ABSTRACT
Background
Prevalence rates of patients with diabetes are growing across countries, and Bangladesh is no exception. Associated costs are also increasing, driven by costs associated with the complications of diabetes including hypoglycemia. Long-acting insulin analogues were developed to reduce hypoglycemia as well as improve patient comfort and adherence. However, they have been appreciably more expensive, reducing their affordability and use. Biosimilars offer a way forward. Consequently, there is a need to document current prescribing and dispensing rates for long-acting insulin analogues across Bangladesh, including current prices and differences, as a result of affordability and other issues.
Methods
Mixed method approach including surveying prescribing practices in hospitals coupled with dispensing practices and prices among community pharmacies and drug stores across Bangladesh. This method was adopted since public hospitals only dispense insulins such as soluble insulins free-of-charge until funds run out and all long-acting insulin analogues have to be purchased from community stores.
Results
There has been growing prescribing and dispensing of long-acting insulins in Bangladesh in recent years, now accounting for over 80% of all insulins dispensed in a minority of stores. This increase has been helped by growing prescribing and dispensing of biosimilar insulin glargine at lower costs than the originator, with this trend likely to continue with envisaged growth in the number of patients. Consequently, Bangladesh can serve as an exemplar to other low- and middle-income countries struggling to fund long-acting insulin analogues for their patients.
Conclusions
It was encouraging to see continued growth in the prescribing and dispensing of long-acting insulin analogues in Bangladesh via the increasing availability of biosimilars. This is likely to continue benefitting all key stakeholder groups.
1. Introduction
There is a growing prevalence of diabetes worldwide enhanced by global incidence rates rising by over 100% between 1990 and 2017, reaching to 22.94 million in 2017 [Citation1]. However, this is not universal with rates of type 2 diabetes falling in some countries in recent years with the introduction of preventative strategies [Citation2]. Overall, 463 million people world-wide had diabetes in 2019, with the vast majority (80%) coming from low-income and middle-income countries (LMICs) [Citation3]. As a result of this increase, the economic burden of diabetes is estimated to reach 2.2% of Gross Domestic Product by 2030 unless addressed [Citation3,Citation4]. Bangladesh is no exception to the general worldwide trend in the growing prevalence of diabetes. Currently, up to 8.4 million adults have diabetes in Bangladesh (8.1%), with prevalence rates expected to increase to 15.0 million by 2045 unless addressed [Citation5,Citation6]. Other authors have suggested higher prevalence rates at 13.0% of the population in Bangladesh by 2030 [Citation7]. Complications associated with diabetes are also increasing, enhanced by poor glycemic control and adherence to treatments [Citation5], thereby increasing the overall morbidity and mortality associated with non-communicable diseases (NCDs) in Bangladesh [Citation3,Citation8].
However, despite the efforts of the government in Bangladesh with initiating many NCD-related programs, there are concerns with their implementation and monitoring in practice [Citation8]. This includes concerns with available facilities, personnel and guidelines to adequately treat patients with coronary vascular disease (CVD) including hypertension and diabetes [Citation9–12]. This is a concern in view of the implications of the poor management of patients with diabetes on subsequent morbidity and mortality [Citation13]. For instance, poor management can increase the risk of CVD by up to threefold, with up to 30% of the patients with diabetes dying from CVD [Citation3,Citation14].
Consequently, there is a need to improve the care of these patients. This includes greater use of long-acting insulin analogues, developed to reduce hypoglycemia where this is a concern as well as improve patient convenience and compliance to treatment [Citation3,Citation15,Citation16]. However, there have been concerns with the additional costs of the long-acting insulin analogues versus neutral protamine hagedorn (NPH) and other insulins [Citation3,Citation17,Citation18]. This is important in Bangladesh, where diabetes patients have paid an average of 35,385 BDT (US$454) per year for their medicines versus only 1609 BDT (US$21) for those without diabetes [Citation19], medicines to manage NCDs in Bangladesh can be expensive by international standards [Citation20], and much of these costs are out-of-pocket [Citation21]. Consequently, an appreciable number of households in Bangladesh are forced to sell their assets or borrow money to fund treatments [Citation22]. This needs to be avoided if Bangladesh is to achieve its sustainable development goals for NCDs [Citation23].
We are aware a number of Government hospitals in Bangladesh only fund NPH and other similar insulins until the monies run out. Consequently, long-acting insulin analogues need to be purchased directly from community pharmacies and drug stores when prescribed in both public and private hospitals. Biosimilars, though, can help to appreciably lower the costs of biologic medicines [Citation24]. However, there have been concerns with hypoglycemia if patients are switched between different administrative devices with different characteristics when dispensed different originators and biosimilars [Citation25,Citation26]. This, though, has to be balanced against improved patient care and outcomes with long-acting insulin analogues. There have also been concerns that limited price reductions for biosimilars versus the originators in some countries will reduce the attractiveness of the market for biosimilars for long-acting insulin analogues in practice [Citation18,Citation27,Citation28]. Limited price differences between originators and biosimilars are a concern particularly in LMICs where there are high patient co-payments and lower costs for essential medicines can alleviate the need for households to sell their assets or borrow money to fund treatments for chronic diseases [Citation22].
In view of this, there is a need to document current prescribing and dispensing rates for long-acting insulin analogues across Bangladesh, including current prices and differences, to provide future guidance. This was the objective of this paper.
2. Methods
We undertook a mixed approach. This initially included collecting current prescribing data on insulins, including long-acting insulins, from five public and private hospitals among a representative sample of these hospitals across Bangladesh. Prescribing as opposed to utilization data was collected as long-acting insulin analogues are not dispensed in hospitals in Bangladesh, and patients typically have to purchase NPH and other insulins themselves from pharmacies and drug stores once supplies run out in public hospitals. Consequently, just collecting utilization data would give a false impression of current prescribing practices.
The information from hospitals was supplemented by a survey among a range of community pharmacies and drug stores across Bangladesh to assess dispensing and pricing patterns for different insulin glargine preparations, as well as different insulin types, e.g., long-acting insulin analogues versus other forms of insulin, in 2019 and 2020. The survey was conducted among pharmacies and drug stores since, as mentioned, patients typically purchase their medicines from these locations, especially long-acting insulin analogues, with hospital physicians the principal initiators and prescribers of insulin for patients with diabetes. Consequently, community pharmacies and drug stores can provide a more accurate picture of physician prescribing patterns for the different insulins, including both originator and biosimilar long-acting insulin analogues, than outpatient hospital pharmacies.
Only insulin glargine was broken down into the originator and biosimilar (100IU/ml) as this was the only long-acting insulin analog biosimilar routinely available in Bangladesh.
With respect to community pharmacies and drug stores, we adopted a similar approach to our recently conducted study on the impact of COVID-19 on the utilization, shortages and prices changes of pertinent medicines and equipment [Citation29,Citation30]. This included documenting actual changes in dispensing rates and prices based on invoices where available. Alternatively, we just documented impressions in view of the confidentiality of some the information being sought, especially surrounding current prices and discounts. In addition, we were not paying pharmacists for their time, similar to previous situations [Citation29,Citation30]. We did not undertake a sample size calculation since, to the best of our knowledge, no previous study has been conducted in this area to provide guidance on such calculations. However, our intention was to approach an appreciable number of pharmacies and drug stores throughout Bangladesh to provide a comprehensive picture, similar to our study with COVID-19 [Citation29].
Where pertinent, pricing data were converted to US$ for comparative purposes using current exchange rates (https://www.xe.com/currencyconverter/).
We did not seek ethical approval as this study did not involve patients. However, we sought approval from pharmacy managers and drug store owners before participation, with interviewees given the opportunity to refuse. This is in line with previous studies undertaken by the coauthors in similar areas and circumstances [Citation29–34]. Overall, 167 pharmacies were included in the study with different information sets provided depending on the information that could be supplied.
3. Results
We first discuss prescribing patterns among the five participating hospitals before discussing dispensing and pricing patterns from the 167 pharmacies providing this data.
depicts current prescribing patterns for long-acting insulins, including different insulin glargine preparations, among the five participating hospitals in Bangladesh. The prescribing of long-acting insulin analogues has increased in recent years, with long-acting insulin analogues more likely to be prescribed by endocrinologists reflecting their perceived benefits of improved patient outcomes and convenience versus NPH and other insulins. Non-endocrinologists are more likely to prescribe NPH and other insulins since these are provide free-of-charge in public hospitals until funds run out. However, even among non-endocrinologists, we have seen increased prescribing on long-acting insulin analogues in recent years.
Table 1. Current long-acting insulin prescribing patterns among target hospitals in Bangladesh
The long-acting insulin analog principally prescribed is insulin glargine, although there is growing prescribing of insulin detemir and insulin degludec (). Issues of affordability are typically discussed with patients during the consultation, with patients likely to follow the advice of their physician when obtaining their insulin from either pharmacies or drug stores. Affordability is a key issue as discussed by Islam et al. (2017) given the high expenditure on medicines among patients with diabetes in Bangladesh versus those without diabetes [Citation19]. However, there is still considerable prescribing of the originator in some hospitals due to concerns with other formulations ().
contains details of the surveyed pharmacies and drug stores including the response rates and locations in Bangladesh. The overall response rate was 66.8%.
Table 2. Details of pharmacies and drugs stored contacted and provided data in Bangladesh
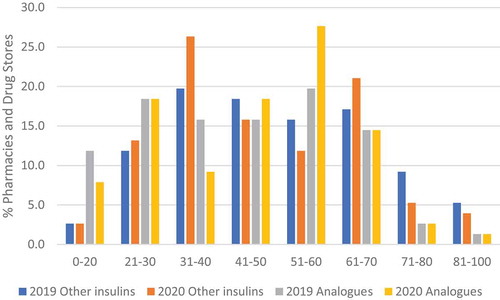
shows overall a similar utilization of insulin analogues vs. other insulins among 76 out of 82 pharmacies ( – first group) providing such data. The percentages in the x-axis represent the percentages of the different insulins dispensed in each pharmacy, i.e. analog versus other insulins, out of the total amount of insulin dispensed. These have been grouped into bands, i.e. 0% to 20%, 21% to 30%, 31% to 40% and 41% to 50%, etc., for comparative purposes. As seen in , the dispensing of the analogues increased in 2020 vs. 2019. The analogues are principally long-acting insulin analogues, and mainly insulin glargine, including both the originator and biosimilars. Similar to , there is considerable variation among the different pharmacies and drug stores in Rajshani and Dhaka regarding which insulin (analog and others) is being dispensed.
Figure 1. Dispensing patterns of different insulins among drug stores and pharmacies in Bangladesh 2019 and 2020
depicts differences in the dispensing patterns of originator vs. biosimilar insulin glargine among the first group of pharmacies and drug stores taking part (Group One – ). Again, the percentages in the x axis represent the percentages of the different insulin glargine preparations dispensed in each pharmacy, i.e., originators vs. biosimilars, out of the total amount of insulin glargine dispensed. These have again been grouped into similar bands for comparative purposes. As seen in , there was greater dispensing of biosimilars versus originators, with again dispensing rates of biosimilars marginally increasing in recent years.
Figure 2. Dispensing patterns of different insulin glargine preparations among 79 of the 82 Pharmacies and Drug Stores 2019 and 2020
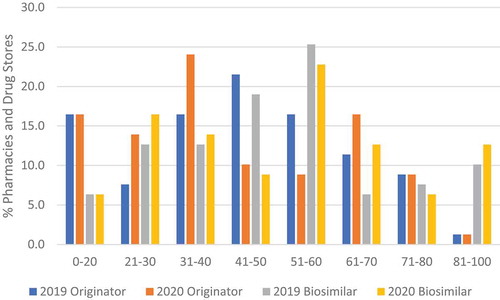
The considerable differences in the dispensing patterns among these 82 pharmacies and drug stores probably reflect appreciable differences in the prescribing habits of local physicians coupled with discussions and issues regarding affordability.
The biosimilars were the principal preparations of insulin glargine dispensed in a further set of 15 pharmacies (Group 3) accounting for just under 90% of all insulin glargine dispensed (89.4% in 2019 and 88.9% in 2020). Overall, there was a 16.7% increase in the number of insulin glargine packs dispensed in these 15 pharmacies between 2019 and 2020.
documents the typical selling prices for the different insulin glargine preparations among 85 different pharmacies in Bangladesh (Groups 2, 3, and 4), with an appreciable price reduction for some biosimilars.
Table 3. Typical selling prices for different insulin glargine preparations among 85 pharmacies and drug stores in Bangladesh
Among the 167 pharmacies and drug stores surveyed, price rises were seen for the different insulin glargine preparations in 2020 vs. 2019 among 10.8% of them, which was greatest for the biosimilars (11.3% vs. 10.3%). However, there was typically no change in prices in the majority of pharmacies and drug stores surveyed (79.3%) in recent years, with reductions noted in just 9.8% of the pharmacies and drug stores, greatest for the originator (13.8%).
contains current prices of common foods in Bangladesh, with workers, such as those working in garment factories of US$2 to 4/day [Citation35]
Table 4. Prices of typical foods in Bangladesh (Source: M Haque personal communication)
4. Discussion
We believe this is the first study to assess prescribing and dispensing patterns for the different insulins, especially long-acting insulin glargine, among key stakeholder groups in Bangladesh. The 66.8% response rate among participating pharmacies and drug stores is encouraging given the confidential nature of some of the information requested. This rate is similar to our low refusal rate in previous studies regarding medicines for patients with COVID-19 in Bangladesh and across Asia [Citation29,Citation30].
It is encouraging to see the growing prescribing and dispensing of long-acting insulin analogues in Bangladesh in view of their impact on lowering rates of hypoglycemia, as well as improving comfort for patients [Citation3,Citation16], with dispensing rates reaching over 80% of all insulins dispensed in a minority of pharmacies (). Overall, long-acting insulin analogues typically now account for between 40% and 60% of the insulins dispensed, mirroring some of the prescribing patterns seen (). This is despite issues of affordability among patients in Bangladesh, with sometimes catastrophic consequences when family members become ill [Citation22] given average salaries of some workers at US$2 4/day [Citation35], the cost of medicines, such as insulins () and those of common foodstuffs (). Issues of affordability, though, are reflected in higher rates of prescribing and dispensing of lower cost biosimilars ( and ) among physicians, pharmacies and drug stores in Bangladesh, with rates approaching 90% among one group of pharmacies (Group 3 – ). These findings are encouraging and provide direction to other LMICs where utilization of long-acting insulin analogues is low, e.g., long-acting insulin analogues are typically not reimbursed or funded within the public health system in Brazil or among a number of African countries due to issues of affordability versus NPH and other insulins as well as perceived limited health gain [Citation17,Citation18,Citation36,Citation37].
The typically greater use of biosimilars versus the originator in our study is encouraging as this should enhance competition among biosimilar manufacturers as seen with recent biosimilars in Europe, which helped to further their lower prices [Citation24,Citation38]. As a consequence, Bangladesh can serve as an exemplar to other countries, especially LMICs, as we see growth in the prescribing of lower cost insulin glargine biosimilars continuing to further benefit patients in the future. There could be additional discounts if the prescribing and dispensing of insulin glargine are threatened by an appreciable growth in the prescribing of insulin detemir and insulin degludec. However, this is unlikely if considerable price differences exist.
Overall, lower cost biosimilars should be welcomed by all key stakeholder groups as this will help with issues of affordability, allowing more patients in Bangladesh and wider to access long-acting insulin analogues to improve their care [Citation3,Citation39]. This, in turn, helps decrease current rates of hypoglycemia and associated consequences. Alongside this, the authorities in Bangladesh need to increase the number of ambulatory care facilities to better diagnose and manage patients with diabetes in the first place given current concerns as well as rising rates of diabetes [Citation16]. In addition, ensure adequate supplies of equipment are available to allow patients to monitor their blood glucose levels at home to prevent complications as this is a concern among LMICs [Citation3,Citation36]. We will continue to monitor this.
We are aware of a number of limitations with this study. These include only approaching a limited number of hospitals. However, this was deliberate for the reasons stated. In addition, we were unable to obtain exact details on changes in the utilization and prices of pertinent insulins from all the pharmacists visited due to issues of confidentiality and having the data readily to hand. However, we are confident with our findings, and believe these can help guide future strategies in Bangladesh and wider to improve the management of patients with diabetes requiring insulin.
5. Conclusion
In conclusion, we do see growing use of long-acting insulin analogues in Bangladesh, which reflects increasing recognition of their role and value in managing patients with diabetes. This is increasingly biosimilars at lower prices in view of issues of affordability in Bangladesh. Increased competition should help to further lower prices further enhancing access to long-acting insulin analogues with resultant benefits to patients, and we will be monitoring this. Alongside this, there is a need for additional educational initiatives among pertinent physicians to enhance their prescribing of long-acting insulin analog biosimilars to further reduce rates of hypoglycemia. In addition, strengthen the health system generally in Bangladesh to improve diagnosis and management of patients with diabetes given the expected increase in their numbers in the coming years.
Declaration of funding
This analysis was commissioned and paid for by the World Health Organization. The authors are totally responsible for the views expressed in this paper, and they do not necessarily represent the decisions, policy or views of the World Health Organization
Declaration of interest
The authors have no relevant conflicts of interest to declare
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Data sharing
The data that support the findings of this study are available from the corresponding author, BG, upon reasonable request.
Acknowledgments
None stated
References
- Liu J, Ren Z-H, Qiang H, et al. Trends in the incidence of diabetes mellitus: results from the global burden of disease study 2017 and implications for diabetes mellitus prevention. BMC Public Health. 2020;20(1):1415. .
- Magliano DJ, Islam RM, Barr ELM, et al. Trends in incidence of total or type 2 diabetes: systematic review. BMJ 2019;366:l5003–l.
- Chan JCN, Lim LL, Wareham NJ, et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2021;396(10267):2019–2082.
- Bommer C, Sagalova V, Heesemann E, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41(5):963–970.
- Afroz A, Zhang W, Wei Loh AJ, et al. Macro- and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab Syndr. 2019;13(5):2939–2946.
- International Diabetes Federation. IDF atlas ninth edition. 2019. Available from: https://diabetesatlas.org/upload/resources/material/20200106_152211_IDFATLAS9e-final-web.pdf
- Bhuyan KC, Fardus J. Factors responsible for diabetes among adult people of Bangladesh. Am J Biomed Sci & Res. 2019;2(4):137–142.
- Biswas T, Pervin S, Tanim MIA, et al. Bangladesh policy on prevention and control of non-communicable diseases: a policy analysis. BMC Public Health. 2017;17(1):582.
- Biswas T, Haider MM, Das Gupta R, et al. Assessing the readiness of health facilities for diabetes and cardiovascular services in Bangladesh: a cross-sectional survey. BMJ Open. 2018;8(10):e022817.
- Chowdhury MZI, Rahman M, Akter T, et al. Hypertension prevalence and its trend in Bangladesh: evidence from a systematic review and meta-analysis. Clin hyperten. 2020;26(1):10.
- Fottrell E, Ahmed N, Shaha SK, et al. Distribution of diabetes, hypertension and non-communicable disease risk factors among adults in rural Bangladesh: a cross-sectional survey. BMJ Glob Health. 2018;3(6):e000787.
- Islam SMS, Islam MT, Islam A, et al. National drug policy reform for noncommunicable diseases in low-resource countries: an example from Bangladesh. Bull World Health Organ. 2017;95(5):382–384.
- Maffi P, Secchi A. The burden of diabetes: emerging data. Develop ophthalmol. 2017;60:1–5.
- Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics-2019 update: a report from the American heart association. Circulation. 2019;139(10):e56–e528.
- Pedersen-Bjergaard U, Kristensen PL, Beck-Nielsen H, et al. Effect of insulin analogues on risk of severe hypoglycaemia in patients with type 1 diabetes prone to recurrent severe hypoglycaemia (HypoAna trial): a prospective, randomised, open-label, blinded-endpoint crossover trial. Lancet Diabetes Endocrinol. 2014;2(7):553–561.
- Rys P, Wojciechowski P, Rogoz-Sitek A, et al. Systematic review and meta-analysis of randomized clinical trials comparing efficacy and safety outcomes of insulin glargine with NPH insulin, premixed insulin preparations or with insulin detemir in type 2 diabetes mellitus. Acta Diabetol. 2015;52(4):649–662. .
- Almeida P, Silva TBC, De Assis Acurcio F, et al. Quality of life of patients with type 1 diabetes mellitus using insulin analog glargine compared with nph insulin: a systematic review and policy implications. Patient. 2018;11(4):377–389.
- Ewen M, Joosse HJ, Beran D, et al. Insulin prices, availability and affordability in 13 low-income and middle-income countries. BMJ Glob Health. 2019;4(3):e001410.
- Shariful Islam SM, Lechner A, Ferrari U, et al. Healthcare use and expenditure for diabetes in Bangladesh. BMJ Glob Health. 2017;2(1):e000033–e.
- Kasonde L, Tordrup D, Naheed A, et al. Evaluating medicine prices, availability and affordability in Bangladesh using World health organisation and health action International methodology. BMC Health Serv Res. 2019;19(1):383.
- Afroz A, Alam K, Ali L, et al. Type 2 diabetes mellitus in Bangladesh: a prevalence based cost-of-illness study. BMC Health Serv Res. 2019;19(1):601.
- Rahman MM, Zhang C, Swe KT, et al. Disease-specific out-of-pocket healthcare expenditure in urban Bangladesh: a Bayesian analysis. PloS One. 2020;15(1):e0227565–e.
- United Nations. Progress towards the sustainable development goals. 2017. [cited 2021 Feb 24]. Available from: https://www.un.org/ga/search/view_doc.asp?symbol=E/2017/66&Lang=E
- Jensen TB, Kim SC, Jimenez-Solem E, et al. Shift from adalimumab originator to biosimilars in Denmark. JAMA Intern Med. 2020;180(6):902–903.
- Chapman SR, Fitzpatrick RW, Aladul MI. Knowledge, attitude and practice of healthcare professionals towards infliximab and insulin glargine biosimilars: result of a UK web-based survey. BMJ Open. 2017;7(6):e016730.
- Lothian Formulary. 6.1.1 Insulins. 2020. [cited 2021 Feb 6]. Available from: https://www.ljf.scot.nhs.uk/LothianJointFormularies/Adult/6.0/6.1/6.1.1/Pages/default.aspx
- Greener M. Why isn’t the NHS making the most of biosimilar insulin? Prescriber August. 2019; 21–24.
- Godman B. Biosimilars are becoming indispensable in the management of multiple diseases although concerns still exist. Bangladesh J Med Sci. 2021;20(1):5–10.
- Haque M, Islam S, Iqbal S, et al. Availability and price changes of potential medicines and equipment for the prevention and treatment of COVID-19 among pharmacy and drug stores in Bangladesh; findings and implications. Bangladesh J Med Sci. 2020;19:S36–S50.
- odman B, Haque M, Islam S, et al. Rapid assessment of price instability and paucity of medicines and protection for COVID-19 across Asia: findings and public health implications for the future. Front Public Health. 2020;8:744.
- Moon JC, Godman B, Petzold M, et al. Different initiatives across Europe to enhance losartan utilization post generics: impact and implications. Front Pharmacol. 2014;5:219.
- Moorkens E, Godman B, Huys I, et al. The expiry of Humira ® market exclusivity and the entry of adalimumab biosimilars in Europe: an overview of pricing and national policy measures. Front Pharmacol. 2021;11:1993.
- ad M, Salem A, Oortwijn W, et al. Mapping of current obstacles for rationalizing use of medicines (CORUM) in Europe: current situation and potential solutions. Front Pharmacol. 2020;11:144.
- Sefah I, Ogunleye O, Essah D, et al. Rapid assessment of the potential paucity and price increases for suggested medicines and protection equipment for COVID-19 across developing countries with a particular focus on Africa and the implications. Front Pharmacol. 2021;11:2055.
- Salary Explorer. Average salary in Bangladesh 2021. [cited 2021 Feb 4]. Available from: http://www.salaryexplorer.com/salary-survey.php?loc=18&loctype=1
- Godman B, Basu D, Pillay Y, et al. Ongoing and planned activities to improve the management of patients with type 1 diabetes across Africa; implications for the future. Hosp Pract. 2020;48(2):51–67.
- alungia CA, Mwale M, Sondashi IS, et al. Availability of essential antihypertensive and antidiabetic medicines in public health facilities in Lusaka District, Zambia. Med J Zambia. 2017;44(3):140–148.
- Davio K. After biosimilar deals, UK spending on adalimumab will drop by 75%. 2018. [cited 2021 Feb 6]. Available from: https://www.centerforbiosimilars.com/news/after-biosimilar-deals-uk-spending-on-adalimumab-will-drop-by–75
- Semlitsch T, Engler J, Siebenhofer A, et al. (Ultra-)long-acting insulin analogues versus NPH insulin (human isophane insulin) for adults with type 2 diabetes mellitus. Cochrane Database Systemat Rev. 2020;11:Cd005613.
