still present [Citation18].
Pathological studies of PBxs after antibiotic therapy revealed prostate cancer in 20.9–25.5%, chronic inflammation in 50.7–74.4%, and BPH in 4.7–21.8% [Citation4,Citation18,Citation25].
With regard to PSA levels, Azab et al. [Citation4] reported that of their 142 patients treated with antibiotic and NSAIDs for 6 weeks, prostate cancer was detected in 12% (three of 25 patients) with PSA levels of < 2.5 ng/mL, 12.7% (six of 47 patients) with PSA levels of ≥ 2.5–< 4.0 ng/mL, and in 30% (21/70 patients) with PSA levels ≥ 4.0 ng/mL.
Shtricker et al. [Citation10] studied the cancer detection rate in patients with PSA levels of 4–10 ng/mL, who received antibiotic therapy (65 patients) vs those who did not (70 patients). The cancer detection rate at PBx in patients who did not have a PSA level decrease was 12% (two of 17 patients) after antibiotic therapy vs 42% (eight of 19 patients) in those no antibiotic therapy [Citation10]. Similarly, Kaygisiz et al. [Citation27] reported that prostate cancer was found at PBx in 10.8% of the patients with PSA levels between 4 and 10 ng/mL, but in none with PSA levels <4 ng/mL.
In the Yoo et al. [Citation32] study, PBx was performed in 50 of 237 patients (21.1%), and only a single case (2%) of prostate cancer was diagnosed. In the Baltaci et al. [Citation13] study, in 17% of the men the tPSA after treatment was < 4 ng/mL and of these five (29.4%) had prostate cancer at PBx.
In the Lee et al. [Citation7] study, the total prostate cancer detection rate was 20.7% in the patients with negative findings on EPS or VB3 tests and 3.3% in the patients with positive findings.
Discussion
Although there is controversy surrounding the value of antibiotics in reducing higher PSA levels, some urologists in daily practice often prescribe antibiotics before PBx to men with a newly increased PSA level. PSA level reduction after antibiotics might identify those patients in whom PBx can be avoided.
Some researchers have found that antibiotic treatment can decrease inflammation-induced PSA elevation and help to reduce unnecessary PBx. Conversely, others have reported that antibiotic treatment has no significant effect on the PSA level, and a lowered PSA level after antibiotic treatment does not mean a decreased risk of prostate cancer [Citation1].
The antibiotic can be prescribed for 2–4 weeks [Citation8–Citation28] or 6–8 weeks [Citation4,Citation7,Citation28–Citation30]. The type of antibiotic used is based on local sensitivities and quinolones are the most frequently used type.
The evidence for inflammation should be addressed before trying antibiotic therapy in patients with high PSA levels. The proof of inflammation can be delineated via EPS [Citation7], symptoms of acute or chronic prostatitis [Citation4,Citation7,Citation9,Citation18,Citation20,Citation21,Citation25,Citation29], and detection of the degree of inflammation after prostatectomy [Citation33,Citation34].
The PSA level in focus for antibiotic therapy ranges from 4 to 10 ng/mL. Some studies assessed PSA levels <4 ng/mL [Citation6,Citation18], whilst others assessed levels >10 ng/mL [Citation9,Citation16,Citation19,Citation21]. In patients with PSA levels higher than the threshold value, definitive treatment should be not postponed for preliminary antibiotic therapy.
After use of antibiotic therapy, the PSA level was normalised by a wide variety of percentages, ranging from 16% to 59% [Citation6–Citation8,Citation10,Citation20,Citation25,Citation29,Citation30]. Furthermore, the range of the PSA level decrease was 17–80% [Citation4,Citation13,Citation15,Citation18,Citation20,Citation23,Citation29,Citation32], or a > 20% decrease from baseline [Citation24].
The f/tPSA ratio rather than tPSA appears to be more helpful in suggesting prostate cancer in cases receiving antibiotic therapy for high PSA levels [Citation12,Citation28,Citation30].
PBx should be considered without trying antibiotic therapy in patients with high PSA values, if a suspicion of prostatitis does not exist [Citation22].
The rate of cancer detection after receiving antibiotic therapy varied from 2% to 29% [Citation4,Citation6,Citation7,Citation10–Citation13,Citation17,Citation18,Citation25,Citation27–Citation29,Citation32].
Carcinoma was found in 40–52% of patients who did not have a PSA decrease. Conversely, a detection rate of 7.7–20.3% was found in patients who had a PSA decrease in comparison with the pre-treatment values [Citation10,Citation17,Citation27,Citation28].
In the context of pathological results after antibiotic therapy, prostate cancer was evident in only 20.9–25.5%, whilst chronic inflammation and BPH was found in 50.7–74.4% and 4.7–21.8%, respectively [Citation4,Citation18,Citation25].
For specific PSA values, prostate cancer was identified in 12% (three of 25 patients) with PSA levels of < 2.5 ng/mL, 12.7% (six of 47 patients) with PSA levels of ≥ 2.5–< 4.0 ng/mL, and in 30% (21/70 patients) with PSA levels ≥ 4.0 ng/mL [Citation4]. While, the cancer detection rate in patients having a PSA level between 4–10 ng/mL was 10.8–12% [Citation10,Citation27].
Conclusion
Antibiotic therapy is clinically beneficial in patients with high PSA levels. PSA reduction or normalisation after medical therapy, either antibiotic and/or NSAID, for ≥2 weeks can avoid unnecessary PBx. Antibiotic therapy is more beneficial when the PSA level is <20 ng/mL, especially when the evidence for inflammation is not overt.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Liu J, Hu WL. [Can antibiotic treatment exclude inflammation in the differential diagnosis of elevated PSA?] [Article in Chinese]. Zhonghua Nan Ke Xue. 2012;18:747–750.
- Singh R, Cahill D, Popert R, et al. Repeating the measurement of prostate-specific antigen in symptomatic men can avoid unnecessary prostatic biopsy. BJU Int. 2003;92:932–935.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
- Azab S, Osama A, Rafaat M. Does normalizing PSA after successful treatment of chronic prostatitis with high PSA value exclude prostatic biopsy? Transl Androl Urol. 2012;1:148–152.
- Erol H, Beder N, Calişkan T, et al. Can the effect of antibiotherapy and anti-inflammatory therapy on serum PSA levels discriminate between benign and malign prostatic pathologies? Urol Int. 2006;76:20–26.
- Heldwein FL, Teloken PE, Hartmann AA, et al. Antibiotics and observation have a similar impact on asymptomatic patients with a raised PSA. BJU Int. 2011;107:1576–1581.
- Lee AG, Choi YH, Cho SY, et al. A prospective study of reducing unnecessary prostate biopsy in patients with high serum prostate-specific antigen with consideration of prostatic inflammation. Korean J Urol. 2012;53:50–53.
- Saribacak A, Yilmaz H, Ciftci S, et al. The role of empiric antibiotic treatment in preventing unnecessary prostate biopsies in asymptomatic patients with PSA levels between 4 and 10 ng/ml. Int J Clin Exp Med. 2014;7:2230–2235.
- Schaeffer AJ, Wu SC, Tennenberg AM, et al. Treatment of chronic bacterial prostatitis with levofloxacin and ciprofloxacin lowers serum prostate specific antigen. J Urol. 2005;174:161–164.
- Shtricker A, Shefi S, Ringel A, et al. PSA levels of 4.0–10 ng/mL and negative digital rectal examination. Antibiotic therapy versus immediate prostate biopsy. Int Braz J Urol. 2009;35:551–558.
- Stopiglia RM, Ferreira U, Silva MM Jr, et al. Prostate specific antigen decrease and prostate cancer diagnosis: antibiotic versus placebo prospective randomized clinical trial. J Urol. 2010;183:940–944.
- Toktas G, Demiray M, Erkan E, et al. The effect of antibiotherapy on prostate-specific antigen levels and prostate biopsy results in patients with levels 2.5 to 10 ng/mL. J Endourol. 2013;27:1061–1067.
- Baltaci S, Süer E, Haliloğlu AH, et al. Effectiveness of antibiotics given to asymptomatic men for an increased prostate specific antigen. J Urol. 2009;181:128–132.
- Busato WF, Almeida GL, Geraldo J, et al. Does PSA reduction after antibiotic therapy permits postpone prostate biopsy in asymptomatic men with PSA levels between 4 and 10 ng/mL? Int Braz J Urol. 2015;41:329–336.
- Karazanashvili G, Managadze L. Prostate-specific antigen (PSA) value change after antibacterial therapy of prostate inflammation, as a diagnostic method for prostate cancer screening in cases of PSA value within 4–10 ng/ml and nonsuspicious results of digital rectal examination. Eur Urol. 2001;39:538–543.
- Lorente JA, Arango O, Bielsa O, et al. Effect of antibiotic treatment on serum PSA and percent free PSA levels in patients with biochemical criteria for prostate biopsy and previous lower urinary tract infections. Int J Biol Markers. 2002;17:84–89.
- Serretta V, Catanese A, Daricello G, et al. PSA reduction (after antibiotics) permits to avoid or postpone prostate biopsy in selected patients. Prostate Cancer Prostatic Dis. 2008;11:148–152.
- Kim YJ, Kim SO, Ryu KH, et al. Prostate cancer can be detected even in patients with decreased PSA less than 2.5 ng/ml after treatment of chronic prostatitis. Korean J Urol. 2011;52:457–460.
- Bulbul MA, Wazzan W, Hijaz A, et al. The effect of antibiotics on elevated serum prostate specific antigen in patients with urinary symptoms and negative digital rectal examination: a pilot study. J Med Liban. 2002;50:23–25.
- Wang W, Hu WL, Yang H, et al. [Effects of antibiotic and anti-inflammatory treatment on serum PSA and free PSA levels in patients with chronic prostatitis IIIA] [Article in Chinese]. Zhonghua Nan Ke Xue. 2006;12:787–790.
- Huang BX, Su HC, Sun FK. [Compound ciprofloxacin suppository combined with ningbitai and yunnan baiyao for histological prostatitis with PSA elevation] [Article in Chinese]. Zhonghua Nan Ke Xue. 2012;18:986–990.
- Faydaci G, Eryildirim B, Tarhan F, et al. [Does antibiotherapy prevent unnecessary prostate biopsies in patients with high PSA values?] [Article in Spanish]. Actas Urol Esp. 2012;36:234–238.
- Del Rosso A, Saldutto P, Di Pierro ED, et al. [Impacts of antibiotic and anti-inflammatory therapy on serum prostate specific antigen in asymptomatic men: our experience] [Article in Italian]. Urologia. 2012;79(Suppl. 19):37–40.
- Kobayashi M, Nukui A, Morita T. Serum PSA and percent free PSA value changes after antibiotic treatment. A diagnostic method in prostate cancer suspects with asymptomatic prostatitis. Urol Int. 2008;80:186–192.
- Bozeman CB, Carver BS, Eastham JA, et al. Treatment of chronic prostatitis lowers serum prostate specific antigen. J Urol. 2002;167:1723–1726.
- Morote J, Lopez M, Encabo G, et al. Effect of inflammation and benign prostatic enlargement on total and percent free serum prostatic specific antigen. Eur Urol. 2000;37:537–540.
- Kaygisiz O, Uğurlu O, Koşan M, et al. Effects of antibacterial therapy on PSA change in the presence and absence of prostatic inflammation in patients with PSA levels between 4 and 10 ng/ml. Prostate Cancer Prostatic Dis. 2006;9:235–238.
- Dirim A, Tekin MI, Koyluoglu E, et al. Do changes in a high serum prostate-specific antigen level and the free/total prostate-specific antigen ratio after antibiotic treatment rule out biopsy and the suspicion of cancer? Urol Int. 2009;82:266–269.
- Magri V, Trinchieri A, Montanari E, et al. Reduction of PSA values by combination pharmacological therapy in patients with chronic prostatitis: implications for prostate cancer detection. Arch Ital Urol Androl. 2007;79:84–92.
- Kyung YS, Lee HC, Kim HJ. Changes in serum prostate-specific antigen after treatment with antibiotics in patients with lower urinary tract symptoms/benign prostatic hyperplasia with prostatitis. Int Neurourol J. 2010;14:100–104.
- Nadler RB, Humphrey PA, Smith DS, et al. Effect of inflammation and benign prostatic hyperplasia on elevated serum prostate specific antigen levels. J Urol. 1995;154:407–413.
- Yoo DS, Woo SH, Cho S, et al. Practice patterns of urologists in managing Korean men aged 40 years or younger with high serum prostate-specific antigen levels. Urology. 2014;83:1339–1343.
- Ozden C, Ozdal OL, Guzel O, et al. The correlation between serum prostate specific antigen levels and asymptomatic inflammatory prostatitis. Int Urol Nephrol. 2007;39:859–863.
- Yaman O, Göğüş C, Tulunay O, et al. Increased prostate-specific antigen in subclinical prostatitis: the role of aggressiveness and extension of inflammation. Urol Int. 2003;71:160–164.
- Irani J, Levillain P, Goujon JM, et al. Inflammation in benign prostatic hyperplasia: correlation with prostate specific antigen value. J Urol. 1997;157:1301–1303.