Abstract
Growing evidence suggests that outbreaks such as the COVID-19 pandemic are better handled in places where social capital is high. Less clear, however, are the channels through which social capital makes communities better able to respond to outbreaks. In this article I develop a multidimensional and multilevel approach that compares the potential dissimilar effects of social capital in different forms and at different levels. As social capital in different forms and at different levels can affect social outcomes through distinctive means, such an approach can help detect the processes underlying how social capital works. I illustrate this new approach by analyzing data from a survey I conducted in late April 2020 in China’s Hubei province as well as data from the most recent World Values Survey (WVS, 2016–2020). Results suggest that social capital affects COVID-19 response mainly through facilitating collective actions and promoting public acceptance of and compliance with control measures in the form of trust and norms at the individual level. Social capital can also help mobilize resources in the form of networks at the community level. In an authoritarian context, compliance with control measures relies more on people’s trust in their political institutions, less on trust in each other.
Introduction
In facing the same COVID-19 pandemic, communities and societies have shown varying responses. Witnessing the variations in responses and thereby the coronavirus’ uneven impacts, U.K. Prime Minster Boris Johnson has totally refuted the notorious Margaret Thatcher quote that “there’s no such thing as society.” Openly, he said that “One thing I think the coronavirus crisis has already proved is that there really is such a thing as society” (see also McLachlan Citation2020).
Johnson’s remark is not without empirical support. In fact, social capital, which captures the features of social organizations and formal and informal norms within societies (Coleman Citation1990; Putnam Citation2000), has been shown to powerfully predict the diverse COVID-19 responses (e.g., Bai, Jin, and Wan Citation2020; Barrios et al. Citation2020; Bartscher et al. Citation2020; Borgonovi and Andrieu Citation2020; Ding et al. Citation2020; Fraser and Aldrich Citation2020; Kokubun Citation2020; Kuchler, Russel, and Stroebel Citation2020; Makridis and Wu Citation2020; Miao and Zeng Citation2020; Varshney and Socher Citation2020; Wu et al. Citation2020). In the United States, for example, scholars find that counties or states with more social capital tend to have higher testing rates (Wu et al. Citation2020), less social mobility (Borgonovi and Andrieu Citation2020), more engagement in social distancing (Ding et al. Citation2020) as well as fewer confirmed cases and slower infection growth rates (Markridis and Wu Citation2020). Similar patterns have also been observed in many other countries such as Austria, Germany, Japan, Italy, the Netherlands, Sweden, Switzerland, and the U.K. (Barrios et al. Citation2020; Bartscher et al. Citation2020; Fraser and Aldrich Citation2020).
Nonetheless, it remains unclear what the channels are through which social capital makes locations better able to respond to the pandemic. Current studies associating social capital with COVID-19 response suffer from several caveats. First, the majority of current studies have measured social capital using an index created by combining various forms or indicators (e.g., the Putnam social capital index, the U.S. Congress social capital measure, and the Penn State social capital measure), thereby obscuring the differential roles that different forms of social capital may play. There is a need to be more explicit about how different forms of social capital work (Carpiano and Moore Citation2020). Second, current studies have considered the association between social capital and COVID-19 response mainly at the place level (e.g., across counties, states, or countries). Largely overlooked is the corresponding processes at the individual level (see also Coleman Citation1990; Wu Citation2020a). Third, current studies have a dominant focus on social capital and the COVID-19 response in democratic regimes and the United States. However, because the role of social capital and COVID-19 response could both vary across different political contexts (Herrmann-Pillath Citation2010; Bartscher et al. Citation2020; Wu et al. Citation2020), understanding how social capital matters for COVID-19 response will also require considering how it might matter in an authoritarian context.
To detect the mechanisms underlying how social works, in this article I develop a multidimensional and multilevel approach that considers the effects of social capital in different forms and at different levels. Indeed, social capital is a multidimensional concept that consists of various forms such as trust, norms, and social network (Coleman Citation1990; Putnam Citation2000; see also Carpiano and Moore Citation2020). Different forms of social capital have different implications as they can imply different resources, levels of support, and obligations (Ferlander Citation2007; Moore and Kawachi Citation2017). Social capital is also a multilevel construct that can be analyzed at both the individual level as well as the contextual level (Carpiano and Moore Citation2020). At different levels, social capital can yield distinct influences on social outcomes (Poortinga Citation2006; Yip et al. Citation2007; Beugelsdijk Citation2009). The effects of social capital across forms and levels can also be culturally specific (Herrmann-Pillath Citation2010). Hence, this new approach comparing the potential dissimilar effects of social capital in different forms and at different levels as well as across contexts can help detect the specific processes underlying how social capital affects response to the COVID-19 pandemic.
To illustrate this multidimensional and multilevel approach, I study how several different forms of social capital including social trust, confidence in institutions, collective efficacy, and social network might affect an individual’s exposure to COVID-19 in Hubei province, the epicenter of the outbreak in China (Qian and Hanser Citation2020). In so doing, this study also fills the gap in literature on how social capital might affect COVID-19 response differently in an authoritarian context. My analysis of data from a survey I conducted in late April 2020 confirms that social capital in different forms and at different levels affect individual exposure to COVID-19 differently in China. In terms of its forms—collective efficacy, social network, and, in particular, political trust—all show significant impacts, but social trust yields no effect in China. Elsewhere, social trust is found to be significant in Western democracies (see e.g., Wu et al. Citation2020). In terms of its levels, while political trust affects individual exposure to COVID-19 at both the individual level and the contextual level, collective efficacy operates mainly at the individual level and social network operates mainly at the contextual level. My additional analysis using data from the most recent wave of the WVS (2016–2020) confirms some of the patterns at the country level. It shows that social and political trust both produce significant impacts on the reduction of the COVID-19 spread, whereas social activism and political participation seem to increase the spread. With controlling for confounding variables such as GDP per capita, health expense, and inequality, the effects of social activism and political participation become nonsignificant. These patterns suggest that social capital affects COVID-19 response mainly through facilitating collective actions and promoting public acceptance of and compliance with control measures in the form of trust and norms at the individual level.
In sum, several conclusions can be drawn from these findings. On a broader level, the results show that different forms of social capital as well as different levels can yield distinctive impacts in response to the COVID-19 pandemic. On a more granular level, I find that in authoritarian China, political trust plays a greater role than social trust in slowing the community spread of COVID-19. At the individual level, social capital in forms of political trust and collective efficacy can increase people’s compliance with control measures thereby slowing the spread of COVID-19. At the contextual level, social networks can help mobilize community resources in fighting against the COVID-19 pandemic. However, this effect is found only at the district or county level. Cross-nationally, network social capital in the form of social activism and political participation shows no significant effects.
Social capital and COVID-19
Social capital has become a tremendously popular concept across social sciences. Its popularity comes from the fact that it can explain a wide range of social phenomenon such as economic growth (Fukuyama Citation1995; Knack and Keefer Citation1997; Tavits Citation2006), quality of government (Putnam Citation1993; Rothstein Citation2003), and people’s health and well-being (Lin Citation2002; Helliwell, Huang, and Wang Citation2014). More recently, a growing body of literature also suggests that social capital even plays a critical role in preventing and controlling epidemics such as SARS, Ebola, and Zika outbreaks as well as the various strains of HN influenzas (e.g., Dynes Citation2006; Koh and Cadigan Citation2008; Aldrich Citation2010, Citation2012; Rönnerstrand Citation2014; Chuang et al. Citation2015; Ali et al. Citation2016; Blair, Morse, and Tsai Citation2017; Wilkinson and Fairhead Citation2017; Vinck et al. Citation2019; Trapido Citation2019). For example, Rönnerstrand (Citation2014) shows that social capital has a positive impact on individuals’ intention to fight against the 2009 H1N1 pandemic in Sweden and the United States. Similarly, Chuang et al. (Citation2015) find that social capital is positively associated with people’s intention to accept vaccinations, to wash their hands more frequently, and to wear a face mask during an influenza pandemic in Taiwan. Low social capital, on the other hand, can explain low compliance with control interventions and high refusal to adopt preventive behaviors (Blair, Morse, and Tsai Citation2017; Vinck et al. Citation2019).
Indeed, while only a few months have passed since the World Health Organization (WHO) declared the COVID-19 outbreak as a global pandemic on March 11, 2020, a number of studies have already shown that social capital can explain why some locations are documenting higher caseloads of COVID-19 infections than others (e.g., Bai, Jin, and Wan Citation2020; Barrios et al. Citation2020; Bartscher et al. Citation2020; Borgonovi and Andrieu Citation2020; Ding et al. Citation2020; Fraser and Aldrich Citation2020; Kuchler, Russel, and Stroebel Citation2020; Markridis and Wu Citation2020; Varshney and Socher Citation2020; Wu et al. Citation2020). provides an overview of these existing studies. It includes information about the authors, date of the online publication, title of the study, site of focus and unit of analysis, measures of social capital and COVID-19 outcomes as well as their main findings. These studies largely find that places with more social capital tend to have more positive responses to the COVID-19 pandemic and fewer confirmed cases as well as a slower growth rate of infection over time.
Table 1. Overview of existing studies on social capital and COVID-19.
However, several more specific patterns from these studies require further attention. First, the effect of social capital seems to be time sensitive. In Japan, Fraser and Aldrich (Citation2020) find that prefectures with strong bridging and linking social ties start out more susceptible to COVID-19 spread, but their rates quickly decrease over time compared to those with stronger intra-group ties. Similarly, Bartscher et al. (Citation2020) show that the number of COVID-19 cases is initially higher in high social-capital areas, but as information on the virus spreads, high-social-capital areas start to show a slower increase in COVID-19 cases in seven countries: Austria, Germany, Italy, the Netherlands, Sweden, Switzerland, and the U.K.
Second, it seems that the association between social capital and the spread of COVID-19 can change according to government policies in controlling the spread. In fact, Borgonovi and Andrieu (Citation2020) have also argued that social capital is most needed when lockdowns, social distancing, and other control measures are not enforced in the beginning of the pandemic. However, the effect of social capital will diminish when strict control policies are in place (Borgonovi and Andrieu Citation2020). Wu et al. (Citation2020) also point out that social capital may be especially important in democratic societies, as compliance cannot be ensured by more forceful means.
Third, conclusions from these studies are sometimes contradictory. In the United States, for example, Kuchler, Russel, and Stroebel (Citation2020) find that regions with stronger social ties to early COVID-19 hotspots such as Westchester County in New York have more documented COVID-19 cases per resident. However, Makridis and Wu (Citation2020) show that social capital can help communities weather the spread: more social capital leads to lower levels of infection and slows the average week-to-week growth in infections across more than 2,700 U.S. counties. Bai, Jin, and Wan (Citation2020) find that U.S. counties with higher civic norms have higher levels of social distancing behavior, whereas counties with higher density of social networks have lower levels of social distancing behavior.
Current studies also suffer from several caveats. First, researchers have largely failed to be more explicit about how they are conceptualizing social capital in their current studies. Instead, they have relied on an overall index of social capital such as the Putnam social capital index, the U.S. Congress social capital measure, and the Penn State social capital measure. Each of these indexes combines various forms of social capital such as trust, community participation, network, and ties, thereby obscuring the differential roles that different forms of social capital may play.
Second, these studies have considered the association between social capital and the response to COVID-19 only at the place level, such as county or state, in the United States (Markridis and Wu Citation2020; Wu et al. Citation2020), at the provincial level in Italy (Bartscher et al. Citation2020; Kuchler, Russel, and Stroebel Citation2020), and at the prefecture level in Japan (Fraser and Aldrich Citation2020). One reason is that social capital is widely conceptualized as a characteristic of place (see also Galea et al. Citation2002; Wu Citation2020a). However, social capital can also be analyzed at the individual level. In fact, to understand how social capital and the spread of COVID-19 are related at the place level, it is important to study the corresponding processes at the individual level (see also Coleman Citation1990; Wu et al. Citation2020). In addition, certain mechanisms that are potentially operating at one level might not be applicable at another level (Carpiano and Moore Citation2020).
Finally, these studies have exclusively focused on democratic regimes. In fact, seven out of the ten studies in have a U.S. focus. However, the role of social capital could vary across different political contexts. On one hand, social capital may be especially important in democratic societies, as compliance cannot be ensured by more forceful means (Wu et al. Citation2020). On the other hand, in authoritarian regimes where there are stricter policies and more forceful implementation, containment may depend less on social capital (Bartscher et al. Citation2020). Hence, understanding how social capital matters for COVID-19 response will also require considering how it might matter in an authoritarian context and cross-nationally.
Consequently, what the channels are through which social capital makes locations more likely to respond to the pandemic remains less clear. There are several potential processes. For example, communities with more social capital might be better able to mobilize resources and foster collective actions in times of crisis. Individuals with more social capital might be more willing to comply with control polices and adopt vital new behaviors such as social distancing and wearing a face mask. There is also the possibility that regions with more social capital might be more likely to see physical interactions between their residents, providing increased opportunities for the virus to spread. To detect the potential mechanism, I introduce a multidimensional and multilevel approach that considers the effects of social capital in different forms, at different levels, and across contexts. The caveats found in current studies as well as the time sensitive and sometimes contradictory findings also demonstrate a strong need to further investigate how social capital really matters for COVID-19 response. In particular, we need to be more explicit about how various forms of social capital can work differently and at what levels they operate (see also Carpiano and Moore Citation2020). There is also a need to consider how the role of social capital may change across contexts (see also Borgonovi and Andrieu Citation2020; Wu et al. Citation2020).
A multidimensional and multilevel approach
Social capital is a multidimensional concept. It exists in different forms including trust, norms, and social networks (Coleman Citation1988; Putnam Citation2000; Rice Citation2001; Wu Citation2020b; Moore and Carpiano Citation2020). Trust refers to one’s faith in other people and also their confidence in institutions (Putnam Citation1995; Wu and Shi Citation2020). While norms are seldom defined in current literature, they often refer to forms of social support and collective efficacy (Ferlander Citation2007). Finally, network means social ties through group membership and social participation that can generate benefits or profits for individuals and social groups (Bourdieu Citation1986; Coleman Citation1990; Lin Citation2002).
Previous research has suggested that that not all forms of social capital are equally important in affecting social outcomes (e.g., Messner, Rosenfeld, and Baumer Citation2004; Yip et al. Citation2007; Sampson and Graif Citation2009; Carpiano and Moore Citation2020). For example, while trust and civic norms are building blocks of a good and prosperous society (Putnam Citation1995, Citation2000; Putnam et al. Citation1994; Fukuyama Citation1995), social ties and network relations can be used for different purposes including good, bad, or neutral (Coleman Citation1990; see also Rice Citation2001). Indeed, different types of social capital can capture different aspects of the social environment (Poortinga Citation2012), and imply different resources, support and obligations (Ferlander Citation2007). Accordingly, different forms of social capital can affect social outcomes through different means, and may also lead to different consequences (Moore and Kawachi Citation2017).
Social capital can be conceptualized as property of both individuals and communities (Lin Citation2002; Kawachi Citation2006; see also Ferlander Citation2007), and therefore can be analyzed at both the individual level and the contextual level (Carpiano and Moore Citation2020). As a multilevel construct, social capital at different levels can yield distinct influences (Yip et al. Citation2007; Beugelsdijk Citation2009). For example, while at the individual level, social capital indicates more about shared individual values and norms as well as resources that are available to, and chosen by, individuals. At the contextual level, social capital captures more about the community features that individuals have less control over and resources that cannot be created by individuals alone (Yip et al. Citation2007). Carpiano and Moore (Citation2020) recently point out that to ensure the fruitful progression and evolution of social capital research, it is essential for researchers to not only be explicit about what forms of social capital they study, but also at what levels they are studied at.
Given that different forms of social capital have different implications and at different levels can yield distinct influences, there is a need to study how social capital in different forms and at different levels may affect the COVID-19 response. In so doing, it will help detect the underlying processes. There are two major reasons for why this is the case. First, different forms of social capital can affect social outcomes through different means and therefore comparing the dissimilar effects can help us understand more about the specific processes that social capital works. Second, social capital can be a multilevel construction and certain mechanisms that are potentially operating at one level might not be applicable to another level (Carpiano and Moore Citation2020). Different effects of social capital at different levels will also tell us whether social capital affect response to COVID-19 as an individual property or as a collective property.
In fact, several studies have already shown that different forms of social capital can yield differential impacts on COVID-19 response. In explaining why U.S. counties respond differently to COVID-19, for example, Ding et al. (Citation2020) have separated between two forms of social capital—community engagement and individual commitment to social institutions—and they find that in counties where there is stronger community engagement, the sensitivity of social distancing to both local COVID-19 cases and statewide mobility restrictions tends to be weaker, while in counties with higher individual commitment to social institutions, the sensitivity of social distancing is stronger. The opposite influences of these two forms of social capital on social distancing tell us that social capital slows the spread of COVID-19 not through social network and ties, but through individuals’ greater commitment to achieving a common goal. Similarly, Bai, Jin, and Wan (Citation2020) find that U.S. counties with higher civic norms have higher levels of social distancing behavior, whereas counties with higher density of social networks have lower levels of social distancing behavior. This suggests that social capital can affect COVID-19 response through two differential means. On one hand, civic norms facilitate cooperation and self-sacrifice for the common good, leading to individuals’ higher compliance with social distancing. On the other hand, social networks increase individual embeddedness and hence inertia in maintaining social interactions, making social distancing more difficult to practice.
To illustrate the multidimensional and multilevel approach, I turn to China and consider how different forms of social capital and at different levels might affect an individual’s exposure to COVID-19 in Hubei province. I focus on four forms of social capital, namely, social trust, political trust, collective efficacy, and social network. In the case of social capital and the COVID-19 response, context also matters. In democratic societies, social capital may be especially important as compliance cannot be ensured by more forceful means (Wu et al. Citation2020). In authoritarian China, however, collective actions may depend less on social capital, but more on forceful means (see also Putnam et al. Citation1994). Accordingly, different forms of social capital may play differential roles in shaping the COVID-19 response, and they may also exert differential effects in authoritarian China than in Western democracies. Additionally, I analyze data from the most recent wave of the WVS and consider how different forms of social capital affect COVID-19 spread at the country level.
Data and methods
Data
The data for this study come from several sources. To test how social capital in different forms and at different levels affect COVID-19 response in China, I conducted an online survey from April 22 to April 28, 2020, in the immediate aftermath of the reopening of the city of Wuhan. Funded by Canadian Institute of Health Research (CIHR), the survey was carried out to gather information on Chinese people’s experiences with the outbreak, their social contacts with family, friends and neighbors as well as their values and behaviors during the crisis. I collaborated with seventeen academics in China. Each faculty member further recruited more university students as interviewers. In total, 613 university students from 53 universities across China joined our team. This served to ensure that the survey was widely distributed across all regions.
We designed an innovative approach to capture aspects of face-to-face survey approaches. We assigned each team leader a unique access code for his or her survey link, to protect and monitor each survey. To conduct an interview, each interviewer would reach out to people in his or her contacts and ask their permission first before sending them the link and an access code that would enable them to fill out the survey. The purpose of this approach was to ensure meaningful engagement with the survey like a face-to-face situation. Respondents were told that their responses would be anonymous. Thus, the survey differed from online surveys that are simply posted through online platforms and where there is little knowledge of respondents.
Using the unique access code, we generated daily reports showing gender and age distributions of respondents overall and separately for each team. In so doing, team leaders and student interviewers could see their own sample distribution, and the overall distributions by gender and age each day. With these daily updates, they were asked to adjust their survey respondents for the next day. Specific guidelines and training sessions were conducted via Zoom. Interviewers were instructed to interview only one individual per household and to aim to generate a gender- and age-balanced sample.
Questionable entries were removed in the data cleaning process. This included respondents who submitted the survey within 200 seconds (3.3 min) and those who indicated that their age was under 15 years old or over 100 years old. In this study, however, I focus on respondents from Hubei province only. Hubei is the epicenter of the outbreak where more than 80 percent of China’s confirmed cases were documented. In the end, I obtained an analyzable total of the 3,250 respondents from across Hubei, including 103 districts or counties in 13 Hubei cities.
As the data collection in China was nonrandom, it should be acknowledged that it is therefore subject to the kinds of biases associated with this kind of sampling. Nonetheless, to further support the main findings, I replicate the analysis at the country level using data from the most recent wave of WVS (2016–2020) (Inglehart et al. Citation2020). The fieldwork for this wave of WVS was conducted from 2017 to early 2020, and the data was officially released on July 20, 2020. The WVS (2016–2020) data includes macro-level variables for each nation such as per capita GDP, measures of social inequality, health expensive, mean schooling, and level of democracy. The final dataset I use here includes forty-seven countries.
Measures
Several forms of social capital I consider here includes social trust, political trust, collective efficacy, and social network. At the individual level, social trust is measured using an index that ranges from 2 to 10 and was created from combining two question items: People in my neighborhood are willing to help each other (1 = strongly disagree, 2 = disagree,3 = neither agree nor disagree, 4 = agree, and 5 = strongly agree); and People in my neighborhood can be trusted (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, and 5 = strongly agree). While Sampson, Raudenbush, and Earls (Citation1997) have used these items to measure social cohesion, others show these items in fact reflect social trust (Wu and Shi Citation2020). Nonetheless, my additional analysis using the single item whether most people can be trusted yields similar findings.
Political trust is measured using an additive index that ranges from 0 to 5 by combing people’s trust in government (0 = no, 1 = yes) at five different levels, including township, county, city as well as provincial and national levels. While it is important to differentiate people’s trust in government at different levels since they could indicate Chinese’s hierarchical trust orientation (see Wu and Wilkes Citation2018a; Citation2018b), here I use this additive index to capture people’s trust in political institutions in general. An analysis of the scale reliability coefficient of these five items shows a Cronbach’s alpha of 0.86.
Collective efficacy is captured using two items: When I see children scribbling on the wall carelessly in my neighborhood, I will go up to stop them (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, and 5 = strongly agree); and When I see children fighting against each other in my neighborhood, I will go up to stop them (1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree, and 5 = strongly agree). The combined index of collective efficacy ranges from 2 to 10.
Social network is also measured using two items. First, I know what people do for a living in my neighborhood? (1 = none, 2 = a few of them, 3 = more than half of them, and 4 = almost everyone). Second, how often do you talk with your neighbors? (1= less than twice a month, 3 = several times a week, 2 = once a week, and 4 = almost daily). The social network index ranges from 2 to 8.
At the contextual level, I created the respective measures for social trust, political trust, collective efficacy, and social network by calculating the overall mean for each measure across all 103 districts or counties in my analysis. The goal of this study is to test how these four forms of social capital at both the individual and the district or county level affect an individual’s exposure to COVID-19.
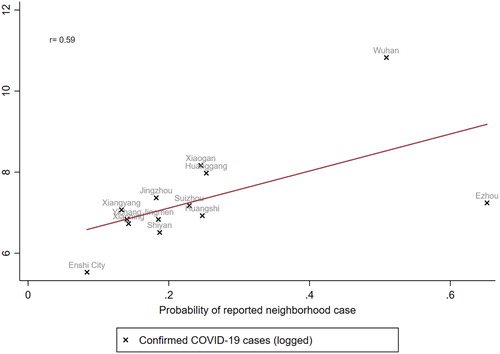
To measure an individual’s exposure to COVID-19, in the survey we asked whether the respondent knew someone who had been infected with COVID-19 in the neighborhood (0 = no, 1 = yes). To test whether this measure can well capture the spread of COVID-19 in Hubei province, I consider how the aggregated probabilities across thirteen Hubei cities correlate the actual numbers of confirmed cases as documented in DXY’s COVID-19 Global Pandemic Real-Time Report. shows the actual number of confirmed cases for each city. For example, as of June 4, there are a total of 50,340 confirmed cases in Wuhan city, the epicenter of the outbreak. shows the scatterplot between the city-level exposure to COVID-19 that I created from the survey and the actual number of cases across twelve cities in Hubei (Ezhou was removed due to its small sample size). As it shows, these two measures are highly correlated (Pearson’s r = 0.94), suggesting that the probability of knowing someone who had COVID-19 in the neighborhood can capture the spread of the virus in Hubei province quite well.
Figure 1. Confirmed COVID-19 cases across Hubei cities. Note: Data on the actual number of confirmed cases for each city come from DXY’s COVID-19 Global Pandemic Real-Time Report (June 4, 2020): https://ncov.dxy.cn/ncovh5/view/en_pneumonia?from=dxy&source=&link=&share=

Figure 2. Scatterplot between community exposure to COVID-19 and the actual number of confirmed cases (logged) across Hubei cities.
In the analysis, I also include controls that capture district- or county-level backgrounds such as level of household income, population education, and level of urbanization. At the individual level, I control for individual demographics including age, gender, urban or rural residency, level of education, and household income. Table A1 in the Appendix provides the summary statistics of key variables in analysis.
At the country level, I measure different forms of social capital using data from the most recent wave of the WVS (2016–2020). I separate between four forms of social capital, namely, social trust, political trust, social activism, and political participation. Social trust is measured using the single item whether most people can be trusted and political trust is measured by individual’s confidence in national government. Social activism is measured by combining respondents’ binary responses to donating to a group or campaign, contacting a government official, encouraging others to take action regarding political issues, and encouraging others to vote. Political participation includes respondents’ binary responses to signing a petition, joining in boycotts, attending lawful/peaceful demonstrations, and joining unofficial strikes. I use their aggregated forms to indicate country-level social capital. Finally, I combine the survey data with data on the spread of COVID-19 collected by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU).
Findings
The China survey
shows, respectively, the scatterplots at the district or county level between four different forms of social capital and an individual’s exposure to COVID-19 as indicated using the probability of a respondent knowing someone who had COVID-19 in their neighborhood.
Figure 3. Scatterplots between the probability of reported neighborhood COVID-19 cases with social trust (A), political trust (B), collective efficacy (C), and social network (D).
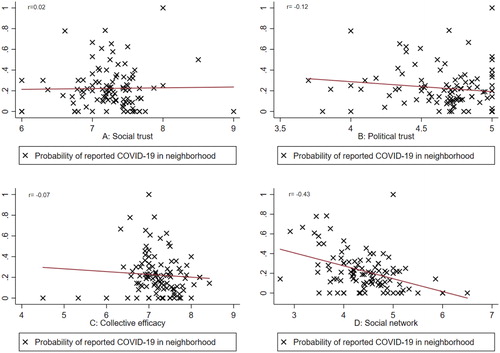
Clearly, we see that the association between exposure to COVID-19 and social capital varies across its different forms. While social trust (r = 0.02) and collective efficacy (r = −0.07) are weakly associated with exposure to COVID-19, political trust (−0.12) and in particular social network (−0.43) are strongly and negatively related to community exposure to COVID-19. This suggests that respondents from districts or counties with more political trust and social network were less likely to report that they knew someone who had COVID-19.
Next, I use multilevel logistic models that include a random intercept component at the district or county level to predict how different forms of social capital might affect the spread of COVID-19. provides a visualization of these modeling results (for full results, please refer to Table A2 in the Appendix). In each model, I control district- or county-level backgrounds such as level of household income, population education, and level of urbanization as well as individual demographics including age, gender, urban or rural residency, education and household income that might also capture some aspects of the neighborhood contexts.
Figure 4. Effects of different forms of social capital on the spread of the COVID-19 virus (odds ratio).
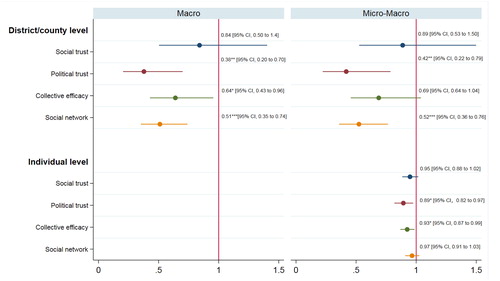
The first four models test how different forms of social capital at the district or county level might affect individual exposure to COVID-19. Model (1) shows that respondents from a district or county with more social capital were less likely to report that they knew someone who had COVID-19 in their neighborhood (odds ratio = 0.84). However, the effect does not seem to be significant. In contrast, political trust, collective efficacy, and social network are all found to significantly affect the diffusion of the COVID-19 virus. Model (2) shows that any one unit increases in political trust in respondents’ district or county would lead to 62 percent less odds of reporting a confirmed COVID-19 case in their neighborhood. This number is 36 percent for collective efficacy and 49 percent for social network. These findings suggest that, after controlling for individual demographics and district- or county-level backgrounds, district- or county-level collective efficacy, social network and political trust in particular all play essential roles in containing the spread of the COVID-19 virus.
Respectively, Model (5) to Model (8) add individual-level social trust, political trust, collective efficacy, and social network to the first four models. In so doing, we can test the macro-micro processes of how different forms of social capital might affect the likelihood of a respondent reporting a confirmed case in the neighborhood. Combining both the individual and the district- or county-level social capital constructs, Model (5) shows that social trust yields no significant effect at both levels. In contrast, Model (6) shows that political trust has a strong and significant impact at both levels. Model (7) shows that the effect of collective efficacy becomes nonsignificant at the district or county level, but it shows a significant effect at the individual level, suggesting that it operates mainly at the individual level. Model (8) shows an opposite pattern for the effect of social network. While at the individual level, it does not seem to have a significant impact, at the district or county level, its negative effect remains highly significant.
The world values survey
shows, respectively, the scatterplots at the country level between four different forms of social capital and the spread of COVID-19 as indicated using the logged form of COVID-19 cases per 100,000 population. These figures show that while social trust and political trust are negatively associated with the COVID-19 spread, social activism and political participation seem to increase the spread of the COVID-19.
Figure 5. Scatterplots between COVID-19 cases with social trust (A), political trust (B), social activism (C), and political participation (D).
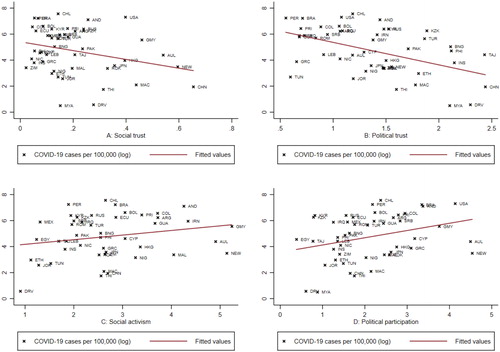
Next, I use multivariable regressions to estimate how these four forms of social capital might predict the COVID-19 spread across countries. The spread of COVID-19 is indicated using the logged form of COVID-19 cases per 100,1000 population. Results confirm that social and political trust have negative impacts on the spread of COVID-19, while social activism and political participation seem to increase the spread. However, when country level background such as GDP per capita, social inequality, share of urban population as well as health expense are controlled, the positive effects of social activism and political participation do not reach any level of significance (for full results, refer to Table A3 in the Appendix).
Conclusion
While the concept of social capital has been highly criticized as being “theoretically underdetermined and fuzzy” (Herrmann-Pillath Citation2010:327; Bjørnskov and Sønderskov Citation2013; Carpiano Citation2006), it is nevertheless a useful one because, as Christoforou (Citation2013:720) points out, it highlights “aspects of human agency, particularly individuals’ capability to serve wider public benefits of social welfare based on a sense of social obligation and shared identity.” Most recently, a growing literature shows that social capital can largely explain the differences in community response and therefore affect the spread of COVID-19 (e.g., Bai, Jin, and Wan Citation2020; Barrios et al. Citation2020; Bartscher et al. Citation2020; Borgonovi and Andrieu Citation2020; Ding et al. Citation2020; Fraser and Aldrich Citation2020; Kuchler, Russel, and Stroebel Citation2020; Markridis and Wu Citation2020; Varshney and Socher Citation2020; Wu et al. Citation2020). Conclusions from these studies, however, are inconsistent and sometimes contradictory. It remains unclear what the channels are through which social capital affects the spread of COVID-19.
In this research, I have introduced a multidimensional and multilevel approach that considers how social capital in different forms and at different levels might affect COVID-19 response differently. My analyses of data from a China survey as well as the most recent wave of the WVS (2016–2020) illustrate that social capital in different forms and at different levels can affect the COVID-19 response in very different ways, and their effects can also vary across regime contexts. In particular, the dissimilar effects of social capital in different forms and at different levels help detect the processes underlying how social capital affects responses to the pandemic. The finding that cognitive social capital in the form of trust and norms has a stronger impact than structural or network social capital in the form of social activism and political participation suggests that social capital largely affects COVID-19 response through facilitating cooperation and self-sacrifice for the common good and promoting public acceptance of and compliance with control measures (see also Bai, Jin, and Wan Citation2020). The finding that political trust plays a greater role than social trust in China suggests that public acceptance of, and compliance with, control measures might depend on forceful top-down means in an authoritarian context. In democratic societies, social trust is also significant as compliance cannot be ensured by more forceful means (Wu et al. Citation2020). These differences suggest that social capital can play varying roles across contexts. The finding that collective efficacy mainly operates at the individual level shows that individual actions can collectively help solve social problems for the common good. Finally, the finding that social network operates mainly at the macro level suggests that at a contextual level, social networks can help communities to better mobilize resources in times of crisis. However, at the country level, some evidence also shows that social activism and political participation might lead to COVID-19 risk.
Ultimately, this study demonstrates that, to ensure fruitful progression, we need to be mindful that social capital is a multidimensional and multilevel concept (Gannon and Roberts Citation2018; Carpiano and Moore Citation2020). First, there is a need to be more explicit about how we are conceptualizing social capital in terms of its various forms, and at what level (e.g., individual or contextual) social capital is producing its effects (Carpiano and Moore Citation2020). Second, we also need to recognize that social capital and its different forms can play varying roles across political contexts. Finally, more social capital is not always better—there are also potential downsides of social capital (Portes Citation2014; Gannon and Roberts Citation2018). The multidimensional and multilevel approach I introduce here can be easily adapted to study how social capital affect other outcomes across different contexts.
Acknowledgements
The author thanks Alicia Filipowich, Christos Makridis, Yue Qian, Chloe Sher, two anonymous reviewers, and editor Xiaogang Wu for their helpful comments and suggestions. The author also gratefully acknowledges the assistance from Zhilei Shi, Dongxia Zhou, Yu Tan, Xiao Zang, Jiaji Wu, Ping Xiong, Zhiwen Gong, Libin Cao, Feng Zhao, Xiaojun Zhang, Nengkun He, Xiufang Yin, Liyong Yang, Qinghua Chu, Hao Zhou, Weijun Lai, Ruijing Tian and 613 university student volunteers across China in data collection.
Additional information
Funding
Notes on contributors
Cary Wu
Cary Wu ([email protected]) is an assistant professor of Sociology at York University in Toronto, Canada. His research focuses on political culture and inequality has appeared in such journals as Social Science Research, The Sociological Quarterly, Social Forces, Urban Studies, Geoforum, International Political Science Review, and International Journal of Comparative Sociology.
References
- Aldrich, D. P. 2010. “Fixing Recovery, Social Capital in Post-Crisis Resilience.” Journal of Homeland Security 6:1–10.
- Aldrich, D. P. 2012. Building Resilience: Social Capital in Post-Disaster Recovery. Chicago: University of Chicago Press.
- Ali, H., B. Dumbuya, M. Hynie, P. Idahosa, R. Keil, and P. Perkins. 2016. “The Social and Political Dimensions of the Ebola Response: Global Inequality, Climate Change, and Infectious Disease.” In Climate Change and Health, 151–69. Cham: Springer.
- Bai, J. J., W. Jin, and C. Wan. 2020. “The Impact of Social Capital on Individual Responses to COVID-19 Pandemic: Evidence from Social Distancing.” SSRN paper. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3609001
- Barrios, J. M., E. Benmelech, Y. V. Hochberg, P. Sapienza, and L. Zingales. 2020. Civic Capital and Social Distancing during the Covid-19 Pandemic (No. w27320). National Bureau of Economic Research. https://www.nber.org/papers/w27320
- Bartscher, A. K., S. Seitz, M. Slotwinski, S. Siegloch, and N. Wehrhöfer. 2020. Social Capital and the Spread of Covid-19: Insights from European Countries. https://www.iza.org/publications/dp/13310/social-capital-and-the-spread-of-covid-19-insights-from-european-countries
- Beugelsdijk, S. 2009. “A Multilevel Approach to Social Capital.” International Studies of Management & Organization 39 (2):65–89. doi:10.2753/IMO0020-8825390203.
- Bjørnskov, C., and K. M. Sønderskov. 2013. “Is Social Capital a Good Concept?” Social Indicators Research 114 (3):1225–42. doi:10.1007/s11205-012-0199-1.
- Blair, R. A., B. S. Morse, and L. L. Tsai. 2017. “Public Health and Public Trust: Survey Evidence from the Ebola Virus Disease Epidemic in Liberia.” Social Science & Medicine (1982) 172:89–97. doi:10.1016/j.socscimed.2016.11.016.
- Borgonovi, F., and E. Andrieu. 2020. “Bowling Together by Bowling Alone: Social Capital and Covid-19.” Covid Economics 17:73–96.
- Bourdieu, P. 1986. “The Forms of Capital.” In Handbook of Theory and Research for the Sociology of Education, edited by J. G. Richardson, 241–58. New York: Greenwood.
- Carpiano, R. M. 2006. “Toward a Neighborhood Resource-Based Theory of Social Capital for Health: Can Bourdieu and Sociology Help?” Social Science & Medicine 62 (1):165–75. doi:10.1016/j.socscimed.2005.05.020.
- Carpiano, R. M., and S. Moore. 2020. “So What’s Next? Closing Thoughts for This Special Issue and Future Steps for Social Capital and Public Health.” Social Science & Medicine 257:113013. doi:10.1016/j.socscimed.2020.113013.
- Christoforou, A. 2013. “On the Identity of Social Capital and the Social Capital of Identity.” Cambridge Journal of Economics 37 (4):719–36. doi:10.1093/cje/bes059.
- Chuang, Y. C., Y. L. Huang, K. C. Tseng, C. H. Yen, and L. H. Yang. 2015. “Social Capital and Health-Protective Behavior Intentions in an Influenza Pandemic.” PLoS One 10 (4):e0122970. doi:10.1371/journal.pone.0122970.
- Coleman, J. S. 1988. “Social Capital in the Creation of Human Capital.” American Journal of Sociology 94:S95–120. doi:10.1086/228943.
- Coleman, J. S. 1990. Foundations of Social Theory. Cambridge: Harvard University Press.
- Ding, W., R. Levine, C. Lin, and W. Xie. 2020. Social Distancing and Social Capital: Why US Counties Respond Differently to COVID-19. Available at SSRN 3624495. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3632620
- Dynes, R. 2006. “Social Capital: Dealing with Community Emergencies.” Homeland Security Affairs 2 (2):1–26.
- Ferlander, S. 2007. “The Importance of Different Forms of Social Capital for Health.” Acta Sociologica 50 (2):115–28. doi:10.1177/0001699307077654.
- Fraser, T., and D. P. Aldrich. 2020. Social Ties, Mobility, and COVID-19 spread in Japan. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3544373
- Fukuyama, F. 1995. Trust: The Social Virtues and the Creation of Prosperity (Vol. 99). New York: Free Press.
- Galea, S., J. Ahern, H. Resnick, D. Kilpatrick, M. Bucuvalas, J. Gold, and D. Vlahov. 2002. “Psychological Sequelae of the September 11 Terrorist Attacks in New York City.” New England Journal of Medicine 346 (13):982–7. doi:10.1056/NEJMsa013404.
- Gannon, B., and J. Roberts. 2018. “Social Capital: Exploring the Theory and Empirical Divide.” Empirical Economics 58 (3):899–919.
- Helliwell, J. F., H. Huang, and S. Wang. 2014. “Social Capital and Well-Being in Times of Crisis.” Journal of Happiness Studies 15 (1):145–62. doi:10.1007/s10902-013-9441-z.
- Helliwell, J. F., and R. D. Putnam. 2004. “The Social Context of Well–Being.” Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences 359 (1449):1435–46. doi:10.1098/rstb.2004.1522.
- Herrmann-Pillath, C. 2010. “Social Capital, Chinese Style: Individualism, Relational Collectivism and the Cultural Embeddedness of the Institutions–Performance Link.” China Economic Journal 2 (3):325–50. doi:10.1080/17538960903529568.
- Inglehart, R., C. Haerpfer, A. Moreno, C. Welzel, K. Kizilova, J. Diez-Medrano, M. Lagos, P. Norris, E. Ponarin & B. Puranen. (eds.). 2020. World Values Survey: Round Seven - Country-Pooled Datafile Version. Madrid: JD Systems Institute. http://www.worldvaluessurvey.org/WVSDocumentationWV7.jsp.
- Kawachi, I. 2006. “Commentary: Social Capital and Health: Making the Connections One Step at a Time.” International Journal of Epidemiology 35 (4):989–93. doi:10.1093/ije/dyl117.
- Kawachi, I., S. V. Subramanian, and D. Kim. 2008a. “Social Capital and Health.” In Social Capital and Health, 1–26. New York: Springer.
- Kawachi, I., S. V. Subramanian, and D. Kim, (eds.). 2008b. Social Capital and Health. New York: Springer.
- Kawachi, I., S. V. Subramanian, and D. Kim, (eds.). 2008c. Social Capital and Health. New York: Springer.
- Knack, S., and P. Keefer. 1997. “Does Social Capital Have an Economic Payoff? A Cross-Country Investigation.” The Quarterly Journal of Economics 112 (4):1251–88. doi:10.1162/003355300555475.
- Koh, H. K., and R. O. Cadigan. 2008. “Disaster Preparedness and Social Capital.” In Social Capital and Health, 273–85. New York, NY: Springer.
- Kokubun, K. 2020. “Social Capital May Mediate the Relationship between Social Distance and COVID-19 Prevalence.” arXiv preprint arXiv:2007.09939. https://arxiv.org/abs/2007.09939
- Kuchler, Theresa, Dominic Russel, and Johannes Stroebel. 2020. “The Geographic Spread of COVID-19 Correlates with Structure of Social Networks as Measured by Facebook.” NBER working paper. https://arxiv.org/abs/2004.03055
- Lin, N. 2002. Social Capital: A Theory of Social Structure and Action (Vol. 19). New York: Cambridge University Press.
- Makridis, C. A., and C. Wu. 2020. “Ties that Bind (and Social Distance): How Social Capital Helps Communities Weather the COVID-19 Pandemic.” SSRN working paper. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3592180
- McLachlan, H. 2020. “Why ‘There’s No Such Thing as Society’ Should not be Regarded with Moral Revulsion.” The Conversation. Accessed August 13, 2020 from https://theconversation.com/why-theres-no-such-thing-as-society-should-not-be-regarded-with-moral-revulsion-136008
- Messner, S. F., R. Rosenfeld, and E. P. Baumer. 2004. “Dimensions of Social Capital and Rates of Criminal Homicide.” American Sociological Review 69 (6):882–903. doi:10.1177/000312240406900607.
- Miao, J., and D. Zeng. (2020). “Can Neighborhood Protect Residents from Mental Disorder during the COVID-19 Pandemic?” Chinese Sociological Review.
- Moore, S., and R. M. Carpiano. 2020. “Measures of Personal Social Capital over Time: A Path Analysis Assessing Longitudinal Associations among Cognitive, Structural, and Network Elements of Social Capital in Women and Men Separately.” Social Science & Medicine (1982) 257:112172. doi:10.1016/j.socscimed.2019.02.023.
- Moore, S., and I. Kawachi. 2017. “Twenty Years of Social Capital and Health Research: A Glossary.” Journal of Epidemiology and Community Health 71 (5):513–17. doi:10.1136/jech-2016-208313.
- Poortinga, W. 2006. “Social Relations or Social Capital? Individual and Community Health Effects of Bonding Social Capital.” Social Science and Medicine 63 (1):255–70. doi:10.1016/j.socscimed.2005.11.039.
- Poortinga, W. 2012. “Community Resilience and Health: The Role of Bonding, Bridging, and Linking Aspects of Social Capital.” Health & Place 18 (2):286–95. doi:10.1016/j.healthplace.2011.09.017.
- Portes, A. 2014. “Downsides of Social Capital.” Proceedings of the National Academy of Sciences of the United States of America 111 (52):18407–18408. doi:10.1073/pnas.1421888112.
- Putnam, R. 1993. “The Prosperous Community: Social Capital and Public Life.” The American Prospect 4:35–42.
- Putnam, R. D., R. Leonardi, and R. Y.Nanetti. 1994. Making Democracy Work: Civic Traditions in Modern Italy. Princeton University Press.
- Putnam, R. D. 1995. “Tuning In, Tuning Out: The Strange Disappearance of Social Capital in America.” PS: Political Science & Politics 28 (4):664–84.
- Putnam, R. D. 2000. Bowling Alone: The Collapse and Revival of American Community. New York: Simon and Schuster.
- Qian, Y., and A. Hanser. 2020. “How Did Wuhan Residents Cope with a 76-Day Lockdown?” Chinese Sociological Review. doi:10.1080/21620555.2020.1820319.
- Rice, T. W. 2001. “Social Capital and Government Performance in Iowa Communities.” Journal of Urban Affairs 23 (3–4):375–389. doi:10.1111/0735-2166.00095.
- Rönnerstrand, B. 2014. “Social Capital and Immunization against the 2009 A(H1N1) pandemic in the American States.” Public Health 128 (8):709–715. doi:10.1016/j.puhe.2014.05.015.
- Rothstein, B. 2003. “Social Capital, Economic Growth and Quality of Government: The Causal Mechanism.” New Political Economy 8 (1):49–71. doi:10.1080/1356346032000078723.
- Sampson, R. J., and C. Graif. 2009. “Neighborhood Social Capital as Differential Social Organization: Resident and Leadership Dimensions.” American Behavioral Scientist 52 (11):1579–605.
- Sampson, R. J., S. W. Raudenbush, and F. Earls. 1997. “Neighborhoods and Violent Crime: A Multilevel Study of Collective Efficacy.” Science (New York, N.Y.) 277 (5328):918–24. doi:10.1126/science.277.5328.918.
- Tavits, M. 2006. “Making Democracy Work More? Exploring the Linkage between Social Capital and Government Performance.” Political Research Quarterly 59 (2):211–25. doi:10.1177/106591290605900204.
- Trapido, J. 2019. “Ebola: public Trust, Intermediaries, and Rumour in the DR Congo.” The Lancet Infectious Diseases 19 (5):457–58. doi:10.1016/S1473-3099(19)30044-1.
- Varshney, L. R., and R. Socher. 2020. COVID-19 Growth Rate Decreases with Social Capital. medRxiv.
- Vinck, P., P. N. Pham, K. K. Bindu, J. Bedford, and E. J. Nilles. 2019. “Institutional Trust and Misinformation in the Response to the 2018–19 Ebola Outbreak in North Kivu, DR Congo: A Population-Based Survey.” The Lancet Infectious Diseases 19 (5):529–36. doi:10.1016/S1473-3099(19)30063-5.
- Wilkinson, A., and J. Fairhead. 2017. “Comparison of Social Resistance to Ebola Response in Sierra Leone and Guinea Suggests Explanations Lie in Political Configurations Not Culture.” Critical Public Health 27 (1):14–27. doi:10.1080/09581596.2016.1252034.
- Wu, C. 2020a. “How Does Gun Violence Affect Americans’ Trust in Each Other?” Social Science Research 91:102449. doi:10.1016/j.ssresearch.2020.102449.
- Wu, C. 2020b “Does Migration Affect Trust? Internal Migration and the Stability of Trust among Americans.” The Sociological Quarterly 61 (3):523–43.
- Wu, C., and Z. Shi. 2020. “Education and Social Trust in Transitional China.” Chinese Sociological Review 52 (2):115–43. doi:10.1080/21620555.2019.1665995.
- Wu, C., and R. Wilkes. 2018a. “Local–National Political Trust Patterns: Why China is an Exception.” International Political Science Review 39 (4):436–54. doi:10.1177/0192512116677587.
- Wu, C., and R. Wilkes. 2018b. “Finding Critical Trusters: A Response Pattern Model of Political Trust.” International Journal of Comparative Sociology 59 (2):110–38. doi:10.1177/0020715218761520.
- Wu, C., R. Wilkes, M. Fairbrother, and G. Giordano. 2020. “Social Capital, Trust, and State Coronavirus Testing.” Contexts. Accessed on May 1, 2020. https://contexts.org/blog/healthcare-and-critical-infrastructure/#wu
- Yip, W., S. V. Subramanian, A. D. Mitchell, D. T. Lee, J. Wang, and I. Kawachi. 2007. “Does Social Capital Enhance Health and Well-Being? Evidence from Rural China.” Social Science & Medicine (1982) 64 (1):35–49. doi:10.1016/j.socscimed.2006.08.027.
Appendix 1
Appendix Table A1. Descriptive statistics of key variables in analysis.
Table A2. Multilevel models predicting effects of social capital in different forms and at different levels on individual exposure to COVID-19.
Table A3. Multivariate regressions estimating effects of different forms of social capital on the spread of COVID-19.
