ABSTRACT
Background: We investigate the role of family history of cancer (FHC) and diagnosis of metachronous and/or synchronous multiple neoplasms (MN), during anti-PD-1/PD-L1 immunotherapy.
Design: This was a multicenter retrospective study of advanced cancer patients treated with anti-PD-1/PD-L1 immunotherapy. FHC was collected in lineal and collateral lines, and patients were categorized as follows: FHC-high (in case of cancer diagnoses in both the lineal and collateral family lines), FHC-low (in case of cancer diagnoses in only one family line), and FHC-negative. Patients were also categorized according to the diagnosis of MN as follows: MN-high (>2 malignancies), MN-low (two malignancies), and MN-negative. Objective response rate (ORR), progression-free survival (PFS), overall survival (OS), and incidence of immune-related adverse events (irAEs) of any grade were evaluated.
Results: 822 consecutive patients were evaluated. 458 patients (55.7%) were FHC-negative, 289 (35.2%) were FHC-low, and 75 (9.1%) FHC-high, respectively. 29 (3.5%) had a diagnosis of synchronous MN and 94 (11.4%) of metachronous MN. 108 (13.2%) and 15 (1.8%) patients were MN-low and MN-high, respectively. The median follow-up was 15.6 months. No significant differences were found regarding ORR among subgroups. FHC-high patients had a significantly longer PFS (hazard ratio [HR] = 0.69 [95% CI: 0.48–0.97], p = .0379) and OS (HR = 0.61 [95% CI: 0.39–0.93], p = .0210), when compared to FHC-negative patients. FHC-high was confirmed as an independent predictor for PFS and OS at multivariate analysis. No significant differences were found according to MN categories. FHC-high patients had a significantly higher incidence of irAEs of any grade, compared to FHC-negative patients (p = .0012).
Conclusions: FHC-high patients seem to benefit more than FHC-negative patients from anti-PD-1/PD-L1 checkpoint inhibitors.
Introduction
After the advent of immune checkpoint inhibitors (ICIs), oncology clinical practice radically changed, leading to an unprecedented improvement of cancer patients' clinical outcomes. Nevertheless, we are still a long way from predicting ICI efficacy in each patient. PD-L1 (programmed death ligand-1) protein expression, evaluated in both tumor and immune cells, is the most investigated predictive biomarkerCitation1; on the other hand, other factors such as tumor mutational burden, body mass index, and gut microbiota, have been investigated as predictors of clinical benefit from immunotherapy across different tumor types.Citation2–Citation5
Mismatch repair (MMR) deficiency, which leads to the condition of genetic hypermutability known as microsatellite instability (MSI), is related to the number of somatic mutations (especially in MSI-high cases); many studies have already confirmed its positive predictive role (MSI-high) for ICI treatment, particularly with anti-PD-1 (programmed death-1) antibodies.Citation6,Citation7 MSI is known to be the hallmark of Lynch syndrome (LS), a familial clustering of colorectal and endometrial cancers. LS is caused by several germline mutations, which result in a defective MMR and is inherited as dominant autosomal character. Similarly, BRCA 1 and 2 (Breast Cancer 1/2) mutations, which are associated with hereditary breast-ovarian cancer syndrome (HBOC), may correlate with the mutational landscape of the tumors, because of the homologous recombination repair deficiency.Citation8 Moreover, patients with inherited cancer susceptibility syndromes are more likely to develop multiple primary tumors during their life.Citation9 “BRCA-like” phenotype may be more sensitive to anti-PD-1/PD-L1 agentsCitation10; thus prospective clinical trials with anti-PD-1 for patients with germline BRCA 1/2 mutations are currently ongoing.Citation11 LS and HBOC syndrome are just two of the forms of inherited cancer susceptibility. Even though notoriously only about 5% to 10% of all cancers result directly from germline mutations,Citation12 we can hypothesize that much about family cancer syndromes and cancer predisposition is still unknown. Starting from this hypothesis and from the suggestion that tumors related to inherited cancer susceptibility syndromes seem to have an “immune sensitive phenotype,” we investigated if positive family history of cancer (FHC) and diagnosis of metachronous and/or synchronous multiple neoplasms (MN) could be somehow related to clinical outcomes with anti-PD-1/PD-L1 treatment.
In the preliminary analysis of the “FAMI-L1” study (211 patients), we found that patients with a positive FHC had higher objective response rate (ORR) and disease control rate (DCR), and prolonged time to treatment failure and overall survival (OS), while patients with diagnosis of MN only had a significantly higher DCR.Citation13 Our first hypothesis has been that the underlying mechanisms to our findings might be DNA damage repair (DDR) gene alterations.Citation14
Here, we present the updated results of the FAMI-L1 study, implemented in the study population, in order to confirm our preliminary findings.Citation13
Results
Patients’ characteristics
822 consecutive, stage IV cancer patients underwent a treatment with anti-PD-1/PD-L1. 458 patients (55.7%) were FHC-negative, while 364 (44.3%) were FCH-positive: 289 (35.2%) were FHC-low and 75 (9.1) were FHC-high patients, respectively. Among FHC-positive patients, 270 (32.8%) were lineal line positive and 167 (20.3%) were collateral line positive. 123 patients (14.9%) had diagnosis of MN: 29 (3.5%) synchronous MN and 94 (11.4%) metachronous MN. 108 patients (13.2%) were MN-low, while 15 (1.8%) were MN-high. All patient features are summarized in .
Table 1. Patient features
Among FHC-positive and FHC-negative patients, 61 (16.8%) and 62 (13.5%) had a diagnosis of MN (p = .1987).
Efficacy analysis
Among 822 patients, 775 were evaluable for activity; the other 47 had not yet evaluated the disease at the time of the data cutoff analysis or were lost to follow-up/death without evaluation of clinical response. ORR in the overall population was 34.8% (95% CI: 30.8–39.2, 270 responses). As summarized in , no significant differences were found regarding ORR among subgroups.
Table 2. Activity data for overall population and subgroups
The median follow-up was 15.6 months; in the overall population, median PFS was 9.2 months (95% CI: 8.2–10.6; 479 events) and median OS was 20.5 months (95% CI: 16.2–27.8; 477 censored patients). and report univariate and multivariate analyses of PFS and OS in detail.
Table 3. Univariate and multivariate analyses for PFS
Table 4. Univariate and multivariate analyses for OS
Median PFS in FHC-negative, FHC-low, and FHC-high patients was 9.3 months (95% CI: 7.5–10.6; 277 events), 8.4 months (95% CI: 7–11.4; 166 events), and 20.5 months (95% CI: 8.7–26.4; 36 events), respectively (). As reported in , FHC-high patients had a significantly longer PFS when compared to FHC-negative patients (HR = 0.69 [95% CI: 0.48–0.97], p = .0379); at multivariate analysis, FHC-high was confirmed an independent predictor for PFS (compared to FHC-negative).
Figure 1. Kaplan–Meier survival curves according to FHC. (a) Progression-free survival. FHC-negative: 9.3 months (95% CI: 7.5–10.6; 277 events); FHC-low: 8.4 months (95% CI: 7–11.4; 166 events); FHC-high: 20.5 months (95% CI: 8.7–26.4; 36 events). (b) Overall survival. FHC-negative: 18.2 months (95% CI: 14.9–23.9; 250 censored patients); FHC-low: 20.8 months (95% CI: 15.4–20.9; 176 censored patients); FHC-high: 31.6 months (95% CI: 26.2–31.6; 51 censored patients)
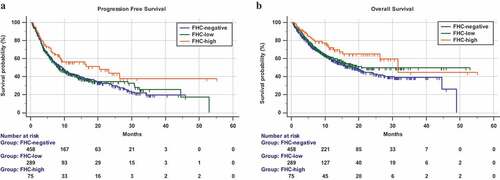
Median OS in FHC-negative, FHC-low, and FHC-high patients was 18.2 months (95% CI: 14.9–23.9; 250 censored patients), 20.8 months (95% CI: 15.4–20.9; 176 censored patients), and 31.6 months (95% CI: 26.2–31.6; 51 censored patients), respectively (). As reported in , FHC-high patients had a significantly longer OS when compared to FHC-negative patients (HR = 0.61 [95% CI: 0.39–0.93], p = .0210); at multivariate analysis, FHC-high was confirmed an independent predictor for OS (compared to FHC-negative).
Median PFS in MN-negative, MN-low, and MN-high patients was 8.7 months (95% CI: 7.6–10.2; 414 events), 12.3 months (95% CI: 8.3–28.9; 58 events), and 14.4 months (95% CI: 3.6–14.5; 7 events), respectively (). As reported in , no significant differences were found regarding PFS, according to MN categories.
Figure 2. Kaplan–Meier survival curves according to MN. (a) Progression-free survival. MN-negative: 8.7 months (95% CI: 7.6–10.2; 414 events); MN-low: 12.3 months (95% CI: 8.3–28.9; 58 events); MN-high: 14.4 months (95% CI: 3.6–14.5; 7 events). (b) Overall survival. MN-negative: 20.5 months (95% CI: 15.7–27.1; 43 censored patients); MN-low: 26.2 months (95% CI: 18.7–48.9; 66 censored patients); MN-high: 15.9 months (95% CI: 10.5–15.9; 8 censored patients)
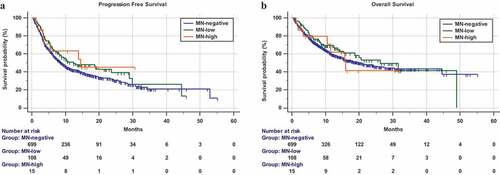
Median OS in MN-negative, MN-low, and MN-high patients was 20.5 months (95% : 15.7–27.1; 43 censored patients), 26.2 months (95% CI: 18.7–48.9; 66 censored patients), and 15.9 months (95% CI: 10.5–15.9; 8 censored patients), respectively (). As reported in , no significant differences were found regarding OS, according to MN categories.
Immune-related adverse events
In the overall population, 329 patients experienced any grade immune-related adverse events (irAEs) (40%). summarizes the univariate and multivariate analysis of irAEs of any grade. Overall, FHC-positive patients had a significantly higher incidence of irAEs of any grade (p = .0132) compared to FHC-negative patients; this also occurs when considering lineal line exclusively (p = .0015), but not when considering collateral line exclusively (p = .1491). FHC-high patients had a significantly higher incidence of irAEs of any grade, compared to FHC-negative patients (p = .0012), while FHC-low did not (p = .1240). FHC overall (positive vs negative) and FHC-high (vs negative) were confirmed as independent predictors for higher incidence of irAEs of any grade at the multivariate analysis.
Table 5. Univariate and multivariate analysis for incidence of irAEs of any grade
Discussion
It is well known that a small percentage (5 – 10%) of cancers are related to inherited mutations, which usually occurs with typical familial patterns.Citation11 Syndromes of inherited cancer predisposition are also one of the underlying mechanisms of MN development.Citation9 In our population, 44.3% and 14.9% of the patients had a positive FHC and diagnosis of MN, respectively; these findings are quite aligned to what was previously reported among cancer patients.Citation9,Citation15,Citation16
In the preliminary analysis of the FAMI-L1 study, including the first 211 patients, FHC-positive patients had significantly higher ORR/DCR and significantly longer time to treatment failure and OS, when compared to FHC-negative patients.Citation13 No significant association was found between diagnosis of MN (all metachronous tumors) and clinical outcomes, with the exception of a higher DCR compared to MN-negative patients.Citation13 In this update, no significant associations were found between FHC, MN, and ORR; however from a speculative point of view, looking at the ORRs for FHC-negative, FHC-low, and FHC-high (32.7%, 36.7%, and 40.3%, respectively), we can notice that there is a trend to a direct proportionality, between the number of the positive familial lines and the ORR. Moreover, we can now confirm that MN does not affect PFS and OS, even considering the different analyses according to “burden of MN” and to synchronous/metachronous diagnosis of MN. Interestingly, only FHC-high patients had a significantly longer PFS and OS, when compared to FHC-negative patients, while no significant differences were found between FHC-low and FHC-negative, nor between FHC-positive and FHC-negative patients (analyzed overall, for lineal line only and for collateral line only, see and ). The aim of the preliminary analysis was exploratory and purely descriptive. We did not compute the sample size nor performed subgroup analyses according to the “FHC burden.” In our opinion, the present results are more reliable, thanks to the bigger sample size and to the more appropriate analysis.
Although our preliminary results seem now mitigated,Citation13 this update seems to confirm our hypothesis that there is at least an association between the “FHC burden” and immunotherapy clinical outcomes, as if the more positive family lines, the greater the benefits. Looking at the hazard ratios, it is noticeable that they are concordantly higher in each comparison between FHC-high and FHC-negative patients than in those between FHC-low and FHC-negative. Intriguingly, adding the irAE analysis, we found a significantly higher incidence of any grade irAEs among FHC-positive patients (overall and for lineal line only) when compared to FHC-negative patients. Moreover, FHC-high patients had a significantly higher incidence of irAEs of any grade, when compared to FHC-negative patients, while FHC-low patients did not. It is also noticeable that the highest incidence of irAEs of any grade was reported among FHC-high patients (56%). In light of the emerging association between the development of irAEs and improved clinical outcomes with ICIs across different tumor types,Citation17–Citation20 these findings would bear our hypothesis.
As previously stated, a history of MN is one of the clinical hallmarks of inherited cancer susceptibility, just as a positive FHC. Despite that, in our population, FHC and diagnosis of MN are not significantly related, and this is reflected in the different correlations that they have with clinical outcomes. Nevertheless, it is noticeable that patients with metachronous MN and MN-high ones had the highest ORRs (43.8% and 41.5%, respectively, see ). Moreover, MN-high patients had at the same time the longest PFS and the shortest OS (compared to MN-negative and MN-low). We can thus speculate that a history of MN may underlie a kind of “immune sensitiveness,” demonstrated by good ORR and PFS to treatment, which is, however, outclassed by the prognostic weight that further malignancies have. We could assume that underlying mechanisms of MN and FHC are the same and lead to the same “immune sensitiveness,” but, on the other hand, patients developing MN surely have some negative prognostic features compared to FHC-positive patients.
The possible relationships between somatic alterations of genes belonging to DNA repair systems (such as homologous recombination, MMR, nucleotide excision repair, cell cycle checkpoints, Fanconi anemia DNA repair pathway, and others), “immune-sensitiveness,” and ICI clinical outcomes have been already explored.Citation21,Citation22 Teo et al. reported a significant association between better clinical outcomes and somatic DDR gene alterations in a cohort of advanced urothelial cancer patients treated with atezolizumab.Citation23 Importantly, a higher response rate was found not only in patients whose tumors harbored known or likely deleterious DDR gene alterations but also in patients with DDR alterations of unknown significance when compared to patients whose tumors were wild-type for DDR genes.Citation23 In a study of single-agent pembrolizumab in docetaxel-refractory metastatic castration-resistant prostate cancer patients (mCRP), those with somatic mutations in BRCA1/2 or ATM (ataxia telangiectasia mutated) had higher response rates.Citation24
That being said, if we are demonstrating that there is a proportional relationship between better clinical outcomes with anti-PD-1/PD-L1 inhibitors and “burden of familiarity,” we are allowed to think that DDR gene alterations (even of unknown clinical significance) might represent the underlying mechanism, which would make the cancer more “immune-sensitive,” maybe throughout an increased production of neo-antigens. However, assuming that FHC is a surrogate of DDR gene alterations, such alterations should not be found exclusively with somatic assays (on the tumor specimen), but also with germline assays. In a recent study of mCRP patients, treated with Durvalumab (an anti-PD-L1 checkpoint inhibitor) and olaparib, patients harboring somatic DDR gene alterations were more likely to benefit from the treatment.Citation25 Interestingly, four out of nine responders harbored germline alterations in DDR genes: one had a known deleterious mutation in NBN (nibrin) and 3 had frameshift BRCA2 indels.Citation25 We must, however, recognize that prostate cancer might be associated with specific syndromes of inherited cancer susceptibility;Citation26 thus it does not represent the most appropriate model to be extended to all other cancers. Nevertheless, it is conceivable that in case of a nonspecific high “burden of familiarity,” even without a peculiar familial pattern of cancers (as in the LS and HBOC syndrome), germline DDR gene alterations might be the substrate which explains the better outcomes with immunotherapy.
Among the limitations of the present study, we must cite the retrospective design, which exposes to selection biases, and the lack of centralized data review (imaging and toxicities). Our cohort was made of patients who received anti-PD-1/PD-L1 as different treatment lines; thus, we are not able to balance the expected immunosuppression induced by previous treatments. Even if the discussion about LS and HBOC syndrome was only a presupposition for our study, which “generated the hypothesis,” we must recognize that our patients were not affected by breast/ovarian cancers nor by colorectal cancer. Moreover, we do not have sufficient data for a proper counseling (e.g., age at diagnosis and type/number of malignancies among the relatives), nor regarding inherited cancer predisposition syndrome diagnosis and DDR gene alteration (including germline BRCA mutations or LS diagnosis).
Collecting family history is one of the first steps in filling each patient medical record. Even though the role of this information is often underestimated, it should be taken into consideration to properly evaluate the development risk of a wide range of diseases, including cancer.Citation27,Citation28 We are a long way from saying that FHC could be used as a selection method for anti-PD-1/PD-L1 treatments. However, our study gives rise to interesting insights, which we intend to validate prospectively.
Conclusion
Thanks to the great sample size, this update confirms our preliminary findings. Particularly, FHC-high patients seem to benefit more than FHC-negative patients from PD-1/PD-L1 checkpoint inhibitors, suggesting that FHC might be the surrogate of some biological features related to the immune-sensitiveness. However, further investigations on the topic are still required.
Materials and methods
Patient eligibility
This multicenter retrospective observational study evaluated advanced cancer patients consecutively treated with single-agent anti-PD-1/PD-L1 immunotherapy from April 2015 to July 2018, regardless of the treatment line, at 17 Italian institutions (Supplementary file 1). Patients were eligible if they had histologically confirmed diagnosis of measurable stage IV cancer, with availability of records about FHC and history of eventual metachronous or synchronous MN. All patients provided written informed consent to the treatment with immunotherapy.
Study design
The primary endpoint of this analysis was to confirm the correlations between FHC and clinical outcomes; the secondary endpoint was to further investigate the relationships between diagnosis of MN and clinical outcomes. ORR, progression-free survival (PFS), OS, and incidence of any grade irAEs were evaluated. Patients were assessed with radiological imaging every 8–12 weeks using the RECIST (v. 1.0) criteriaCitation29 according to the local clinical practice and national guidelines required by the Agenzia Italiana del Farmaco (AIFA). ORR was defined as the portion of patients experiencing an objective response (complete or partial response) as best response to immunotherapy. PFS was defined as the time from ICI treatment’s start to disease progression or death whichever occurred first; OS as the time from the beginning of treatment to death. For PFS as well as for OS, patients without events were considered as censored at the time of the last follow-up.
On the basis of our previous results,Citation13 and what was reported in other studies,Citation15,Citation16,Citation30 we hypothesized that 48% of the evaluated patients were FHC-positive, and 52% were FHC-negative. With a probability of Type I error of 0.05 and of Type II error of 0.20 and assuming a possible survival benefit for FHC-positive patients with a reduction of the risk of death by 70%, 247 total events were necessary and at least 712 patients had to be included. Univariate and multivariate analyses were performed using the following covariates: age (<70 vs ≥70 years old),Citation31–Citation34 sex (male vs. female), primary tumor (NSCLC, melanoma, renal cell carcinoma, and others), Eastern Cooperative Oncology Group Performance Status (ECOG-PS) (0–1 vs ≥2), number of metastatic sites (≤2 vs >2), and treatment line (first vs nonfirst). χ2 test was used to correlate ORR and incidence of any grade irAEs with patient features.Citation35 χ2 test was also used to evaluate the correlation between FHC (yes vs no) and diagnosis of MN (yes vs no). Logistic regression was used for the multivariate analysis of ORR and incidence of irAEs of any grade.Citation36 Median PFS and median OS were evaluated using the Kaplan–Meier method.Citation37 The median period of follow-up was computed according to the reverse Kaplan–Meier method.Citation38 Cox proportional hazards modelCitation39 was used to evaluate predictor variables in univariate and multivariate analysis for median PFS and median OS. Data cutoff period was October 2018. All statistical analyses were performed using MedCalc Statistical Software version 18.11.3 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2019).
Definition of FHC and MNs
Given the lack of data availability in medical records, we did not use the traditional designations of first and second degree of relatedness for family history. Family history was collected in lineal (descendants or ascendants) and collateral lines (not-descentants/ascendants) till the second degree of relatedness (grandparents for lineal line and brothers/sisters for the collateral line). FHC was defined as “positive” with at least one diagnosis of cancer among the considered relatives. Patients were also categorized according to their FHC as follows: FHC-high (in case of cancer diagnoses in both the lineal and collateral family lines), FHC-low (in case of cancer diagnoses in only one family lines, lineal or collateral), and FHC-negative. Diagnosis of metachronous and/or synchronous MN was defined according to the international association of cancer registry (IARC/IACR) rules.Citation40 Patients were also categorized according to the diagnosis of MN as follows: MN-high (in case of more than two cancer diagnoses in their medical history), MN-low (in case of two cancer diagnoses in their medical history), and MN-negative. A further analysis was performed categorizing patients into synchronous MN, metachronous MN, and MN-negative.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Ethics approval and consent to participate
All patients provided written informed consent to treatment with immunotherapy. All patients alive at the time of data collection provided an informed consent for the present retrospective analysis. The procedures followed were in accordance with the precepts of Good Clinical Practice and the declaration of Helsinki. The study was approved by the respective local ethical committees on human experimentation of each institution, after previous approval by the coordinating center (University of L’Aquila, Internal Review Board protocol number 32865, approved on July 24, 2018).
Authors contributions
All authors contributed to the publication according to the ICMJE guidelines for the authorship as follows:
Study conception and design: AC, PAA, CF, SB, MT, MB.
Acquisition of data: AC, RG, FP, PDM, NT, MDT, AG, KC, AT, FZ, EV, FM, MR, CA, TZ, MF, PM, AB, GCAC, FDG, MGV, FR, RRS, AP, SR, MT, MRM, AG, MAO, FM, AI, SG, SB, CZ, CM, AP, GP, DM, MCF.
Analysis and interpretation of data: AC, SB MB, PAA, CF.
Drafting of manuscript: PAA, CF, SB, MB, RB, DS.
Critical revision: PAA, CF, MT, RB, DS, MCF.
All authors read and approved the submitted version of the manuscript (and any substantially modified version that involves the author’s contribution to the study). Each author has agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Availability of data and materials
The datasets used during the present study are available from the corresponding author upon reasonable request.
Conflicts of interest
Dr Alessio Cortellini received grants as speaker by MSD, Astra-Zeneca and Boehringer Ingelheim, grant consultancies by BMS, Roche, Novartis, Istituto Gentili, and Ipsen; Dr Marcello Tiseo received grant as speaker and advisory role by Astra-Zeneca, Pfizer, Eli-Lilly, BMS, Novartis, Roche, MSD, Boehringer Ingelheim, Otsuka, Pierre Fabre; Dr Maria Giuseppa Vitale received travel grants and speaker fees by BMS, Ipsen Astellas, Janssen, Novartis, and Pfizer; Dr Sebastiano Buti received grants as speaker and advisory role by BMS, Pfizer, MSD, Ipsen, Novartis, Astra-Zeneca, and research funding from Novartis; Dr. Melissa Bersanelli received honoraria as speaker at scientific events and as consultant for advisory role by BMS, Novartis, and Pfizer and research funding by Seqirus; Dr Paolo A. Ascierto has/had a consultant/advisory role for Bristol Myers-Squibb, Roche-Genentech, Merck Sharp & Dohme, Array, Novartis, Merck Serono, Pierre Fabre, Incyte, NewLink Genetics, Genmab, Medimmune, AstraZeneca, Syndax, SunPharma, Sanofi, Idera, Ultimovacs, Sandoz, Immunocore, he also received research funds from Bristol Myers-Squibb, Roche-Genentech, Array, and travel support from MSD.
Supplemental Material
Download ()Acknowledgments
This work was supported by the Consorzio Interuniversitario Nazionale per la Bio-Oncologia (CINBO).
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
References
- Taube JM, Klein A, Brahmer JR, Xu H, Pan X, Kim JH, Chen L, Pardoll DM, Topalian SL, Anders RA, et al. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clin Cancer Res. 2014;20(19):5064–10. doi:10.1158/1078-0432.CCR-13-3271.
- Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, Lee W, Yuan J, Wong P, Ho TS. Mutational landscape determines sensitivity to PD-1 blockade in non–small cell lung cancer. Science. 2015;348(6230):124–128. doi:10.1126/science.aaa1348.
- Hellmann MD, Ciuleanu T-E, Pluzanski A, Lee JS, Otterson GA, Audigier-Valette C, Minenza E, Linardou H, Burgers S, Salman P, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med. 2018 May 31;378(22):2093–2104. doi:10.1056/NEJMoa1801946. Epub 2018 Apr 16.
- Cortellini A, Bersanelli M, Buti S, Cannita K, Santini D, Perrone F, Giusti R, Tiseo M, Michiara M, Di Marino P, et al. A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: when overweight becomes favorable. J Immuno Ther Cancer. 2019 Feb 27;7(1):57. doi:10.1186/s40425-019-0527-y.
- Routy B, Le Chatelier E, Derosa L, Duong CPM, Alou MT, Daillère R, Fluckiger A, Messaoudene M, Rauber C, Roberti MP, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science. 2018 Jan 5;359(6371):91–97. doi:10.1126/science.aan3706.
- Le DT, Uram JN, Wang H, Bartlett BR, Kemberling H, Eyring AD, Skora AD, Luber BS, Azad NS, Laheru D, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372:2509–2520. doi:10.1056/NEJMoa1500596.
- Viale G, Trapani D, Curigliano G. Mismatch repair deficiency as a predictive biomarker for immunotherapy efficacy. Biomed Res Int. 2017;4719194:2017.
- Dai Y, Sun C, Feng Y, Sun C, Jia Q, Zhu B. Potent immunogenicity in BRCA1-mutated patients with high-grade serous ovarian carcinoma. J Cell Mol Med. 2018 May 31;22:3979–3986. doi:10.1111/jcmm.13678. [Epub ahead of print].
- Vogt A, Schmid S, Heinimann K, Frick H, Herrmann C, Cerny T, Omlin A. Multiple primary tumours: challenges and approaches, a review. ESMO Open. 2017 May 2;2(2):e000172. doi:10.1136/esmoopen-2017-000172. eCollection 2017.
- Strickland KC, Howitt BE, Shukla SA, Rodig S, Ritterhouse LL, Liu JF, Garber JE, Chowdhury D, Wu CJ, D’Andrea AD, et al. Association and prognostic significance of BRCA1/2-mutation status with neoantigen load, number of tumor-infiltrating lymphocytes and expression of PD-1/PD-L1 in high grade serous ovarian cancer. Oncotarget. 2016;7(12):13587–13598. doi:10.18632/oncotarget.v7i12.
- Pembrolizumab in advanced BRCA-mutated breast cancer. Identifier: NCT03025035. [ accessed 2019 Mar 9]. https://clinicaltrials.gov/ct2/show/NCT03025035.
- Garber JE, Offit K. Hereditary cancer predisposition syndromes. J Clin Oncol. 2005 Jan 10;23(2):276–292. doi:10.1200/JCO.2005.10.042.
- Cortellini A, Bersanelli M, Buti S, Gambale E, Atzori F, Zoratto F, Parisi A, Brocco D, Pireddu A, Cannita K et al. Family history of cancer as surrogate predictor for immunotherapy with anti-PD1/PD-L1 agents: preliminary report of the FAMI-L1 study. Immunotherapy. 2018 Jun;10(8):643–655. doi:10.2217/imt-2017-0167.
- Cortellini A, Bersanelli M, Ficorella C, Buti S. Family history of cancer and DNA damage response genes: two sides of the same coin? Thorac Cancer. 2019 Feb;10(2):401. doi:10.1111/1759-7714.12926.
- Ogawa H, Kato I, Tominaga S. Family history of cancer among cancer patients. Jpn J Cancer Res GANN. 1985;76:113–118.
- Gaughan EM, Cryer SK, Yeap BY, Jackman DM, Costa DB. Family history of lung cancer in never smokers with non-small-cell lung cancer and its association with tumors harboring EGFR mutations. Lung Cancer. 2013 Mar;79(3):193–197. doi:10.1016/j.lungcan.2012.12.002. Epub 2012 Dec 27.
- Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber JS. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2016 Feb 15;22(4):886–894. doi:10.1158/1078-0432.CCR-15-1136.
- Haratani K, Hayashi H, Chiba Y, Kudo K, Yonesaka K, Kato R, Kaneda H, Hasegawa Y, Tanaka K, Takeda M, et al. Association of immune-related adverse events with nivolumab efficacy in non-small-cell lung cancer. JAMA Oncol. 2018 Mar 1;4(3):374–378. doi:10.1001/jamaoncol.2017.2925.
- Teraoka S, Fujimoto D, Morimoto T, Kawachi H, Ito M, Sato Y, Nagata K, Nakagawa A, Otsuka K, Uehara K, et al. Early immune-related adverse events and association with outcome in advanced non-small cell lung cancer patients treated with nivolumab: a prospective cohort study. J Thorac Oncol. 2017 Dec;12(12):1798–1805. doi:10.1016/j.jtho.2017.08.022. Epub 2017 Sep 20.
- Cortellini A, Chiari R, Ricciuti B, Metro G, Perrone F, Tiseo M, Bersanelli M, Bordi P, Santini D, Giusti R. Correlations between the immune-related adverse events spectrum and efficacy of anti-PD1 immunotherapy in NSCLC patients. Clin Lung Cancer. 2019 Feb 21:pii: S1525-7304(19)30025–7. doi:10.1016/j.cllc.2019.02.006. [Epub ahead of print].
- Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, Lee W, Yuan J, Wong P, Ho TS, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015 Apr 3;348(6230):124–128. doi:10.1126/science.aaa1348. Epub 2015 Mar 12.
- Wang Z, Zhao J, Wang G, Zhang F, Zhang Z, Zhang F, Zhang Y, Dong H, Zhao X, Duan J, et al. Comutations in DNA damage response pathways serve as potential biomarkers for immune checkpoint blockade. Cancer Res. 2018 Nov 15;78(22):6486–6496. doi:10.1158/0008-5472.CAN-18-1814. Epub 2018 Aug 31.
- Teo MY, Seier K, Ostrovnaya I, Regazzi AM, Kania BE, Moran MM, Cipolla CK, Bluth MJ, Chaim J, Al-Ahmadie H, et al. Alterations in DNA damage response and repair genes as potential marker of clinical benefit from PD-1/PD-L1 blockade in advanced urothelial cancers. J Clin Oncol. 2018 Jun 10;36(17):1685–1694. doi:10.1200/JCO.2017.75.7740. Epub 2018 Feb 28.
- De Bono J, Goh J, Ojamaa K, Piulats Rodriguez JM, Drake CG, Hoimes CJ, Wu H, Poehlein CH, Antonarakis ES. KEYNOTE-199: pembrolizumab (pembro) for docetaxel-refractory metastatic castration-resistant prostate cancer (mCRPC). J Clin Oncol. 2018;36(suppl):abstr5007. doi:10.1200/JCO.2018.36.15_suppl.5007.
- Karzai F, VanderWeele D, Madan RA, Owens H, Cordes LM, Hankin A, Couvillon A, Nichols E, Bilusic M, Beshiri ML, et al. Activity of durvalumab plus olaparib in metastatic castration-resistant prostate cancer in men with and without DNA damage repair mutations. J Immuno Ther Cancer. 2018 Dec 4;6(1):141. doi:10.1186/s40425-018-0463-2.
- Wang G, Zhao D, Spring DJ, DePinho RA. Genetics and biology of prostate cancer. Genes Dev. 2018 Sep 1;32(17–18):1105–1140. doi:10.1101/gad.315739.118.
- Walter FM, Emery J. ‘Coming down the line’– patients’ understanding of their family history of common chronic disease. Ann Fam Med. 2005 Sep-Oct;3(5):405–414. doi:10.1370/afm.368.
- Nathan PA, Johnson O, Clamp S, Wyatt JC. Time to rethink the capture and use of family history in primary care. Br J Gen Pract. 2016 Dec;66(653):627–628. doi:10.3399/bjgp16X688273.
- Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–247. doi:10.1016/j.ejca.2008.10.026.
- Song JL, Chen C, Yuan JP, Li -J-J, Sun S-R. Family history of cancer other than breast or ovarian cancer in first-degree relatives is associated with poor breast cancer prognosis. Breast. 2017 Apr;32:130–134. doi:10.1016/j.breast.2017.01.016. Epub 2017 Feb 5.
- Minana B, Cozar JM, Palou J, Unda Urzaiz M, Medina-Lopez RA, Subirá Ríos J, de la Rosa-kehrmann F, Chantada-Abal V, Lozano F, Ribal MJ, et al. Bladder cancer in Spain 2011: population-based study. J Urol. 2014 Feb;191(2):323–328. doi:10.1016/j.juro.2013.08.049.
- Ciocan D, Barbe C, Aubin F, Granel-Brocard F, Lipsker D, Velten M, Dalac S, Truchetet F, Michel C, Mitschler A, et al. Distinctive features of melanoma and its management in elderly patients: a population-based study in France. JAMA Dermatol. 2013 Oct;149(10):1150–1157. doi:10.1001/jamadermatol.2013.706.
- Gridelli C, Balducci L, Ciardiello F, Di Maio M, Felip E, Langer C, Lilenbaum RC, Perrone F, Senan S, de Marinis F, et al. Treatment of elderly patients with non-small-cell lung cancer: results of an international expert panel meeting of the italian association of thoracic oncology. Clin Lung Cancer. 2015 Sep;16(5):325–333. doi:10.1016/j.cllc.2015.02.006.
- Azawi NH, Joergensen SM, Jensen NV, Clark PE, Lund L. Trends in kidney cancer among the elderly in Denmark, 1980–2012. Acta Oncol. 2016;55(Suppl 1):79–84. doi:10.3109/0284186X.2015.1115121.
- Mantel N. Chi-square tests with one degree of freedom: extensions of the Mendel-Haenszel procedure. J Am Stat Assoc. 1963;58:690–700.
- Hosmer DW Jr, Lemeshow S. Sturdivant RX applied logistic regression. Third ed. New Jersey: John Wiley & Sons; 2013.
- Kaplan EL, Meier P. Nonparametric estimation of incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi:10.1080/01621459.1958.10501452.
- Schemper M, Smith TL. A note on quantifying follow-up in studies of failure time. Control Clin Trials. 1997;17:343–346. doi:10.1016/0197-2456(96)00075-X.
- Cox DR. Regression models and life tables (with discussion). J R Stat Soc Ser B. 1972;74:187–200.
- International rules for multiple primary cancers ICD-O third edition. Internal Report No.2004/02. Lyon: International Agency for Research on Cancer. IARC (2004).
