ABSTRACT
Objectives: Many hospitals have recently instituted policies mandating preoperative COVID-19 testing. However, it is uncertain whether institutions can dictate such policies based on infection rates found in the general population. Therefore, the main aims of the study were to determine (1) what proportion of preoperative patients tested positive, (2) what percentage was asymptomatic, and (3) whether variations throughout time in numbers of positive patients reflected changes observed in our state.Methods: All COVID-19 preoperative screening tests (nasopharyngeal-swab RT-PCR testing) performed in our hospital between 04/13/2020 and 08/27/2020 were retrospectively reviewed. The unit of analysis was number of patients who tested negative/positive. Medical records of positive patients were reviewed to determine the presence of COVID-19 symptoms. A curve was created showing our number of positive patients per week and another one presenting the number of positive patients per day in Florida, both figures were compared.Results: A total of 7,213 patients from all specialties were preoperatively tested, out of which 85 were positive for an overall infection rate of 1.2%. In 18% (15/85) of positive patients, it was not possible to determine symptomatology. Among remaining patients, 49% (34/70) were asymptomatic while 51% (36/70) were symptomatic for COVID-19. Peak of positive cases occurred in mid-July in both curves, and the upward and downward tendencies in positive numbers mirrored each other.Conclusion: COVID-19 infection rate among our preoperative patients was very low. Nearly 50% of positive patients were asymptomatic. Our data suggest that a tertiary hospital can promulgate COVID-19 preoperative screening policies based on infection trends observed in the general population. However, in addition to the test, patients should be encouraged to self-quarantine for 14 days before surgery.
Introduction
As of 19 August 2020, according to the Center for Disease Control and Prevention (CDC), the United States identified a total of 5,422,242 residents who tested positive for SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2), the virus for the COVID-19 pandemic [Citation1]. Concurrently, in the state of Florida, where our tertiary care facility is located, 584,047 residents tested positive for COVID-19 which resulted in 9,932 deaths [Citation2]. In view of the magnitude of the pandemic, many hospitals across the nation (including ours) have instituted policies mandating preoperative COVID-19 testing before all hospital admissions. Starting 13 April 2020, preoperative COVID-19 nasopharyngeal swab real-time quantitative polymerase-chain reaction (RT-PCR) screening test was mandatory within 3 days prior to any procedure (this included elective and unelective surgeries as well as inpatient and outpatient procedures). The rationale behind this universal preoperative COVID-19 screening policy was to protect hospital staff and patients from infection. A secondary intent of this intervention was to identify those patients that are infected and prevent complications related to surgical interventions. Recent literature reports suggest that the pro-inflammatory state generated by COVID-19 results in a significant proportion of patients to develop postoperative complications related to a prothrombotic and/or thrombotic tendency [Citation3].
Recently, in the state of New York, there were reports regarding the results of universal RT-PCR screening for SARS-CoV-2 in admitted patients for delivery or surgical interventions [Citation4,Citation5]. It is unknown whether the findings of this type of screening performed in tertiary level hospitals in regions with a high incidence of COVID-19 infection can be extrapolated to hospitals located in other areas with lower, similar, or higher infection rates. Similarly, it remains to be demonstrated whether hospitals can dictate institutional policies regarding preoperative COVID-19 screening based on infection rates found in the general population. We sought to determine whether the variations observed throughout time in the number of infections in our tertiary level facility (based on universal preoperative screening results) mirrored the pattern seen in the general population.
Consequently, the three aims of this study were (1) to determine what proportion of our preoperative patient population tested positive for COVID-19, (2) what proportion of positive COVID-19 patients was asymptomatic or had symptoms due to this condition, and (3) to ascertain whether the variations in the numbers of positive preoperative patients identified from 13 April 2020 to 27 August 2020 at our hospital reflected the changes observed in the general population of the state of Florida during the same period of time. We hypothesized that variations observed in the number of positive preoperative cases throughout time would diverge from the pattern seen in Florida.
Materials and methods
Since 13 April 2020, all patients with planned or unplanned procedures at our institution had a mandatory preoperative screening for COVID-19. After Institutional Review Approval, we retrospectively reviewed the results of the preoperative screening tests (all specialties) performed between 13 April 2020 and 27 August 2020. Test results were provided by our Department of Clinical Quality. We reviewed the medical records to determine whether patients with a positive COVID-19 result were asymptomatic or not. All patients underwent nasopharyngeal swab RT-PCR testing within 3 days prior to their procedure. Because many patients underwent multiple testing, it is important to make clear that, in the current investigation, the unit of analysis is the number of patients tested for COVID-19 instead of the number of tests performed.
Statistical analysis
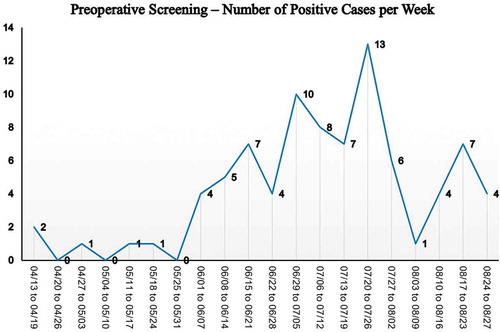
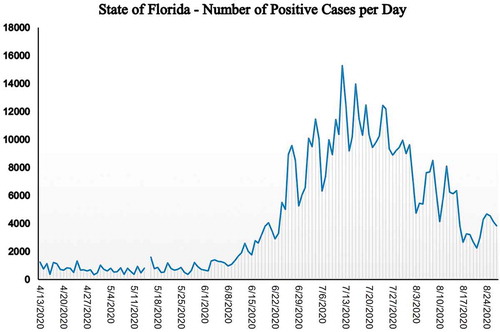
A curve () was created showing the number of preoperative positive cases per week (y axis) among those patients who underwent procedures in our institution between 13 April 2020 and 27 August 2020 (x axis). To ascertain the number of positive COVID-19 residents reported each day in the state of Florida, we accessed daily data provided by The COVID Tracking Project at The Atlantic which is available under a Creative Commons CC BY 4.0 license [Citation6,Citation7]. We then created a curve () illustrating the number of positive cases reported per day in the state of Florida during the same period of time used for the preoperative curve (). The curves of both figures (preoperative screening vs. Florida) were compared to determine whether there were similarities or differences in the patterns representing the number of infections throughout time (curve peaks, valleys, and/or plateau).
Results
Between 13 April 2020 and 27 August 2020, a total of 7,213 patients from all specialties were preoperatively tested for COVID-19, out of which 85 tested positive for an overall infection rate of 1.2%. In 15 of these 85 patients (18%), it was not possible to determine whether there were COVID-19 symptoms or not. It is important to note that none of these 15 patients underwent emergency department visits or hospitalizations due to COVID-19. The remaining 70 patients had explicit chart notes regarding their COVID-19 symptomatology. Among them, 49% (34/70) were asymptomatic and 51% (36/70) were symptomatic.
Regarding the variations throughout time in the numbers of positive results, only five patients tested positive before June 1st. From this date onwards, there was a significant increment in the number of positive cases that tested positive. We further observed a distinct peak on the fourth week of July when a total of 13 patients tested positive. After this week, there was a significant decline in the number of positive cases. The pattern observed among preoperative patients is illustrated in .
Similarly to the trend observed at our institution, there were a relatively stable number of daily cases that tested positive in the state of Florida until the first week of June. After that week, the numbers started to consistently increase reaching a peak on July 12th when 15,300 residents tested positive. From this date forward, and until July 25th, there were multiple days when more than 10,000 residents tested positive. Starting July 26th, the reported incidence of cases that tested positive remained below 10,000 a day. To follow this trend, there was a consistent decrease in reported numbers so that by 27 August 2020, only 3,838 residents were reported positive in the state of Florida. This configuration is illustrated in . The trends observed in (preoperative screening) and 2 (Florida population) were strikingly similar to the peak of positive COVID-19 cases occurring on mid-July in both curves. The upward and downward tendencies in the number of positive cases were also parallel in both curves.
Discussion
To the best of our knowledge, there are no previous reports on whether tertiary hospitals can establish preoperative COVID-19 screening policies based on infection rates that are present in the general population. Therefore, the three main purposes of this investigation were to determine (1) what proportion of preoperative patients tested positive for COVID-19 in our facility, (2) what proportion of positive patients was symptomatic, and (3) whether the variations observed in the numbers of positive preoperative patients reflected the changes detected in the general population. We hypothesized that the variations observed in the number of positive preoperative cases throughout time would diverge from the pattern seen in Florida. The rationale for this is that our hospital is a highly specialized tertiary level facility that treats a particularly complex case mix of patients, which might not be representative of the general population. Our data demonstrated that a tertiary hospital can promulgate COVID-19 preoperative screening policies based on infection trends observed in the general population. In previous reports, it was unknown whether data from specialized institutions could be extrapolated to the general population, or vice versa [Citation4,Citation5].
In view of the very low infection rate found among our preoperative patients, and that about half of these positive patients were asymptomatic, the costs (i.e., financial/resources) of preoperative testing cannot be ignored. Particularly, when the whole preoperative screening policy is based on a test with 99% specificity but only 60–70% reported sensitivity [Citation8,Citation9] meaning that 1 out of 3 patients who tests negative before surgery might actually be infected. It is important to note that serological testing is not useful as a preoperative screening tool because it cannot confirm nor exclude acute infection. Furthermore, IgG or IgM antibody positivity is not an assurance of protection against COVID-19 [Citation10].
The current study should be viewed in light of several limitations. Firstly, this is a retrospective study and consequently there is always the possibility of bias. However, this report is not an inferential study but a descriptive one. Second, the reporting of positive COVID-19 cases in Florida relies on information provided by laboratories, and it has been reported that a major provider did not report thousands of them to the Florida Department of Health in a timely manner [Citation11]. The reporting of old cases seemed to affect the positivity rate in Florida for 31 August 2020 [Citation12] which is a date not included in the study period (13 April 2020 to 27 August 2020). It is important to keep in mind that data from public sources depend on timely and proper reporting.
The objective of RT-PCR screening for COVID-19 is to detect viral RNA in the presymptomatic phase of infection, and for a positive result, viral RNA needs to reach detectable thresholds [Citation13]. Strategies different from RT-PCR testing could be implemented to minimize the risk to patients and providers. Perhaps the best way to ensure that patients arrive at the hospital for surgery without subclinical COVID-19 infection is a mandated self-quarantine for 14 days prior to surgery [Citation13]. We acknowledge that this might not be feasible in urgent cases or other unusual clinical settings, but patients should be encouraged to self-quarantine for 14 days before surgery due to the suboptimal sensitivity of the COVID-19 test [Citation8,Citation9] We are mindful that patient compliance is difficult to verify. However, it might be possible for providers to make use of electronic devices and/or applications to verify and monitor patient’s well-being and compliance with self-quarantine.
It is important to note that a quarantine radically alters the daily habits and may have a negative impact on the well-being of patients. It has been demonstrated that ‘social distancing’ helps contain the spread of the virus but at a price for patients and entire communities. Prolonged self-isolation negatively affects the lifestyle, psychological well-being, and physical status of persons who undergo such practice [Citation14]. At the same time that patients should be encouraged to self-quarantine before surgery, they should be encouraged to maintain exercise routines at home in order to minimize the detrimental effects of inactivity on the physical and psychological well-being [Citation15,Citation16]. The social effects caused by the COVID-19 pandemic are yet to be measured and its impact seemed to be aggravated within certain socio-economic groups [Citation14]. Yet, for the well-being of patients and providers, patients should be encouraged to self-quarantine for 14 days before surgery and maintain exercise routines to minimize the detrimental effects of such measures.
Conclusion
In conclusion, the COVID-19 infection rate in our series was low and about 50% of positive cases were asymptomatic. Our data suggest that a tertiary hospital can promulgate COVID-19 preoperative screening policies based on infection trends observed in the general population. Nevertheless, it is worth mentioning that the whole policy is questionable because the alleged benefits of universal preoperative RT-PCR screening may not materialize due to low disease prevalence and/or the limited accuracy of the test. The ‘take-home message’ of this investigation is that for the well-being of patients and providers, and in an attempt to overcome the limitations of the COVID-19 test, we should encourage patients to strictly self-quarantine for 14 days before surgery in addition to the performance of the test. Precautions need to be implemented in all cases due to the suboptimal sensitivity of the RT-PCR test. Hospitals cannot afford having a positive case and then hospital linked transmission.
Declaration of financial/other relationships
Drs. Jesus M. Villa and Tejbir S. Pannu reported no biomedical financial interests or potential conflicts of interest. Dr. Carlos A. Higuera reports the following: American Association of Hip and Knee Surgeons, Mid-American Orthopaedic Association, and Musculoskeletal Infection Society: Board or committee member; American Journal of Orthopedics, Journal of Arthroplasty, Journal of Hip Surgery, and Journal of Knee Surgery: Editorial or governing board; CD Diagnostics, Cymedica, Ferring Pharmaceuticals, Lyfstone, OREF, Orthofix, Inc., Stryker, and Zimmer: Research support; KCI: Paid consultant, Paid presenter or speaker, Research support; PSI: Stock or stock Options. Dr. Patel reports being paid consultant for Stryker and Zimmer. Dr. Raul J. Rosenthal reports being a paid consultant for Medtronics, Arthrex, and Diagnostic Green. Dr. Carla McWilliams reports being a paid consultant for Gilead. Chandra Kizer reported no biomedical financial interests or potential conflicts of interest.
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Declaration of interest
No potential conflict of interest was reported by the authors.
Declaration of funding
The current study did not receive any specific grant from funding agencies in the commercial, public, or not-for-profit sectors.
Acknowledgments
None stated
References
- Centers for Disease Control and Prevention. n.d.. ( accessed 2020 Aug 19). https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- Florida Department of Health. n.d.. ( accessed 2020 Aug 19). https://floridahealthcovid19.gov/#latest-stats
- Oudkerk M, Büller H. Diagnosis, prevention and treatment of thromboembolic complications in COVID-19. Radiology. 2020;77:1–7.
- Sutton D, Fuchs K, D’Alton M. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382(22):2163–2164.
- Gruskay JA, Dvorzhinskiy A, Konnaris MA. Universal testing for COVID-19 in essential orthopaedic surgery reveals a high percentage of asymptomatic infections. J Bone Joint Surg Am. 2020;102(16):1379–1388.
- The COVID Tracking Project at The Atlantic n.d. (accessed 2020 Aug 19). https://covidtracking.com/data/download
- The COVID Tracking project at The Atlantic. Data License. n.d. ( accessed 2020 Aug 19). https://covidtracking.com/about-data/license. 2020 Aug 19.
- Gershengorn HB, Warde PR, Nguyen DM. Pre-procedural screening for COVID-19 with nasopharyngeal polymerase chain reaction testing Hayley. Br J Anaesth. 2020;125(5):e422–e424.
- Ai T, Yang Z, Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2014;80:1–8.
- Kovoor JG, Tivey DR, Williamson P. Screening and testing for COVID-19 before surgery. ANZ J Surg. 2020;90(10):1845–1856.
- Florida Dept. of Health Cuts Ties With Quest Over Delay in Reporting 75K COVID Test Results. n.d.. ( accessed 2020 Sept 11). https://www.nbcmiami.com/news/local/florida-dept-of-health-cuts-ties-with-quest-over-delay-in-reporting-75k-covid-test-results/2286584/
- Delays in Reporting Results of COVID-19 Clinical Laboratory Tests Prompt Florida Governor to End SARS-CoV-2 Testing Contract with Quest Diagnostics. DARKDaily. n.d.. ( accessed 2020 Sept 11). https://www.darkdaily.com/delays-in-reporting-results-of-covid-19-clinical-laboratory-tests-prompt-florida-governor-to-end-sars-cov-2-testing-contract-with-quest-diagnostics/
- Lother SA. Preoperative SARS-CoV-2 screening: can it really rule out COVID-19?. Can J Anesth. 2020;67(10):1321–1326.
- Maugeri G, Musumeci G. Adapted physical activity to ensure the physical and psychological well-being of COVID-19 patients. J Funct Morphol Kinesiol. 2021 Jan 29; 6(1):13.
- Ravalli S, Musumeci G. Coronavirus outbreak in Italy: physiological benefits of home-based exercise during pandemic. J Funct Morphol Kinesiol.2020 May 7; 5(2):31. PMID: 33467247; PMCID: PMC7739427.
- Maugeri G, Castrogiovanni P, Battaglia G, et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. 2020 Jun 24;6(6):e04315. PMID: 32613133; PMCID: PMC7311901.