Abstract
Rabies is a devastating viral disease affecting the central nervous system. The fatality rate is very high compared to other viral diseases. Inadequate vaccination, lack of awareness, cost of medications and ineffective post-prophylactic surveillance are some of the major reasons for the high prevalence of rabies in tropical regions, leading to more than 40,000 cases annually presenting a major threat to public health. The present report aims to provide an overview of the lethal effects of rabies in major regions of the tropics, such as China and its neighboring countries, India, Bangkok, Thailand, all major regions of Africa, such as Tanzania and Ethiopia, and tropical regions of South America. The review is based on rich literature sources including epidemiological and endemic surveys, sample analysis, and health and hygiene reports from various parts of the world. The epidemiology is elucidated in the present article. The review also highlights the incidence of cases and aspects of prophylaxis. A bird's-eye view of rabies and its epidemic impact will encourage researchers to act further on the disease, which will lead to better awareness and treatment options.
Introduction
Rabies, from the Latin word for madness, is a viral disease that causes deadly maladies such as encephalitis in animals (Drew Citation2009). The disease is generally transmitted to humans from other species (such as dogs), commonly by a bite from an infected animal. Rabies is fatal to humans if prophylaxis is not administered before the onset of severe symptoms. The rabies virus infects the central nervous system (CNS), causing disruptions in the brain and finally leading to death (Drew Citation2009).
The major symptoms of rabies are headache, fever, severe acute pain, excitement, hydrophobia, lethargy in the later stages, coma and finally death, which is generally due to respiratory failure (Cotran et al. Citation2005). Approximately 60,000 deaths are recorded annually worldwide (WHO Citation2011). Ninety-five percent of human deaths due to rabies occur in Asia and Africa alone (CitationWHO: http://www.who.int/rabies/en). Dogs are responsible for 97% of human rabies cases (Voice of America Citation2009). Rabies elimination has been carried out in several countries, including Australia, Japan and Singapore.
Deadly transmission
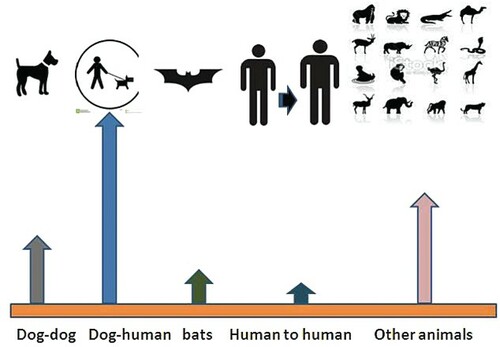
Apart from the dog (Canis lupus) (), the rabies virus also acclimatizes in cold-blooded animals (Campbell & Charlton Citation1988). Rabies can be transmitted not only by dogs, but also by other animals such as weasels, bears, raccoons, skunks and other wild carnivores. Small rodents, such as squirrels, hamsters, guinea pigs, gerbils, chipmunks, rats and mice, and lagomorphs, such as rabbits and hares, are also transmitters of the virus. Many tourists catch rabies (Taylor Citation1993; McRuer & Jones Citation2009); every year, people visiting Thailand and other oriental countries are affected by the virus.
The rabies virus turns deadly when it enters the human body. When the virus reaches the brain, it rapidly causes encephalitis, the prodromal phase, with the onset of symptoms. Once the symptoms appear in the patient, treatment is almost impossible. The probability of mortality at this stage is over 99%. Rabies may also inflame the spinal cord, producing transverse myelitis (Larry et al. Citation2005).
This lethal transmission has been a public health concern for centuries. Many governing bodies, such as the Centers for Disease Control (CDC), have been working to improve public health.
What the virus does
The virus enters the salivary glands of dogs before their death from rabies. Other possible routes of transmission include contamination of mucous membranes, aerosol transmission and corneal transplantation. The incubation period may range from 10 days to many years. However, it depends mostly on the distance of the wound from the CNS. The virus moves in the nerves to reach the brain and other multiple locations. The final location is the efferent nerves, from which it can move to the salivary glands. Rabies virus infection forms cytoplasmic inclusion bodies similar to Negri bodies, which are considered to be the sites of viral transmission and replication (Larry et al. Citation2005).
Figure 1. A rabies-infected dog. Source: http://en.wikipedia.org/wiki/Rabies#/media/File:Dog_with_rabies.jpg. Content Providers: CDC/Barbara Andrews [public domain].
![Figure 1. A rabies-infected dog. Source: http://en.wikipedia.org/wiki/Rabies#/media/File:Dog_with_rabies.jpg. Content Providers: CDC/Barbara Andrews [public domain].](/cms/asset/4ad4c498-46f6-4d6a-b24b-5df4b9767c37/tfls_a_1041186_f0001_b.gif)
Epidemiological devastation and concerns
Almost all recorded deaths due to the rabies virus occur in developing countries, and 80% of fatalities occur in Asia (Knobel et al. Citation2005; Zhenyang et al. Citation2013). India has the highest number of rabies cases in humans, followed by China, which has seen more than 117,500 deaths since 1950 (Tang et al. Citation2005). Owing to reasons like poor dog control, in Asia 85–90% of cases are due to transmission of the virus through dog bites (Tao et al. Citation2009; Nadin et al. Citation2011). Rabies virus collected from China shares genetic characteristics with its ancestors (Yamagata et al. Citation2007; Shao et al. Citation2011; Zhenyang et al. Citation2013). Zhenyang et al. (Citation2013) affirmed the phylogenetic variations and relationships between different strains collected in China and neighboring countries. Multiple sampling and broader isolation techniques were incorporated in this study to overcome problems of limited sampling (Zhenyang et al. Citation2013). Some clustered clades with isolates from countries in the Indochina peninsula and mainland Southeast Asia were observed, suggesting that this may be a convergent region for rabies virus panmixis owing to frequent animal trade between neighboring countries. Migration of people from villages to towns, and from towns to cities, with their domestic dogs could be another reason for the spread of the virus. Increased domestication of dogs and a remarkable increase in dog meat markets are contributing to the escalation of rabies prevalence (Zhenyang et al. Citation2013). Bats are also important potential transmitters of rabies (Jiang et al. Citation2010).
Tropical Asian countries are notable for the spread of the virus not only among residents, but also in tourists, who are most susceptible to the virus. A novel study on backpackers (Watcharapong et al. Citation2010) highlighted the percentage risk of transmission of rabies to the travelers. The study focused on the attitude and awareness of the travelers, and these factors were found to play a role in the spread of the disease (Watcharapong et al. Citation2010). Although international guidelines recommend pre-exposure to the rabies vaccine, only 18.1% of people in the study had been vaccinated. Nearly 70% of the people never obtained rabies immunization, and the major reason for the lack of immunization was the cost of the vaccine. Rabies vaccination is necessary if travelers are either moving to rabies-prone areas or staying for a period of more than 10 days. In the study by Watcharapong et al. (Citation2010), half of the exposures took place within the first 10 days. Such studies confirm the need for health education and awareness of this deadly disease (Krause et al. Citation1999). Pre-exposure would be a better strategy than seeking medical assistance after a bite, as many areas in tropical Asian countries lack medical and immunization facilities. In the Watcharapong et al. (Citation2010) study, only four of the backpacking travelers who were bitten by dogs managed to obtain medical aid. Studies have confirmed that only 64% of the public hospitals in Thailand have stocks of rabies immunoglobulin (Kositprapa et al. Citation1998). Other South Asian countries also have limited medical facilities and a lack of rabies immunization (Wilde et al. Citation2005; Ly et al. Citation2009). Therefore, travelers should have proper awareness of rabies and be pre-immunized for their own benefit.
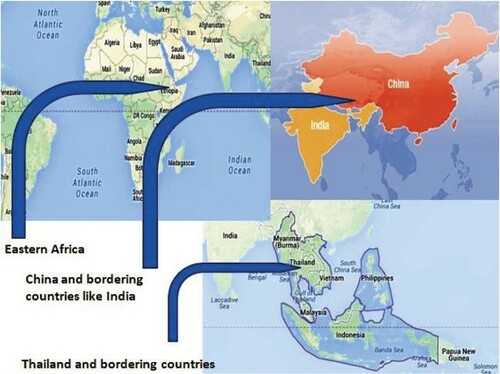
shows the geographical distribution of rabies. The figure highlights areas in eastern Africa, e.g. Ethiopia, China and neighboring countries, and other countries including Thailand, using data from previous epidemic and endemic studies.
After Asia, Africa is in second place in the spread of rabies in humans and domestic animals (Jemberu et al. Citation2013). In Africa, Ethiopia has one of the highest levels of endemic rabies. With regard to the incidence of deaths due to rabies, Ethiopia is one of the worst affected countries in the world, having 10,000 deaths annually (Fekadu Citation1997). Africa suffers huge losses of livestock due to rabies (Knobel et al. Citation2005). Jemberu et al. (Citation2013) conducted a thorough study which included a survey of the area, a questionnaire on practices and people's knowledge and awareness, and the incidence of rabies, both epidemically and endemically. Although the total number of cases was highest in dogs, humans were supposed to be at higher risk than other animals (). According to the rabies exposure charts in various districts, humans were exposed to the greatest extent. After Ethiopia, Kenya and Tanzania have the next highest incidence of rabies (Kitalaa et al. Citation2000; Cleaveland et al. Citation2002). Among all the cases recorded, and with regard to their severity, most of the cases were from rural areas as the people and livestock had a high risk of exposure. Dogs were found to be the major reservoir and source of infection.
In Africa, Ethiopia had some of the rarest encounters, which most people would never have thought possible, including human-to-human rabies transmission (Fekadu et al. Citation1996). A case of rabies was recorded in two individuals of the same family and the disease was likely to have been spread by human-to-human transmission. However, the high incidence of rabies in areas like the Serengeti district (Tanzania, Africa) was due to domestic dogs (Hampson et al. Citation2008), whereas in areas like the Ngorongoro district of Tanzania the high prevalence of rabies was more likely to be due to the high proportion of wildlife (Cleaveland & Dye Citation1995).
Laboratory confirmation, prophylaxis and treatment
Definitive diagnostic assays include quantitative reverse transcriptase–polymerase chain reaction, nucleic acid sequence-based amplification, direct rapid immunohisto- chemical tests and isolation of the virus from the cerebrospinal fluid or saliva. Antibodies can be detected in the serum and cerebrospinal fluid. Pathological specimens often demonstrate round or oval eosinophilic inclusion bodies in the cytoplasm of neuronal cells (Angela et al. Citation2011).
Prevention by pre-exposure immunization
This process includes treating people with three intramuscular injections of human diploid cell vaccine (1 ml on days 0 and 7, and 21 or 28), especially those who are at a high risk of exposure. Backpackers who explore countries in Africa, Asia, and other high-risk areas should receive an intradermal dose, over the deltoid, on days 0, 7 and 21 (Maxine et al. Citation2013).
Post-exposure immunization
The patient is generally treated on the basis of the extent of the bite, intensity, location of the wound, animal, history of previous immunization and epidemiology. Immediate consultation with local health departments is highly recommended. The optimal form of passive immunization is a human rabies immunoglobulin (HRIG; 20 IU/kg), administered once. The full dose is administered around the wound (Maxine et al. Citation2013). Equine rabies antiserum (40 IU/kg) is used as an alternative. As much as possible of the rabies immunoglobulin is injected at the site of the wound and the remainder at a site distant from the vaccine administration.
At present, purified vaccines are grown on Vero cells, and a sixth generation Vero cell vaccine is under development. This method produces more allergy-resistant vaccines compared to the previous chicken embryo cell-grown vaccines. HRIG is unnecessary in previously vaccinated patients. The post-exposure vaccine includes 1 ml in the deltoid, administered twice (on days 0 and 3). Post-exposure prophylaxis (PEP) is considered safe and does not even cause fetal complications (CDC Citation2011; Maxine et al. Citation2013).
Need for elimination and ways of prevention
As the rabies virus is spread mainly by domestic dogs, elimination of the virus is the best option (Lembo et al. Citation2010). The virus can be eliminated by mass vaccination (Coleman & Dye Citation1996).
illustrates the spread and reported cases of rabies in China. It is evident that the numbers of cases have been significantly and consistently increasing, thus provoking the need for the elimination of the virus to stop the spread of this disease.
Figure 4. Reported cases of rabies in China during 2007–2012 (extracted from Wenwu et al. Citation2013).
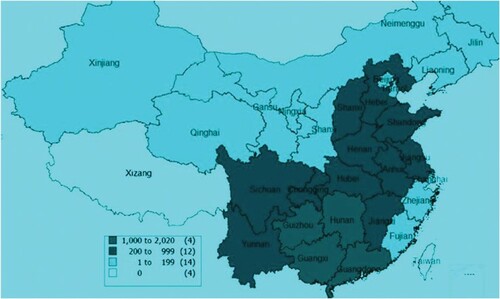
Shanghai was one region of China in which the post-exposure vaccination coverage was about 99% (Wenwu et al. Citation2013). However, lack of awareness of the vaccine and lack of medical facilities in areas like Guizhou and Guangdong is evident, as nearly 1000–2020 cases of rabies were recorded. A Chinese survey on injuries in children, conducted among 319,543 people (including 98,335 children aged < 18 years) in Jiangxi province in 2007, estimated that 89 children may have died of animal (mainly dog) bites, whereas China CDC reported 21 rabies cases (i.e. four-fold underreporting) in the same year and the same age group (Wenwu et al. Citation2013).
Previous elimination principles included controlling rabies in dogs, providing access to adequate PEP in humans to ensure effective disease control, and animal reservoir surveillance throughout the course of the campaign (Wenwu et al. Citation2013).
The need for elimination in South American countries was also high. A high proportion of people who were affected in South American cities were low-income individuals (Vigilato et al. Citation2013). As a result, a number of canine vaccination programs have been arranged in South American cities. Nearly 81% of animals were vaccinated from 2001 to 2003. Latin American and tropical countries such as Brazil, Venezuela and Argentina have participated in these programs. More than 2,500,000 doses of human vaccine have been used annually in pre- and post-prophylaxis (PAHO 2011; Vigilato et al. Citation2013). Key procedures, such as technical cooperation, quality assurance of biological products, providing a motivated staff, control of the canine population, establishing early prophylaxis protocols and calculating the doses of biological supplies, have been implemented (PAHO 2011). It has been crucial to understand the rabies life cycle and design an appropriate treatment path.
Other rabies elimination programs have been implemented in India, such as the street dog sterilization program. Information on street dog breeding was analyzed by experts in the Jaipur region in India. Animal bites and their correlation with the season were also estimated. Under this program, dog bites have decreased significantly since 2003 and the roaming dog population has been reduced (Reece et al. Citation2013).
Many tropical countries need to implement 100% pre-prophylaxis and other similar procedures to reduce the numbers of rabies cases. Successful strategies have to be put in place, including issuing biological supplies to rural areas, running awareness camps and conducting mass vaccination programs.
Conclusion
Today, many countries are facing rabies as an endemic and epidemic challenge. Establishing intensive surveillance, awareness protocols and communication with local communities can only aid in eradicating the disease.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Angela A, et al. 2011. Failure of the Milwaukee protocol in a child with rabies. Clin Inf Dis. 53:572–574. doi: https://doi.org/10.1093/cid/cir483
- Campbell JB, Charlton KM. 1988. Developments in veterinary virology: rabies. Springer: Kluwer Academic Publishers. p. 48.
- Centers for Disease Control and Prevention (CDC). Human rabies – Wisconsin. 2010. MMWR Morb Mortal Weekly report. 2011 September 2; 60(34):1164–1166.
- Cleaveland S, Dye C. 1995. Maintenance of a microparasite infecting several host species: rabies in the Serengeti. Parasitology. 111:S33–S47. doi: https://doi.org/10.1017/S0031182000075806
- Cleaveland S, Fevre EM, Kaar M, Coleman PG. 2002. Estimating human rabies mortality in the United Republic of Tanzania from dog bites injuries. Bull World Health Organ. 80:304–310.
- Coleman P, Dye C. 1996. Immunization coverage required to prevent outbreaks of dog rabies. Vaccine. 14:185–186. doi: https://doi.org/10.1016/0264-410X(95)00197-9
- Cotran RS, Kumar V, Fausto N. 2005. Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis: Elsevier/Saunders. p. 1375.
- Drew WL. 2009. Chapter 41: Rabies. In Ryan KJ, Ray CG, editors. Sherris medical microbiology (4th ed.). McGraw Hill, New York, USA. p. 597–600.
- Fekadu M, et al. 1996. Possible human-to-human transmission of rabies in Ethiopia. Ethiop Med J. 34:123–7.
- Fekadu, M. 1997. Human rabies surveillance and control in Ethiopia. In: proceeding of the southern and eastern African rabies group meeting 1997 March 4–6; Nairobi, Kenya. 2.
- Hampson, K. et al. 2008. Rabies exposures, post-exposure prophylaxis and deaths in a region of endemic canine rabies. PLoS Negl Trop Dis. 2:e339. doi: https://doi.org/10.1371/journal.pntd.0000339
- Jemberu WT, Molla W, Almaw G, Alemu S. 2013. Incidence of rabies in humans and domestic animals and people's awareness in North Gondar Zone, Ethiopia. PLoS Negl Trop Dis. 7:e2216. doi:https://doi.org/10.1371/journal.pntd.0002216.
- Jiang Y, et al. 2010. Seroprevalence of rabiesvirus antibodies in bats from southern China. Vector Borne Zoonotic Dis. 10:177–181. doi: https://doi.org/10.1089/vbz.2008.0212
- Kitalaa PM, McDermotta JJ, Kyulea MN, Gathuma JM. 2000. Community based active surveillance for rabies in Machakos District, Kenya. Prev Vet Med. 44:73–85. doi: https://doi.org/10.1016/S0167-5877(99)00114-2
- Knobel DL, et al. 2005. Re-evaluating the burden of rabies in Africa and Asia. Bull World Health Organ. 83:360–368.
- Kositprapa C, et al. 1998. Problems with rabies post exposure management: a survey of 499 public hospitals in Thailand. J Travel Med. 5:30–32. doi: https://doi.org/10.1111/j.1708-8305.1998.tb00453.x
- Krause E, Grundmann H, Hatz C. 1999. Pretravel advice neglects rabies risk for travelers to tropical countries. J Travel Med. 6:163–167. doi: https://doi.org/10.1111/j.1708-8305.1999.tb00854.x
- Larry ED, Molly MKK, Jessica LS. 2005. Fundamentals of neurologic disease. Demos Medical Publishing, New York, USA. p. 73.
- Lembo T, Hampson K, Kaare MT, Ernest E, Knobel D. 2010. The feasibility of canine rabies elimination in Africa: dispelling doubts with data. PLoS Negl Trop Dis. 4:e626. doi: https://doi.org/10.1371/journal.pntd.0000626
- Ly S, et al. 2009. Rabies situation in Cambodia. PLoS Negl Trop Dis. 3:e511. doi: https://doi.org/10.1371/journal.pntd.0000511
- Maxine P, Stephen JM, Micheal WR. 2013. Current medical diagnosis and treatment. McGraw Hill. p. 1377.
- McRuer DL, Jones KD. 2009. Behavioral and nutritional aspects of the Virginian opossum (Didelphis virginiana). The veterinary clinics of North America. Exotic Animal Practice. 12:217–236. doi: https://doi.org/10.1016/j.cvex.2009.01.007
- Nadin-Davis SA, Sheen M, Wandeler AI. 2011. Recent emergence of the Arctic rabies virus lineage. Virus Res. 163:352–362. doi: https://doi.org/10.1016/j.virusres.2011.10.026
- Reece JC, Chawla CK, Hiby AR. 2013. Decline in human dog-bite cases during a street dog sterilisation programme in Jaipur, India. Vet Rec. 172:473. doi:https://doi.org/10.1136/vr.101079.
- Shao XQ, et al. 2011. Genetic evidence for domestic raccoon dog rabies caused by Arctic-like rabies virus in Inner Mongolia, China. Epidemiol Infect. 139:629–635. doi: https://doi.org/10.1017/S0950268810001263
- Tang X, et al. 2005. Pivotal role of dogs in rabies transmission, China. Emerg Infect Dis. 11:1970–1972. doi: https://doi.org/10.3201/eid1112.050271
- Tao XY, et al. 2009. Molecular epidemiology of rabies in Southern People's Republic of China. Emerg Infect Dis. 15:1192–1198. doi: https://doi.org/10.3201/eid1508.081551
- Taylor PJ. 1993. A systematic and population genetic approach to the rabies problem in the yellow mongoose (Cynictispenicillata). Onderstepoort J Vet Res. 60(4):379–87.
- Vigilato MAN, et al. 2013. Progress towards eliminating canine rabies: policies and perspectives from Latin America and the Caribbean. Phil Trans R Soc B. 368:20120143. doi:https://doi.org/10.1098/rstb.2012.0143
- Voice of America. New rabies vaccine shows promise for prevention, treatment. 2009-07-08. Retrieved 2010-01-30.
- Watcharapong P, Prapimporn S, Weerapong P. 2010. Rabies exposure risk among foreign backpackers in Southeast Asia. Am J Trop Med Hyg. 82:1168–1171. doi: https://doi.org/10.4269/ajtmh.2010.09-0699
- Wenwu Y, et al. 2013. Challenges and needs for China to eliminate rabies. Infec Dis pov. 0:2–23.
- Wilde H, et al. 2005. Rabies control in South and Southeast Asia. Vaccine. 23:2284–2289. doi: https://doi.org/10.1016/j.vaccine.2005.01.030
- World Health Organization (WHO). September 2011. Retrieved 31 December 2011.
- World Health Organization (WHO). http://www.who.int/rabies/en.
- Yamagata J, et al. 2007. Molecular epidemiology of rabies in Vietnam. Microbiol Immunol. 51:833–840. doi: https://doi.org/10.1111/j.1348-0421.2007.tb03979.x
- Zhenyang G, Xiaoyan T, Cuiping Y. 2013. National borders effectively halt the spread of rabies: the current rabies epidemic in China is dislocated from cases in neighboring countries. PLoS Negl Trop Dis. 7:e2039. doi: https://doi.org/10.1371/journal.pntd.0002039