ABSTRACT
To analyse the current therapeutic options for patients with premature ejaculation (PE) and highlight their mechanism(s) of action, effectiveness, advantages and limitations. A literature search was conducted using the PubMed database searching for articles exploring different PE treatment modalities. A Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) approach was used to report the results of the literature search. A total of 149 articles were included in this review. The currently available treatment methods for PE include behavioural therapy, local anaesthetics, tricyclic antidepressants, selective serotonin reuptake inhibitors, and selective phosphodiesterase inhibitors. Most PE treatments are either experimental or used off-label. New treatments are certainly warranted to overcome this exasperating sexual dysfunction.
Abbreviations: AIPE: Arabic Index of Premature Ejaculation; CNS: central nervous system; CYP: cytochrome P450; ED: erectile dysfunction; FDA: United States Food and Drug Administration; H1: histamine receptors; 5-HT: 5-hydroxytryptamine; IELT: The intravaginal ejaculation latency time; IPE: Index of Premature Ejaculation; M1: muscarinic receptors; OCD: obsessive–compulsive disorder; PDE5: phosphodiesterase type 5; PE: premature ejaculation; PEP: Premature Ejaculation Profile; PRO: patient-reported outcome; RCT: randomised controlled trial; SS: Severance Secret (cream); SSRIs: selective serotonin reuptake inhibitors; TCAs: tricyclic antidepressants
Introduction
Premature ejaculation (PE) is perhaps the most common sexual dysfunction amongst men. The prevalence rate of PE is variable, but it is believed that one out of three men may complain of this sexual dysfunction at some point during their lives [Citation1]. This disease entity has suffered from significant ambiguities in the past with respect to its definition and pathophysiology, and it was not until 2014 when the first standardised evidence-based definition of PE was established [Citation2].
The evaluation of patients presenting with PE is initiated with a complete medical history looking for comorbidities that would make them prone to this clinical condition or would rather alter the offered treatment options (e.g. endocrine, urological, or psychorelational/psychosexual) [Citation3,Citation4] (). A detailed sexual history is obviously relevant to assess the frequency and nature of sexual encounters and to identify sexual comorbidities (e.g. erectile dysfunction [ED]) that would render PE simple (occurring in the absence of other sexual dysfunctions) or complicated (occurring in the presence of other sexual dysfunctions) [Citation3]. The International Society for Sexual Medicine (ISSM) guidelines on PE recommends asking patients with such a presentation about the time between penetration and ejaculation (‘cumming’), their ability to delay ejaculation and the impact of such condition on their psychological wellbeing [Citation5].
Table 1. The key steps for evaluation of patients with PE
It is also imperative to classify PE based on its onset into either lifelong or acquired PE and to assess the severity of the symptoms. Involving the partner during the initial and subsequent interviews is preferred to determine their view of the situation and the impact of PE and its treatment outcome on the couple as a whole. A genital examination is also recommended to evaluate the phallus and scrotal contents.
In addition, assessment of patients with PE includes the use of validated questionnaires and patient-reported outcome (PRO) measures (the ability to have control over ejaculation and the extent of patient and partner sexual satisfaction) in addition to stopwatch measures of ejaculatory latency. Stopwatch measures of intravaginal ejaculatory latency time (IELT) were widely used in clinical trials and observational studies of PE, but have not been recommended for use in routine clinical management of PE [Citation6]. Despite the potential advantage of objective measurement, stopwatch measures have the disadvantage of being intrusive and potentially disruptive of sexual pleasure or spontaneity.
Five validated questionnaires have been developed and published to date. Two measures (Index of Premature Ejaculation [IPE] and Premature Ejaculation Profile [PEP]) have extensive databases. One measure (PE Diagnostic Tool) has a modest database. Two other measures (Arabic and Chinese PE Questionnaires) have few clinical trial data available [Citation6].
Currently, no therapy is approved by the United States Food and Drug Administration (FDA) for treatment of PE [Citation7–9]. However, several therapies for PE are marketed and used in many countries. Treatment modalities as recommended by the British Association of Sexual Health and HIV include behavioural therapy, tricyclic antidepressants (TCAs), selective serotonin reuptake inhibitors (SSRIs), local anaesthetic agents, and phosphodiesterase type 5 (PDE5) inhibitors [Citation10] (). Numerous studies have shown that SSRIs and drugs with SSRI-like side-effects are safe and effective in the treatment of PE [Citation11]. The aim of the present review was to explore the various therapeutic options available for PE and highlight their mechanism(s) of action, effectiveness, advantages, and limitations.
Table 2. The currently available treatment methods for PE
Methods
Search strategy
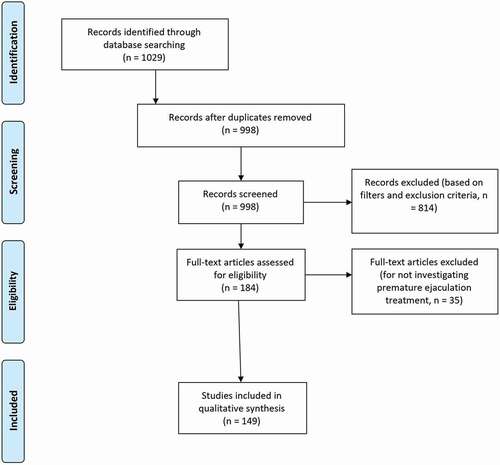
This review was conducted according to Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) criteria. The PubMed database was searched using the key words ((‘premature ejaculation’)) AND ((‘treatment’ OR ‘management’)) from the time of its initiation until 10 January 2021. The following filters were applied to the searched results: (1) Humans, (2) English, (3) Male, and (4) Adults (aged >18 years). Screening of the searched articles’ titles, abstracts and main text was performed successively. Reviews, commentaries, editorials, abstracts, and case reports were excluded from this review. Articles not specifically designed to investigate a PE treatment modality were also excluded; these constituted studies exploring PE aetiology, epidemiology, pathophysiology, psychological impact etc. Relevant articles were selected for inclusion in the discussion of various PE treatment modalities in this review ().
Results
A total of 1029 articles were initially retrieved with the literature search, and 814 articles were excluded after removing duplicates and applying the search filters and exclusion criteria. Additionally, 35 articles did not meet the main objective of the search and were excluded leaving 149 studies that were included in the discussion of this manuscript.
Discussion
Various treatment methods for PE have been described and include the following ().
Behavioural therapy
The two most frequently used techniques in behavioural therapy are the ‘stop-and-start’ technique described by Semans in 1956 [Citation12], and the ‘squeeze’ method developed by Masters and Johnson in 1970 [Citation13]. These techniques were proven to be effective in most cases. However, couples can be averse to using them, with some women reluctant to squeeze their partner’s penis and some couples unwilling to interrupt sexual interaction once initiated [Citation14]. These techniques focus on distraction and reduction of sexual excitement or stimulation, which may reduce overall sexual satisfaction.
1. Squeeze technique
The man relaxes on his back and the wife starts to stimulate his penis. When the man indicates high arousal and orgasm is about to occur, the woman stops stimulation and applies a firm squeeze to the head of the penis for 5–10 s with the thumb on the frenulum and the index and middle fingers just above the coronal ridge on opposite side until the man feels that the ejaculation reflex is inhibited. The female repeats the technique again two or three times and then the man proceeds to ejaculation. After several times of this practice, the male will be more able to control his ejaculation and gains confidence.
The couple is instructed to start with the ‘woman-on-top’ position of intercourse. The man lies on his back and the wife sits on top of him. Once he has a firm erection, he inserts his penis into her vagina, with his hands on her thighs to guide her movement. He asks her to stop moving once ejaculation is about to occur. She can start moving when the man’s arousal subsides a little and so on.
The aim is to tolerate penetration without ejaculation for ~15 min. If the man is initially unable to do so, he should not worry; he just needs to repeat the exercise as often as he needs. Once he can control his ejaculation, the couple can make love in any position they like [Citation13].
2. Start/stop technique
This technique is more preferable and similar to the above one except that the female stops stimulation only and does not apply squeeze to the glans penis when the orgasm is about to occur. When the male assumes control with the hand of his partner, intercourse can be done, with the female on top, then lateral, and finally male on top position. At all times coitus is stopped near orgasm until control is possible [Citation12].
The goals of traditional psychotherapy/behavioural interventions
Psychotherapy/behavioural interventions improve ejaculatory control by helping men/couples to: (1) learn techniques to control and/or delay ejaculation, (2) gain confidence in their sexual performance, (3) lessen performance anxiety, (4) modify rigid sexual repertoires, (5) surmount barriers to intimacy, (6) resolve interpersonal issues that precipitate and maintain the dysfunction, (7) come to terms with feelings/thoughts that interfere with sexual function, and (8) increase communication [Citation15–17].
The effectiveness of the start/stop and squeeze techniques
Masters and Johnson [Citation13] reported success rate of up to 98% of men with PE treated with the start/stop and squeeze techniques at a 5-years follow-up. This has often, erroneously, been translated into a success rate. It has been reported that only 64% of patients successfully gained ejaculatory control using the squeeze technique, and only one-third showed continued control for 3 years after treatment [Citation18]. It was also found that men treated for PE using the same techniques experienced significant immediate benefits [Citation19]. However, these gains were not sustained when measured at a follow-up visit 3 years later.
As it is not entirely clear why the intervention works in the first place, it is difficult to identify why the treatment gains were lost over time. Decrease in motivation, additional sexual problems occurring in the relationship, and changes in attraction between partners, could all play a role in the loss of gained ejaculatory control. Although, squeeze and start/stop techniques, have been the mainstay of PE management for many years, evidence of their short-term efficacy and long-term benefit is lacking [Citation20].
Pharmacological interventions () [24,26,27,32,47,48,50–52,55–59,66,67,72,73,76–79,81,84–87,89,90,116,151–163]
Table 3. Studies investigating various antidepressants for the treatment of PE
1. Tricyclic antidepressants (TCAs)
All TCAs have a three-ring nucleus in their molecular structures [Citation21]. TCAs, and their derivatives, have been a cornerstone in medical treatment of depression. They are very effective, but, their use is often associated with a variety of unpleasant and sometimes dangerous side-effects [Citation22] () [29,74,75,80,83,164–174]. Unwanted effects of TCAs arise through interactions with several different neurotransmitter systems.
Table 4. List of the dosage, pharmacokinetics and side-effects of commonly prescribed TCAs and SSRIs for PE
Clomipramine
Clomipramine is a TCA that is indicated for the treatment of major depressive episodes, secondary depression, panic disorder with agoraphobia, generalised anxiety disorder, and obsessive–compulsive disorder (OCD) [Citation23]. Low doses of clomipramine have been suggested to be effective for the treatment of PE [Citation24].
Mechanism of action and efficacy of clomipramine in the treatment of PE
The mechanism by which clomipramine delays ejaculation is unclear. Decreased reuptake of serotonin (or 5-hydroxytryptamine [5-HT]) has been suggested as a mechanism by which several antidepressants including clomipramine delay ejaculation. Clomipramine may increase the sensory threshold for the stimuli in the genital area [Citation25].
Administration of 25 mg clomipramine orally 4 h before planned sexual intercourse was effective in the treatment of patients with PE [Citation26,Citation27]. However, the drug may cause mild yet annoying non-sexual side-effects such as sleepiness and yawning on the day of coitus, and significant nausea the day after. On-demand use of 15 mg clomipramine orally 4 h before sexual intercourse for 4 weeks was safe and effective in prolonging IELT in the treatment of patients with PE [Citation28].
Drug interactions
The antihypertensive effect of propranolol and clonidine may be blocked by clomipramine. Clomipramine with α-methyldopa may cause behavioural agitation. The plasma levels of clomipramine and antipsychotics are increased by their co-administration. The sedation effect of clomipramine and opioids, alcohol and hypnotics are increased by their co-administration [].
2. Selective serotonin reuptake inhibitors (SSRIs)
The SSRIs have emerged as an effective treatment for patients with PE whether or not these patients suffer from depression [Citation29]. They were especially indicated in cases of failed or rejection of psychological treatment, and when partners were unwilling to cooperate in treatment. The SSRIs are widely used because of their safety, tolerability and demonstrated efficacy across a broad range of clinical conditions [Citation11].
The ability of SSRIs to delay ejaculation was first coincidentally discovered as a result of use of these drugs in the treatment of depression in men in the 1970s [Citation30]. The basic principle is that serotonin is a central inhibitory neurotransmitter for sexual function whereas dopamine is a central excitatory neurotransmitter. Antidepressants either elevate serotonin levels leading to inhibition of genital reflexes, or decrease dopamine with the same results [Citation31].
All SSRIs inhibit reuptake of serotonin into presynaptic serotonergic neurones, an action that increases the availability of serotonin at the synapse and ultimately, enhances serotonergic function in the central nervous system (CNS). This mechanism of action depends on the binding of the drug to serotonin transporter protein [Citation32]. It has also been suggested that the efficacy of SSRIs in inhibiting PE, is probably due to increase synaptic 5-HT concentrations via blockade of the 5-HT transporter and activation of the 5-HT 2 C receptor, which then decreases the function of the 5-HT 1A receptor or restores the balance between the two receptor functions (5-HT 1A and 5-HT 2 C) [Citation33,Citation34].
Methods of administration of SSRIs
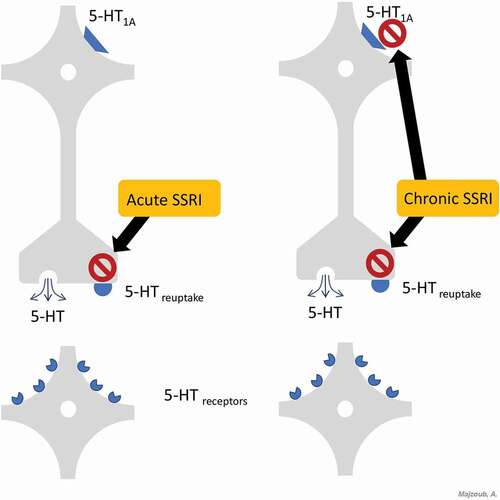
1. Acute SSRI administration
The 5-HT transporter blockade induced by acute administration of all current SSRIs leads to higher serotonin levels in the synapse and in the space around the cells [Citation35]. Increasing serotonin levels activates 5-HT1A auto-receptors, resulting in less serotonin being released into the synaptic cleft within minutes [Citation36]. A higher serotonin concentration increases activation of presynaptic 5-HT1B auto-receptors, which alone can reduce the release of serotonin.
Under normal physiological conditions, the net effect of acute administration of SSRIs is little to no increase in serotonin neurotransmission and minimal or no stimulation of postsynaptic 5-HT receptors (). Given this background, on-demand SSRI treatment would not be expected to result in acute stimulation of 5-HT postsynaptic receptors. Consequently, one would expect minimal increase in synaptic serotonin levels and, thus, little or no synaptic stimulation of 5-HT receptors. Little or no activation of postsynaptic 5-HT receptors should then result in no clinically relevant delay of ejaculation [Citation37].
2. Chronic SSRI administration
In contrast to their acute administration, chronic use of currently available SSRIs causes some physiological changes that delay ejaculation. Ongoing blockade of 5-HT receptors that mediate serotonin reuptake results in a persistent increase in serotonin levels in the synapse and in the space around the cells (). As opposed to the acute administration of SSRIs, this ongoing blockage leads to desensitisation of the 5-HT1A auto-receptors in a few weeks; and possibly of the 5-HT1B auto-receptors [Citation38].
The net effect of the chronic administration of SSRIs is an increase in the serotonin released into the synapse and enhanced serotonin neurotransmission, thus resulting in a stronger activation of the 5-HT postsynaptic receptors compared with that observed in acute SSRI administration [Citation38]. These data predict that daily treatment of SSRI will stimulate the 5-HT postsynaptic receptors, leading to a clinically relevant ejaculation delay after 1–2 weeks of continuous intake [Citation37].
Limitations associated with of SSRIs
While serotonergic drugs are extensively used for the treatment of PE, there are limitations associated with their use. Some of these limitations include unwanted sexual side-effects such as decreased sexual desire and ED [Citation39]. A sudden reduction or cessation of long-term treatment with an SSRI can lead to ‘SSRI discontinuation syndrome’, a group of physical and psychological symptoms including nausea, vomiting, dizziness, headache, ataxia, drowsiness, excitement, anxiety, and insomnia. These symptoms begin 1–3 days after drug cessation and typically continue for >1 week. These side-effects were reversible with SSRI re-introduction [Citation40].
An SSRI overdose or interaction with other drugs, can enhance serotonin activity in the CNS to the point of causing the ‘serotonin syndrome’, a group of serious, persistent symptoms including myoclonus, hyperreflexia, sweating, shivering, discoordination, and mental status changes [Citation41].
Fluoxetine
Fluoxetine is the parent drug of all SSRIs. It has largely (albeit not completely) substituted older and less safe drugs such as TCAs. Fluoxetine is a serotonin-specific antidepressant approved in 1987 by the FDA for treatment of depression [Citation42]. It is also a treatment option for patients with Alzheimer’s disease who have severe obsessive–compulsive symptoms [Citation43] and for patients with intention myoclonus [Citation44].
Efficacy of fluoxetine in treatment of PE
Fluoxetine is more selective and more potent in retarding ejaculation as compared to TCAs [Citation45]. At a dose of 20 mg daily for 1 week followed by 40 mg daily for ~4 weeks, fluoxetine successfully improved PE in a double-blind placebo controlled study of 17 patients [Citation46]. Another study revealed that a significant decrease in self-reported ‘poor’ ejaculatory control, high personal distress and high partner distress were noted in men receiving 20 mg fluoxetine for 12 months [Citation47].
The rationale with which fluoxetine is thought to exhibit its beneficial effects is through increasing the penile sensory threshold, without changing the amplitudes and latencies of sacral evoked response and cortical somatosensory evoked potentials [Citation48]. A study compared 90 mg once weekly dose with 20 mg daily doses fluoxetine on 80 patients with PE [Citation49]. After a 4-month treatment period, the authors reported significant prolongation in the IELT, together with improved International Index of Erectile Function (IIEF) results and partner sexual satisfaction in both groups. There were no significant differences between both treatment methods in terms of efficacy and reported side-effects.
The co-administration of fluoxetine and PDE5 inhibitors appears to have a potentiating effect on sexual satisfaction. The combination of fluoxetine (20 mg fluoxetine daily for 4 weeks followed by 20 mg on-demand 2–3 h before planned sexual activity for 4 months) with sildenafil (50 mg 1 h before sexual activity for 4 months) resulted in significantly better IELT and intercourse satisfaction compared with fluoxetine alone in patients with PE [Citation50]. Similarly, administration of 90 mg fluoxetine once per week plus 20 mg tadalafil within 36-h before planned sexual intercourse for 12 weeks in patients with lifelong PE resulted in significantly longer IELT compared with fluoxetine only or tadalafil only treatment [Citation51].
Citalopram
Citalopram is a potent specific inhibitor of neuronal serotonin reuptake [Citation52] that is indicated for the treatment of depression, anxiety, panic disorder, OCD, premenstrual dysphoria, alcohol dependence, and behavioural disturbances of dementia [Citation53].
Efficacy of citalopram in treatment of PE
The daily administration of 20 mg citalopram in patients with PE resulted in significant increase in IELT, improved overall patient sexual satisfaction, and decreased performance anxiety [Citation54,Citation55]. Citalopram was compared to SSRIs in several studies. A randomised controlled trial (RCT) compared the efficacy of citalopram 20 mg to sertraline 50 mg for a treatment period of 8 weeks in patients with PE. The authors reported a statistically significant increase in the results of the IPE questionnaire in both the citalopram and sertraline groups, without a significant difference in efficacy between the two treatments. No serious adverse effects were detected in any of the patients and both drugs were well tolerated [Citation56].
A randomised, placebo-controlled, double-blind study evaluated the effects of 20 mg/day citalopram and 20 mg/day fluoxetine [Citation57]. The authors assessed the effect of the intervention on masturbation IELT, Rigiscan, and the IIEF-15 questionnaire. Results revealed a delay in the IELT in both the treatment groups compared with placebo; however, the difference was only statistically significant for the citalopram group. No significant effect on nocturnal penile tumescence, measured with Rigiscan, was observed in any of the treatment groups.
The authors of the latter study concluded that while there was no objective effect on penile erection, the subjective sexual impairment could be attributed to the significant delay in ejaculation achieved with citalopram). Another study evaluated IELT and sexual satisfaction in 16 newly married men with PE, and a history of unsuccessful treatment with fluoxetine, using citalopram as a salvage treatment [Citation58]. The IELT was significantly improved after treatment with citalopram together with a significant increase in sexual satisfaction
Escitalopram
Escitalopram is the S-isomer of the racemic compound citalopram, that is widely used in both psychiatric and primary care practices for the treatment of depression. It was found to be effective and well tolerated in treating depression at a dose of 10 mg/day [Citation59,Citation60]. At this dose, escitalopram is at least as effective as citalopram 40 mg/day [Citation59]. Escitalopram also has been shown to be rapidly effective in treating symptoms of anxiety associated with depression [Citation61].
Escitalopram is the most selective molecule for serotonin receptors compared to other antidepressants [Citation62]. In a radio-ligand binding study of cells expressing human serotonin transporters, escitalopram proved to be ~30-times more potent than its enantiomer, R-citalopram, in its capacity to bind to the serotonin transporter receptor site [Citation32].
Escitalopram was more selective for serotonergic transport proteins when compared with other SSRIs such as fluoxetine, paroxetine, fluvoxamine or sertraline [Citation32]. Escitalopram had little or no binding affinity for >100 binding sites tested in vitro, including α-adrenergic (α1) receptors, muscarinic (M1) receptors and histamine (H1) receptors [Citation63]. Selectivity for serotonergic, rather than muscarinic, histaminergic, or adrenergic receptors suggested a lower potential for causing dry mouth, sedation, or cardiovascular side-effects [Citation32,Citation62]. Patients who have switched from fluoxetine, sertraline, paroxetine, or citalopram to escitalopram due to adverse events experienced a lower incidence of side-effects [Citation64].
Efficacy of escitalopram in treatment of PE
A double-blind placebo-controlled study assessing the efficacy of daily administration of 10 mg escitalopram in 276 patients with PE for 12 weeks revealed a significant 4.9-fold increase in the IELT in the treatment group together with significant increase in intercourse satisfaction (measured with the IIEF-15) [Citation65]. Similar results were re-demonstrated by another study of similar design showing that the effect of escitalopram was well maintained up to 2 months after stopping the drug [Citation66]. A study compared the efficacy of three SSRIs (escitalopram 10 mg/day, fluoxetine 20 mg/day and paroxetine 20 mg/day) on subjective PE symptoms of 100 men measured using the Arabic Index of Premature Ejaculation (AIPE) [Citation67]. The authors reported a significant improvement in PE symptoms after treatment, without a statistically significant difference in efficacy between the three treatments.
Sertraline
Sertraline is another SSRI that is used for a number of conditions, including major depressive disorder, OCD, body dysmorphic disorder, and panic disorder [Citation68]. Sertraline is a potent inhibitor of serotonin reuptake and is ~14-times more potent than fluoxetine in enhancing serotonergic neurotransmission [Citation69].
Efficacy of sertraline in treatment of PE
Several studies have shown that sertraline is an effective agent in the treatment of PE, indicated by increased IELT and partner’s sexual satisfaction [Citation31,Citation70]. A daily dose of 25–50 mg for 2–3 weeks is recommended after which the drug can be taken on-demand, 4–6 h before sexual activity [Citation31]. A prospective placebo-controlled crossover study of 147 men with PE receiving sertraline 50 mg/day or placebo for 4-week intervals demonstrated significant improvement in the IELT and sexual satisfaction, using the AIPE, only in patients receiving sertraline treatment [Citation71].
Another study compared the efficacy of sertraline 50 mg/day vs citalopram 20 mg/day for 8 weeks in 80 patients with PE [Citation56]. The authors documented significant increase in IPE results in both treatment groups without any significant difference in the efficacy of the two agents. No serious adverse effects were detected in any of the patients and both drugs were well tolerated. A recent study suggested that increasing the dose of sertraline to 100 mg/day in patients not responding to an 8-week treatment with sertraline 50 mg/day demonstrated good tolerance to the higher dose regimen [Citation72].
Paroxetine hydrochloride
Paroxetine is an antidepressant SSRI that has been shown to be effective in treatment of major depression, panic disorder, OCD, and social anxiety disorder [Citation73,Citation74].
Efficacy of paroxetine in treatment of PE
Paroxetine in a dose of 20 mg was an adequate treatment for primary PE, and a further increase in ejaculation latency may be achieved by increasing the dose [Citation75]. The effect of paroxetine on the prolongation of the IELT after 6 weeks of treatment was significantly better if patients were treated initially with 20 mg paroxetine daily for 2 weeks, followed by 4 weeks of on-demand dosing compared with patients who began on-demand dosing with 20 mg [Citation76]. Compared with other medications used for the treatment of PE, administration of 20 mg/day paroxetine for 12 weeks in patients with PE resulted in comparable efficacy to dapoxetine 60 mg/day with a statistically significant increase in the IELT and intercourse satisfaction domains of the IIEF-15 [Citation77].
Paroxetine 20 mg/day was also compared to tramadol HCl 50 mg on-demand in 35 patients with lifelong PE who were randomised to receive either treatment and were followed-up after 6 and 12 weeks of therapy [Citation78]. Paroxetine and tramadol increased IELT significantly by 11-fold and sevenfold after 6 weeks of therapy, respectively. However, after 12 weeks, further increase in the IELT to 22-fold was only detected in patients receiving paroxetine. Changes in the IELT were demonstrated by the AIPE results, as patients receiving paroxetine reported significant improvement after 6 and 12 weeks of therapy, while those receiving tramadol reported a significant improvement after 6 weeks and not 12 weeks of therapy
Fluvoxamine
Fluvoxamine is a potent specific inhibitor of neuronal serotonin reuptake with few side-effects [Citation79]. It appears to be effective in treatment of depression, OCD, and PE [Citation22].
Efficacy of fluvoxamine in treatment of PE
Fluvoxamine is probably the least effective SSRI in the treatment of PE. A double-blind, placebo-controlled study was conducted in men with lifelong PE to compare the efficacy of four SSRIs (fluoxetine, fluvoxamine, paroxetine, and sertraline) in delaying ejaculation [Citation80]. Patients were randomised to receive fluoxetine 20 mg/day, fluvoxamine 100 mg/day, paroxetine 20 mg/day, sertraline 50 mg/day, or placebo for 6 weeks. A significant increase in the IELT was only observed in the paroxetine, fluoxetine, and sertraline groups, whereas in the fluvoxamine group, a minimal increase in the IELT was detected.
Dapoxetine
Dapoxetine is the first member of the SSRI family to be developed specifically for the treatment of PE [Citation81]. Its rapid absorption and elimination in the body makes it suitable for the treatment of PE, but not as an antidepressant [Citation82].
Efficacy in treatment of PE
A systemic review of five randomised, placebo-controlled phase III clinical trials [Citation83–86] including 4232 men with PE from 32 countries confirmed that dapoxetine 30 and 60 mg increased the IELT and improved PROs of control, ejaculation-related distress, interpersonal distress and sexual satisfaction compared with placebo [Citation87]. The pooled data revealed a statistically significant increase in the IELT with dapoxetine 30 mg (+2.3 min), dapoxetine 60 mg (+2.7 min) compared with placebo (+1.5 min). Dapoxetine 30 and 60 mg were well tolerated with a low incidence of severe adverse effects.
A recent single-blind placebo-controlled clinical study compared the efficacy of on-demand treatment with paroxetine 30 mg, dapoxetine 30 mg, sildenafil 50 mg, combined dapoxetine 30 mg + sildenafil citrate 50 mg and placebo on 150 patients with PE for a period of 6 weeks [Citation88]. The authors reported significant improvement in the IELT, sexual satisfaction score and PE diagnostic tool score in all groups after treatment, with the best values reported in the combined dapoxetine + sildenafil citrate group. Another comparative study assessed the efficacy of on-demand dapoxetine 30 mg, on-demand dapoxetine 60 mg and daily paroxetine 20 mg on 150 patients with PE for a 1-month duration [Citation89]. The IELT increased by 117%, 170% and 117% from baseline to post-treatment in the 30 mg dapoxetine group, 60 mg dapoxetine group and paroxetine group; respectively. Dapoxetine was found to have an additive effect on psychotherapy for the treatment of patients with PE.
SSRI drug interactions
Almost all SSRIs are dependent on liver metabolism by cytochrome P450 (CYP450) enzyme isoforms each with a distinct profile of inhibition (). When SSRIs are co-administered with drugs that are metabolised by a specific CYP450 enzyme, they compete for binding to the active site of the enzyme [Citation90], inhibiting the metabolism of the other drug substrates and elevating their plasma levels. This prolonged drug action can place patients at increased risk of drug toxicity. This drug interaction is often faced when SSRIs are co-administered with psychiatric drugs, as well as other medications given for a variety of medical conditions.
The SSRIs are not uncommonly combined with TCAs to treat psychiatric patients. As both drug classes are metabolised by CYP450 enzymes, the resulting interaction is well documented and increased plasma concentrations of TCAs have been reported. More specifically, concomitant use of fluoxetine or paroxetine, both potent CYP2D6 inhibitors, with TCAs was shown to be associated with up to fivefold increase in plasma concentrations of TCAs, and patients undergoing this interaction exhibited toxicity symptoms such as sedation, dry mouth, and urinary retention [Citation91–93]. Fluvoxamine, a potent CYP2C19 inhibitor, caused up to fourfold increases in plasma concentrations of the TCAs amitriptyline, imipramine, and clomipramine and related clinical signs of toxicity [Citation92].
Antipsychotics are another example of drugs that interact with SSRIs as they are metabolised by one or more of the CYP450 enzymes. Clozapine, olanzapine, and risperidone are the antipsychotics with the most frequent reported effects [Citation94,Citation95]. Fluoxetine and fluvoxamine can interact with anticonvulsants valproate and carbamazepine through their inhibitory effect on CYP2C9 and CYP3A4/5 respectively. Serious reactions including excessive tiredness, irritability, dizziness, and tremor have been reported leading to the discontinuation of the SSRI [Citation96,Citation97].
Serotonin syndrome is a group of symptoms that may occur following the combination of two or more serotonergic medications. It is typically seen when SSRIs are co-administered with lithium, tryptophan and monoamine oxidase inhibitors [Citation98]. The release of serotonin by platelets is important for maintaining haemostasis, thus SSRIs may increase the risk of bleeding.
Interactions have been reported with anticoagulants such as warfarin and clopidogrel. Based on their strong inhibition of CYP2C9, fluoxetine and fluvoxamine have the highest potential risk for inhibiting warfarin metabolism thereby causing excessive bleeding. Furthermore, several SSRIs are potent inhibitors to CYP2C19 abolishing the antiplatelet response to clopidogrel [Citation99].
Topical therapy (anaesthetics)
A. Lidocaine-prilocaine 5% cream
Topical anaesthetics have been used for treatment of PE to decrease penile stimulation, and thus delay the time to ejaculation. The application of lidocaine-prilocaine 5% cream to penis before covering it with a condom 20–30 min before intercourse delayed ejaculation in men with PE. Prolonged application (30–45 min) before intercourse resulted in loss of erection [Citation100]. Reduction in genital sensitivity of both partners may limit repeated use of topical anaesthetics [Citation101].
Lidocaine-prilocaine cream used for a period of 30–60 days significantly increases the mean IELT, especially when penile hypersensitivity is likely to be the cause. The main side-effects of topical anaesthetic application included retarded ejaculation of >30 min, decreased penile sensitivity, penile irritation, and decreased vaginal sensitivity [Citation102]. Topical anaesthetics are contraindicated for patients and/or their partners with allergies to any component of the product [Citation103]. Administration of 20 mg fluoxetine daily plus local application of lidocaine ointment was found to be more effective than fluoxetine alone [Citation104].
B. Local Severance Secret (SS) cream
The SS-cream is formed from nine natural substances including ginseng and cinnamon and has local desensitising and vasoactive effects differing from the local anaesthetics in the fact that it persists for up to 2 h. It promises to be an effective and safe therapeutic modality for patients with PE [Citation105]. Applying SS-cream on the glans penis 1 h before planned sexual intercourse, lead to prolongation of ejaculatory latency time and improvement of sexual satisfaction for both partners with no adverse effect [Citation105,Citation106]. A study assessed penile vibratory threshold change using a bio-thesiometer using various doses of SS-cream and found that SS-cream increased the penile sensory threshold in a dose-dependent manner [Citation107].
C. Lidocaine-prilocaine spray
Topical eutectic mixture for PE (TEMPE or PSD502) is a formulation of lidocaine and prilocaine in a metered dose aerosol-delivery system. Each spray delivers 7.5 mg lidocaine and 2.5 mg prilocaine. It is fast acting (within 5 min) and appears to be effective in improving the IELT and sexual satisfaction in patients with PE. It does not penetrate keratinised epithelium, and so only anaesthetises the glans, with no systemic side-effects and a low incidence of local side-effects [Citation108,Citation109].
D. Dyclonine/alprostadil cream
Dyclonine is a local anaesthetic usually used in the field of dentistry. It has been combined with the vasodilator alprostadil and used to treat PE. The product is applied 5–20 min before intercourse to the tip of the penis in the region of the meatus. One pilot study claimed positive results with it; however, the data were limited and further studies are warranted before conclusions can be made [Citation110].
Phosphodiesterase type 5 inhibitors
Several clinical trials have examined the potential effectiveness of the PDE5 inhibitor, sildenafil, in the treatment of PE. The rationale for the use of PDE5 inhibitors in the treatment of PE may be due to peripheral and/or central mechanisms. Ejaculation retarding by peripheral actions may include modulation of contractile response of vas deferens, seminal vesicles, prostate and urethra, induction of a state of peripheral analgesia, and prolongation of the total duration of erection. Central mechanisms may involve lessening of the central sympathetic output [Citation111].
The on-demand administration of 50–100 mg sildenafil citrate for 1–3 months, in patients with PE complicated by ED, was found to safely and effectively improve erectile function and prolong ejaculation [Citation112]. In addition, sildenafil citrate increased confidence, perception of ejaculatory control, and overall sexual satisfaction, and decreased the refractory time to achieve a second erection after ejaculation in men with PE [Citation113]. It has also been shown that sildenafil combined with behavioural therapy produced more prolongation of the IELT and better male and female satisfaction than behavioural therapy alone in the treatment of patients with PE [Citation114]. On-demand administration of 50 mg sildenafil 1 h before planned sexual activity combined with 10 mg paroxetine daily for 3 weeks and then 20 mg on demand, for 6 months provided significant increases in the ILET and intercourse satisfaction than paroxetine alone in potent patients with PE. However, combined treatment is associated with a mild increase in drug-related side-effects (headache and flushing episodes) [Citation115].
Sildenafil citrate combined with paroxetine and psychological and behavioural counselling alleviated PE in patients in whom other treatments failed [Citation116]. Administration of 50 mg sildenafil on-demand 1 h before planned sexual activity combined with 50 mg sertraline daily, for 12 weeks produced more prolongation of the IELT, and better male and female satisfaction than sertraline alone in patients with PE [Citation117]. Furthermore, the on-demand administration of 50 mg sildenafil citrate 1 h before planned sexual activity for 6 months in patients with PE provided significant increases in the IELT and intercourse satisfaction than 20 mg paroxetine daily and the squeeze technique. However, adverse effects were more frequent in the sildenafil and paroxetine groups compared to the squeeze technique group. The most frequent adverse effects for sildenafil were headache and nasal congestion [Citation118].
Other forms of PDE5 inhibitors have been used for the treatment of PE. The administration tadalafil 20 mg within 36 h before planned sexual intercourse combined with fluoxetine 90 mg once per week for 12 weeks in patients with lifelong PE resulted in significant increase in the IELT when compared to fluoxetine or tadalafil alone [Citation51]. The on-demand administration of 10 mg vardenafil for 16 weeks provided significant increase of IELT and reduced post-ejaculatory refractory time in men with lifelong PE [Citation119]. Improvement in confidence, perception of ejaculatory control and overall sexual satisfaction were reported.
The use of 5 mg tadalafil once daily plus lidocaine anaesthetic spray in treatment of lifelong PE was more effective than tadalafil alone or lidocaine anaesthetic spray alone [Citation120]. In a single- blind placebo-controlled clinical study, the combined use of on-demand dapoxetine (30 mg) with sildenafil (50 mg) for patients with PE for 6 weeks had the best values of IELT and satisfaction scores in comparison with dapoxetine alone or sildenafil alone [Citation88].
Opioid agonist
Tramadol is a centrally acting analgesic with two mechanisms of action. It exerts an effect on the μ-opioid receptor, but also inhibits noradrenaline and serotonin reuptake. Its mechanism of action in PE is poorly understood; however, it is thought to be related to its action on the μ-opioid receptor, which may reduce sensitivity, as well as the inhibition of serotonin reuptake, which may delay ejaculation. It has a safety profile that is well tolerated with few side-effects [Citation121].
Administration of 50 mg tramadol HCl 2 h before planned sexual activity for 8 weeks, resulted in a significant increase of IELT and intercourse satisfaction vs placebo [Citation55]. Administration of 25 mg tramadol, 1–2 h before planned sexual activity for 8 weeks, significantly increased the IELT and intercourse satisfaction [Citation121]. Administration of 50 mg tramadol with behavioural modification, 2 h before planned sexual activity for 8 weeks resulted in significant improvement in the IELT and overall sexual satisfaction [Citation122]. On-demand administration of 62 mg tramadol (oral disintegrating tablet), 2–8 h before planned sexual intercourse for 12 weeks in patients with mild to severe PE resulted in significant increase in the IELT, improvement in overall sexual satisfaction and control over ejaculation, and decreased ejaculation-related personal distress and interpersonal difficulty [Citation123].
As tramadol is an opioid, with weak µ-opioid activity, there are concerns about its abuse and dependence. Long-term studies are needed to determine the verifiable risk of opioid addiction [Citation9,Citation124].
Surgical treatments
a. Glans augmentation
Glans augmentation has been a technique proposed to desensitise the glans penis and slow the ejaculatory reflex. It is a method in which hyaluronic acid is injected into the glans at the coronal edge to provide analgesia of the penis. Hyaluronic acid is a glycosaminoglycan and bulking agent that has been used to insulate the nerve endings and provide long-term (>1 year) local anaesthesia. It was reported to increase the IELT and satisfaction in patients with PE [Citation125,Citation126].
b. Dorsal neurectomy
Dorsal neurectomy with or without glandular augmentation with hyaluronic acid gel has been reported for treatment of refractory PE. It showed a significant increase in the IELT and patient satisfaction but associated with significant side-effects, including penile numbness, paraesthesia and pain [Citation125]. It has been reported that selective neurotomy of the dorsal penile nerve preserved potency and decreased sensitivity [Citation127].
c. Pulsed radiofrequency neuromodulation
Pulsed radiofrequency neuromodulation has been used for treatment of PE by desensitisation of the dorsal penile nerves. It showed a significant increase in the IELT in patients with PE. There were no reported side-effects post-procedure such as pain, penile hypoesthesia, or ED [Citation128].
d. Frenectomy
Frenectomy has been studied as a possible surgical therapy for PE because of the association of PE with a short frenulum, or frenulum breve [Citation129]. This condition can be congenital resulting from defects during sexual development or acquired secondary to excessive scarring occurring after rupture of a normal frenulum [Citation130]. It hinders complete retraction of the prepuce during erection causing a ventral curvature of the glans. It is thought that a short frenulum may illicit PE through two plausible premises: (1) an uncomfortable sense of traction during intercourse that may trigger the end of coitus, (2) being a reservoir of nerve endings that are directly exposed to the tactile stimulation during intercourse [Citation129].
e. Surgical removal of foreskin remnants
Surgical removal of foreskin remnants in incomplete circumcised adult patients with PE resulted in a significant increase in the IELT, overall sexual satisfaction, and control over ejaculation because it significantly decreased hypersensitivity of penis [Citation131].
f. Varicocelectomy
A higher prevalence of PE has been reported in men with varicocele for unclear reasons [Citation132,Citation133]. Some have postulated that an increase in local genital temperature or the resulting androgen disruption that occurs with varicocele could be possible explanations [Citation134]. Several studies have clearly reported an improvement in PE and testicular hormonal function in patients following varicocele ligation [Citation135,Citation136]. However, such an indication for varicocelectomy is not yet supported by any of the international guidelines of male reproduction.
Other treatment
A. Adrenergic nerve blockade has been proposed as a treatment for PE. A clinical trial showed modest efficacy with alfuzosin and terazosin [Citation137]. Silodosin, a highly selective α1A-adrenoceptor antagonist and on-demand use of 4 mg silodosin orally 1 h before sexual intercourse in treatment of patients with PE was effective in improving PE profile and the IELT [Citation138]. The treatment was based on the fact that emission and ejaculation are under the influence of the sympathetic nervous system [Citation139].
B. Folic acid provides the methyl group for the conversion of methionine to S-adenosylmethionine, which itself has been shown to influence serotonin metabolism. It has an important role in the synthesis of tetrahydrobiopterin, the rate limiting step in the synthesis of dopamine, noradrenaline and serotonin [Citation140,Citation141]. Folic acid supplementation was reported to produce an antidepressant-like effect, mediated by an interaction with the noradrenergic receptors (α1 and α2) and serotonergic receptors (5-HT1A and 5-HT2A/2 C) [Citation142]. Low folate is associated with poorer response to SSRIs. Folate deficiency is associated with decreased serotonin activity [Citation143] and folate supplementation increases cerebrospinal fluid levels of 5-hydroxyindoleacetic acid (the main metabolite of serotonin) in folate deficient patients suffering from depression [Citation144]. Therefore, folic acid was suggested to exert a significant role in the pathogenesis of PE. Folic acid administration produces anti-PE-like effects dependent on the 5-HT systems. Folic acid may offer a cheaper, safer, more efficacious and more acceptable alternative to the conventional SSRIs for men with PE. However, more information is needed about the dosage, possible side-effects, and populations suited for the therapy [Citation122].
C. Caffeine is a recently proposed treatment for PE. A double-blind RCT found that using 100 mg caffeine 2 h before intercourse significantly improved the IELT and sexual satisfaction of 40 patients with PE [Citation145]. Being a purine alkaloid, caffeine is a CNS stimulant and can increase the levels of multiple neurotransmitters including dopamine and serotonin [Citation146].
D. A RCT using rat models, injections of botulinum toxin into each bulbospongiosus muscle increased the IELT relative to the group with saline injections. There was no effect on the rats’ ability to achieve and maintain an erection [Citation147]. Mechanism would likely rely on the toxin’s ability to paralyse the neural end-plate, decreasing the ability of the muscles associated with ejaculation to contract [Citation148].
Conclusions
Premature ejaculation is a commonly encountered male sexual dysfunction, with a potential negative impact on the patient and his partner. In the present review, we explored the different therapeutic approaches that are currently available for the treatment of PE including behavioural, pharmacological, and surgical options. Interestingly, the medications currently used in the treatment of PE are sold off-label. Except for the newly licensed dapoxetine, which provides an effective, on-demand treatment regimen with relatively minimal side-effects, it is not clear whether it received final FDA approval for treatment of PE. Therefore, it is important for the clinician to recognise all PE treatment options as each patient may respond differently and experience variable side-effects. Future efforts should be directed towards understanding the exact pathophysiology of PE at different clinical setups and developing additional therapies with higher efficacy and minimal or no adverse effects.
Disclosure statement
The authors report no conflict of interest.
References
- Saitz TR, Serefoglu EC. The epidemiology of premature ejaculation. Transl Androl Urol. 2016;5(4):409–415.
- Serefoglu EC, McMahon CG, Waldinger MD, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second international society for sexual medicine ad hoc committee for the definition of premature ejaculation. Sex Med. 2014;2(2):41–59.
- El-Hamd MA, Saleh R, Majzoub A. Premature ejaculation: an update on definition and pathophysiology. Asian J Androl. 2019;21(5):425–432.
- Majzoub A, Arafa M, Al-Said S, et al. Premature ejaculation in type II diabetes mellitus patients: association with glycemic control. Transl Androl Urol. 2016;5(2):248–254.
- Althof SE, McMahon CG, Waldinger MD, et al. An Update of the International Society of Sexual Medicine’s Guidelines for the Diagnosis and Treatment of Premature Ejaculation (PE). Sex Med. 2014 Jun;2(2):60–90.
- Althof SE, Abdo CH, Dean J, et al. International Society for Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation. J Sex Med. 2010;7(9):2947–2969.
- Wang WF, Chang L, Minhas S, et al. Selective serotonin reuptake inhibitors in the treatment of premature ejaculation. Chin Med J (Engl). 2007;120(11):1000–1006.
- Hellstrom WJ. Available and future therapies for premature ejaculation. Drugs Today (Barc). 2010;46(7):507–521.
- Hellstrom WJ. Update on treatments for premature ejaculation. Int J Clin Pract. 2011;65(1):16–26.
- Richardson D, Goldmeier D. Pharmacological treatment for premature ejaculation. Int J STD AIDS. 2005;16(10):709–711.
- Stone KJ, Viera AJ, Parman CL. Off-label applications for SSRIs. Am Fam Physician. 2003;68(3):498–504.
- Semans JH. Premature ejaculation: a new approach. South Med J. 1956;49(4):353–358.
- Masters WM, Johnson VE. Human sexual inadequacy. Boston, MA: Little, Brown; 1970.
- de Carufel F, Trudel G. Effects of a new functional-sexological treatment for premature ejaculation. J Sex Marital Ther. 2006;32(2):97–114.
- Althof SE, Wieder M. Psychotherapy for erectile dysfunction: now more relevant than ever. Endocrine. 2004;23(2–3):131–134.
- Althof S. The psychology of premature ejaculation: therapies and consequences. J Sex Med. 2006;3(Suppl 4):324–331.
- Althof S. Therapeutic weaving: the integration of treatment techniques. In: Levine S, Risen C, Althof S, editors. Handbook of Clinical Sexuality for Mental Health Professionals. New York, NY: Bruner-Routledge; 2003. pp. 359–376
- Hawton K, Catalan J, Martin P, et al. Long-term outcome of sex therapy. Behav Res Ther. 1986;24(6):665–675.
- De Amicis LA, Goldberg DC, LoPiccolo J, et al. Clinical follow-up of couples treated for sexual dysfunction. Arch Sex Behav. 1985;14(6):467–489.
- Sharlip I. Diagnosis and treatment of premature ejaculation: the physician’s perspective. J Sex Med. 2005;2(Suppl 2):103–109.
- Labrid C, Moleyre J, Poignant JC, et al. Structure-activity relationships of tricyclic antidepressants, with special reference to tianeptine. Clin Neuropharmacol. 1988;11(Suppl 2):S21–31.
- Goodman WK, Gilman HM. The pharmacological basis of therapeutics. 8th ed. New York, NY: Pergamon Press; 1990.
- Koen N, Stein DJ. Pharmacotherapy of anxiety disorders: a critical review. Dialogues Clin Neurosci. 2011;13(4):423–437.
- Segraves RT, Saran A, Segraves K, et al. Clomipramine versus placebo in the treatment of premature ejaculation: a pilot study. J Sex Marital Ther. 1993;19(3):198–200.
- Colpi GM, Fanciullacci F, Aydos K, et al. Effectiveness mechanism of chlomipramine by neurophysiological tests in subjects with true premature ejaculation. Andrologia. 1991;23(1):45–47.
- Strassberg DS, de Gouveia Brazao CA, Rowland DL, et al. Clomipramine in the treatment of rapid (premature) ejaculation. J Sex Marital Ther. 1999;25(2):89–101.
- Waldinger MD, Zwinderman AH, Olivier B. On-demand treatment of premature ejaculation with clomipramine and paroxetine: a randomized, double-blind fixed-dose study with stopwatch assessment. Eur Urol. 2004;46(4):510–516.
- Kim SW, Choi JB, Kim SJ, et al. Tolerability and adequate therapeutic dosage of oral clomipramine for the treatment of premature ejaculation: a randomized, double-blind, placebo-controlled, fixed-dose, parallel-grouped clinical study. Int J Impot Res. 2018;30(2):65–70.
- Balon R. Antidepressants in the treatment of premature ejaculation. J Sex Marital Ther. 1996;22(2):85–96.
- Patterson WM. Fluoxetine-induced sexual dysfunction. J Clin Psychiatry. 1993;54(2):71.
- McMahon CG. Treatment of premature ejaculation with sertraline hydrochloride: a single-blind placebo controlled crossover study. J Urol. 1998;159(6):1935–1938.
- Owens MJ, Knight DL, Nemeroff CB. Second-generation SSRIs: human monoamine transporter binding profile of escitalopram and R-fluoxetine. Biol Psychiatry. 2001;50(5):345–350.
- Waldinger MD, Olivier B. Utility of selective serotonin reuptake inhibitors in premature ejaculation. Curr Opin Invest Drugs. 2004;5(7):743–747.
- Olivier B, Chan JS, Pattij T, et al. Psychopharmacology of male rat sexual behavior: modeling human sexual dysfunctions? Int J Impot Res. 2006;18(Suppl 1):S14–23.
- Siesser WB, Sachs BD, Ramsey AJ, et al. Chronic SSRI treatment exacerbates serotonin deficiency in humanized Tph2 mutant mice. ACS Chem Neurosci. 2013;4(1):84–88.
- Albert PR, Lemonde S. 5-HT1A receptors, gene repression, and depression: guilt by association. Neuroscientist. 2004;10(6):575–593.
- Waldinger MD, Schweitzer DH, On-demand OB. SSRI treatment of premature ejaculation: pharmacodynamic limitations for relevant ejaculation delay and consequent solutions. J Sex Med. 2005;2(1):121–131.
- Altieri SC, Garcia-Garcia AL, Leonardo ED, et al. Rethinking 5-HT1A receptors: emerging modes of inhibitory feedback of relevance to emotion-related behavior. ACS Chem Neurosci. 2013;4(1):72–83.
- Montejo AL, Llorca G, Izquierdo JA, et al. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the Study of Psychotropic-Related Sexual Dysfunction. J Clin Psychiatry. 2001;62(Suppl 3):10–21.
- Black K, Shea C, Dursun S, et al. Selective serotonin reuptake inhibitor discontinuation syndrome: proposed diagnostic criteria. J Psychiatry Neurosci. 2000;25(3):255–261.
- Greenier E, Lukyanova V, Reede L. Serotonin syndrome: fentanyl and selective serotonin reuptake inhibitor interactions. AANA J. 2014;82(5):340–345.
- Goodnick PJ. Pharmacokinetics of second generation antidepressants: fluoxetine. Psychopharmacol Bull. 1991;27(4):503–512.
- Marksteiner J, Walch T, Bodner T, et al. Fluoxetine in Alzheimer’s disease with severe obsessive compulsive symptoms and a low density of serotonin transporter sites. Pharmacopsychiatry. 2003;36(5):207–209.
- Sommi RW, Crismon ML, Bowden CL. Fluoxetine: a serotonin-specific, second-generation antidepressant. Pharmacotherapy. 1987;7(1):1–15.
- Hsieh JT, Chang HC, Law HS, et al. In vivo evaluation of serotonergic agents and alpha-adrenergic blockers on premature ejaculation by inhibiting the seminal vesicle pressure response to electrical nerve stimulation. Br J Urol. 1998;82(2):237–240.
- Kara H, Aydin S, Yucel M, et al. The efficacy of fluoxetine in the treatment of premature ejaculation: a double-blind placebo controlled study. J Urol. 1996;156(5):1631–1632.
- Jenkins LC, Gonzalez J, Tal R, et al. Compliance with fluoxetine use in men with primary premature ejaculation. J Sex Med. 2019;16(12):1895–1899.
- Yilmaz U, Tatlisen A, Turan H, et al. The effects of fluoxetine on several neurophysiological variables in patients with premature ejaculation. J Urol. 1999;161(1):107–111.
- Manasia P, Pomerol J, Ribe N, et al. Comparison of the efficacy and safety of 90 mg versus 20 mg fluoxetine in the treatment of premature ejaculation. J Urol. 2003;170(1):164–165.
- Hosseini MM, Yarmohammadi H. Effect of fluoxetine alone and in combination with sildenafil in patients with premature ejaculation. Urol Int. 2007;79(1):28–32.
- Mattos RM, Marmo Lucon A, Srougi M. Tadalafil and fluoxetine in premature ejaculation: prospective, randomized, double-blind, placebo-controlled study. Urol Int. 2008;80(2):162–165.
- Andersen P. Effective vaccination of mice against Mycobacterium tuberculosis infection with a soluble mixture of secreted mycobacterial proteins. Infect Immun. 1994;62(6):2536–2544.
- Pollock BG. Citalopram: a comprehensive review. Expert Opin Pharmacother. 2001;2(4):681–698.
- Atmaca M, Kuloglu M, Tezcan E, et al. The efficacy of citalopram in the treatment of premature ejaculation: a placebo-controlled study. Int J Impot Res. 2002;14(6):502–505.
- Safarinejad MR, Hosseini SY. Safety and efficacy of citalopram in the treatment of premature ejaculation: a double-blind placebo-controlled, fixed dose, randomized study. Int J Impot Res. 2006;18(2):164–169.
- Akgul T, Karakan T, Ayyildiz A, et al. Comparison of sertraline and citalopram for treatment of premature ejaculation. Urol J. 2008;5(1):41–45.
- Madeo B, Bettica P, Milleri S, et al. The effects of citalopram and fluoxetine on sexual behavior in healthy men: evidence of delayed ejaculation and unaffected sexual desire. A randomized, placebo-controlled, double-blind, double-dummy, parallel group study. J Sex Med. 2008;5(10):2431–2441.
- Dadfar MR, Baghinia MR. Salvage use of citalopram for treatment of fluoxetine-resistant premature ejaculation in recently married men: a prospective clinical trial. J Urol. 2010;7(1):40–44.
- Burke WJ, Gergel I, Bose A. Fixed-dose trial of the single isomer SSRI escitalopram in depressed outpatients. J Clin Psychiatry. 2002;63(4):331–336.
- Wade A, Michael Lemming O, Bang Hedegaard K. Escitalopram 10 mg/day is effective and well tolerated in a placebo-controlled study in depression in primary care. Int Clin Psychopharmacol. 2002;17(3):95–102.
- Gorman JM, Korotzer A, Su G. Efficacy comparison of escitalopram and citalopram in the treatment of major depressive disorder: pooled analysis of placebo-controlled trials. CNS Spectr. 2002;7(Suppl 1):40–44.
- Owens MJ, Rosenbaum JF. Escitalopram: a second-generation SSRI. CNS Spectr. 2002;7(Suppl 1):34–39.
- Sanchez C, Brennum L. The S-enantiomer of citalopram (Lu 26-054) is a highly selective and potent serotonin reuptake inhibitor. Biol Psychiatry. 2000;47:885.
- Rosenthal MH, Li D Efficacy and tolerability of escitalopram in patients intolerant of other SSRIs. 23rd Congress of the Collegium internationale Neuro-Psychopharmacologium; Montreal, Canada 2002.
- Safarinejad MR. Safety and efficacy of escitalopram in the treatment of premature ejaculation: a double-blind, placebo-controlled, fixed-dose, randomized study. J Clin Psychopharmacol. 2007;27(5):444–450.
- Saleh R, Nada E, Abu Al HM. The use of escitalopram in treatment of patients with premature ejaculation: a randomized, double-blind, placebo-controlled study. 2008;22(1):48–56. Egyptian Journal of Andrology and Reproduction.
- Arafa M, Shamloul R. A randomized study examining the effect of 3 SSRI on premature ejaculation using a validated questionnaire. Ther Clin Risk Manag. 2007;3(4):527–531.
- Cipriani A, La Ferla T, Furukawa TA, et al. Sertraline versus other antidepressive agents for depression. Cochrane Database Syst Rev. 2010;14(4):CD006117.
- Koe BK. Preclinical pharmacology of sertraline: a potent and specific inhibitor of serotonin reuptake. J Clin Psychiatry. 1990;51(Suppl B):13–17.
- Kim SW, Paick JS. Short-term analysis of the effects of as needed use of sertraline at 5 PM for the treatment of premature ejaculation. Urology. 1999;54(3):544–547.
- Arafa M, Shamloul R. Efficacy of sertraline hydrochloride in treatment of premature ejaculation: a placebo-controlled study using a validated questionnaire. Int J Impot Res. 2006;18(6):534–538.
- Xu G, Jiang HW, Fang J, et al. An improved dosage regimen of sertraline hydrochloride in the treatment for premature ejaculation: an 8-week, single-blind, randomized controlled study followed by a 4-week, open-label extension study. J Clin Pharm Ther. 2014;39(1):84–90.
- Heydorn WE. Paroxetine: a review of its pharmacology, pharmacokinetics and utility in the treatment of a variety of psychiatric disorders. Expert Opin Investig Drugs. 1999;8(4):417–441.
- Green B. Focus on paroxetine. Curr Med Res Opin. 2003;19(1):13–21.
- Waldinger MD, Hengeveld MW, Zwinderman AH. Ejaculation-retarding properties of paroxetine in patients with primary premature ejaculation: a double-blind, randomized, dose-response study. Br J Urol. 1997;79(4):592–595.
- McMahon CG, Touma K. Treatment of premature ejaculation with paroxetine hydrochloride. Int J Impot Res. 1999;11(5):241–246.
- Safarinejad MR. Comparison of dapoxetine versus paroxetine in patients with premature ejaculation: a double-blind, placebo-controlled, fixed-dose, randomized study. Clin Neuropharmacol. 2006;29(5):243–252.
- Alghobary M, El-Bayoumy Y, Mostafa Y, et al. Evaluation of tramadol on demand vs. daily paroxetine as a long-term treatment of lifelong premature ejaculation. J Sex Med. 2010;7(8):2860–2867.
- Kaplan HI, Sadock BJ. Psychiatric drug treatment. Baltimore: Williams and Wilkins Press; 1996.
- Waldinger MD, Hengeveld MW, Zwinderman AH, et al. Effect of SSRI antidepressants on ejaculation: a double-blind, randomized, placebo-controlled study with fluoxetine, fluvoxamine, paroxetine, and sertraline. J Clin Psychopharmacol. 1998;18(4):274–281.
- Dresser MJ, Desai D, Gidwani S, et al. Dapoxetine, a novel treatment for premature ejaculation, does not have pharmacokinetic interactions with phosphodiesterase-5 inhibitors. Int J Impot Res. 2006;18(1):104–110.
- Andersson KE, Mulhall JP, Wyllie MG. Pharmacokinetic and pharmacodynamic features of dapoxetine, a novel drug for ‘on-demand’ treatment of premature ejaculation. BJU Int. 2006;97(2):311–315.
- Buvat J, Tesfaye F, Rothman M, et al. Dapoxetine for the treatment of premature ejaculation: results from a randomized, double-blind, placebo-controlled phase 3 trial in 22 countries. Eur Urol. 2009;55(4):957–967.
- Kaufman JM, Rosen RC, Mudumbi RV, et al. Treatment benefit of dapoxetine for premature ejaculation: results from a placebo-controlled phase III trial. BJU Int. 2009;103(5):651–658.
- McMahon C, Kim SW, Park NC, et al. Treatment of premature ejaculation in the Asia-Pacific region: results from a phase III double-blind, parallel-group study of dapoxetine. J Sex Med. 2010;7(1 Pt 1):256–268.
- Pryor JL, Althof SE, Steidle C, et al. Efficacy and tolerability of dapoxetine in treatment of premature ejaculation: an integrated analysis of two double-blind, randomised controlled trials. Lancet. 2006;368(9539):929–937.
- McMahon CG. Dapoxetine: a new option in the medical management of premature ejaculation. Ther Adv Urol. 2012;4(5):233–251.
- Abu El-Hamd M, Abdelhamed A. Comparison of the clinical efficacy and safety of the on-demand use of paroxetine, dapoxetine, sildenafil and combined dapoxetine with sildenafil in treatment of patients with premature ejaculation: a randomised placebo-controlled clinical trial. Andrologia. 2018;50:1.
- Simsek A, Kirecci SL, Kucuktopcu O, et al. Comparison of paroxetine and dapoxetine, a novel selective serotonin reuptake inhibitor in the treatment of premature ejaculation. Asian J Androl. 2014;16(5):725–727.
- Roy K, Roy PP. QSAR of cytochrome inhibitors. Expert Opin Drug Metab Toxicol. 2009;5(10):1245–1266.
- Spina E, Santoro V, D’Arrigo C. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther. 2008;30(7):1206–1227.
- Vandel S, Bertschy G, Baumann P, et al. Fluvoxamine and fluoxetine: interaction studies with amitriptyline, clomipramine and neuroleptics in phenotyped patients. Pharmacol Res. 1995;31(6):347–353.
- Muller N, Brockmoller J, Roots I. Extremely long plasma half-life of amitriptyline in a woman with the cytochrome P450IID6 29/29-kilobase wild-type allele--a slowly reversible interaction with fluoxetine. Ther Drug Monit. 1991;13(6):533–536.
- Joos AA, Konig F, Frank UG, et al. Dose-dependent pharmacokinetic interaction of clozapine and paroxetine in an extensive metabolizer. Pharmacopsychiatry. 1997;30(6):266–270.
- Venkatakrishnan K, Obach RS. In vitro-in vivo extrapolation of CYP2D6 inactivation by paroxetine: prediction of nonstationary pharmacokinetics and drug interaction magnitude. Drug Metab Dispos. 2005;33(6):845–852.
- Fritze J, Unsorg B, Lanczik M. Interaction between carbamazepine and fluvoxamine. Acta Psychiatr Scand. 1991;84(6):583–584.
- Kasper S, Resinger E. Panic disorder: the place of benzodiazepines and selective serotonin reuptake inhibitors. Eur Neuropsychopharmacol. 2001;11(4):307–321.
- Volpi-Abadie J, Kaye AM, Kaye AD. Serotonin syndrome. Ochsner J. 2013;13(4):533–540.
- Hemeryck A, Belpaire FM. Selective serotonin reuptake inhibitors and cytochrome P-450 mediated drug-drug interactions: an update. Curr Drug Metab. 2002;3(1):13–37.
- Atikeler MK, Gecit I, Senol FA. Optimum usage of prilocaine-lidocaine cream in premature ejaculation. Andrologia. 2002;34(6):356–359.
- Sahin H, Bircan MK. Re: efficacy of prilocaine-lidocaine cream in the treatment of premature ejaculation. J Urol. 1996;156(5):1783–1784.
- Busato W, Galindo CC. Topical anaesthetic use for treating premature ejaculation: a double-blind, randomized, placebo-controlled study. BJU Int. 2004;93(7):1018–1021.
- Jannini EA, Simonelli C, Lenzi A. Disorders of ejaculation. J Endocrinol Invest. 2002;25(11):1006–1019.
- Atan A, Basar MM, Aydoganli L. Comparison of the efficacy of fluoxetine alone vs. fluoxetine plus local lidocaine ointment in the treatment of premature ejaculation. Arch Esp Urol. 2000;53(9):856–858.
- Choi HK, Jung GW, Moon KH, et al. Clinical study of SS-cream in patients with lifelong premature ejaculation. Urology. 2000;55(2):257–261.
- Choi HK, Xin ZC, Choi YD, et al. Safety and efficacy study with various doses of SS-cream in patients with premature ejaculation in a double-blind, randomized, placebo controlled clinical study. Int J Impot Res. 1999;11(5):261–264.
- Xin ZC, Choi YD, Lee WH, et al. Penile vibratory threshold changes with various doses of SS-cream in patients with primary premature ejaculation. Yonsei Med J. 2000;41(1):29–33.
- Dinsmore WW, Wyllie MG. PSD502 improves ejaculatory latency, control and sexual satisfaction when applied topically 5 min before intercourse in men with premature ejaculation: results of a phase III, multicentre, double-blind, placebo-controlled study. BJU Int. 2009;103(7):940–949.
- Dinsmore WW, Hackett G, Goldmeier D, et al. Topical eutectic mixture for premature ejaculation (TEMPE): a novel aerosol-delivery form of lidocaine-prilocaine for treating premature ejaculation. BJU Int. 2007;99(2):369–375.
- Gurkan L, Oommen M, Hellstrom WJ. Premature ejaculation: current and future treatments. Asian J Androl. 2008;10(1):102–109.
- Abdel-Hamid IA. Phosphodiesterase 5 inhibitors in rapid ejaculation: potential use and possible mechanisms of action. Drugs. 2004;64(1):13–26.
- Li X, Zhang SX, Cheng HM, et al. [Clinical study of sildenafil in the treatment of premature ejaculation complicated by erectile dysfunction]. Zhonghua Nan Ke Xue. 2003;9(4):266–269.
- McMahon CG, Stuckey BG, Andersen M, et al. Efficacy of sildenafil citrate (Viagra) in men with premature ejaculation. J Sex Med. 2005;2(3):368–375.
- Tang W, Ma L, Zhao L, et al. Clinical efficacy of Viagra with behavior therapy against premature ejaculation. Zhonghua Nan Ke Xue. 2004;10(5):366–267, 370.
- Salonia A, Maga T, Colombo R, et al. A prospective study comparing paroxetine alone versus paroxetine plus sildenafil in patients with premature ejaculation. J Urol. 2002;168(6):2486–2489.
- Chen J, Mabjeesh NJ, Matzkin H, et al. Efficacy of sildenafil as adjuvant therapy to selective serotonin reuptake inhibitor in alleviating premature ejaculation. Urology. 2003;61(1):197–200.
- Zhang XS, Wang YX, Huang XY, et al. Comparison between sildenafil plus sertraline and sertraline alone in the treatment of premature ejaculation. Zhonghua Nan Ke Xue. 2005;11(7):520–522, 525.
- Wang WF, Wang Y, Minhas S, et al. Can sildenafil treat primary premature ejaculation? A prospective clinical study. Int J Urol. 2007;14(4):331–335.
- Aversa A, Pili M, Francomano D, et al. Effects of vardenafil administration on intravaginal ejaculatory latency time in men with lifelong premature ejaculation. Int J Impot Res. 2009;21(4):221–227.
- Dell’Atti L, Galosi AB, Ippolito C. A randomized single-center study to compare the efficacy and tolerability of tadalafil once daily plus lidocaine anesthetic spray on premature ejaculation. Eur Rev Med Pharmacol Sci. 2017;21(5):1036–1040.
- Salem EA, Wilson SK, Bissada NK, et al. Tramadol HCL has promise in on-demand use to treat premature ejaculation. J Sex Med. 2008;5(1):188–193.
- Xiong GG, Wu FH, Chen SH, et al. [Safety and efficacy of tramadol hydrochloride with behavioral modification in the treatment of premature ejaculation]. Zhonghua Nan Ke Xue. 2011;17(6):538–541.
- Bar-Or D, Salottolo KM, Orlando A, et al. A randomized double-blind, placebo-controlled multicenter study to evaluate the efficacy and safety of two doses of the tramadol orally disintegrating tablet for the treatment of premature ejaculation within less than 2 minutes. Eur Urol. 2012;61(4):736–743.
- Palmer NR. Tramadol for premature ejaculation. J Sex Med. 2009;6(1):299.
- Kim JJ, Kwak TI, Jeon BG, et al. Effects of glans penis augmentation using hyaluronic acid gel for premature ejaculation. Int J Impot Res. 2004;16(6):547–551.
- Kwak C, Ku JH, Kim T, et al. Effect of subclinical prostatic inflammation on serum PSA levels in men with clinically undetectable prostate cancer. Urology. 2003;62(5):854–859.
- Moon DG. Is there a place for surgical treatment of premature ejaculation? Transl Androl Urol. 2016;5(4):502–507.
- Basal S, Goktas S, Ergin A, et al. A novel treatment modality in patients with premature ejaculation resistant to conventional methods: the neuromodulation of dorsal penile nerves by pulsed radiofrequency. J Androl. 2010;31(2):126–130.
- Gallo L, Perdona S, Gallo A. The role of short frenulum and the effects of frenulectomy on premature ejaculation. J Sex Med. 2010;7(3):1269–1276.
- Song B, Cai ZM. Possible function of the frenulum of prepuce in penile erection. Andrologia. 2012;44(1):23–25.
- Namavar MR, Robati B. Removal of foreskin remnants in circumcised adults for treatment of premature ejaculation. Urol Ann. 2011;3(2):87–92.
- Comhaire F, Vermeulen A. Plasma testosterone in patients with varicocele and sexual inadequacy. J Clin Endocrinol Metab. 1975;40(5):824–829.
- Lotti F, Corona G, Mancini M, et al. The association between varicocele, premature ejaculation and prostatitis symptoms: possible mechanisms. J Sex Med. 2009;6(10):2878–2887.
- Ahmed AF, Abdel-Aziz AS, Maarouf AM, et al. Impact of varicocelectomy on premature ejaculation in varicocele patients. Andrologia. 2015;47(3):276–281.
- Asadpour AA, Aslezare M, Nazari Adkani L. et al. The effects of varicocelectomy on the patients with premature ejaculation. Nephrourol Mon. 2014;6(3):e15991.
- Abu El‑Hamd M, Abdel Hameed FA. The Role of Varicocelectomy on Patients with Premature Ejaculation and Varicoceles. 2016;3(4):121–125. Journal of Integrative Nephrology and Andrology.
- Cavallini G. Alpha-1 blockade pharmacotherapy in primitive psychogenic premature ejaculation resistant to psychotherapy. Eur Urol. 1995;28(2):126–130.
- Sato Y, Otani T, Amano T, et al. Silodosin versus naftopidil in the treatment of premature ejaculation: a prospective multicenter trial. Int J Urol. 2017;24(8):626–631.
- Başar MM, Yilmaz E, Ferhat M, et al. Terazosin in the treatment of premature ejaculation: a short-term follow-up. Int Urol Nephrol. 2005;37(4):773–777.
- Mattson MP, Shea TB. Folate and homocysteine metabolism in neural plasticity and neurodegenerative disorders. Trends Neurosci. 2003;26(3):137–146.
- Taylor MJ, Carney S, Geddes J, et al. Folate for depressive disorders. Cochrane Database Syst Re. 2003(2):CD003390
- Brocardo PS, Budni J, Kaster MP, et al. Folic acid administration produces an antidepressant-like effect in mice: evidence for the involvement of the serotonergic and noradrenergic systems. Neuropharmacology. 2008;54(2):464–473.
- Botez MI, Young SN, Bachevalier J, et al. Folate deficiency and decreased brain 5-hydroxytryptamine synthesis in man and rat. Nature. 1979;278(5700):182–183.
- Botez MI, Young SN, Bachevalier J, et al. Effect of folic acid and vitamin B12 deficiencies on 5-hydroxyindoleacetic acid in human cerebrospinal fluid. Ann Neurol. 1982;12(5):479–484.
- Saadat SH, Ahmadi K, Panahi Y. The effect of on-demand caffeine consumption on treating patients with premature ejaculation: a double-blind randomized clinical trial. Curr Pharm Biotechnol. 2015;16(3):281–287.
- Fisone G, Borgkvist A, Usiello A. Caffeine as a psychomotor stimulant: mechanism of action. Cell Mol Life Sci. 2004;61(7–8):857–872.
- Serefoglu EC, Hawley WR, Lasker GF, et al. Effect of botulinum-A toxin injection into bulbospongiosus muscle on ejaculation latency in male rats. J Sex Med. 2014;11(7):1657–1663.
- Serefoglu EC, Silay MS. Botulinum toxin-A injection may be beneficial in the treatment of life-long premature ejaculation. Med Hypotheses. 2010;74(1):83–84.
- Choi JB, Kang SH, Lee DH, et al. Efficacy and safety of on demand clomipramine for the treatment of premature ejaculation: a multicenter, randomized, double-blind, phase III clinical trial. J Urol. 2019;201(1):147–152.
- Abdel-Hamid IA, El Naggar EA, El Gilany AH. Assessment of as needed use of pharmacotherapy and the pause-squeeze technique in premature ejaculation. Int J Impot Res. 2001;13(1):41–45.
- Siroosbakht S, Rezakhaniha S, Rezakhaniha B. Which of available selective serotonin reuptake inhibitors (SSRIs) is more effective in treatment of premature ejaculation? A randomized clinical trial. Int Braz J Urol. 2019;45(6):1209–1215.
- Kim SC, Seo KK. Efficacy and safety of fluoxetine, sertraline and clomipramine in patients with premature ejaculation: a double-blind, placebo controlled study. J Urol. 1998;159(2):425–427.
- Mathers MJ, Klotz T, Roth S, et al. Safety and efficacy of vardenafil versus sertraline in the treatment of premature ejaculation: a randomised, prospective and crossover study. Andrologia. 2009;41(3):169–175.
- Mendels J, Camera A, Sikes C. Sertraline treatment for premature ejaculation. J Clin Psychopharmacol. 1995;15(5):341–346.
- Murat Başar M, Atan A, Yildiz M, et al. Comparison of sertraline to fluoxetine with regard to their efficacy and side effects in the treatment of premature ejaculation. Arch Esp Urol. 1999;52(9):1008–1011.
- Balbay MD, Yildiz M, Salvarci A, et al. Treatment of premature ejaculation with sertralin. Int Urol Nephrol. 1998;30(1):81–83.
- Polat EC, Ozbek E, Otunctemur A, et al. Combination therapy with selective serotonin reuptake inhibitors and phosphodiesterase-5 inhibitors in the treatment of premature ejaculation. Andrologia. 2015;47(5):487–492.
- McMahon CG, Giuliano F, Dean J, et al. Efficacy and safety of dapoxetine in men with premature ejaculation and concomitant erectile dysfunction treated with a phosphodiesterase type 5 inhibitor: randomized, placebo-controlled, phase III study. J Sex Med. 2013;10(9):2312–2325.
- Tuken M, Culha MG, Serefoglu EC. Efficacy and safety of dapoxetine/sildenafil combination tablets in the treatment of men with premature ejaculation and concomitant erectile dysfunction-DAP-SPEED Study. Int J Impot Res. 2019;31(2):92–96.
- Peng J, Fang D, Li H, et al. Efficacy of dapoxetine treatment in Chinese patients with premature ejaculation and possible factors affecting efficacy in the real-world practice. BMC Urol. 2020;20(1):11.
- Altamura AC, Moro AR, Percudani M. Clinical pharmacokinetics of fluoxetine. Clin Pharmacokinet. 1994;26(3):201–214.
- Mandrioli R, Forti GC, Raggi MA. Fluoxetine metabolism and pharmacological interactions: the role of cytochrome p450. Curr Drug Metab. 2006;7(2):127–133.
- Bejerot S, Bodlund O. Response to high doses of citalopram in treatment-resistant obsessive-compulsive disorder. Acta Psychiatr Scand. 1998;98(5):423–424.
- Baldessarini RJ. Current status of antidepressants: clinical pharmacology and therapy. J Clin Psychiatry. 1989;50(4):117–126.
- Sanchez C, Bergqvist PB, Brennum LT, et al. Escitalopram, the S-(+)-enantiomer of citalopram, is a selective serotonin reuptake inhibitor with potent effects in animal models predictive of antidepressant and anxiolytic activities. Psychopharmacol (Berl). 2003;167(4):353–362.
- Hyttel J, Bogeso KP, Perregaard J, et al. The pharmacological effect of citalopram residues in the (S)-(+)-enantiomer. J Neural Transm Gen Sect. 1992;88(2):157–160.
- Jiang K, Li L, Wang X, et al. Efficacy and tolerability of escitalopram in treatment of major depressive disorder with anxiety symptoms: a 24-week, open-label, prospective study in Chinese population. Neuropsychiatr Dis Treat. 2017;13:515–526.
- Aronson S, Delgado P. Escitalopram. Drugs Today (Barc). 2004;40(2):121–131.
- van Harten J. Clinical pharmacokinetics of selective serotonin reuptake inhibitors. Clin Pharmacokinet. 1993;24(3):203–220.
- De Jonghe F, Swinkels J, Tuyaman Qua H. Randomized double-blind study of fluoxamine and maprotiline in treatment of depression. Pharmacopsychiatry. 1991;24:21–23.
- McMahon CG. Efficacy of dapoxetine in the treatment of premature ejaculation. Clin Med Insights Reprod Health. 2011;5:25–39.