ABSTRACT
Objective
To review the role of elastography in the evaluation and decision-making of adult, infertile men with varicocele.
Methods
A systematic search using the terms (Elastography) AND (Varicocele), (Stiffness) AND (Varicocele), (Elastography) AND (Male infertility) was performed in Pubmed/Medline. Studies reporting a) elastographic characteristics in varicocele-bearing comparing to normal testicles, and b) the correlation of elastography with varicocele grading, parameters of spermatogenesis, and outcomes of varicocele treatment were selected. Exclusion criteria were animal, adolescents, abstracts, and non-English language studies.
Results
In total, 453 articles were identified; 11 eligible studies were selected. Several modalities were used (shear wave elastography, strain elastography, quasistatic ultrasound elastography, acoustic radiation force impulse). Varicocele-bearing testicles have significantly different stiffness and elasticity in comparison to normal and non-varicocele testicles. Although not in full agreement, elastography readings are correlated with semen parameters. Conflicting results were reported regarding grading as most of the studies failed to demonstrate a significant correlation. Shear wave elastography showed a significant correlation with the improvement in semen parameters after varicocelectomy, but the association with pregnancy rates is unknown. Finally, no studies were identified comparing elastography with other modalities.
Conclusions
Elastography can detect changes in the architecture of varicocele-bearing testicles. Although the role of the modality in grading is uncertain, elastography showed a meaningful correlation with spermatogenesis parameters. Importantly, elastography readings could predict the improvement in semen parameters after varicocelectomy which is useful in terms of decision-making in infertile men with varicocele.
Abbreviations
ARFI: acoustic radiation force impulse; CDUS: colour Doppler ultrasonography; DWI: diffusion-weighted imaging; PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses; SWE: shear wave elastography; VC: varicocele
Introduction
Varicocele (VC) is defined as the ‘abnormal dilatation of the pampiniform plexus in the spermatic cord’. A clinical VC can be seen in 15% of the normal male population, while it might be involved in up to 40% and 80% of primary and secondary infertility patients, respectively [Citation1]. Pathophysiologically, VC alters the blood flow in the testes provoking a cascade of oxidative stress phenomena that can finally result in testicular damage and possible subfertility [Citation2].
Although the co-existence of infertility and VC is considered a strong indication for treatment, not all patients will enjoy fatherhood after intervention [Citation3]. This highlights the necessity of proper patients’ selection and modern practice has explored the role of various imaging modalities for the optimal management of VC. Grey-scale and conventional colour Doppler ultrasonography (CDUS) facilitate the diagnosis, whereas they contribute partially to the evaluation of the effect on spermatogenesis and the outcome of treatments, utilising parameters such as the vein size, the type of reflux and the intratesticular haemodynamics [Citation4–6]. Other novel modalities such as MRI and multiparametric CDUS appear more promising as they can evaluate the degree of testicular interstitial fibrosis and architecture, which is can reflect the possible damage caused by the VC [Citation7]. However, the interpretation of the US findings has not been standardised, whereas the modality is not fully decisive in the decision-making. Moreover, although MRI looks promising and offers an objective evaluation of the testicular parenchyma, the greater limitation lies in the cost, availability and experience of the operator.
Ultrasonic elastography is a novel ultrasonic modality which has been previously used in male infertility and for the investigation of scrotal and prostate pathologies [Citation8–10]. There are two basic elastography approaches. Strain elastography measures the longitudinal tissue displacement before and after compression, usually by manual manipulation of the ultrasound transducer, providing an indication of relative stiffness of an area of interest compared to its surroundings. Using shear wave elastography (SWE), shear waves are generated by repetitive compression produced by high-intensity pulses from the ultrasound transducer, which allows a more quantitative estimate of tissue stiffness [Citation11]. Early elastography results in patients with VC have shown a significant correlation between testicular elasticity and grade in infertile men with dyspermia, broadening the potential of the modality in these patients [Citation12]. Elastography could be able to combine an affordable cost along with increased objectivity, allowing reproducibility in the interpretation of the findings and facilitating the patients’ selection for treatment.
To the best of our knowledge, no previous cumulative data have been presented regarding the role of the modality in men with VC. In the present literature review, we investigated the role and usefulness of elastography in the evaluation and management of adult men with VC.
Methods
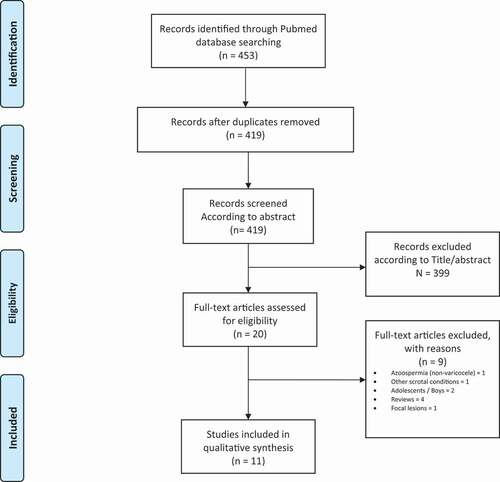
A systematic search according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines was performed on PubMed/MEDLINE [Citation13]. No time limitations or type of studies (prospective, retrospective) were applied. We used the terms (Elastography) AND (Varicocele), (Stiffness) AND (Varicocele), (Elastography) AND (Male infertility), and an advanced search using the terms (ultrasound [Title/Abstract]) AND (varicocele [Title/Abstract]) was performed searching for additional results. Inclusion criteria were studies reporting observations on and application of elastography in adult men with VC. Exclusion criteria were studies on animals, adolescents, abstracts, and non-English language studies. The studies were selected based on the follow criteria: a) reports on stiffness characteristics in testicles with VC, b) the correlation of elastography with VC grading (clinical or sonographic), c) the correlation of elastography with parameters of spermatogenesis (hormones, semen parameters, testicular volume, or pregnancy rates), and d) the role of elastography as predictor of VC treatment (improvement in semen parameters or pregnancy rates). Our strategy search is illustrated in . The data extracted included: publication year, age, number of participants, indication, modality used, study design, fertility status, aim and primary and secondary outcomes of the studies relevant to our principal scientific question.
Results
The search engine provided 453 articles for evaluation. After the removal of duplicates, 419 articles were screened through Title/Abstract and 20 full-text articles were examined for their eligibility. Finally, 11 articles were identified meeting the search criteria. All trials were prospective, whereas no studies were identified comparing or correlating elastography with other modalities. The characteristics of the studies are presented in [Citation8,Citation12,Citation14–22]. In we present and comment on the studies related to our scientific questions.
Table 1. Studies characteristics
Table 2. Elastography values in men with VC
Table 3. Correlation with parameters of spermatogenesis
Table 4. Correlation with grade
Table 5. Prediction of treatment outcome
Testicular stiffness in VC- in comparison to non-VC-bearing testicles and normal controls
In a study using acoustic radiation force impulse (ARFI) elastography, the authors found that all elastography measurements (upper, middle, lower pole and mean readings) were significantly lower in the VC-bearing testicles (oligospermic men with various grades of clinical VC) in comparison to the left testicles of normospermic men with no VC [Citation12]. The testicular stiffness measure with SWE of the VC-bearing testicles in infertile men with unilateral clinical or subclinical VC and oligo-astheno-teratozoospermia (OAT) was found to be significantly lower in comparison to fertile men and normal testes [Citation14]. Turna and Aybar [Citation15] found that VC testicles were stiffer in comparison to the contralateral normal ones in patients who were normospermic or oligospermic, whereas testicles with VC were stiffer in comparison to testicles of normal controls regardless of dyspermia; on the other hand, there was no difference in stiffness between the right and left testicles of normal controls. Higher SWE values in VC-bearing testicles in comparison to the contralateral normal ones were also seen in a recent study but the fertility status of the participants was not documented [Citation16]. Finally, a recent prospective study of men with Grade III VC and worsening semen parameters reported significantly higher SWE values in the left testicles carrying VC in comparison to the right side [Citation17].
Using real-time strain elastography, Salama et al. [Citation18] reported a significantly higher strain ratio and elasticity scores in infertile men with VC in comparison to normal controls, whereas in a second study, the left testicle strain ratio median value was found to be significantly lower in oligospermic men in comparison to a normal group [Citation19]. In a study by Küçükdurmaz et al. [Citation8], dyspermic men including men with VC had different strain ratio readings in comparison to controls but the authors after sub-analysis concluded that the presence of VC did not have effect on elastography findings. Finally, in men being evaluated with strain elastography for various scrotal pathology, elastograms between VC-bearing testicles and normal controls were similar and the strain ratios were not significantly different [Citation20].
Correlation of stiffness with markers of spermatogenesis
The landmark study of Dede et al. [Citation12] showed a significant negative correlation between FSH and elasticity, which might directly reflect the subsequent testicular impairment. Although in the same study there was no correlation between elastography and semen parameters. Using strain elastography, a study showed no correlation with FSH in infertile men with VC (with dyspermia or normospermia), although the trial showed significant correlations of strain values with total motile sperm count and sperm morphology in infertile men with dyspermia (including men with VC) [Citation8]. In another study, no significant relationship between the left testicular strain ratio and the seminal parameters, hormonal values and the left testicular volume was found in oligospermic infertile men with VC [Citation19]. Finally, Salama et al. [Citation18] reported that the strain ratio and elasticity scores showed a significant negative correlation with sperm morphology, whereas the elasticity score showed a significant negative correlation with testicular volume.
The use of SWE has also shown significant correlations with parameters of spermatogenesis. In 100 men with various degrees of dyspermia (azoospermia, oligospermia, decreased motility and agglutination, complete normospermia) including 36 patients with VC, the mean shear wave velocity values showed strong negative correlations with the mean testicular volume and sperm count [Citation21]. Erdogan et al. [Citation16] noted a significant difference in testicular volume between VC-bearing testicles, contralateral normal testicles, and controls, but no correlation between SWE readings and testicular volume. The authors mentioned that ‘testicular volume is not a reliable parameter for reflecting the degree of parenchymal damage’, but there was no correlation with histopathological findings where the participants were not mentioned to be infertile. Finally, in a study including oligospermic and normospermic men with VC, testicular volume was also lower on the side with VC in comparison to the contralateral normal ones (irrespective of oligospermia or not), but no significant correlation was observed between SWE stiffness and the volume of the testes [Citation15].
Correlation of stiffness with VC grade
While some studies report a significant correlation of elastography with VC grades, others found no merit. The discrepancies might be related to the modality used, the stage of VC development or the grading system (clinical vs sonographic).
In the study by Dede et al. [Citation12], a significant negative correlation was found between elastography readings and grade, which in practical terms means that the when grade increases, the elasticity decreases. Another study using strain elastography assessed the relationship between clinical grading and VC. The authors found significant differences between the different grades of VC and the elastographic parameters, whereas VC grade showed a significant positive correlation with both the strain ratio and elasticity score [Citation18].
On the other hand, a study found no correlation between the sonographic grade (classified according to the Sarteschi system) and SWE readings in 36 infertile patients with Grade I–III VC [Citation21]. Using the same modality, no correlation was found between clinical grade and SWE readings in a study of 58 men with VC (normospermic and oligospermic) [Citation15]. Finally, in a similar population of patients, a study stated no correlation between grade and strain elastography readings. In this study, the sample was rather small as 23 men with VC and fertility issues were included; 11 men had normal semen analysis whereas 12 men were dyspermic [Citation8].
Pre- and postoperative elastography as predictor of treatment outcome
Two prospective studies have reported the utility of testicular stiffness relating to outcome after surgical intervention.
The first trial included 48 men with a mean age of 30.9 years, with unilateral clinical VC and mean duration of infertility of 3 years. Using testicular SWE, the authors found that a mean cut-off value of 4.5 kPa predicted efficiently the improvement in semen parameters after microsurgical varicocelectomy. The aforesaid cut-off had a sensitivity of 86.4% and a specificity of 84.2%, and a statistically significant negative correlation between the stiffness index and improvement in sperm count and total motility was found [Citation22].
A second study included 82 men with a mean age of 27.44 years and Grade III–IV VC (according to the Sarteschi system) who had significant deterioration in their semen analysis during follow-up. After a laparoscopic transperitoneal varicocelectomy, the authors noticed that the left testicular volume increased whereas the left SWE decreased, and both parameters showed significant differences compared to baseline. Moreover, a significant positive correlation between the difference of pre- and postoperative left SWE and testicular volume was found. Also, a significant negative correlation between postoperative SWE of left testis and ipsilateral testicular volume and sperm count at 3 months was observed [Citation17].
Discussion
In summary, elastography was found to be able to differentiate between VC-bearing testicles and the normal ones in most cases. The finding implies that elastography might be able to detect the effect of VC on the testicular parenchyma assisting the physical examination and when assessing the eutrophic or atrophic status of the testicles. Regarding the association of elastography with grading though, reports have been conflicting and it cannot be supported that the modality could replace clinical grading. Although some parameters of spermatogenesis were correlated significantly with some elastography features, the most promising findings were observed regarding the association of SWE and the outcomes of treatment. The evidence that elastography could predict the improvement in semen parameters is significant and it might help the clinician when the most cost-effective modality for the management of infertile men with VC is sought.
Specifically, elastography was reported as a marker of underlying architecture or atrophy and is considered more informative than palpation [Citation12]. When using elastography in infertile men, a clinical correlation with the current clinical context is mandatory though. For example, in their study, Rocher et al. [Citation14] included infertile men with VC and OAT, and reported lower SWE in comparison to controls but no significant difference with the contralateral testis. In contrast, other authors found that the VC testicles were stiffer compared to the contralateral normal testicles regardless of the presence of dyspermia [Citation15]. The discrepancy in the above findings is explicable considering that infertile men with severe damage to spermatogenesis and semen abnormalities may have similar histological changes in both testicles extending up to the degree of testicular failure. Similarly, two studies using strain elastography reported inverse elasticity readings in VC testicles in comparison to controls [Citation18,Citation19]. If infertility is absent, no difference might be found between VC-bearing and normal testicles as reported in one study [Citation20]. Thus, the clinical context has to be considered; discrepancies due to the modality used, and the experience of the operator need to be considered prior to selection of the optimal modality.
For a correlation with spermatogenesis parameters, elastography readings have been shown to be correlated with testicular volume, FSH and semen parameters. In a group of men with dyspermia including men with VC, an inverse relationship between strain values and total motile sperm count has been reported [Citation8]. Total motile sperm count is considered a reliable marker of pregnancy rates and the findings sound meaningful [Citation23]. Whether all these correlations are useful though is uncertain, as in practice, when male infertility has been diagnosed and VC has been implied as the cause, clinical rather than radiological criteria will guide the management [Citation24]. However, elastography might be useful when evaluating newly diagnosed men with VC or post-pubertal, young men not desiring fatherhood at the time of diagnosis. Although the specificity and the sensitivity of the modality must be clarified, the proper use of elastography by experienced radiologists also carries merit when surveillance rather than intervention has been decided. In adolescents, the significant correlations between elastography and testicular volume might assist with the indication for treatment, although the modality does not seem to alter dramatically other traditional clinical criteria used for intervention [Citation25,Citation26].
The clinical classification by Dubin and Amelar remains the cornerstone of diagnosis, but the main drawback is the lack of predictive significance [Citation27]. Therefore, although elastography has shown correlation with clinical grade [Citation12,Citation18], we consider that the practical merit of the correlation of imaging characteristics with clinical grading is uncertain, unless the former ones contribute to the assessment of the severity of the condition relating to spermatogenesis. CDUS systems based on vein size, duration of reflux and testicular volume are useful for the diagnosis and can stratify VCs [Citation4,Citation28–30], whereas individual parameters such as reflux might also draw useful conclusions [Citation31,Citation32]. Multiparametric MRI using dynamic contrast-enhanced MRI, diffusion-weighted imaging (DWI) and MR spectroscopy have been proposed for the stratification of testicular damage induced by the VC, as a significant correlation has been shown between the apparent diffusion coefficient and venous diameter on one hand, and DWI and testicular damage on the other hand [Citation33]. Ultrasound testicular contrast harmonic imaging is also as an adjunctive tool for the assessment of spermatogenesis in VC-bearing testicles [Citation34]. In a similar manner, regardless of the direct association with clinical grading, elastography should be considered useful due to the correlation with parameters of spermatogenesis. This can extend to the assessment of mild or subclinical forms of VC where the data are still conflicting and not supporting an invasive approach except in a select group of patients [Citation35,Citation36].
In terms of treatment outcomes, SWE readings were found to be predictive of the improvement in sperm parameters. Yet, relevant studies did not assess the pregnancy rates after treatment or define semen deterioration as an indication for treatment, which does not necessarily imply infertility. However, elastography might be an adjunctive tool predicting which patients might benefit from meaningful improvements in their semen quality. The latter is important in men undergoing varicocelectomy followed by assisted reproduction techniques [Citation37]. Whether elastography would save unnecessary treatments though remains uncertain. To date, the indications for VC correction are mainly dictated by clinical parameters and varicocelectomy has been proven to be cost-effective if assisted reproduction techniques are to be followed, or even in azoospermic patients [Citation38]. Thus, elastography might not be as decisive and the clinical context will guide the management. However, Fuschi et al. [Citation17] reported that the histopathological reversal of testicular architecture follows the shift in SWE readings, which implies that elastography could document the recovery of spermatogenesis and the success of treatment. Moreover, this might give new insights in unexplored fields, such as bilateral subclinical VCs, where there is no clinical tool apart from a testicular biopsy to assist in the prognosis of men undergoing surgery [Citation39]. Furthermore, elastography could identify sites of healthy testicular tissue and facilitate testicular tissue extraction in men warranting invasive approaches for their fertility treatment, with or without varicocelectomy.
Our present review has some potential limitations that should be appreciated. First, although we attempted to provide a systematic review on the topic, due to the different modalities used and the heterogeneity of the studies, we did not attempt to provide a summary of evidence or recommendations. Similarly, we did not examine the bias accompanying the studies, considering that elastography should be considered experimental in patients with VC and principal issues, e.g. the cost-effectiveness or the reproducibility of the modality, are still under evaluation. However, we have presented our relevant comments in the tables. Finally, considering that the data were not eligible for synthesis of the results, we considered it inappropriate to perform a meta-analysis; therefore, we decided to present our results in a narrative manner.
Conclusions
Varicocele seems to alter the histological architecture of the affected testicles and this phenomenon can be detected as a change in stiffness by elastography. These differences might be attributed to underlying fibrosis or atrophy. As elastography has also shown a meaningful correlation with spermatogenesis parameters, this modality could provide an in-depth assessment of the severity of VC. In infertile men who are candidates for treatment, elastography could predict the improvement in semen parameters. However, the exact merit of elastography to date remains uncertain as clinical indications still come first when dealing with VCs in infertile men. Further research should clarify the exact role of elastography in the evaluation and management of infertile men with VC.
Disclosure Statement
No potential conflict of interest was reported by the authors.
References
- Alsaikhan B, Alrabeeah K, Delouya G, et al. Epidemiology of varicocele. Asian J Androl. 2016;18(2):179–181.
- Valentino M, Bertolotto M, Derchi L, et al. Children and adults varicocele: diagnostic issues and therapeutical strategies. J Ultrasound. 2014;17(3):185–193.
- Yuan R, Zhuo H, Cao D, et al. Efficacy and safety of varicocelectomies: a meta-analysis. Syst Biol Reprod Med. 2017;63(2):120–129.
- Chiou RK, Anderson JC, Wobig RK, et al. Color doppler ultrasound criteria to diagnose varicoceles: correlation of a new scoring system with physical examination. Urology. 1997;50(6):953–956.
- Alshehri FM, Akbar MH, Altwairgi AK, et al. Preoperative duplex ultrasound parameters predicting male fertility after successful varicocelectomy. Saudi Med J. 2015 Dec;36(12):1439–1445.
- Tarhan S, Ucer O, Sahin MO, et al. Long-term effect of microsurgical inguinal varicocelectomy on testicular blood flow. J Androl. 2011;32(1):33–39.
- Tsili AC, Xiropotamou ON, Sylakos A, et al. Potential role of imaging in assessing harmful effects on spermatogenesis in adult testes with varicocele. World J Radiol. 2017;9(2):34–45.
- Küçükdurmaz F, Sarıca MA, Emre Ö, et al. Evaluation of the diagnostic efficacy of strain elastography in infertile population with normal and abnormal semen parameters. Turkish J Urol. 2017 Sep;43(3):261–267.
- Roy C, de Marini P, Labani A, et al. Shear-wave elastography of the testicle: potential role of the stiffness value in various common testicular diseases. Clin Radiol. 2020 Jul;75(7):560.e9–560.e17.
- Mannaerts CK, Wildeboer RR, Postema AW, et al. Multiparametric ultrasound: evaluation of greyscale, shear wave elastography and contrast-enhanced ultrasound for prostate cancer detection and localization in correlation to radical prostatectomy specimens. BMC Urology. 2018 Nov;18(1):98.
- Garra BS. Elastography: history, principles, and technique comparison. Abdom Imaging. 2015 Apr;40(4):680–697.
- Dede O, Teke M, Daggulli M, et al. Elastography to assess the effect of varicoceles on testes: a prospective controlled study. Andrologia. 2016 Apr;48(3):257–261.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7). DOI:https://doi.org/10.1371/journal.pmed.1000100
- Rocher L, Criton A, Gennisson J-L, et al. Testicular shear wave elastography in normal and infertile men: a prospective study on 601 patients. Ultrasound Med Biol. 2017 Apr;43(4):782–789.
- Turna O, Aybar MD. Testicular stiffness in varicocele: evaluation with shear wave elastography. Ultrasonography. 2020 Mar;39(4):350–355.
- Erdogan H, Durmaz MS, Arslan S, et al. Shear wave elastography evaluation of testes in patients with varicocele. Ultrasound Quarterly. 2020 Mar;36(1):64–68.
- Fuschi A, Capone L, Abuorouq S, et al. Shear wave elastography in varicocele patients: prospective study to investigate correlation with semen parameters and histological findings. Int J Clin Pract. 2020 Sep;e13699. Ahead of Print. DOI:https://doi.org/10.1111/ijcp.13699
- Salama N, Samir M, Blgozah S. Evaluation of normal and varicocele-bearing testes using real-time strain elastography. J Ultrasound Med off J Am Inst Ultrasound Med. 2019 Mar;38(3):621–627.
- Bitkin A, Başak Ozbalci A, Aydin M, et al. Effects of varicocele on testicles: value of strain elastography: a prospective controlled study. Andrologia. 2019 Feb;51(1):e13161.
- Zeng B, Chen F, Qiu S, et al. Application of quasistatic ultrasound elastography for examination of scrotal lesions. J Ultrasound Med Off J Am Inst Ultrasound Med. 2016 Feb;35(2):253–261.
- Yavuz A, Yokus A, Taken K, et al. Reliability of testicular stiffness quantification using shear wave elastography in predicting male fertility: a preliminary prospective study. Med Ultrason. 2018 May;20(2):141–147.
- Abdelwahab K, Eliwa AM, Seleem MM, et al. Role of preoperative testicular shear wave elastography in predicting improvement of semen parameters after varicocelectomy for male patients with primary infertility. Urology. 2017 Sep;107:103–106.
- Hamilton JAM, Cissen M, Brandes M, et al. Total motile sperm count: a better indicator for the severity of male factor infertility than the WHO sperm classification system. Hum Rep. 2015 May;30(5):1110–1121.
- Shridharani A, Owen RC, Elkelany OO, et al. The significance of clinical practice guidelines on adult varicocele detection and management. Asian J Androl. 2016;18(2):269–275.
- Camoglio FS, Bruno C, Peretti M, et al. The role of sonoelastography in the evaluation of testes with varicocele. Urology. 2017 Feb;100:203–206.
- Jedrzejewski G, Osemlak P, Wieczorek AP, et al. Prognostic values of shear wave elastography in adolescent boys with varicocele. J Pediatr Urol. 2019 May;15(3):223.e1–223.e5.
- Belay R, Huang G, Shen J-C, et al. Diagnosis of clinical and subclinical varicocele: how has it evolved? Asian J Androl. 2016;18(2):182.
- Pilatz A, Altinkilic B, Köhler E, et al. Color Doppler ultrasound imaging in varicoceles: is the venous diameter sufficient for predicting clinical and subclinical varicocele World J Urol. 2011;29(5):645–650.
- Liguori G, Trombetta C, Garaffa G, et al. Color Doppler ultrasound investigation of varicocele. World J Urol. 2004;22(5):378–381.
- Hirsh AV, Cameron KM, Tyler JP, et al. The Doppler assessment of varicoceles and internal spermatic vein reflux in infertile men. Br J Urol. 1980 Feb;52(1):50–56.
- Grasso M, Lania C, Castelli M, et al. Low-grade left varicocele in patients over 30 years old: the effect of spermatic vein ligation on fertility. BJU Int. 2000;85(3):305–307.
- Donkol RH, Salem T. Paternity after varicocelectomy: preoperative sonographic parameters of success. J Ultrasound Med. 2007 May;26(5):593–599.
- Karakas E, Karakas O, Cullu N, et al. Diffusion-weighted MRI of the testes in patients with varicocele: a preliminary study. AJR Am J Roentgenol. 2014 Feb;202(2):324–328.
- Caretta N, Palego P, Schipilliti M, et al. Testicular contrast harmonic imaging to evaluate intratesticular perfusion alterations in patients with varicocele. J Urol. 2010 Jan;183(1):263–269.
- Kohn TP, Ohlander SJ, Jacob JS, et al. The effect of subclinical varicocele on pregnancy rates and semen parameters: a systematic review and meta-analysis. Curr Urol Rep. 2018;19(7):1–10.
- Sun X, Yun W, Tao G, et al. Bilateral is superior to unilateral varicocelectomy in infertile males with left clinical and right subclinical varicocele : a prospective randomized controlled study. Int Urol Nephrol. 2018;50(2):205–210.
- Thirumavalavan N, Scovell JM, Balasubramanian A, et al. Subclinical and clinical varicoceles on total motile sperm count : is there a. Urology. 2018;1–5. DOI:https://doi.org/10.1016/j.urology.2018.06.036
- Yan S, Shabbir M, Yap T, et al. Should the current guidelines for the treatment of varicoceles in infertile men be re-evaluated? Hum Fertil. 2019;24:1–15.
- Teixeira TA, Pariz JR, Dutra RT, et al. Cut-off values of the Johnsen score and Copenhagen index as histopathological prognostic factors for postoperative semen quality in selected infertile patients undergoing microsurgical correction of bilateral subclinical varicocele. Transl Androl Urol. 2019 Aug;8(4):346–355.