ABSTRACT
Background
Benign prostatic hyperplasia is the most common cause of urinary retention in men (BPH). The gold standard surgical treatment is transurethral resection of the prostate (TURP). However, due to the morbidity and mortality associated with TURP, more minimally invasive treatments, such as vaporizing the prostate with the Rezum system, have been introduced. We investigated the efficacy of Rezum in the treatment of refractory urinary retention due to BPH in this review.
Methodology and materials
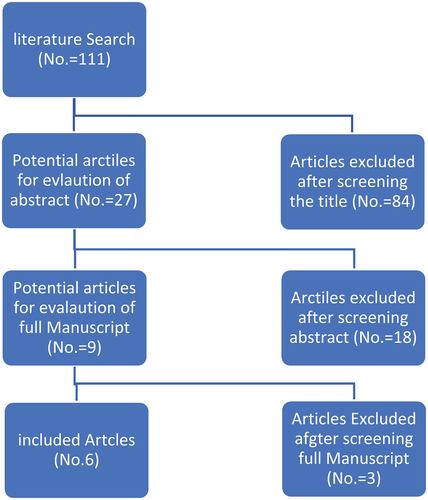
To conduct this review, the Cochrane methodology for systematic reviews was used. All studies that used Rezum to treat catheter-dependent patients with enlarged prostates were included. The literature search showed 111 studies, 84 of which were excluded due to non-relevance based on titles and 18 due to lack of relevance based on abstract review. Full manuscripts were reviewed in nine studies, three of which were excluded because they did not meet the inclusion criteria.
Results
This review included 301 patients in total. The rate of a successful trial of voiding post Rezum therapy was 85%. The complication rated between 3.8 and 4.3% all of which were mild and self-limited. As there was no major complication of Rezum (clavien dindo >2), the procedure-related morbidity is negligible.
Conclusion
In this review, Rezum was found to be an efficacious and safe alternative in the treatment of refractory retention with mild complications and minimal morbidity.
Introduction
Benign prostatic hyperplasia (BPH) is the most common cause of voiding and lower urinary tract symptoms in men, particularly in men over the age of 60 [Citation1,Citation2]. Patients who present with urinary retention are initially fitted with a urethral catheter and start medical treatment, principally alpha blockers, followed by a voiding trial; failure to void despite medical treatment is considered refractory retention, which is an absolute indication for surgical intervention in the management of BPH [Citation3].
The gold standard surgical treatment for BPH remains transurethral resection of the prostate (TURP) [Citation4]. However, morbidity and mortality of TURP along with the effects on sexual function and infertility necessitated the development of a more minimal invasive intervention such as Aquablation, Prostatic urethral lift (Urolift), and Rezum systems [Citation5–7].
The Rezum System ablates prostatic tissue using convective water vapor energy and can be performed as an office-based procedure with local anaesthesia and oral analgesia to avoid the morbidities associated with general or even spinal anaesthesia required in TURP. The efficacy and safety of Rezum system have been reported in multiple prospective and retrospective studies as efficacy was associated with low rate of shortlived mild side effects [Citation8–10]. Due to its low complication profile and efficacy, Rezum is a promising intervention for BPH, especially in patients with multiple comorbidities who cannot tolerate TURP or in patients who are concerned about fertility and sexual function complication of TURP.
Several studies looked into the effectiveness of Rezum in treating lower urinary tract symptoms caused by BPH, but the role of Rezum in the treatment of refractory retention remains uncertain. In this review, we evaluated the efficacy of Rezum in treating patients with refractory urinary retention due to benign prostate hyperplasia as an alternative to TURP.
Methodology and materials
Search strategy
To conduct this review, the Cochrane methodology for systematic reviews was used [Citation11,Citation12]. The risk of bias within each study was assessed using the ROBINSI tool to ensure the validity and reliability of the retrospective studies included in this paper [Citation13]. Google Scholar, the US National Library of Medicine’s life science database (MEDLINE), and individual recognized urology journals were used in the search strategy. ‘Rezum’ and ‘urinary retention’ were two search terms that were used together. (Rezum[All Fields] AND (‘urinary retention’[MeSH Terms] OR (‘urinary’[All Fields] AND ‘retention’[All Fields]) OR ‘urinary retention’[All Fields]) AND (‘2016/1/1’[PubDate]: ‘3000’[PubDate]) AND (‘2016/1/1’[PubDate]: ‘3000’[PubDate]).
Study selection and data extraction
We included all studies that reported on the use of Rezum in the treatment of enlarged prostate patients with chronic retention and catheter-dependent patients. Two authors independently identified studies that were eligible for inclusion and extracted the data. The authors’ disagreement was settled by unanimous agreement. Patient demographics, prostate size, a successful voiding trial, and catheter-free rate were among the variables extracted for the patient with retention.
Results
Literature search
The literature search showed 111 studies, of which 84 were eliminated due to non-relevance based on titles and 18 were eliminated due to lack of relevance based on abstract review (). Full manuscripts were reviewed in nine studies, three of which were excluded because they did not meet the inclusion criteria.
Inclusion criteria
The inclusion criteria articles that describe the use of Rezum in the treatment of refractory urinary retention. Articles that do not have data regarding patients with retention were excluded.
Characteristics of the included studies
The studies spanned between Nov 2016 and April 2022. The included studies evaluated the efficacy of Rezum in managing enlarged prostate. The number of patients in the included articles ranged from 8 to 136 patients. All the included studies found to have low risk of bias on ROBINS-I tool.
Patient demographics
This study included 301 patients in total; all of whom had urinary retention due to enlarged prostate and were catheter-dependent; the mean age was 75.7 years (59 − 89). Mean prostate volume was 74(20–200) cc. The mean preoperative retention volume of 888(566–2100) cc was reported in three articles involving 195 patients ().
Table 1. The included studies, patients demographics and outcomes after Rezum treatment for BPH with chronic urinary retention.
Intervention and outcome
All patients in this review underwent Rezum procedure; the median number of vapor injections used was 10 [5–12] [Citation14–19].
The success rate of a voiding post Rezum therapy trial was 85%, as 256 out of 301 patients were catheter free after the procedure, with follow-up periods ranging between 3 and 12 months. Two articles subclassified patients according to prostate volume to < 80 ccs and > 80 ccs, the catheter-free rate of those groups was 83% and 77.5%, respectively.
The outcome of patients who failed TWOC was reported in 2 articles, 10 patients had reintervention, 3 of them underwent transurethral resection of prostate; 2 of them failed TWOC after it; another 3 patients underwent redo Rezum; and all of them failed TWOC. Four of them remained catheter-dependent either SPC or CIC.
Post-Rezum PVR was 144 ccs, and a post Rezum Q max of 11.6 ml/sec has reported in three studies. The post-Rezum improvement of lower urinary tract symptoms reported in five studies, the mean post-Rezum IPSS was 6.2 (SD+-2.9} in four studies, while one study used the AUA symptoms score, which was 12.75 post-Rezum.
The reported complications were mild in nature with clavien dindo grade I treated conservatively. The complication was reported in four studies involving 233 patients; in which, 10 (4.3%) patients had gross haematuria and 9 (3.8%) patients had urinary tract infection; no other complications were reported.
Discussion
The most common cause of urinary retention in men is BPH; the incidence increases with age where men aged 70 and above are at higher risk [Citation6,Citation20]. The decision between catheterization, surgical intervention for chronic and refractory is challenging. The studies showed the favourable outcome of TURP compared to catheterization in terms of quality of life, and the rate of urinary tract infections [Citation21].
In this review, we studied the Rezum system’s efficacy in refractory urinary retention and found that the catheter-free rate post-Rezum is 85% (number of studies 6 and number of patients 301). The most important factor affecting the rate of successful TWOC was prostate volume, as prostate volume > 80 ccs was associated with lower catheter-free rates (number of studies 2 and number of patients 196). The catheter-free rate of the gold-started transurethral resection of the prostate in the treatment of BPH-induced urinary retention is 92% [Citation22], which is comparable to the results of Rezum in our review (85%). The higher catheter-free rate comes with the expense of higher morbidity and mortality as TURP has a higher incidence of bleeding, incontinence, erectile dysfunction, and retrograde ejaculation compared to Rezum [Citation23].
The reported suboptimal Q max and PVR post-Rezum in patients with refractory retention might be a result of an element of decreased bladder contractility as the patients who failed to void without catheter after Rezum also failed to void after going TURP or redo Rezum and remained catheter-dependent [Citation15,Citation17,Citation24]. In addition, the preoperative risk factors affecting voiding function such as decreased bladder contractility has been reflected in comparable retreatment rates between Rezum and TURP (4.76%–8.33% and 3%–14.5%, respectively) [Citation24–26]. Those findings that emphasize the importance of proper evaluation of the bladder contractility are the cases of failed treatment to avoid unnecessary reinterventions and to predict the outcome.
The effect on sexual function is a major determinant in the management of BPH, for instance the gold standard surgical treatment TURP results in retrograde ejaculation in 50–70% of patients [Citation27]. On the other hand, alpha blocker therapy is associated with reduced ejaculate volume in 90% of patients and anejaculation in 35% of patients. [Citation28]. While the rate of retrograde ejaculation of Rezum is as low as 2% of patients [Citation29]. In our review, the studies showed that erectile function was not affected by Rezum treatment [Citation17,Citation18]. This minimal effect of Rezum on the overall sexual function when compared to TURP makes Rezum superior in terms of preservation of sexual function and fertility.
The adverse effects of Rezum are related to endoscopic instrumentation during the procedure. When compared to TURP, Rezum complications are mild and self-resolving that includes haematuria (11.8%), dysuria (16.9%), urgency (5.9%), frequency and acute urinary retention (3.7%) and urinary tract infection (3.7%) [Citation10,Citation18] . On the other hand, TURP is associated to be more severe that might be life-threatening complications. TURP complication includes but not limited to significant bleeding (0.4%–7.1%), clot retention (2%–5%), electrolyte imbalance and TUR syndrome (0.0%–1.1%), urinary tract infection (1.7%−8.2%) and urinary retention (3% – 9%). Also complications of TURP can be delayed and present in the picture of bladder neck contractures and urethral strictures in about 0.3–9.8% of the cases [Citation25]. While no mortality was reported as post-Rezum, the TURP mortality rate ranges between 0 and 0.25% and increases with age and comorbidities [Citation6,Citation25].
In this review, we observed that Rezum is a safe and effective alternative to TURP in the treatment of refractory urinary retention due to BPH. The main limitation of this review is the low quality of the studies included, as the majority of the studies were retrospective and had a relatively short follow-up period. In addition, some studies included patients with refractory urinary retention as a subgroup.
Conclusion
In this review, Rezum was found to be an efficacious and safe alternative in the treatment of refractory retention with mild complications and minimal morbidity. More research is needed to prove the efficacy of Rezum as an alternative to TURP and to evaluate its long-term complications.
Acknowledgments
We would like to thank The Arab Urology Association for providing Open Access funding for this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Berry SJ, Coffey DS, Walsh PC, et al. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479. PubMed] [Google Scholar] [Ref list.
- Jm D, Aeddula NR. Male urinary retention. 2021 Jul 10. [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. PMID: 30860734. In: StatPearls.
- Foster HE, Barry MJ, Dahm P, et al. Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline. J Urol. 2018 September;200(3):A1-A30,467–668.
- Mishriki SF, Grimsley SJS, Nabi G, et al. Improved quality of life and enhanced satisfaction after TURP: prospective 12-year follow-up study. Urology. 2008;72(2):322–326. [Crossref], [PubMed], [Web of Science ®], [Google Scholar]
- Sagen E, Namnuan RO, Hedelin H, et al. The morbidity associated with a TURP procedure in routine clinical practice, as graded by the modified Clavien-Dindo system. Scand J Urol. 2019 Aug;53(4):240–245. Epub 2019 Jun 3. PMID: 31156002.
- Senior K. Age and comorbidity status predict post-TURP mortality. Nat Rev Urol. 2009;6(463). 10.1038/nrurol.2009.163
- Chung ASJ, Woo HH. Update on minimally invasive surgery and benign prostatic hyperplasia. Asian J Urol. 2018;5(1):22–27.
- Nair SM, Pimentel MA, Gilling PJ. Evolving and investigational therapies for benign prostatic hyperplasia. Can J Urol. 2015;22(Suppl.1):5. [PubMed] [Google Scholar] [Ref list].
- McVary KT, Gange SN, Gittelman MC, et al. Minimally invasive prostate convective water vapor energy ablation: a multicenter, randomized, controlled study for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol. 2016;195:1529–1538. [PubMed] [Google Scholar] [Ref list].
- Dixon C, Cedano ER, Pacik D, et al. Efficacy and safety of Rezūm system water vapor treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Urology. 2015 Nov;86(5):1042–1047. Epub 2015 Jul 26. PMID: 26216644.
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560.
- Higgins JPGS. Cochrane handbook for systematic reviews of interventions: the cochrane collaboration. 2011. cited 2018 Jan 30. Available from: www.cochrane-handbook.org
- JAC S, MA H, BC R, et al. ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016;355:i4919.
- Bole R, Gopalakrishna A, Kuang R, et al. Comparative postoperative outcomes of Rezūm prostate ablation in patients with large versus small Glands. J Endourol. 2020 Jul;34(7):778–781. Epub 2020 Jun 12. PMID: 32408768.
- Bassily D, Wong V, Phillips JL, et al. Rezūm for retention-retrospective review of water vaporization therapy in the management of urinary retention in men with benign prostatic hyperplasia. Prostate. 2021 Oct;81(14):1049–1054. Epub 2021 Jul 20. PMID: 34287992.
- Alegorides C, Fourmarier M, Eghazarian C, et al. Treatment of benign prostate hyperplasia using the Rezum® water vapor therapy system: results at one year. Prog Urol. 2020 Oct;30(12):624–631. Epub 2020 Aug 18. PMID: 32826195.
- Eredics K, Wehrberger C, Henning A, et al. Rezūm water vapor therapy in multimorbid patients with urinary retention and catheter dependency. Prostate Cancer Prostatic Dis. 2022 Feb;25(2):302–305. Epub 2021 Sep 29. PMID: 34588631.
- Wong A, Mahmalji W. The role of Rezūm ™ team ablation of the prostate in the treatment of patients with acute urinary retention secondary to benign prostatic hyperplasia. A single center, single surgeon case series and literature review. Aging Male. 2020 Dec 5;23:1620–1626. Epub 2021 Apr 5.
- McVary KT, Rogers T, Roehrborn CG. Rezūm water vapor thermal therapy for lower urinary tract symptoms associated with benign prostatic hyperplasia: 4-year results from randomized controlled study. Urology. 2019Apr; 126: 171–179 Epub 2019 Jan 21. PMID: 30677455
- Groves HK, Chang D, Palazzi K, et al. The incidence of acute urinary retention secondary to BPH is increasing among California men. Prostate Cancer Prostatic Dis. 2013;16:260–265.
- Lin YH, Hou CP, Chen TH, et al. Transurethral resection of the prostate provides more favorable clinical outcomes compared with conservative medical treatment in patients with urinary retention caused by benign prostatic obstruction. BMC Geriatr. 2018;18(15). 10.1186/s12877-018-0709-3
- Karavitakis M, Kyriazis I, Omar MI, et al. Management of urinary retention in patients with benign prostatic obstruction: a systematic review and meta-analysis. Eur Urol. 2019 May;75(5):788–798. Epub 2019 Feb 14. PMID: 30773327.
- Tanneru K, Jazayeri SB, Alam MU, et al. An indirect comparison of newer minimally invasive treatments for benign prostatic hyperplasia: a network meta-analysis model. J Endourol. 2021 Apr;35(4):409–416. Epub 2021 Jan 25. PMID: 32962442.
- Blanchard K, Hananel A, Rutchik S, et al. Transurethral resection of the prostate: failure patterns and surgical outcomes in patients with symptoms refractory to alpha-antagonists. South Med J. 2000 Dec;93(12):1192–1196. PMID: 11142455.
- Rassweiler J, Teber D, Kuntz R, et al. Complications of transurethral resection of the prostate (TURP)–incidence, management, and prevention. Eur Urol. 2006 Nov;50(5):969–979.
- EB G, Shukla D, KT R, et al. Rezum therapy for patients with large prostates (≥ 80 g): initial clinical experience and postoperative outcomes. World J Urol. 2021 Aug;39(8):3041–3048. Epub 2021 Jan 3. PMID: 33392646; PMCID: PMC7779102.
- Couteau N, Duquesne I, Frédéric P, et al. and benign prostatic hyperplasia: an impossible compromise? A comprehensive review. J Clin Med. 2021 Dec 10;10;24:5788. PMID: 34945084; PMCID: PMC8704358.
- Hellstrom WJ, Sikka SC. Effects of acute treatment with tamsulosin versus alfuzosin on ejaculatory function in normal volunteers. J Urol. 2006;176:1529–1533.
- Lokeshwar SD, Valancy D, Lima TFN, et al. Review of reported ejaculatory dysfunction in clinical trials evaluating minimally invasive treatment modalities for BPH. Curr Urol Rep. 2020 Oct26;21(12):54. PMID: 33104947.