ABSTRACT
Background
Standard 24-h antibiotic prophylaxis (AP) is widely employed to minimize the risk of infection complications (ICs) within 30 days following a radical cystectomy (RC). However, a considerable variety of prophylaxis protocols do not prevent a high ICs rate after surgery (37–67%). Therefore, antibiotic’s type and its duration are still controversial for AP.(
Objective
To compare standard 24-h AP with a prolonged 120-h regimen in a multicenter randomized clinical trial.
Methods
Patients were randomized in a 1:1 ratio to standard 24-h AP regimen (Group A) versus the prolonged meropenem AP 120-h (Group B). The primary endpoint was an event rate defined as the frequency of ICs within 30 days. The secondary endpoint were biomarker’s analysis and antibiotic re-administration rate (ArAR).
Results
A total of 92 patients were enrolled. The Clavien-Dindo complications rate did not differ between the groups (p = 0.065), however the overall complication rate was higher in Group A (63.0% vs. 34.8%, p = 0.007). The infection complication rate was 2.75 times higher in the standard antibiotic prophylaxis group: 47.8% compared to 17.4% cases in Group B (p = 0.002). The new prolonged antibiotic regimen decreased the risk of ICs (OR 0.23; 95% CI 0.08–.598; p = 0.003).
The event-free survival for ICs of clinical interest in group A was 7.00 days and in group B was 9.00 days (HR = 0.447; 0.191–1.050, p = 0.065). The ArAR was higher in Group A -47.8%, while in Group B it was only in 17.4% of the cases. The incidence of bacteriuria before RC was the same between groups (p = 0.666), however, after stent removal the risk of a positive culture was lower in group B (RR = 0.64; 95% CI 0.37–1.08; p = 0.05).
Conclusions
The administration AP over 120-h appears to be safe and feasible, demonstrating a reduction in the total number of complications and ArAR. Trial registration in Clinical Trials: NCT05392634.
Trial registration in Clinical Trials: NCT05392634.
Introduction
Radical cystectomy (RC), employing various methods of urinary diversion, is the primary approach for treating very high-risk non-muscle invasive bladder cancer (NMIBC), as well as muscle-invasive bladder cancer (MIBC) [Citation1,Citation2]. However, RC is frequently associated with a substantial incidence of postoperative complications, notably urinary tract infections (UTIs) and surgical site infections, with reported rates up to 67% [Citation3,Citation4]. Symptomatic UTIs can trigger more severe infectious complications (ICs) such as sepsis (48.5%) or septic shock and are associated with a higher frequency of readmission (33.3%) [Citation5,Citation6].
Antibiotic prophylaxis (AP) is a prominent approach in the management of antimicrobial therapy with the goal of mitigating the risk of postoperative infection by employing systemic antibiotics before operation [Citation7]. In alignment with clinical guidelines, the initial antibiotic dose should be administered 30–60 min before operation and the time window for antibiotic administration is confined to 24 h following the RC (standard AP) [Citation7].
The choice of AP often depends on the surgeon’s decisions, bacterial culture, or local practices. However, Kransnow (2017) investigated AP protocols in 8,351 patients undergoing RC across 353 hospitals in the United States. It was reported that 579 unique antibiotic regimens were prescribed on the day of the operation. Furthermore, only 15.0% of the patients received AP in accordance with guidelines, while 51.0% of the patients were administered 2 or more antibiotics [Citation8]. In a retrospective analysis by Ross (2021) high body mass index (BMI), American Society of Anesthesiologists score (ASA), type of urinary diversion (UD) or AP type did not impact on the frequency of ICs was observed (RR = 0.99, 95% CI 0.50–1.99) [Citation9]. Atduev et al. (2019) demonstrated a shift in the paradigm of RC from ‘conditionally contaminated surgery’ to ‘highly contaminated’ by providing evidence of the association between the intraoperative contamination of the abdominal cavity and ileus and ICs (OR 3.4; 95% CI: 1.742–6.637; p < 0.001). Bacterial contamination was emerged as a significant predictor of postoperative ileus and infectious complications (OR 3.4; 95% CI: 1.742–6.637, p < 0.001). The findings demonstrate that RC is considered a contaminated and ‘dirty’ procedure, and in an experiment (n = 32), the effectiveness of Meropenem in reducing the frequency of complications of grades 3–4 was demonstrated [Citation10]. These data formed the basis for a prospective study.
The obtained data cast doubt on the contemporary choice of antimicrobial agents (AMAs), the regimen, and the duration of AMA administration limited to only 24 h after RC. The justification for using the type of AP in RC is to reduce the frequency of ICs, with the secondary goal being the reduction of unwarranted and excessive antibiotic use. Therefore, the aim of this study is to assess the risk of developing ICs depending on the length of the AP regimen.
Materials and methods
The MACS trial is a prospective, randomized phase III study assessing the efficacy of the standard 24-h AP regimen (Group A) compared to the prolonged meropenem AP over 120-h (Group B) for reduction of postoperative ICs within 30 days following RC. The study was registered at ClinicalTrials.gov (NCT05392634).
Participants of both genders >18 years old with morphologically confirmed of very high-risk NMIBC or non-metastatic MIBC, an Eastern Cooperative Oncology Group (ECOG) performance status 0–1, without uncontrolled concomitant chronic diseases or individual intolerance to the antibacterial drugs specified in the study protocol or systemic inflammatory response syndrome at the time of hospitalization – were enrolled in the study. Recruiting centers should work according to the principles Enhanced Recovery After Surgery (ERAS).
One hundred and sixteen patients were included in three centers from May 2022 to March 2024, and 92 participants were randomly assigned into a 1:1 ratio to receive different types of AP. Patients were stratified based on two criteria: the administration of neoadjuvant therapy (presence or absence of therapy) and the type of urinary diversion (orthotopic; heterotopic). Group A (n = 46) received standard AP where either Amoxicillin/clavulanic acid 1.2 g or a Cefuroxime 1.5 g was administered parenterally 30 min before incision. The duration of the perioperative AP more than 24 h was not allowed. In Group B (n = 46), prolonged AP used Meropenem (1 g every 8 h for 5 days). To treat emerging infectious complications, it was allowed to prescribe another antibiotic. The radical cystectomy was performed with laparoscopic approach with extended lymphadenectomy and intracorporeal UD. Postoperative silicone drainage F24–26 of the abdominal cavity was not prohibited. Coloplast single loop ureteral stents 90 cm Ch 7–8 were used. For orthotopic UD a silicone catheter Foley Ch20–22 type was used.
The primary endpoint was an event rate (frequency of ICs within 30 days following RC). Secondary endpoints were biomarkers analysis and re-administration of any antibiotics during hospitalization (antibiotic re-administration rate) [Citation11]. In both groups, urine culture was collected intraoperatively before skin incision with bladder catheterization in sterile conditions (sample 1). The second urine sampling (sample 2) was performed after the complete removal of ureteral stents/urethral catheter (in case of orthotopic ureteric diversion). The third collection of biological material (sample 3) was done if any infectious complication occurred. The result was considered positive at a microbiological score of ≥10^5 CFU/l. Clinically significant carbapenemase genes were detected using an in vitro visual multiplex immunochromatographic assay ‘NG-Test CARBA 5’, which detects one or more of the five common types of carbapenemase enzymes (KPC, OXA-48, VIM, IMP, and NDM) from bacterial colonies [Citation12].
The planned sample size of 92 patients was estimated using an inequality test for 2 independent proportions (‘Sample Size Calculators’ UCSF CTSI, Kohn MA, Senyak J.). The Type I error was 5%, and type II error was 20% [Citation13,Citation14]. All analyses were performed in accordance with the intention-to-treat principle. Statistical analysis was performed using StatTech v. 4.1.1 (Developer – StatTech LLC, XXXX). Differences were considered statistically significant at p < 0.05.
Results
The study groups were well-balanced in terms of age, gender, BMI, neoadjuvant treatment, staging and the presence of nephrostomy drainage (see ). Neoadjuvant therapy was performed in 60/92 cases (65.2%): platinum-based chemotherapy was predominantly prescribed in 54/92 (59.0%) of cases, and 4/92 (4.3%) patients received a PD-1 inhibitor antibody. The groups were balanced with respect to the planned type of urinary diversion (intent-to-treat): 40/46 (87.0%) in Group A and 39/46 (84.8%) in Group B (p = 1.0) were planning heterotopic urinary diversion.
Table 1. Baseline characteristics of patients.
Most surgeries were performed using the minimally invasive laparoscopic approach: in Group A in 44/46 (95.7%) and in Group B in 43/46 (93.5%) cases. The drainage of the abdominal cavity or pelvis was the same in groups (p = 635). When assessing the postoperative indicators (as treated), no statistically significant differences were found (p = 0.822). It is noteworthy that 12 (13.0%) patients underwent RC without intracorporeal urinary diversion. In 11 cases were completed with placement of nephrostomy drainage and in 1 (1.1%) case in Group A, the treatment volume was not completed due to technical difficulties (see ). The length of hospitalization was shorter on 2 days in Group B, but it was not significant (p > 0.5). Other perioperative features are detailed in .
Table 2. Perioperative features of patients.
The severity of the complications according to the Clavien-Dindo classification did not differ between the groups (p = 0.065) (see ). The total number of complications in the standard AP group was 63.0% compared to the prolonged AP group 34.8% (p = 0.007). The relative risk (RR) of developing any adverse event was lower in the prolonged AP group by 45.0% (RR = 0.55, 95% CI 0.35–0.87, p = 0.005). The total number of ICs of clinical interest was also higher in group A versus Group B: 47.8% (22/46) and 17.4% (8/46) (p = 0.002). The RR of ICs of clinical interest was lower in the prolonged AP group by 64.0% (RR = 0.36, 95% CI 0.18–0.73, p = 0.002).
Table 3. Types of complications within 30 days following a radical cystectomy with urinary diversion.
Among events of clinical interest, UTIs were more frequently identified in the standard AP group – in 22.0% of the cases (10/46), and surgical site infection in 13.0% (6/46). In the prolonged group, UTIs were identified in only 2.2% (1/46) of cases, and no cases of wound infection were reported. At the same time, there were 2 cases (4.3%) of eventration in the prolonged group. When assessing the impact of the AP variant on the UTI frequency, a significant deviation in favor of prolonged AP was found (RR = 0.10; 95% CI 0.01–0.75; p = 0.012). Among other complications, different frequencies of therapeutic complications such as thrombosis, lung infarction pneumonia, and COVID-19 infection were observed. Reoperation was required for 20 patients. Indications for surgery included wound dehiscence, wound infection, urine leakage, bowel obstruction or intestinal perforation. The 30-days mortality did not differ between the groups (p = 1.0).
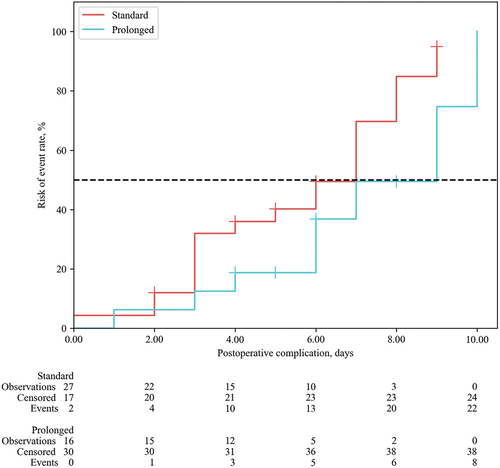
The median time to the development of any complication was 1.0 (0.0–6.0) days. The median time of event-free survival (EFS) for ICs of clinical interest in group A was 7.00 days (95% CI: 3.00–7.00 days), and the median time of EFS in group B was 9.00 days (95% CI: 6.00–10.00 days) (log rank test p = 0.05). However, Cox proportional hazards model did not reveal a significant difference between groups (HR = 0.447; 0.191–1.050, p = 0.065) (see ). The antibiotic re-administration rate within 30 days following RC was 47.8% (22/46) in the standard AP group, while in the prolonged AP group, it was only 17.4% of the cases (8/46). The use of meropenem prolonged regimen reduced the risk of additional administration of another antibiotic by 64.0% (RR = 0.36, 95% CI 0.18–0.73; p = 0.002).
Figure 2. Time to the development of events of clinical interest (event-free survival) within 30 days following radical cystectomy with urinary diversion (HR = 0.447; 0.191–1.050, p = 0.065).
The incidence of bacteriuria before RC was 34.8% (16/46) in the control group and 39.1% (18/46) in the Group B (p = 0.666) (). In Sample 1, bacteriuria was attributed to E. coli in 13.0% of participants in Group A and 6.5% in Group B; E. faecalis was found in 6.5% of Group A participants and 13.0% of Group B participants, while K. pneumonia was present in equal proportions at 4.3% in both groups. All the stents were removed on postoperative day 9 (±1 day), and analysis of Sample 2 determined the same bacterial colonization (p = 0.087). However, the risk of a positive culture was lower in group B than in the standard group, but it was not statistically significant (RR = 0.64; 95% CI 0.37–1.08; p = 0.05). The most frequent pathogen in Sample 2 of both groups was E. faecalis 6.5% and 13.0%, respectively and in group A: K. oxytoca (6.5%) and E. coli 15.2%. The Sample 3 was also not differed between groups, but in the prolonged AP group E. coli (4.3%), Sph. Epidermidis (4.3%) and K. aerogenes (2.2%) were predominant. The NG-Test Carba 5 revealed the Carbapenemase producer’s strain in 3.95 times less in the prolonged AP group than in the standard group: 15.2% (7/46 cases) versus 4.3% (2/46 cases), but it was not statistically significant (RR = 0.29; 95% CI: 0.06–1.3; p = 0.052).
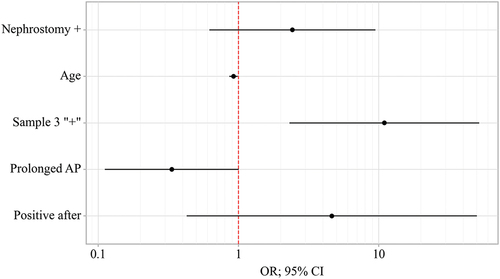
Multivariate logistic regression was performed to identify risk factors for infectious complications of clinical interest with the results shown in and . The presence of nephrostomy, abdominal drain and time to remove stents/catheters did not influence the ICs rate of clinical interest. The new prolonged antibiotic regimen independently decreased the risk for infectious complications (odds ratio [OR] 0.23; 95% CI 0.08–.598; p = 0.003). Additional independent risk factors included Age (OR 0.94; 95% CI 0.88–0.99; p = 0.019), positive bacterial culture in Sample 3 (OR 13.11; 95% CI 3.33–51.63; p < 0.001) and detection the Carbapenemase producer’s strain after RC in Sample 2 or 3 (OR 15.25; 95% CI 1.74–133.49; p = 0.014).
Table 4. Univariate and multivariate logistic regression of risk factors for infectious complications of clinical interest.
Discussion
The study groups in the article were well-balanced in terms of various factors such as age, gender, BMI, neoadjuvant treatment, TNM stage, and the presence of nephrostomy drainage. Neoadjuvant therapy was performed in the majority of cases, with platinum-based chemotherapy being the most commonly prescribed. The planned type of urinary diversion was also similar between the groups, with a high percentage planning for heterotopic diversion.
The intestinal UD is a key challenge for postoperative infection’s risk. In long-term studies on RC outcomes, UTIs were common within the first 3 months post-surgery [Citation15,Citation16]. Recent research by Kim et al. (2018) compared extended and short-term AP for orthotopic UD. The rates of short UTIs within 60 days were similar (28.6% vs. 28.4%, p = 0.969), and bacteremia rates were comparable (h = 0.415). According to this research, short-term AP effectively prevents UTIs and does not require the use of a combination of three or more antibacterial drugs [Citation17]. In a study by Numau et al. (2020), comparing single dose vs. prolonged AP, the overall IC rate was 44% and no significant difference between groups (25.0% vs. 34.0%, p = 0.23) [Citation18]. In this MACS trial type of UD (intent-to-treat or as treated) according to logistic regression of risk factors for ICs of clinical interest did not reveal any influence on results.
There were differences in the frequency of UTIs and surgical site infections between the two groups, however, with UTIs being more common in the standard AP group. The prolonged AP group had a lower frequency of UTIs and no reported cases of wound infection, although there were cases of eventration. The impact of the AP variant on UTI frequency favored the prolonged AP group. Multivariate logistic regression had shown that prolonged antibiotic regimen independently decreased the risk for infectious complications by 77% (odds ratio [OR] 0.23; 95% CI 0.08–.598; p = 0.003) and suggests that the results of this study are positive.
In this study, patient age was a significant predictor of complications after radical cystectomy. However, the effectiveness of AP is even less studied among elderly patients (>65 years old). According to the systematic review by Ahmed (2017), prolonged AP demonstrated a 24% reduction in the risk of recurrent UTIs for elderly female patients (RR = 0.76; 95% CI 0.61–0.95). Importantly, no statistically significant increase in the risk of adverse events was noted (RR 1.52; 95% CI 0.76–3.03) [Citation19]. The medium age in this study was 65.01 ± 8.7 (37–82) years. On the contrary, a decrease in age below the average was associated with an increased risk of a clinical event occurring: RR 0.91 (95% CI: 0.85–0.98; p = 0.010). This fact underscores the necessity of determining indications or contraindications for the length of AP in the elderly patient population. Furthermore, there is a need to assess the frequency of readmissions after RC with urinary diversion and investigate the occurrence of adverse events associated with anticoagulant therapy in this demographic group. This warrants further exploration in research studies.
This study has several limitations. A major flaw was that Group A and Group B vary both by the duration of AP and by type of antibiotic. Therefore, it cannot be concluded that prolonged AP (and not simply the type of antibiotic) improves ICs. Furthermore, this trial was not enough to demonstrate the preventive benefits in subgroup analysis. In 26.0% of patients, the intent-to-treat urinary diversion was not performed, which could subsequently distort the results of surgical treatment and reduce the expected incidence of complications. Additionally, all RC with UD were performed at large clinics, but the potential impact of surgical experience on the incidence of complications was not taken into account (in one center the surgeon’s experience >500 cystectomies).
Conclusion
In conclusion, our study highlights the potential benefits of a prolonged antibiotic prophylaxis regimen in reducing postoperative complications and infections following radical cystectomy. We found that the prolonged AP group had lower overall complication rates, reduced incidence of urinary tract infections, and a lower need for additional antibiotic administration compared to the standard AP group. These findings suggest that optimizing antibiotic prophylaxis protocols could improve patient outcomes and reduce healthcare resource utilization in this surgical setting. Further research and larger studies are warranted to validate these results and determine the optimal duration and type of antibiotic prophylaxis for patients undergoing radical cystectomy.
(see ).
Nephrostomy± presence of nephrostomy before radical cystectomy; Sample 3 – presence of bacterial culture at biological material during any infectious complication occurred; Prolonged AP – prolonged 120-h regimen with meropenem (Group B); Positive after – revealed the Carbapenemase producer’s strain after radical cystectomy;
The data was present for all variables in all patients.
Data sharing
The trial protocol and deidentified participant data collected for this trial are available from the corresponding author B.M.V. on a reasonable request.
Ethics approval and consent to participate
This study was approved by The Local Ethics Committee of the FSBI ‘NMRC of oncology N.N. Petrov’ MH of the Russian Federation (No. 1/129 on 28 April 2022). All patients gave their written informed consent.
Specific author contributions
N.A.K., G.T.Yu., B.M.V.: conception and design. B.A.M., N.A.K., G.T.Yu. administrative support. B.M.V., T.N.I., R.S.A.: provision of patients. B.M.V., T.N.I., R.S.A.: collection and assembly of data. B.M.V. data analysis and interpretation. All authors: manuscript writing. All authors: Final approval of the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Witjes JA, Bruins HM, Cathomas R, et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. Eur Urol. 2020;79(1):82–104. doi: 10.1016/j.eururo.2020.03.055
- Gontero P. Guidelines on mon-muscle-invasive bladder cancer (Ta, T1 and CIS). In: EAU Guidelines published at the 38th Annual Congress Milan; Arnhem, the Netherlands. European Associaton of Urology Guidelines Office; 2023.
- Lawrentschuk N, Colombo R, Hakenberg OW, et al. Prevention and management of complications following radical cystectomy for bladder cancer. Eur Urol. 2010;57(6):983–1001. doi: 10.1016/j.eururo.2010.02.024
- Nosov AK, Reva SA, Dzhalilov IB, et al. Radical cystectomy for bladder cancer: сomparison of early surgical complications during laparoscopic, open-access, and video-assisted surgery. Oncourology. 2015;11(3):71–78 (In Russ.). doi: 10.17650/1726-9776-2015-11-3-71-78
- van Hemelrijck M, Thorstenson A, Smith P, et al. Risk of in-hospital complications after radical cystectomy for urinary bladder carcinoma: population-based follow-up study of 7608 patients. BJU Int. 2013;112(8):1113–1120. doi: 10.1111/bju.12239
- Browne E, Lawrentschuk N, Jack GS. A systematic review and meta-analysis of the long-term outcomes of ileal conduit and orthotopic neobladder urinary diversion. Can Urol Assoc J. 2021;15(1):E48–E57. doi: 10.5489/cuaj.6466
- Lightner DJ, Wymer K, Sanchez J, et al. Best practice statement on urologic procedures and antimicrobial prophylaxis. J Urol. 2020;203(2):351. doi: 10.1097/JU.0000000000000509
- Krasnow RE, Mossanen M, Koo S, et al. Prophylactic antibiotics and postoperative complications of radical cystectomy: a population based analysis in the United States. J Urol. 2017;198(2):297–304. doi: 10.1016/j.juro.2017.02.3340
- Ross J, Breau RH, Vigil H, et al. Association between radical cystectomy prophylactic antimicrobial regimen and postoperative infection. Can Urol Assoc J. 2021;15(12):E644–E651. doi: 10.5489/cuaj.7158
- Atduev VA, Gasrataliev VE, Ledyaev DS, et al. Predictors for postoperative complications from radical cystectomy. Onkol Z im PA Gercena. 2019;8(5):348–357 (In Russ). doi: 10.17116/onkolog20198051348
- Timsit JF, de Kraker ME, Sommer H, et al. Appropriate endpoints for evaluation of new antibiotic therapies for severe infections: a perspective from COMBACTE’s STAT-Net//Intensive. Intensive Care Med. 2017;43(7):1002–1012. doi: 10.1007/s00134-017-4802-4
- Volland H, Girlich D, Laguide M, et al. Improvement of the immunochromatographic NG-Test carba 5 assay for the detection of IMP variants previously undetected. Antimicrob Agents Chemother. 2019 [cited 2019 Dec 20];64(1):e01940–19. doi: 10.1128/AAC.01940-19
- Hulley SB, Cummings SR. Designing clinical research: an epidemiologic approach. Wilkins, Philadelphia; 2013. p. 75.
- Fleiss JL, Tytun A, Ury HK. A simple approximation for calculating sample sizes for comparing independent proportions. Biometrics. 1980;36(2):343–346. doi: 10.2307/2529990
- Hautmann RE, de Petriconi Rc, Volkmer BG, de Petriconi RC. 25 years of experience with 1,000 neobladders: long-term complications. J Urol. 2011;185(6):2207–2212. doi: 10.1016/j.juro.2011.02.006
- Mano R, Baniel J, Goldberg H, et al. Urinary tract infections in patients with orthotopic neobladder. Urol Oncol. 2014;32(1):.e50.9–.e50.14. doi: 10.1016/j.urolonc.2013.07.017
- Kim CJ, Kim KH, Song W, et al. Impact of a change in duration of prophylactic antibiotics on infectious complications after radical cystectomy with a neobladder. Med (Baltimore). 2018;97(47):e13196. doi: 10.1097/MD.0000000000013196
- Numao N, Fujiwara R, Uehara S, et al. Intraoperative only versus extended duration use of antimicrobial prophylaxis for infectious complications in radical cystectomy with intestinal urinary diversion. Urol Int. 2020;104(11–12):954–959. doi: 10.1159/000509881
- Ahmed H, Davies F, Francis N, et al. Long-term antibiotics for prevention of recurrent urinary tract infection in older adults: systematic review and meta-analysis of randomised trials. BMJ Open. 2017;7(5):e015233. doi: 10.1136/bmjopen-2016-015233