ABSTRACT
Since 2011, the annual improving outcomes in the treatment of opioid dependence (IOTOD) meeting has brought together a broad range of primarily European healthcare professionals as part of an ongoing effort to promote best practice for this particularly vulnerable patient population. IOTOD, a comprehensive educational initiative, includes the annual Continuing Medical Education (CME)-accredited IOTOD conference, which is dedicated to measuring practice change and outcomes resulting from attendance at its educational sessions. Following each session, delegates are asked to vote for or against incorporating specified changes into their clinical practice. These “commitments to change” have formed one measure of the effectiveness and impact of the IOTOD conference. Here, we look at why educational initiatives like the IOTOD conference are valuable, examine our methods for conducting a CME-accredited event, and highlight individualised treatment plans and delivery. We examine this approach – increasingly seen as best practice – as an example of how it may be changing attitudes and eventually affecting clinical applications in the field of opioid dependence. The measured commitments to change offer insight into HCPs’ attitudes towards opioid dependence management and show that attitudes towards individualised treatment plans seem to be progressively positive, with a general consensus to incorporate psychosocial interventions.
Introduction
Introducing opioid dependence and appropriate interventions
Opioid dependence is a chronic disorder characterised by craving, physiological withdrawal, increased tolerance and persistence of use despite harm caused [Citation1]. It is associated with considerable morbidity, including psychiatric disorders, homelessness and, in people who inject opioids, hepatitis C virus (HCV) and human immunodeficiency virus (HIV). Opioid use also increases the risk of opioid overdoses, a common cause of death among the opioid-dependent population [Citation1,Citation2].
At present, opioid overdoses are a major health concern worldwide, with 15 million individuals believed to be at risk and an estimated 69,000 dying as a result each year [Citation3]. In Europe, there are 1.3 million people at risk and opioids were associated with the majority of the 8,441 overdose fatalities registered in 2015, which have been on the rise since 2012 [Citation4].
There is a strong evidence base for treating opioid dependence with opioid agonist treatment (OAT), usually either methadone or buprenorphine, together with psychosocial interventions (PSIs). OAT has been shown to reduce morbidity, mortality and offending among those receiving it, and now plays a significant role in treatment demands and health harms in a number of European countries [Citation4]. Overdose deaths are reduced among people who use opioids while they are in OAT [Citation5,Citation6]. For example, one meta-analysis showed that the mortality rate of people in methadone treatment was less than a third of the expected rate in opioid users out of treatment [Citation4].
Tailoring treatment plans to the needs of individual patients, their preferences and goals is strongly supported by guidelines for dependence, with the UK clinical guidelines on drug misuse and dependence advising healthcare professionals (HCPs) against rigidly using the same approach and care plan for every patient. In addition to treatment plans, treatment delivery should also be individualised; monitoring patients’ symptoms and listening to feedback is key to this, and in cases where patients do not respond well to treatment, HCPs may adjust the dose of OAT or switch to another OAT. PSIs, a crucial component of treatment, should also be individualised, taking into account a patient’s preferences and achievable goals. In addition, HCPs may wish to change the frequency of patient visits and of monitoring [Citation7,Citation8]. Therefore, tailoring care for opioid-dependent patients is recommended at all stages and across all components of treatment.
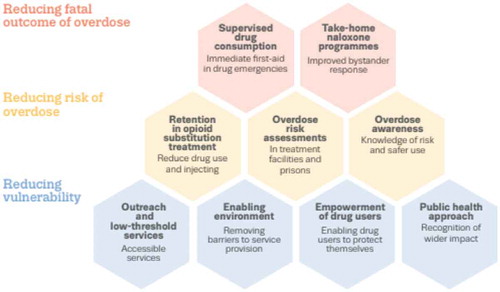
It is important to note the existence of other interventions, in addition to treatment, which aim to reduce opioid-related harm and overdoses (). Examples of these include the distribution of naloxone, an opioid overdose reversal drug, to individuals who are likely to experience and/or witness an overdose, through take-home naloxone programmes; in addition, needle and syringe exchange programmes and supervised drug consumption rooms promote safer injecting practices and a safe injecting environment, respectively [Citation9]. Despite the accumulation of evidence that these interventions reduce opioid-related harms and mortality, their implementation has been considerably limited worldwide.
Principles underlying continuing medical education best practice
PCM Scientific is the medical education and continuing medical education (CME) company acting as the secretariat for IOTOD, with a long track record in running European CME initiatives that deliver measurable outcomes.
PCM Scientific is a founding member of the Good CME Practice group (gCMEp) that works to establish and raise standards in the provision of CME in Europe. The gCMEp has defined and validated the standards of good CME practice along with four core principles, using a consensus research process across Europe relating to:
Appropriate education
Effective education
Fair balance
Transparency [Citation10]
As a CME provider, PCM Scientific aims to contribute to improving public health outcomes by championing best practice in CME, maintaining and improving standards and collaborating with stakeholders. This is done out of a belief that CME is a positive and influential force for change in clinical practice.
A number of recent studies in the area of opioid management have shown the effect that CME can have. McCalmont and colleagues were able to show that higher hours of recent CME positively benefited provider confidence in pain management and use of Centers for Disease Control and Prevention (CDC)-recommended practices [Citation11]. Another found that by educating surgeons at an institution in the US [Citation12], they were able to decrease the number of opioids initially prescribed post-operatively by just over half. Information was presented about variability and overprescription of opioids and recommendations were made on the number of opioid pills that should be prescribed for specific operation types. As well as demonstrating the potential of CME in general, this also shows that early educational interventions could have important implications in future opioid use.
About IOTOD
Improving Outcomes in the Treatment of Opioid Dependence (IOTOD) is an educational initiative, organised and developed by PCM Scientific since 2011, that aims to improve patient care in the field of opioid dependence. This is primarily achieved through the CME-accredited annual IOTOD conference, which explores the most pressing challenges faced by the opioid-dependent population and emphasises the importance of individualising care. In addition to the stand-alone conference, IOTOD now includes online education, such as webcasts, reports and the take-home naloxone (THN) toolkit.
The IOTOD conference has become a key event in the opioid dependence therapy sphere owing to its impactful learning experiences and range of clinically relevant, advanced, cutting-edge topics discussed at the annual event. The delegates, mostly HCPs, have also benefited from the conference’s interactive technology since 2011. This interactive element has increased discussions with the speakers and allowed PCM Scientific to document the changes that delegates have committed to implementing in their clinical practice, also known as the IOTOD “commitments to change.”
Here, we reflect on IOTOD delegates’ commitments to change since 2011 and consider these as markers of the potential effectiveness of PCM Scientific’s educational methods. Although the IOTOD conference discusses a range of topics, here we have focused on attitudes towards individualised treatments and integrated PSIs as these have been consistent themes since commitments to change were first recorded in 2011.
Methods
As the secretariat, PCM Scientific undertakes the organisational work for the conference, incorporating needs assessments, speaker recruitment, topic selection, logistical support, delegate practice change assessment, report creation and website hosting/curation.
To reflect the ever-changing field of opioid dependence, the IOTOD conference programme evolves year-on-year. The programme content is put together following a comprehensive needs assessment comprising:
The previous year’s delegates’ expressions of interest and needs
The chairs’ opinions on the most pressing issues
Practice gaps identified by the chairs and literature searches
Relevant upcoming legislation changes and product availabilities
Recently published research that has the potential to change practice
New clinical guidelines
The sessions are delivered in an engaging format in order to drive change in participant behaviours:
Plenary education sessions
Complex case studies
Expert panel discussions
Interactive audience response system (ARS) technology throughout
Commitment-to-change manifesto driven by delegates’ submissions of what they wish to change in their day-to-day practice as a result of what they learned during the sessions
Furthermore, enduring materials from the conferences, such as highlights reports and webcasts, are hosted on the IOTOD website (http://www.iotodeducation.com/) and distributed to relevant databases for an increased reach.
A learning objective is always set ahead of time for each speaker’s presentation and they are usually aligned with the commitments to change. Learning objectives for IOTOD have been routinely created by leading with a measurable verb, such as those described in Bloom’s taxonomy of measurable outcomes [Citation13]. Examples of learning objectives used at IOTOD to date are shown below.
“Following this presentation, participants should be able to:
Formulate recovery-orientated treatment plans for all patients, from the outset of care
Identify the importance of combining or sequencing psychological interventions with pharmacological interventions as best practice
Recognise the importance of post-withdrawal care and link their patients to appropriate services”
Delegate assessment data are collected during and after the conference. Data are collected on-site through the use of slide show questions after each session, with delegates answering via voting handsets.
Evaluation comprises:
On-site – during each of the presentations in the session: a brief assessment of the baseline level of learner knowledge and self-reported current practice (via the ARS)
On-site – at the end of the conference: attendees pledge their commitment to change their clinical practice as a result of attending each session (via the ARS), agreeing to specific change targets that are compiled and circulated as the commitment-to-change manifesto
Post-meeting evaluation timepoints have varied historically, but are usually completed at 6 months and 1 year after the conference – attendees are asked to participate in an online survey based on their commitment to change, which assesses any changes in physician performance that have occurred as a result of the session
Unlike the online survey, data for the percentage of delegates responding to the interactive questions or commitments to change using the ARS on-site are not available.
Cut-offs for commitments to change were assigned as follows:
Commitment accepted, ≥70% agreement
Commitment rejected, ≤69% agreement
For the purpose of this publication, data were taken from archived material from 2011 to 2017 focusing on any commitment to change that involved an integrated approach to the treatment of opioid dependence (sometimes historically referred to as medication-assisted treatment [MAT]). IOTOD did not take place in 2014 and data from 2018 have not yet been processed.
Results
Participant information
Most attendees identified themselves as a general practitioner (GP)/family physician, psychiatrist or, in later years, as an addictions specialist doctor ().
Table 1. Summary of attendee profession 2011–2017.
Attendee geography: most delegates were from the UK (33%), France (15%) and Germany (12%), with small percentages from Ireland, Italy, Croatia, Belgium, Turkey and the USA, and 7% from the rest of the world.
Commitments to change: general attitudes towards individualised treatment
Individualised treatment has been a major theme throughout the 7 years of IOTOD’s commitments to change. In 2013, 90% of the IOTOD delegates agreed that treatments should be individualised by adapting interventions to treatment response, and 91% agreed that medication should be individualised and guided by assessment and review.
This call to action increased in 2015 and 2016, when 98% and 97% of the delegates, respectively, committed to individualising treatment planning and delivery for both medication and non-medication therapies ().
Table 2. Level of participant agreement for individualising treatment.
Furthermore, a one-year follow-up survey with attendees from IOTOD 2016 showed 100% of respondents reported that they now use an individualised treatment approach in their daily practice.
Commitments to change: review and optimisation of treatment
Delegates attending the IOTOD conference have consistently supported optimising medication during different phases of treatment. In 2011, 96% of attendees committed to monitoring and assessing therapeutic dosing of maintenance medication based on patients’ clinical response. The same sentiment was echoed in 2017, with 99% committing to adjusting doses according to individual patients’ signs, symptoms and personal feedback ().
Table 3. Level of participant agreement for reviewing and optimising treatment.
In a 3-month follow-up survey, which was circulated to all attendees of IOTOD 2017, 25% of respondents had implemented this, 69% said that they were already doing it and the remaining 6% said that they intended to implement it in the future. Of note, none of the respondents said they were unable to implement this change or did not intend to.
In 2011, 100% of IOTOD attendees responding on-site committed to review each of their patients’ treatment. In 2013, 88% of attendees agreed that clinicians should be trained to transition between appropriate treatments and in 2016, 92% of participants committed to make a larger selection of treatments available to patients ().
Commitments to change: provision of PSIs
Incorporating PSIs into patients’ treatment plans has consistently been supported by IOTOD delegates, with 97% agreeing that PSIs should be used alongside opioid pharmacotherapy in 2011 and in 2017, 97% committed to incorporating PSIs in the treatment plans of all opioid-dependent patients ().
Table 4. Level of participant agreement for providing psychosocial care.
In 2017, 98% of delegates committed to encourage all their opioid-dependent patients actively to participate in psychosocial therapies. From a 3-month follow-up survey, 76% said they currently incorporate psychosocial therapies in the treatment plans of their opioid-dependent patients, and 69% said they now encourage all their opioid-dependent patients actively to participate in psychosocial therapies. Those who had not implemented the commitments at the time of the survey, all answered that they intended to implement them in the future.
While agreement to incorporate PSIs has remained relatively consistent, there was variation over which type of behavioural intervention to incorporate. In terms of cognitive behavioural therapy (CBT), 84% of delegates agreed to introduce or scale up CBT in their routine clinical practice in 2015, and in 2016, 83% agreed to explore CBT with suitable patients; this increased to 97% in 2017.
In a three-month follow-up survey following the IOTOD 2016 conference, 33% confirmed they were currently exploring CBT with suitable patients, 33% said that they were not doing this and 33% said that they were unable to; in the 1-year follow-up survey, 39% of respondents said that they had increased the use of CBT with relevant patients.
Commitments to change: post-meeting response rates
A representation of the response rate seen with the post-meeting follow-up surveys:
IOTOD 2016 at three months: 27%
IOTOD 2016 at one year: 14%
IOTOD 2017 at three months: 12%
IOTOD 2017 at one year: 12%
Discussion
Commitments to change: general attitudes towards individualised treatment
The results show a high proportion of delegates agree with individualising treatment plans (≥90%) and support for this has increased (90–98%) over the seven-year period. These consistent commitments to change results indicate a trend in favour of personalising treatment at all stages of a patient’s journey, highlighting the critical importance of this ongoing process to improve patient outcomes and mirroring the wider trend towards this approach in clinical practice guidelines, such as the UK clinical guidelines for drug misuse and dependence [Citation7]. Furthermore, positive results from the IOTOD 2016 1-year follow-up survey suggests the commitment to individualising treatment plans was durable.
Commitments to change: review and optimisation of treatment
The commitments to change regarding reviewing and optimising treatment were consistently positive and illustrate an overall readiness of HCPs to commit regularly to reviewing and optimising the therapeutic dosing of medication based on clinical parameters and patient-reported symptoms. The data also suggest that HCPs generally wish to be competent at successfully transitioning between treatments.
Commitments to change: provision of PSIs
Implementing PSIs together with pharmacotherapy is a common evidence-based and guideline-recommended strategy for managing opioid dependence [Citation7,Citation14]. The IOTOD data highlight strong support for the integrated use of PSIs (97–98% agreement). According to the 2016 and 2017 follow-up surveys, more than one third of respondents said that they were either currently implementing at least one form of PSI or intending to do so.
Educational outcomes and potential for improvement
PCM Scientific believes that the format and content of the IOTOD conference have driven substantial and sustainable performance improvements. However, a commitment to the principles of CME means continually aiming to improve assessment methods, communication, reach and relevance. IOTOD already offers scholarships, providing free registrations, in part to improve accessibility to HCPs that may not otherwise be able to attend.
IOTOD educational materials and conferences currently satisfy levels 1 (participation), 2 (participant satisfaction), 3A (learning declarative knowledge) and 3B (learning procedural knowledge) of Moore’s expanded outcomes framework for assessing learners and evaluating instructional activities, as well as subjective measurements (self-reported) for level 4 (competence) and 5 (performance). However, they do not gather objective measurements (observing competence or performance) for levels 4 and 5 or measure changes in level 6 (patient health outcomes) and 7 (community health) [Citation15], the possibility of obtaining information pertaining to these is a potential avenue for improvement.
It is becoming more accepted that passive educational information dissemination is largely ineffective, rather, a multifaceted behaviour change strategy is more powerful. Additionally, audit and feedback processes can potentially have a reinforcing effect, as well as providing valuable information on delegates’ opinions [Citation16]. Future approaches for building on the methods of learning offered include the use of simulation-based medical education (SBME). SBME has been shown to enhance retention of training information compared with lectures [Citation17], and could be incorporated into the event.
Although the post-meeting assessment response rates reported here may seem low, typical response rates for online surveys reported elsewhere are similar. A recent study attempting to evaluate the impact of a low-cost non-monetary incentive and paper mail reminders on response rates for internet-based physician surveys found that of 3,966 physicians surveyed, their response rates ranged from 9% to 11.6%[Citation18]. Perhaps novel methods of post-conference response collection could improve on this in the future.
Finally, the role of the IOTOD educational platform is currently limited to practising HCPs; however, an exploration of how to influence the incorporation of opioid dependence education into undergraduate teaching could potentially have a wider impact on:
Identifying patients at risk
Recognising signs and symptoms of opioid dependency
Following proper opioid prescription guidelines
Identifying systems-based practice for referral of patients who are dependent on opioids
This would more effectively prepare future HCPs to respond to more situations, manage care and prevent overdoses [Citation17].
Limitations
This study has a number of limitations regarding the robustness of the data. Despite the same themes being explored year to year, these were not accompanied by identical commitments to change, therefore conclusive trends in attitudes and practice cannot be drawn. Other limitations include the changing samples, as the attending delegate list varies each year. Furthermore, the sample sizes for on-site commitments to change assessment are small and the on-site response rates of attendees are unavailable, so the results do not represent the whole opioid dependence healthcare community. Although the follow-up assessment rates are comparable with other online questionnaire response rates for HCPs, the fact that only a small proportion of delegates complete the follow-up assessments means that this sample may not be representative of the conference attendees as a whole, which might also lead to sampling and convenience bias, distorting the result outcomes. Finally, all assessments are self-reported and, as such, do not capture real-world behavioural changes. Our results can only be viewed as circumstantial observations and should be interpreted with caution.
Conclusion
The data indicate that HCPs attending the IOTOD conference are supportive of individualised treatment planning and delivery, and follow-up surveys suggest that attendees are motivated to adhere to their commitments in the medium to long term. Notably, delegates were in agreement to review and monitor therapeutic medication doses and treatment types and incorporate PSIs into treatment plans.
As IOTOD approaches its ninth year as a CME-accredited conference, we appreciate the important role that it has in the continuing education of HCPs involved in opioid dependence across Europe, and in providing comprehensive insight and commentary into the latest advances in the field. Throughout its history, the IOTOD conference has evolved beyond conventional CME conferences in this area and by harnessing multi-format educational interventions and behaviour change techniques, IOTOD is potentially influencing physician behaviours in an enduring way.
The multidimensional IOTOD educational format not only enhances delegates’ knowledge but inspires them to reflect on their practice and commit to making changes when they return to their daily practices. The convention of following up with delegates using online surveys not only allows us to gain insight into the effectiveness of the education in driving sustainable changes to clinical practice, but also potentially reinforces the intention to commit to the changes.
Declarations of interest
Sarah Webster is a medical writer employed by PCM Scientific, the medical education company acting as secretariat for the IOTOD annual meeting.
Sarah Robinson is a medical writer employed by PCM Scientific, the medical education company acting as secretariat for the IOTOD annual meeting.
Robert Ali has received untied educational grants from Reckitt Benckiser for the post-marketing surveillance of opioid substitution therapy medications in Australia and for conducting a study into the pharmacogenetic predictors of treatment success.
John Marsden declares investigator-led, educational grant funding from Indivior (administered by Action-on-Addiction) for a study of personalised psychosocial intervention for non-response to opioid agonist treatment (ARC Trial), and support from NIHR (HTA) for a trial of extended-release naltrexone. He acknowledges part-time employment as Senior Academic Advisor for the Alcohol, Drugs and Tobacco Division, Health Improvement, Public Health England and consultancy for the US National Institute on Drug Abuse, Centre for Clinical Trials Network. In the past three years, he received honoraria from Merck Serono (2015; clinical oncology training); Martindale (2017; expert meeting on OUD); and Indivior (via PCM Scientific) as co-chair (2015, 2016) and chair (2017) for the conference on Improving Outcomes in Treatment of Opioid Dependence. He holds no stocks in any company.
Additional information
Funding
References
- National Institute for Health and Care Excellence. Clinical knowledge summary. Available at: Opioid dependence. Available at: https://cks.nice.org.uk/opioid-dependence last accessed 2018 Jun.
- Roncero C, Barral C, Rodríguez-Cintas L, et al. Psychiatric comorbidities in opioid-dependent patients undergoing a replacement therapy programme in Spain: the PROTEUS study. Psychiatry Res. 2016;243:1–8.
- World Health Organization (WHO). Information sheet on opioid overdose. Available at: http://www.who.int/substance_abuse/information-sheet/en/last accessed 2018 Jun.
- EMCDDA European Drug Report. Trends and Developments 2017. Available at: http://www.emcdda.europa.eu/system/files/publications/4541/TDAT17001ENN.pdf last accessed 2018 Jun.
- European Monitoring Centre for Drugs and Drug Addiction (2017). Health and social responses to drug problems: a European guide, publications office of the European Union, Luxembourg. Available at: http://www.emcdda.europa.eu/system/files/publications/6343/TI_PUBPDF_TD0117699ENN_PDFWEB_20171009153649.pdf last accessed 2018 Jun
- Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550.
- Drug misuse and dependence: UK guidelines on clinical management. 2017. Department of Health. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/628634/clinical_guidelines_2017.pdf last accessed 2018 Jun.
- Gowing L, Ali R, Dunlop A, et al. National Guidelines for Medication-Assisted Treatment of Opioid Dependence. Australian Government Department of Health; 2014.
- European Monitoring Centre for Drugs and Drug Addiction. Preventing overdose deaths in Europe. Available at: http://www.emcdda.europa.eu/topics/pods/preventing-overdose-deaths last accessed 2018 Jun.
- Farrow S, Gillgrass D, Pearlstone A, et al. Setting CME standards in Europe: guiding principles for medical education. Curr Med Res Opin. 2012;28(11):1861–1871.
- McCalmont JC, Jones KD, Bennett RM, et al. Does familiarity with CDC guidelines, continuing education, and provider characteristics influence adherence to chronic pain management practices and opioid prescribing? J Opioid Manag. 2018;14(2):103–116.
- Hill MV, Stucke RS, McMahon ML, et al. An educational intervention decreases opioid prescribing after general surgical operations. Ann Surg. 2018;267(3):468–472.
- Bloom BS, Engelhart MD, Furst EJ, et al. Taxonomy of educational objectives: the classification of educational goals. Handbook I: cognitive domain. New York: David McKay Company; 1956.
- World Health Organization (WHO). Guidelines for the psychosocially assisted pharmacological treatment of opioid dependence. Geneva, Switzerland: Management of Substance Abuse Team, Department of Mental Health and Substance Abuse, World Health Organization; 2009.
- Moore DE Jr, Green JS, Gallis HA. Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. 2009;29(1):1–15.
- Robertson R, Jochelson K Interventions that change clinician behaviour: mapping the literature. King’s Fund literature review. Available at: https://www.nice.org.uk/Media/Default/About/what-we-do/Into-practice/Support-for-service-improvement-and-audit/Kings-Fund-literature-review.pdf last accessed 2018 Jun.
- Ratycz MC, Papadimos TJ, Vanderbilt AA. Addressing the growing opioid and heroin abuse epidemic: a call for medical school curricula. Med Educ Online. 2018;23(1):1466574.
- Cook DA, Wittich CM, Daniels WL, et al. Incentive and reminder strategies to improve response rate for internet-based physician surveys: a randomized experiment. J Med Internet Res. 2016;18(9):e244.