ABSTRACT
Introduction: Although in-person hospitalist presence, increasingly staffed by dedicated nocturnists, has become the norm overnight in the hospital, the scope of nocturnist practice and typical workload has not been defined. This study examines the clinical responsibilities and patient safety perceptions of hospitalists who work night shifts in the United States.
Methods: In the fall of 2019, a cross-sectional, web-based survey was administered to physician and nurse practitioner/physician assistant (NP/PA) hospitalists who work night shifts. The questionnaire assessed night staffing structure, typical responsibilities, patient volume, perceptions of safety overnight, as well as demographic information. The survey was posted on the Society of Hospital Medicine (SHM) Hospital Medicine Exchange (HMX) Online Discussion Forum. Additionally, the survey was distributed by ‘snowball method’ by respondents to other night hospitalists. Responses were collected anonymously.
Results: Of the 167 respondents, 157 reported working night shifts. There was at least one respondent from 32 different states. In addition to performing admissions to medicine services and covering inpatients, night hospitalists cover ICU patients, participate in RRT/Code teams and procedure teams, perform consults, participate in medical education, and take outpatient calls. Across institutions, there was a large distribution in numbers of patients covered in a night shift; however, patient volume fell into typical ranges: 5–10 admissions for physicians, 0–6 admissions for NP/PAs, and 25–75 patient cross-coverage census. When physicians perform more than five admissions per night, hospitalists were less likely to agree that they could provide safe care (88% vs. 63%, p = 0.0006).
Conclusions: This is the first national study to examine the clinical responsibilities of hospitalists working overnight. Overnight responsibilities are heterogeneous across institutions. As hospitals are increasingly employing nocturnists, more research is needed to guide night staffing and optimize patient safety.
Introduction
Most hospitals and hospital medicine groups deploy hospitalists overnight, and nocturnists (hospitalists who primarily work night shifts) are increasingly being hired to fill this role[Citation1]. Hospitalist/nocturnist coverage of overnight shifts has become essential due to residency work hour limitations, increased attending-level trainee supervision requirements, and a trend toward on-site coverage of hospital wards overnight [Citation2-5]. In one tertiary care hospital staffed exclusively by nocturnists, there was no difference in hospitalization-relevant outcomes for patients admitted overnight, compared to those admitted during the day [Citation6]. Also, the introduction of nocturnist nurse practitioners and physician assistants (NP/PAs) demonstrated similar outcomes to traditional resident overnight coverage [Citation7].
The presence of academic nocturnists has been studied with regard to education and supervision of trainees; while nocturnist availability did not specifically improve outcomes or dramatically improve revenue generation [Citation5], residents perceived that the addition of nocturnist supervision did improve the educational experience [Citation4], though possibly reducing decision-making autonomy [Citation8,Citation9]. In a large survey of Internal Medicine residents, those working in hospitals with nocturnists perceived fewer barriers to contacting supervising physicians overnight; however, residents did note that the nocturnists’ own workload was sometimes a barrier to supervision [Citation10].
Nocturnist workload has not been well studied. The negative impacts of higher census for day-shift hospitalists have been evaluated and included increased costs and longer length-of-stay [Citation11,Citation12]; however, the ideal scope and volume of work for a night hospitalist have not been quantified. Moreover, in addition to patient census, patient severity [Citation13], the number of pages, and rapid response team (RRT) activation/intensive care unit (ICU) transfers [Citation14] also contribute to nocturnist workload.
The Society of Hospital Medicine (SHM) publishes a biennial survey of hospitalist leaders, which includes information about nocturnist staffing, salary differentials, and shift number differentials overnight; however, information about workload and overnight responsibilities is not covered [Citation1]. Due to an absence of published data regarding typical patient volumes, scope of practice, and staffing structure, nocturnists and hospitalist service leaders alike turn to word-of-mouth accounts and anecdotes to determine best overnight hospital staffing practices. This study is an initial examination of the experiences of nocturnist physicians and NP/PAs.
Methods
The Night Medicine Special Interest Group of SHM convened a panel of members to survey hospitalists who work night shifts. The panel included nocturnist physicians and NP/PAs with practice experience in a variety of settings, including academic and community hospitals. Members reviewed SHM’s prior validated national hospitalist survey [Citation1] and identified gaps in published information about overnight care. Based on the authors’ expertise/leadership as nocturnists and identified unknowns in the field of night medicine, survey elements were suggested to obtain specific information about night hospitalist work. Survey items to be included were determined by consensus, first round via e-mail, followed by virtual phone meeting. The initial questionnaire was pretested on a small group of night hospitalists for validity, with feedback incorporated into the final instrument.
The study was reviewed by an author’s institutional review board and was determined to be an exempt protocol. After receiving and letter introducing the survey, respondents acknowledged consent to participate by proceeding to the questionnaire.
Survey instrument
A 27-item REDCap survey instrument was developed, including items about night staffing structure, volume of patients, perceived acuity, perceived patient safety, and demographic questions. Respondents selected the types of clinicians performing overnight work, selecting all that apply (daytime hospitalists covering overnight shifts, dedicated nocturnists, NP/PAs, moonlighting residents/fellows, and other). It asked about typical shift duration, as well as whether the hospital also utilized a ‘swing’ shift, defined as a shift that starts in the late afternoon and ends around midnight. The survey tool used branch logic collecting data about the types and quantity of work performed on the night shift only from hospitalists who report that they worked night shifts. It also used branch logic to include survey items about NP/PA workload only from those who indicated an overnight NP/PA workforce at their hospital. Respondents selected items from a list of possible primary and secondary tasks performed during the night shift. They also selected from a range for average number of admissions performed on the night shift (0, 1–5, 6–10, 11–15, 16–20, and more than 20) as well as the typical range of cross-coverage patient volume (none, less than 25, 25–50, 51–75, 76–100, 101–150, and more than 150). Respondents were asked to select the subjective acuity of their patients (very straightforward/not complicated, sometimes complicated but mostly straightforward, mostly complicated/sick, and very high acuity/ICU level) and a typical range of time it took to complete an admission. They indicated how often overnight admissions had to be held over for daytime providers and whether there was backup available if a nocturnist is overwhelmed by workload.
Night hospitalists were asked to select a range for number of admissions (less than 5, 5–6, 7–8, 9–10, 11–15, 16–20, more than 20, and not applicable) and cross-coverage census (less than 25, 25–50, 51–75, 76–100, 101–150, more than 150, and not applicable) they felt physicians and NP/PAs could safely manage ‘if there are no additional responsibilities’ while ‘still providing safe, high-quality care.’ The survey included a Likert-type item, ‘During my night shift I feel that I can safely care for the volume and acuity of patients for whom I am responsible,’ (strongly agree, agree, unsure, disagree, and strongly disagree).
Demographic items included questions about location by state, hospital position [physician, NP/PA, physician or NP/PA leader, administrator, and locum tenens (select all that apply)], and the type of entity that employs hospitalists. It also asked the respondent to indicate their involvement in medical education. All responses were anonymous, and identification of hospital or city was not requested to further preserve the anonymity.
Survey distribution
As there is no comprehensive list of night hospitalists, and nocturnists are sometimes not included in hospital faculty directories, several sampling methods were used in order to reach the highest number of night shift workers possible. The survey was posted on the SHM online community platform (HMX) as well as the Night Medicine interest group platform, followed by three additional posts requesting that night hospitalists complete the survey. Because many night hospitalists are not active in this community, a ‘snowball’ sampling technique was also used, whereby panel members distributed the survey by e-mail to a convenience sample of night hospitalists in their clinician networks. All respondents were then asked to also forward the survey to night hospitalists at other institutions. The survey site remained open and available for completion for 2 months.
Statistical analysis
Results were analyzed using REDCap software and Microsoft Excel. Descriptive statistics were performed. For the Likert-type question, selections of ‘strongly agree’ and ‘agree’ were collapsed to a single value of ‘agree’ to compare proportions between study groups, and a chi-squared test was performed using MedCalc Statistical Software version 19.2.6 (MedCalc Software bv, Ostend, Belgium; https://www.medcalc.org; 2020).
Results
A total of 167 individuals completed the survey, and of these, 157 respondents reported working night shifts. One hundred and fifty-one (and 143 who work night shifts) responded to all survey items. One hundred and eleven identified as physicians, 17 as physician leaders, 31 as NP/PAs, 8 as NP/PA leaders, and 4 as hospital administrators. One individual identified as locum tenens. There was at least one respondent from 32 different states in the US: of the 131 who answered the question, 41% were from the Northeastern US, 29% from the South, 15% from the Midwest, and 13% from the West. Large percentages were from New York (13%), Massachusetts (14%), and Virginia (11%), and 2 individuals indicated state ‘not applicable.’ More than half of respondents reported working exclusively on non-teaching services (24%) or in non-teaching hospitals (27%). Forty-six percent report working on both teaching and non-teaching services. Hospitalists were employed by hospitals (57%), universities (27%), private medical groups (6%), multi-state hospitalist management companies (5%), and private local/regional hospitalist-only medical groups (4%).
Night staffing
Of the 167 respondents, 114 indicated the utilization of more than one type of night staff. Seventy-six percent indicated that night shifts were covered by dedicated nocturnists, 57% used daytime hospitalists, and 53% had NP/PAs overnight. Moonlighting residents/fellows were selected by 31% of respondents, and 2% selected ‘other.’ Most reported a 12-h shift (69%), with another 22% reporting 9–11-h shifts. Half of respondents also reported utilization of a swing shift (a shift that starts in the afternoon or early evening and ends around midnight) staffed every night, and another 17% reported having a swing shift at least some nights.
Scope of overnight work
The clinicians who reported working night shifts (N = 157) were asked about their primary and secondary responsibilities overnight, and 148 completed this item. They identified their primary responsibilities by selecting the activities performed: 99% admit patients to medical services, 95% cross-cover inpatients, 29% admit patients to non-medical services, 28% admit and cover ICU patients, 28% triage to medical services, and 7% admit and cover rehab patients. Seven percent selected ‘other’ primary responsibilities which included supervision of trainees and NP/PAs, RRT/Code team coverage, palliative care/hospice unit coverage, observation unit coverage, and procedures. Reported secondary responsibilities, or tasks performed during the night shift in addition to their primary responsibilities, included performing consults (83%), RRT/Code team (68%), medical education (28%), triage to medical services (21%), procedure team (9%), outpatient calls for primary care or nursing home (9%), telemedicine (3%), and other (2%). Ninety-one percent of hospitalists report that when they are admitting patients they also have other responsibilities overnight.
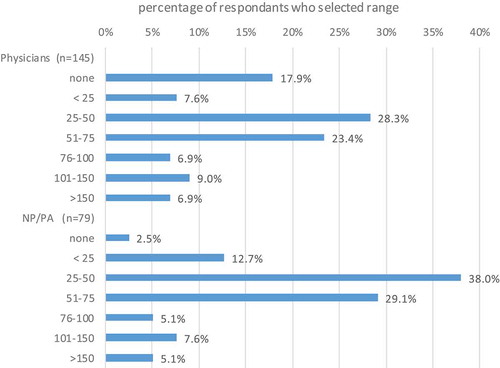
Of the night shift clinicians (N = 157), 147 answered the survey item about the average number of admissions performed by physicians. The night shift clinicians who indicated their hospital had NP/PA staff overnight (N = 83) were also asked about admissions performed by NP/PAs overnight, and 79 individuals responded to this item. Respondents selected a typical range () for the number of overnight admissions performed. Most physicians typically complete 6–10 (48%), followed by 1–5 admissions per shift (42%). Seven percent complete 11–15 admissions and only 1% indicated more than 15. Most NP/PAs typically perform 1–5 admissions per shift (56%), followed by zero admissions (24%). Another 19% report performing 6–10 admissions per shift, and 1% reported completing 11–15%. Respondents (N = 148) reported that it usually takes 30–60 min (42%) or 1–2 h (50%) to complete one admission. Two percent take less than 30 min and 3% take more than 2 h.
Figure 1. Typical number of admissions per night
Respondents also reported a typical range for the overnight cross-coverage census (). Physicians most frequently cover 25–50 patients (28%), followed by 51–75 patients (23%). Some are responsible for substantially more: 7% cover 76–100, 9% cover 101–150, and 7% cover over 150 patients. Eighteen percent of physicians do not cross-cover patients. NP/PAs typically cross-cover 25–50 patients (38%) or 51–75 patients (29%). A smaller proportion cover less than 25 (13%), and some NP/PAs cover over 75 patients per night (5% cover 76–100, 8% cover 101–150, and 5% cross-cover more than 150 patients).
Perception of acuity and workload
Night hospitalist indicated their perception of patient acuity by selecting an option from a list of choices. Less than 1% felt their typical patients were ‘very straightforward/not complicated,’ 42% felt they were ‘sometimes complicated but mostly straightforward,’ 55% felt they were ‘mostly complicated/sick,’ and few (2%) felt their patients were ‘very high acuity/ICU level care.’ When asked ‘how often are overnight admissions held over for daytime providers because the night shift did not have time to complete them?’ 3% reported ‘all the time,’ 8% reported ‘most of the time,’ 26.2% reported ‘sometimes,’ 52% reported ‘rarely,’ and 11% reported ‘never.’
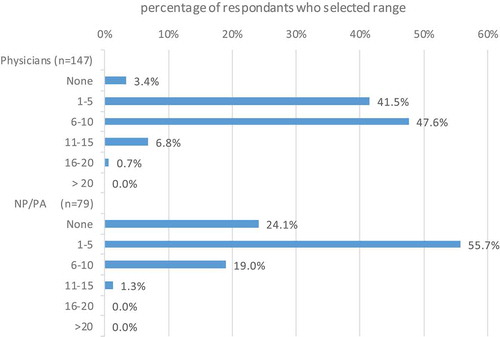
Respondents were asked about how many patients they feel physicians and NP/PAs can admit and cross-cover ‘if there are no additional responsibilities’ while ‘still providing safe, high-quality care.’ For physicians (N = 145), most selected a range of 5–10 admissions [5–6 (22%), 7–8 (30%), 9–10 (27%)]. In settings with NP/PAs (n = 78), most selected a safe range of 0–6 admissions per shift [less than 5 (42%), 5–6 (23%)]. With regard to cross-coverage patient volumes, most felt that physicians can cross-cover between 25 and 50 patients (29%) or between 51 and 75 patients (27%) safely. Most also felt that NP/PAs could safely cover either 25–50 patients (31%) or 51–75 patients (31%).
When given the statement ‘During my night shift I feel that I can safely care for the volume and acuity of the patients for whom I am responsible,’ 75% agreed or strongly agreed (50% and 25%, respectively). Others, however, disagreed (10%), strongly disagreed (1%), or were unsure (14%). When comparing those who reported physicians perform up to five admissions per night (N = 66) with those who admit more than five patients (N = 81), those who performed less admissions were more likely to agree that they could provide safe care (88% vs. 63%, p = 0.0006). There was no significant difference in the perception that safe care was provided between NP/PAs who perform five or less admissions (N = 63) verses more than five admissions (N = 16) (81% vs. 63%, p = 0.1), between physicians cross covering as smaller census (50 or fewer patients, N = 78) versus a higher census (more than 50, N = 67) (73% vs. 75%, p = 0.8), and between NP/PAs cross covering smaller (N = 42) versus larger census (N = 37) (83% vs. 70%, p = 0.2). Also, there were no observable differences in perceptions of safety between those reporting swing shift staffing most/always (N = 96) versus sometimes/never (N = 63) (68% vs. 63%, p = 0.5).
Discussion
This initial study of nocturnist responsibilities is important because it addresses the typical workload of overnight hospitalists by directly surveying the hospitalists performing this work. This survey included both physician and NP/PA respondents from different parts of the country and different types of hospitals. The survey revealed that the scope of practice for overnight hospitalist is heterogeneous, encompassing many different responsibilities. Beyond admitting and cross-coverage of inpatients, some night hospitalists cover ICU patients, are part of procedure teams and code/RRT teams, supervise and teach, answer calls regarding outpatients, triage, and transfer patients, among other tasks.
Most of the night hospitalists surveyed felt that physicians can safely admit 5–10 patients, and NP/PAs can admit 1–6 patients overnight – if they do not have other responsibilities. Both physician and NP/PAs felt that, with no additional responsibilities, they could safely cross-cover somewhere between 25 and 75 patients. Reassuringly, hospitalists generally are covering the patient volumes they feel to be appropriate though they do have additional responsibilities that simultaneously occupy their attention. Therefore, in this typical practice setting, the ideal patient volumes should perhaps be skewed lower. The perception of workload on the night shift is also affected by patient acuity, number of pages, and RRT activations [Citation13,Citation14], so the ideal patient census to ensure patient safety is uncertain and clearly does not have a one-size-fits-all solution. For instance, we found that more than 25% of night hospitalists provide intensive care coverage, so these clinicians would likely need to care for fewer patients. Fortunately, most respondents of this study felt like they could provide safe care for their patients though a substantial minority (25%) disagreed or were unsure if they could provide safe care. Fewer admissions per physician were significantly associated with the feeling that safe, high-quality care was provided. We did not find similar differences with NP/PA admissions or across different cross-coverage volumes though this study was not designed for this purpose.
The results of this survey help nocturnists to know whether their job responsibilities are reasonable compared to other institutions. Moreover, when night hospitalists report concerns about safe workloads, hospital leaders can use these results to determine if the overnight patient volumes are typical and advocate for their staff accordingly. Up to 11% of respondents reported that overnight admissions are held over for daytime providers ‘all’ or ‘most of the time,’ which may further indicate inadequate overnight staffing. Further guidelines as to the ideal patient volume per night clinician, factoring in acuity, are needed.
There are several limitations to this study. First, despite respondents from 32 different states, the Northeast had increased representation. This study also did not seek to specifically include the experiences of night hospitalists outside the US. This may impair the applicability of these findings to clinicians outside the overrepresented settings. Future work should obtain a more representative sample of hospitalists who cover night shifts, including locum tenens clinicians and NP/PAs. This survey did not attempt to quantify the time night hospitalists spend on the variety of tasks required of them or whether these tasks represent billable work. Nor did it attempt to determine objective quality metrics based on workload.
More research is also needed to address the perceptions of burnout, especially related to the physiologic and health challenges of night hospitalist work [Citation15], and the need for many nocturnists to also be present for daytime obligations (meetings, teaching, and coverage of undesirable daytime shifts). Sleep deprivation among nocturnists is also a risk factor for medical errors[Citation15], as are multitasking and frequent interruptions [Citation16,Citation17], and further work is needed to understand and optimize night staffing to mitigate these risks.
Conclusions
This study is an important first step in understanding night hospitalist workload. This is the first national study to identify typical ranges for number of admissions and cross-coverage census, as well as nocturnists’ breadth of practice and perceptions of safety. The trend toward employing dedicated nocturnists is on the rise, and the field of hospital medicine needs to have a better understanding of the perspectives of the clinicians who perform this work.
Declaration of funding
Transparency No funding was received to produce this article
Declaration of financial/other relationships
The authors have no disclosures or conflicts of interest.
Reviewer disclosure
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Declaration of interest
No potential conflict of interest was reported by the author(s).
Supplemental Material
Download MS Word (26.2 KB)Supplementary material
Supplemental data for this article can be accessed here.
References
- Society of Hospital Medicine Practice Analysis Committee. State of hospital medicine report: 2020 report based on 2019 data. Englewood, CO and Philadelphia, PA: Medical Group Management Association and Society of Hospital Medicine; 2020.
- Nasca TJ, Day SH, Amis ES Jr., et al. The new recommendations on duty hours from the ACGME task force. N Engl J Med. 2010;363(2):e3.
- Shulkin DJ. Like night and day – shedding light on off-hours care. New Engl J Med. 2008;358(20):2091–2093.
- Trowbridge RL, Almeder L, Jacquet M, et al. The effect of overnight in-house attending coverage on perceptions of care and education on a general medical service. J Grad Med Educ. 2010;2(1):53–56.
- Gonzalo JD, Kuperman EF, Chuang CH, et al. Impact of an overnight internal medicine academic hospitalist program on patient outcomes. J Gen Intern Med. 2015;30(12):1795–1802.
- Khanna R, Wachsberg K, Marouni A, et al. The association between night or weekend admission and hospitalization-relevant patient outcomes. J Hosp Med. 2011;6(1):10–14.
- Johnson SA, Ciarkowski CE, Lappe KL, et al. Comparison of resident, advanced practice clinician, and hospitalist teams in an academic medical center: association with clinical outcomes and resource utilization. J Hosp Med. 2020;15(12):709–715.
- Farnan JM, Burger A, Boonyasai RT, et al. Survey of overnight academic hospitalist supervision of trainees. J Hosp Med. 2012;7(7):521–523. .
- Devendra GP, Ortiz GM, Haber LA. By the light of day: quality, safety, and education during the overnight admission handoff. Cureus. 2019;11(4):e4529.
- Catalanotti JS, O’Connor AB, Kisielewski M, et al. Barriers to accessing nighttime supervisors: a national survey of internal medicine residents. J Gen Intern Med. 2021. DOI:https://doi.org/10.1007/s11606-020-06516-4
- Michtalik HJ, Yeh HC, Pronovost PJ, et al. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med. 2013;173(5):375–377.
- Elliott DJ, Young RS, Brice J, et al. Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med. 2014;174(5):786–793.
- Hsu NC, Yang MC, Chang RE, et al. Patient severity matters for night-shift workload for internal medicine residents in Taiwan. BMC Health Serv Res. 2014;14:587.
- Bates RE, Kesselring GM, Breunig MJ, et al. Overnight cross-coverage on hospital medicine services: perceived workload based on patient census, pager volumes, and patient acuity. Hosp Pract (1995). 2020;48(2):108–112.
- Schaefer EW, Williams MV, Zee PC. Sleep and circadian misalignment for the hospitalist: a review. J Hosp Med. 2012;7(6):489–496.
- Rosenthal L. Enhancing communication between night shift RNs and hospitalists: an opportunity for performance improvement. J Nurs Adm. 2013;43(2):59–61.
- Weigl M, Muller A, Holland S, et al. Work conditions, mental workload and patient care quality: a multisource study in the emergency department. BMJ Qual Saf. 2016;25(7):499–508.