ABSTRACT
The anti-Ly6G antibody is used to deplete Ly6Gpos neutrophils and study their role in diverse pathologies. However, depletion is never absolute, as Ly6Glow neutrophils resistant to depletion rapidly emerge. Studying the functionality of these residual neutrophils is necessary to interpret anti-Ly6G-based experimental designs. In vitro, we found anti-Ly6G binding induced Ly6G internalization, surface Ly6G paucity, and primed the oxidative burst of neutrophils upon TNF α co-stimulation. In vivo, we found neutrophils resistant to anti-Ly6G depletion exhibited anti-neutrophil-cytoplasmic-antibodies. In the pre-clinical KrasLox-STOP-Lox-G12D/WT; Trp53Flox/Flox mouse lung tumor model, abnormal neutrophil accumulation and aging was accompanied with an N2-like SiglecFpos polarization and ly6g downregulation. Consequently, SiglecFpos neutrophils exposed to anti-Ly6G reverted to Ly6Glow and were resistant to depletion. Noting that anti-Ly6G mediated neutrophil depletion alone had no anti-tumor effect, we found a long-lasting rate of tumor regression (50%) by combining anti-Ly6G with radiation-therapy, in this model reputed to be refractory to standard anticancer therapies. Mechanistically, anti-Ly6G regulated neutrophil aging while radiation-therapy enhanced the homing of anti-Ly6G-boundSiglecFneg neutrophils to tumors. This anti-tumor effect was recapitulated by G-CSF administration prior to RT and abrogated with an anti-TNFα antibody co-administration. In summary, we report that incomplete depletion of neutrophils using targeted antibodies can intrinsically promote their oxidative activity. This effect depends on antigen/antibody trafficking and can be harnessed locally using select delivery of radiation-therapy to impair tumor progression. This underutilized aspect of immune physiology may be adapted to expand the scope of neutrophil-related research.
Introduction
The anti-Ly6G antibody (ab) has been widely used to deplete neutrophils and investigate their role in malignancies.Citation1–6 However, this strategy suffers limitations: the depletion efficacy of anti-Ly6G is partial, transient, and neutrophil numbers rebound as soon as 3 d after treatment initiation.Citation7 The mechanism involved in this rebound or resistance to depletion is unclear, but seems independent from schedule of treatmentCitation7 or from the occurrence of abs against the anti-Ly6G ab.Citation7 Enhanced granulopoiesis was further proposed as a depletion resistance mechanism, but the transient efficacy of anti-Ly6G has also been shown in granulocyte colony-stimulating factor (G-CSF)-driven models, Citation5 suggesting that resistance could be dependent upon an adaptative process. Recently, we reported that neutrophils silence ly6g under physiological condition as they exit from the bone marrow (BM) and that neutrophils resistant to anti-Ly6G depletion had low surface expression of Ly6G .Citation8
In cancer studies, partial or transient neutrophil depletion complicates the interpretation of results, as cancer models require several weeks of antibody-treatment and follow-up.Citation9 The biological significance of residual and anti-Ly6G bound neutrophils has not been investigated. However, clinical pathologies, such as transfusion-related acute lung injury, Citation10 and granulomatosis polyangiitis ;Citation11 where antibodies targeting the membrane of neutrophils and anti-neutrophil cytoplasmic antibodies (ANCAs) are, respectively, found; suggest that antibody-targeted neutrophils can be harmful, especially to lung tissues. Whether this latter feature might be used to enhance the efficacy of anti-cancer treatment has not been envisaged previously.
Neutrophilia after radiation therapy (RT) translates to poor clinical outcome.Citation1,Citation12–15 These correlative studies are mostly based on blood neutrophil analysis, but the physiology of tumor-associated-neutrophils (TANs) after RT requires further investigation. The KrasLox-STOP-Lox-G12D/WT; Trp53Flox/Flox (KP) non-small-cell lung cancer (NSCLC) model mimics the natural course of human adenocarcinoma.Citation16 KP-tumor infiltrating myeloid cells, including TANs, are conserved across individuals and mouse/human species, Citation17 according to a single-cell RNAseq analysis publically available.Citation17 High KP-TAN prevalence was shown to correlate with KP-tumor progression.Citation2 Treatment with the anti-Gr1 ab, which recognizes both Ly6C and Ly6G antigens (ags), reduced KP-TAN prevalence by 70%, slowed KP-tumor growth but did not induce tumor regression.Citation2,Citation3 A N2-like subset of SiglecFpos TANs with a tumor-associated transcriptomic profile has recently been described and shown to arise from a tumor-induced specific ontogeny.Citation3,Citation18 Additionally, TANs transiently dominated the microenvironment of KP-tumors after RT.Citation19 KP-tumors have been shown to be refractory to various anti-cancer treatment including RT; whole thorax irradiation (WTI) with a single dose of 15.5GyCitation20 and single-nodule stereotactic irradiation at 2 × 8.5GyCitation21 comparably slowed KP-tumor growth down, but did not induce any tumor regression. In KPs, several tumors arise asynchronously and their immune microenvironment display strong intra-inter individual heterogeneity.Citation2,Citation3,Citation22 Therefore, radiological evaluation has been used in those studies to monitor the growth of single nodules to avoid histological section plan biases.Citation2,Citation3 In a KP-sarcoma model, anti-Ly6G administration prior to RT enhanced its efficacy, but did not result in tumor regression.Citation1
We investigated the intrinsic effect of anti-Ly6G binding on residual neutrophil physiology. Based on our data, we propose that anti-Ly6G/Ly6G internalization along with the presence of ANCA, respectively, act as a resistance mechanism to anti-Ly6G-mediated depletion; and as an intrinsic signal for TNFα-mediated cytotoxic oxydative burst. Using the treatment-resistant KP model, we report that an anti-Ly6G ab exhibits synergy with RT to achieve a 50% partial KP-tumor regression rate in a TNFα-dependent manner, in absence of neutrophil depletion. This novel proposed function of anti-Ly6G ab treatments bring into question previous interpretations of neutrophil depletion (reviewed in 24) and opens some exciting new opportunities to study and manipulate neutrophil function.
Results
Anti-Ly6G ab is rapidly internalized in vitro
We used the imagestream technology to track the anti-Ly6G-PE ab localization after binding. BM neutrophils were incubated in cytochalasin D to block cytoskeleton prior anti-Ly6G staining ()). We observed 4 PE distribution patterns: 1) membrane diffuse; 2) membrane condensation; 3) intra-cellular condensation; 4) diffuse intracellular ()). After 1 hour of binding, 80% of neutrophils showed anti-Ly6G-PE internalization versus 20% of them if cytoskeleton was chemically inhibited ()). PE signal colocalizing with membrane CD45 inversely varied ()). A less sensitive additional methodology, using fluoro-labeled anti-rat antibody to detect the rat anti-Ly6G ab, validated this point (Fig. S1a-f).
Figure 1. Neutrophils resistant to anti-Ly6G depletion exhibit ANCAs
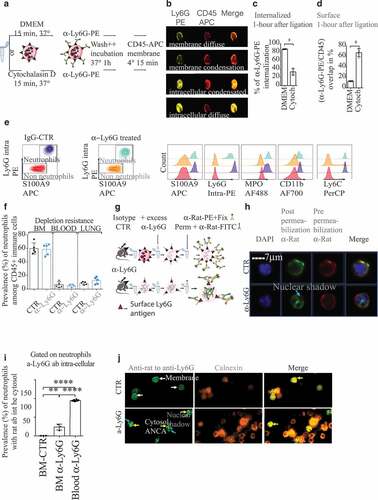
Anti-Ly6G ab generates ANCAs in vivo
We treated mice C57Bl6 mice with anti-Ly6G ab for 5 d and tracked its distribution in vivo. Despite daily treatment with anti-Ly6G, neutrophil prevalence was not affected in BM, blood and lung (). As we previously reported, adult C57Bl6 mice background is refractory to neutrophil depletion as newly synthesized Ly6Glow neutrophils reconstitute the pool of circulating neutrophils as early as 1 d after treatment initiation.Citation8 We then characterized the anti-Ly6G ab localization in the cell with imagestream. In anti-Ly6G treated cells, we found, respectively, 25% and 90% of BM and blood neutrophils exhibiting cytosolic anti-Ly6G ab ()). Additionally, on cytospined BM cells, we observed a colocalization of the in vivo delivered anti-Ly6G ab with calnexin, an endoplasmic reticulum protein. Despite an ethanol fixation, the distribution of the in-vivo delivered anti-Ly6G was cytosolic and not peri-nuclear. We conclude anti-Ly6G generates cytoplasmic-ANCA (c-ANCA) in vivo. Our setting was not adapted to determine whether anti-Ly6G entered the cytosol directly through membrane pores in vivo, or if it leaked from endosomes to the cytosol after internalization.
The Ly6G/anti-Ly6G complex internalization is a depletion resistance mechanism
The expression of Ly6G on the surface of neutrophils increases as they mature.Citation23 Accordingly, the mean fluorescence intensity (MFI) for Gr1 (that recognizes the Ly6G ag despite previous anti-Ly6G binding) in blood neutrophils was higher than in BM ()). However, in anti-Ly6G treated mice, blood neutrophils had a lower Gr1 MFI than BM neutrophils, suggesting an active loss of the Ly6G ag during/after they exit from the BM ()). Moreover, TNF α exposure enhanced Ly6G translocation to the membrane ()) and partially rescued the Gr1 MFI loss in anti-Ly6G treated BM-neutrophils, but not those in blood ()). Since ly6g is downregulated at the RNA level when neutrophils exit from the BM, Citation8 we hypothesized that neutrophils may exhibit lower levels of Ly6G protein on the membrane when internalization exceeds translocation of Ly6G. Since the anti-Gr1 ab also recognizes Ly6C, we confirmed that there were no differences in Ly6C expression ()). Since anti-Ly6G and anti-Gr1 are pauci-competitive (Fig. S2a-g), we implemented our recently published methodCitation8 to stain Ly6G in a specific and sequential manner. This approach confirmed that neutrophils treated with anti-Ly6G were Ly6Glow both at the membrane and intracellular levels (Fig. S2h-k). Control experiments using CD11b, another membrane marker of neutrophil maturation, showed no changes in its level of expression (Fig. S2l.m). In conclusion, anti-Ly6G ab physically triggers depletion resistance via Ly6G internalization that limits its functional recognition ()).
Figure 2. Anti-Ly6G ligation enhances TNFα-induced neutrophil oxidative burst
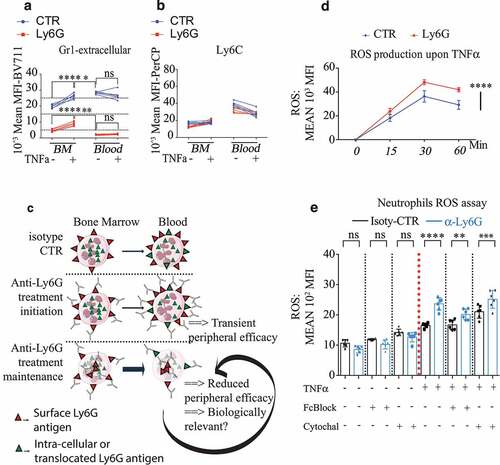
Anti-Ly6G binding potentiates TNF α- mediated oxidative burst
Next, we investigated whether the process of antigen/antibody (Ag/Ab) binding and intracellular trafficking were able to modify neutrophil biology ()). We incubated neutrophils with or without anti-Ly6G for 15 minutes and stimulated them with TNFα. Anti-Ly6G treatment increased reactive oxygen species (ROS) production in both onset and intensity after TNFα stimulation ()). Both Fc-receptor blockade and cytoskeleton inhibition with cytochalasin D limited the relative increase in TNF α-induced ROS ()), suggesting that anti-Ly6G binding and trafficking primes the cytotoxic oxidative function of neutrophils under TNFα stimulation.
In summary, we found anti-Ly6G binding at the neutrophil surface-induced internalization of the Ag/Ab complex causing subsequent resistance to depletion. We also report in the present study that anti-Ly6G produced ANCAs. We characterized the phenotype of the residual neutrophils as Ly6Glow and found a potentiation of their cytotoxic function with an enhanced capacity to produce ROS upon a pro-inflammatory stimulus. With this new information, we sought to validate the relevance of these findings using a KP NSCLC model, where the neutrophil contribution in modulating tumor response has been well documented.
TAN aging in KP mice is associated with SiglecF+ differentiation
First, we characterized TANs in KP tumors with a specific focus on their lifespan and kinetics of infiltration, since we previously reported anti-Ly6G reduces the longevity of neutrophils.Citation8 After a single-injection of BrdU ()), we found that CD11bhigh Ly6Cint Ly6Ghigh F4/80neg SSCalow neutrophils started to infiltrate tumors 60-hours after BrdU incorporation. Following BrdU injection, BrdU+ TANs were detected up to 10 d afterward ()). While 50% of TANs expressed SiglecF ()), none of the young (60-hour) infiltrating neutrophils expressed SiglecF ()). From day 6, the prevalence of BrdU among the SiglecFneg TANs declined while reaching a transient plateau in SiglecFpos TANs. At 10 d after BrdU injection, the rare remaining BrdU+ TANs were exclusively SiglecFpos ()). Additional markers and histological analyses confirmed those results and excluded an eosinophil contamination (Fig. S3). Thus, we conclude that TANs have an aberrantly long lifespan and that they locally differentiate toward N2-like SiglecFpos cells in a time-dependent manner. We next evaluated the effect of anti-Ly6G delivery on these TAN populations.
Figure 3. TAN aging enables SiglecF differentiation and depletion resistant Ly6Gneg neutrophils
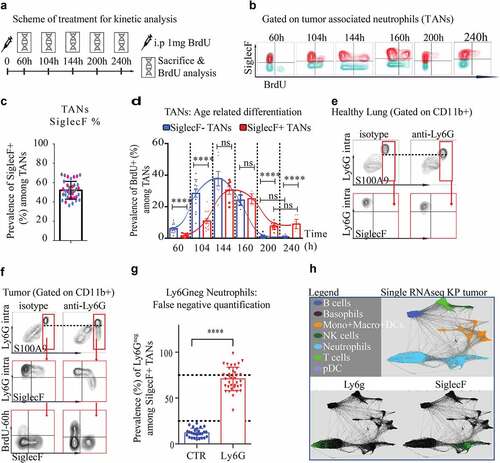
Anti-Ly6G treatment gives rise to Ly6G negative TANs
The occurrence of Ly6G negative MDSCs has been reported after anti-Ly6G treatment (reviewed inCitation24). The existence of these cells is controversial as they were proposed to result from a Ly6G ag masking issue.Citation24 To clarify this point and evaluate the efficacy of neutrophil depletion in KPs, we used intracellular staining for Ly6G to circumvent membrane masking, and S100A9 as an additional neutrophil marker, to investigate this further ()). In untreated KP-TANs, flow cytometry revealed that SiglecFhigh and SiglecFneg TANs had comparable cell surface levels of Ly6G. Additionally, S100A9 was specific and sensitive for identification of TANs and neutrophils ()). Upon anti-Ly6G treatment, intracellular staining for Ly6G resolved any potential confounding effects of ag masking and was sufficient to detect neutrophils in BM, blood, and lung tissues, despite reduced MFI Ly6G signal (). However, the Ly6G ag was lost in SiglecFpos TANs after anti-Ly6G treatment ()), suggesting that 70% of SiglecFpos TANs are no longer detectable with the Ly6G epitope after anti-Ly6G treatment. This loss of Ly6G expression may reflect an uncompensated Ly6G degradation after antibody binding, since SiglecF TANs were reported as ly6g low at the RNA level () adapted from an available online databaseCitation17).
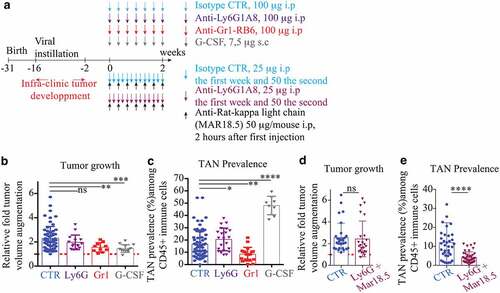
Antibody-mediated TAN depletion is limited and exhibits no anti-tumor effect
We challenged KP mice with three antibody-based neutrophil depletion strategies (Anti-Gr1, Anti-Ly6G, Anti-Ly6G+Mar18.5) and monitored tumor response with unbiased CT-scan imagery. Consistent with previous studies, Citation2,Citation21,Citation25 untreated KP-tumors grew 2.3 fold in 2 weeks (). Anti-Gr1-reduced TAN prevalence and decreased tumor growth by 35% in the absence of regression (). Anti-Ly6G failed to reduce TAN prevalence and did not affect tumor growth (). Anti-Gr1 is less specific than anti-Ly6G, as it recognizes Ly6C, but was more efficient than anti-Ly6G to reduce TAN prevalence (). To discriminate between these two variables, we used a recent strategy involving anti-Ly6G+anti-Rat-Mar18.5 to reduce TAN prevalence comparably to anti-Gr1.Citation8 Despite an incremental improvement in TAN depletion, an anti-tumor effect was not observed () suggesting that reductions in the prevalence of TAN alone does not impede tumor growth. Finally, the anti-tumor effect of anti-Gr1 was recapitulated by G-CSF administration, while TAN prevalence was drastically enhanced (). Altogether, we conclude TAN depletion per se does not impair tumor growth. The common phenotype observed with G-CSF and anti-Gr1 administration suggests that the whole number of TAN is less relevant than their functionality to appreciate the physiology of KP tumors.
Figure 4. Neutrophil depletion alone has no anti-tumor effect
RT partially removes TANs but enhances neutrophil homing into tumors
We then investigated the effect of anti-Ly6G when combined with RT, a standard lung cancer treatment. A single clinically relevantCitation26–28 dose of 11,7 Gy, partially removed TANs, as detected by a BrdU chase (Fig. S4a-d). However, the absolute count of TAN was compensated by day 1.5 as an enhanced recruitment of old CXCR4+ BrdU-60hneg neutrophils (Fig. S4). A reduction of CD62L SiglecFneg TANs was also found after RT (Fig. S4), compatible with enhanced trans-endothelial migration.Citation29,Citation30 Additionally, CD62L SiglecFneg TANs exhibited a higher MFI for CXCR4, Citation23 a marker typically upregulated as neutrophils mature.
RT uncovers the anti-tumor effect of Ly6G-bound residual neutrophils
At the tumor level, RT lowered tumor growth by 50%, but did not elicit tumor regression ()). This result was comparable to various RT treatment schemes published previously,Citation19,Citation21 using either WTI or stereotactic RT to spare the BM. When anti-Ly6G ab was delivered prior to RT, a partial regression rate of 50% was found 1 month after treatment ()). Data confirmed that RT alone enhanced TAN prevalence among CD45 immune cells 1.5 d after treatment, but not their absolute count, as measured with histological myeloperoxidase staining ( and Fig. S5a-d). After day 1.5 of the anti-Ly6G+RT treatment, an enhanced recruitment of neutrophils both in terms of prevalence and absolute numbers was observed ( and Fig. S5a-d). As opposed to RT alone, the anti-Ly6G+RT combination preferentially enhanced the recruitment of young SiglecFneg BrdU-60hpos neutrophils (). This latter result suggests that anti-Ly6G accelerates the recruitment of neutrophils after RT. Furthermore, we observed that radiosensitization with anti-Ly6G was independent from the duration of antibody treatment (Fig. S6a.b). Finally, this effect was partially recapitulated with an adoptive transfer of BM neutrophils pre-incubated with anti-Ly6G, although a lower regression rate was observed in the absence of systemic anti-Ly6G treatment (Fig. S6c.d). Altogether, we conclude that the anti-Ly6G ab intrinsically enhance the anti-tumoral activity of TANs.
Figure 5. Anti-Ly6G enhances the recruitment of young neutrophils and synergizes with RT
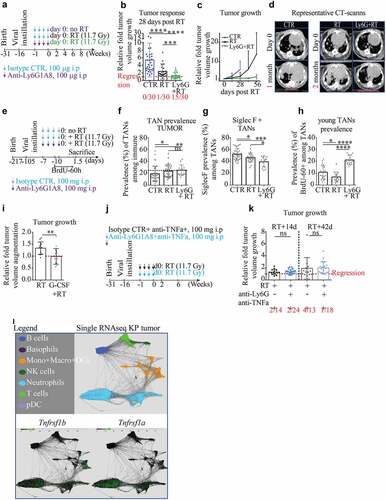
Anti-Ly6G mediated radiosensitization is reversed by anti-TNF α administration
To experimentally validate neutrophils can potentiate RT, we administered a single dose of G-CSF 1-hour prior RT, which recapitulated the efficacy of the anti-Ly6G+RT treatment ()). Given that we found anti-Ly6G bound neutrophils to produce more ROS upon TNFα, together with RNA sequencing data showing that TANs prominently express TNFα receptors, and given that RT leads to the overexpression of TNFα, Citation31 we decided to investigate directly the role of this cytokine (). TNF α inhibition consistently abrogated the radiosensitizing effect of anti-Ly6G treatment, demonstrating that anti-Ly6G synergizes with RT through a TNFα-dependent neutrophil gain-of-function.
Discussion
In the present study, we have reported that anti-Ly6G/Ly6G binding and internalization mediates the resistance of neutrophils to depletion. In mice treated with anti-Ly6G, we highlighted the occurrence of Ly6Glow neutrophils with ANCAs, a diagnostic feature of granulomatosis with polyangiitis. At a mechanistic level, in vitro studies showed anti-Ly6G binding and trafficking potentiated the pro-oxidant activity of neutrophils in response to TNFα. Therefore, while anti-Ly6G is typically used to deplete neutrophils, we investigated whether such a classical strategy actually modified neutrophil biology. In the pre-clinical NSCLC KP-model, we report abnormal neutrophil aging associated with a SiglecF differentiation and a ly6g downregulation. Those cells were prone to depletion resistance. Further, we showed specific reduction of TANs was not sufficient to reduce tumor growth. However, anti-Ly6G administration combined with RT induced a strong and long-lasting tumor regression that was TNF α dependent, while RT alone only slowed tumor growth. Phenotypically, this response was associated with an enhanced homing of anti-Ly6G bound neutrophils to the tumor. Importantly, this acceleration could only be determined on the basis of dynamic measures of newly born neutrophils using BrdU, whereas previous studies generally quantify net yields of neutrophils. Altogether, our data suggest an early anti-tumor effect of neutrophils in the KP tumor model, properties that are gradually lost with aging. This work highlights how anti-neutrophil ab therapy can be harnessed further to unleash increased functionality in the fight against cancer.
In cancer patients, neutrophilia is often associated with poor prognosis, Citation32 which may reflect a multitude of underlying immune-modulated activities. Several approaches are available to modify neutrophil functionCitation33 in efforts to provide mechanistic insight. Genetic neutrophil ablation with Csfr3r knockout mice revealed that TANs impair uterine carcinogenesis by enhancing elimination of hypoxic tumor cells.Citation34 TAN analysis performed with human primary tumor resections showed they were promoting anti-tumor T cell response in early-stage disease.Citation34 In mouse Lewis Lung Carcinoma and the spontaneous mammary MMTV-PyMT+ models, genetic ablation of the neutrophil MET proto-oncogene impaired their recruitment and worsened tumor status.Citation35 In the same PyMT+ model, tail vein infusion of neutrophils reduced the metastatic burden while anti-Ly6G administration increased it.Citation36 However, the role of neutrophils in the PyMT+ model has been challenged several times using distinct approaches dedicated to promoting neutrophil deficiency, including Gcsf-null background, diphtheria toxin-mediated depletion and anti-Ly6G administration. All these approaches have induced an impairment of the metastatic process in the PyMT+ model. In addition, a subset of IL-17-producing γδ T cells were shown to elicit granulopoiesis and neutrophil polarization, leading to CD8 repression and metastasis enhancement.Citation5 Interestingly, γδ T cells were since then shown to have low expression of the antioxidant glutathione and to be highly sensitive to neutrophil-derived ROS.Citation33 Thus, the reported immune-suppressive loop in PyMT may be auto-regulated by neutrophil ROS activation.Citation33 Collectively, these studies highlight the intricacies, if not confounding impact of neutrophils in cancer, an apparent duality that is recapitulated by the TAN1/TAN2 differentiation paradigm.Citation37 Interestingly, our work reports that neutrophil aging enables such differentiation.The temporal progression of the neutrophil response is critical to understand their function during infection and inflammation.Citation38 For instance, upon infection or inflammation, old CXCR4pos neutrophils home fasterCitation39 to the injury site to mitigate threats, while after myocardial lesion, local neutrophil aging results in SiglecF neutrophil differentiation prone to remodeling based on transcriptomic signatures.Citation40 In the present study, we show for the first time that both paradigms are relevant to the physiology of neutrophils after RT.
Under physiological conditions, neutrophils have an intrinsically short lifespan and are produced at a high rate.Citation23 We propose that anti-Ly6G binding and internalization maintain newly synthesized neutrophils under a threshold of Ly6G surface expression that impairs depletion. Regardless, neutrophils under anti-Ly6G pressure retain a shorter lifespan than non-treated neutrophils.Citation8 However, coupled with the enhanced granulopoiesis, a reduced lifespan remains sufficient to rescue neutrophil prevalence. A key finding of our study is that young neutrophils limit tumor growth after RT. Further work is required to clarify the pro-versus anti-tumoral role of older TANs and if/how sequestrated neutrophils may develop an exhausted profile, or passively compete with fresh neutrophil recruitment, thereby losing anti-tumor efficacy.
Some human patients develop anti-neutrophil abs. On one hand, auto-antibodies targeting neutrophil at their surface, such as anti- Human Neutrophil Antigen 1 and 2 (HNA1-2), -CD16/32 and -CD11b are classically associated with primary and secondary auto-immune neutropenia.Citation41 On the other hand, antibodies targeting intracellular proteins or ANCAs, such as anti-MPO/proteinase3 abs, are associated with vasculitis.Citation11 How antibodies enter into the neutrophil cytosol is not well understoodCitation11 and models to study ANCAs-related diseases are scarce.Citation42 Noting that anti-Ly6G treatment did not induce neutropenia but instead generated ANCAs and as given the known severity of ANCA-related disease, the anti-Ly6G may, under specific circumstances, actually activate neutrophil rather than limit their functionality. Furthermore, since Ly6Gneg MDSCs have been described previously, and as given the frequently reported limited depleting efficacy of anti-Ly6G ab; it is likely that the present report showing the sequence: 1) neutrophil aging, 2) anti-Ly6G internalization and 3) depletion resistance, 4) neutrophil gain of function; may apply for other inflammatory/cancer models.Citation24 Finally, given the emerging importance of neutrophil extracellular traps (NETs) in cancerCitation43 and considering ANCA may intrinsically promote the NET formation, Citation44,Citation45 it would be interesting to address either administration of anti-Ly6G recapitulates this physiology and to question the role of NET in this primary lung cancer model, especially in the context of radiation-therapy.
To date, anti-Ly6G has been used to induce neutropenia and mimic neutrophil loss of function. Since neutrophil depletion and neutrophil acute activation are functionally antagonistic, a shift in the interpretation of the results is required where the treatment with anti-Ly6G ab would not induce neutrophil depletion but rather “an enhanced turn-over,” where neutrophils have a shorter lifespan but a higher production incidence. This scenario enables the following: 1) to integrate young neutrophil anti-tumoral properties; 2) to implement ANCA generation and potential intrinsic activator effects of anti-Ly6G binding; 3) to consider undesirable age-related pro-tumoral differentiation. Realization of these potential opportunities may improve clinical outcomes for cancer patients and provides the rationale for advancing the clinical development of non-depleting anti-neutrophil antibodies.
Material and methods
Animal experiments
Animal experiments were approved by the Swiss (VD2920 and 3242) Ethics Committee for Animal Experimentation and performed within institutional guidelines.
Anti-Ly6G/Gr1 treatments
Anti-Ly6G (BP0075-1), anti-Gr1 (BE0075) and corresponding isotype controls (BP0290 and BP0089) were purchased from BioXcell. Antibodies were injected every other day i.p. Doses and schedule are indicated in Fig. S. An alternative approach with anti-Ly6G+anti-rat kappa Mar18.5 described previouslyCitation8 has been additionaly used. For in vitro analysis, BM were collected from untreated C57Bl6 mice and maintained in DMEM. Ex-vivo antibody incubation is performed in 200 µL of PBS with a 10 µg/mL concentration. To avoid cellular interaction, re-incubations at 37° Celsius are performed in 1 mL of PBS under gentle agitation.
Autochthonous mouse model
K-rasLSL-G12D/WT and p53FL/FL mice in a C57BL6/J background purchased from the Jackson Laboratory, bred to obtain K-rasLSL-G12D/WT; p53FL/FL (KP) mice and provided by E.Meylan’s laboratory, (EPFL-Lausanne). KP tumors were initiated upon infection of lung epithelial cells with a lentiviral vector delivering Cre recombinase to activate oncogenic KrasG12D and delete p53 .Citation22 Thirteen to sixteen-week-old mice were infected intratracheally with 3000 Cre-active lentiviral units.
Irradiation and imaging device
X-ray irradiations were performed using an XRad 225Cx (Pxi Precision X-Ray). The dose prescription was determined at 10 mm depth for a 20 × 20 mm2 field according to previous depth dose measurements in a solid water phantom. Irradiations were performed at 225 keV, 13 mA, with a 0.3 mm copper filter and delivered after fluoroscan imaging to position the mice. Whole thorax irradiation was performed with one vertical beam delivering 11.7 Gy in 256 seconds. During the follow-up period, the tumor volume was monitored once every two weeks starting from the fourteenth-week post-lentiviral instillation. Mice were imaged using the X-rad 225CX irradiator under isoflurane anesthesia. Single tumor volumes were assessed after contouring and reconstruction using the Osirix Lite Software. Treatment groups are randomized and tumor contouring is done blindly. As KP tumors have strong intra and inter-individual heterogeneity,Citation2 we chose whole thorax radiation (WTI) to limit the number of animals since KP mice require 30 weeks of housing.
Tissue sampling and analysis
For flow cytometry analysis, single-cell suspension was obtained after tissue macro-dissection, following a procedure described previously.Citation2 A LSRII SORP flow cytometer was used for acquisition. For histological analysis, lungs were gently insufflate with 0.5 mL of 50%PBS-50%OCT (Cell-Path ref 81–0771-00) via the trachea using an I.V surflo catheter (ref SR+OX2225C1). Lobes were separated and OCT-frozen on dry ice. 20 sections of six µm were cut at different depths and then HE stained or stained with appropriated antibodies. Images were obtained with upright microscope Axio Imager.Z1 motorized and analyzed with Zen Zeiss blue software.
G-CSF treatment
Solution of G-CSF was prepared at 250ug/mL of PBS. Mice were subcutaneously injected with 1uL/g daily over 14 d or with a single injection 1 hour prior RT.
BrdU injection and staining procedure
1 mg of BrdU (BD-552598) was injected into mice intra-peritoneally at 10 mg/mL in PBS. BrdU labeling was performed according to the provider’s protocol. Labeled samples were acquired within 48 hours.
Statistical analysis
All results are disclosed in the main text, as mean±SD. Statistical analysis was performed using nonparametric T-test “Mann-Whitney” using Prism 6 software. Statistical significance is indicated as *p < .05, **p < .01, ***p < .001, ****p < .0001, or ns (not significant).
Main findings
Anti-Ly6G binding and internalization renders neutrophils resistant to depletion
Anti-Ly6G binding primes neutrophils to TNF α-induced oxidative burst
In vivo anti-Ly6G administration generates ANCAs
TAN aging enables N2-like SiglecFpos differentiation
Residual anti-Ly6G bound neutrophils synergize with radiation-therapy
Abbreviations
Antibody (ab); antigen (ag); Granulocyte colony-stimulating factor (G-CSF); Tumor-associated neutrophil (TAN) Radiation Therapy (RT); Bone Marrow (BM); Whole thorax radiation (WTI); anti-neutrophil cytoplasmic antibody (ANCA); Non-small cell lung cancer (NSCLC) Mean Fluorescence Intensity (MFI); Reactive oxygen species (ROS).
Competing interests:
The authors have declared that no conflicts of interest exist.
Supplemental Material
Download ()Acknowledgments
Animal Facilities of Epalinges for the animal husbandry; Until Flow cytometry, histology and imaging platforms of UNIL for data acquisition. Pr Limoli C for his kind proofreading of the manuscript.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
Additional information
Funding
References
- Wisdom AJ, Hong CS, Lin AJ, Xiang Y, Cooper DE, Zhang J, Xu ES, Kuo H-C, Mowery YM, Carpenter DJ, et al. Neutrophils promote tumor resistance to radiation therapy. Proc Natl Acad Sci. 2019;116:18584–12.
- Faget J, Groeneveld S, Boivin G, Sankar M, Zangger N, Garcia M, Guex N, Zlobec I, Steiner L, Piersigilli A, et al. Neutrophils and snail orchestrate the establishment of a pro-tumor microenvironment in lung cancer. Cell Rep. 2017;21:3190–3204.
- Engblom C, Pfirschke C, Zilionis R, Da J, Martins S, Bos SA, Courties G, Rickelt S, Severe N, Baryawno N, et al., Osteoblasts remotely supply lung tumors with cancer-promoting SiglecF. Science (2017), doi:10.1126/science.aal5081.
- Szczerba BM, Castro-giner F, Vetter M, Krol I, Gkountela S, Landin J, Scheidmann MC, Donato C, Scherrer R, Singer J, et al. Neutrophils escort circulating tumour cells to enable cell cycle progression. Nature (2019). doi:10.1038/s41586-019-0915-y.
- Coffelt SB, Kersten K, Doornebal CW, Weiden J, Vrijland K, Hau C, Verstegen NJM, Ciampricotti M, Hawinkels LJAC. IL17-producing γδ T cells and neutrophils conspire to promote breast cancer metastasis. Nature. 2015;522:345–348.
- Takeshima T, Pop LM, Laine A, Iyengar P, Vitetta ES, Hannan R. Key role for neutrophils in radiation-induced antitumor immune responses : potentiation with G-CSF. Proc Natl Acad Sci. 2016;1:2–7.
- Stephens-Romero SD, Mednick AJ, Feldmesser M. The pathogenesis of fatal outcome in murine pulmonary aspergillosis depends on the neutrophil depletion strategy. Infect Immun. 2005;73:114–125.
- Boivin G, Faget J, Ancey P-B, Gkasti A, Mussard J, Engblom C, Pfirschke C, Contat C, Pascual J, Vazquez J, et al. Durable and controlled depletion of neutrophils in mice. Nat Commun. 2020;11:2762.
- Vafadarnejad E, Rizzo G, Krampert L, Arampatzi P, Time-resolved single-cell transcriptomics uncovers dynamics of cardiac neutrophil diversity in murine myocardial infarction. (2019).
- Silliman CC, Fung YL, Bradley Ball J, Khan SY. Transfusion-related acute lung injury (TRALI): current concepts and misconceptions. Blood Rev. 2009;23:245–255.
- Hilhorst M, Van Paassen P, Tervaert JWC. Proteinase 3-ANCA vasculitis versus myeloperoxidase- ANCA vasculitis. J Am Soc Nephrol. 2015;26:2314–2327.
- Schernberg A, Nivet A, Dhermain F, Ammari S, Escande A, Pallud J, Louvel G, Deutsch E. Clinical and translational radiation oncology neutrophilia as a biomarker for overall survival in newly diagnosed high-grade glioma patients undergoing chemoradiation. Clin Transl Radiat Oncol. 2018;10:47–52.
- Schernberg A, Nivet A, Dhermain F, Ammari S, Chargari C, Escande A, Pallud J, Louvel G, Deutsch E. Neutrophilia as a biomarker for overall survival in newly diagnosed high-grade glioma patients from chemoradiation. Int J Radiat Oncol. 2017;99:E106.
- Schernberg A, Blanchard P, Chargari C, Ou D, Levy A, Gorphe P, Breuskin I, Atallah S, Caula A, Escande A, et al. Leukocytosis, prognosis biomarker in locally advanced head and neck cancer patients after chemoradiotherapy. Clin Transl Radiat Oncol. 2018;12:8–15.
- Schernberg A, Escande A, Rivin Del Campo E, Ducreux M, Nguyen F, Goere D, Chargari C, Deutsch E. Leukocytosis and neutrophilia predicts outcome in anal cancer. Radiother Oncol. 2017;122:137–145.
- Caswell DR, Chuang C-H, Yang D, Chiou S-H, Cheemalavagu S, Kim-Kiselak C, Connolly A, Winslow MM. Obligate progression precedes lung adenocarcinoma dissemination. Cancer discov. 2015;85:1–27.
- Zilionis R, Engblom C, Pfirschke C, Savova V, Zemmour D, Saatcioglu HD, Krishnan I, Maroni G, Meyerovitz CV, Kerwin CM, et al. Single-cell transcriptomics of human and mouse lung cancers reveals conserved myeloid populations across individuals and species. Immunity. 2019;50:e10.
- Soukup K, Joyce JA. A long-distance relay-tionship between Tumor and Bone. Immunity. 2018;48:13–16.
- Boivin G, Kalambaden P, Faget J, Rusakiewicz S, Montay-Gruel P, Meylan E, Bourhis J, Lesec G, Vozenin M-C. Cellular composition and contribution of tertiary lymphoid structures to tumor immune infiltration and modulation by radiation therapy. Front Oncol. 2018;8:1–13.
- Perez BA, Ghafoori AP, Lee C-L, Johnston SM, Li Y, Moroshek JG, Ma Y, Mukherjee S, Kim Y, Badea CT, et al. Assessing the radiation response of lung cancer with different gene mutations using genetically engineered mice. Front Oncol. 2013;3:72.
- Herter-Sprie GS, Korideck H, Christensen CL, Herter JM, Rhee K, Berbeco RI, Bennett DG. Image-guided radiotherapy platform using single nodule conditional lung cancer mouse models. Nat Commun. 2016;93:292–297.
- DuPage M, Dooley AL, Jacks T. Conditional mouse lung cancer models using adenoviral or lintiviral delivery of Cre recombinase. Nat Protoc. 2009;4:1064–1072.
- Adrover JM, Nicolás-Ávila JA, Hidalgo A. Aging: a temporal dimension for neutrophils. Trends Immunol. 2016;37:334–345.
- Ma C, Greten TF. Editorial: “Invisible” MDSC in tumor-bearing individuals after antibody depletion: fact or fiction? J Leukoc Biol. 2016;99:794.
- Kirsch DG, Grimm J, Guimaraes AR, Wojtkiewicz GR, Perez BA, Santiago PM, Anthony NK, Forbes T, Doppke K, Weissleder R, et al. Imaging primary lung cancers in mice to study radiation biology. Int J Radiat Oncol. 2010;76:973–977.
- Taioli E, Lieberman-Cribbin W, Rosenzweig S, van Gerwen MAG, Liu B, Flores RM. Early stage lung cancer survival after wedge resection and stereotactic body radiation. J Thorac Dis. 2018;10:5702–5713.
- Schonewolf CA, Heskel M, Doucette A, Singhal S, Frick MA, Xanthopoulos EP, Corradetti MN, Friedberg JS, Pechet TT, Christodouleas JP, et al. Five-year long-term outcomes of stereotactic body radiation therapy for operable versus medically inoperable stage i non–small-cell lung cancer: analysis by operability, fractionation regimen, tumor size, and tumor location. Clin Lung Cancer. 2018;20:e63–e71.
- Katz MS, Husain ZA. Stereotactic radiotherapy or surgery for early-stage non-small-cell lung cancer. Lancet Oncol. 2016;17:e41–e42.
- Kishimoto TK, Jutila MA, Butcher EC. Identification of a human peripheral lymph node homing receptor: A rapidly down-regulated adhesion molecule. Proc Natl Acad Sci U S A. 1990;87:2244–2248.
- Filippi MD. Neutrophil transendothelial migration: updates and new perspectives. Blood. 2019;133:2149–2158.
- Sathishkumar S, Dey S, Meigooni AS, Regine WF, Kudrimoti M, Ahmed MM, Mohiuddin M. The impact of TNF-α induction on therapeutic efficacy following high dose spatially fractionated (GRID) radiation. Technol Cancer Res Treat. 2002;1:141–147.
- Wu L, Saxena S, Awaji M, Singh RK. Tumor-associated neutrophils in cancer: going pro. Cancers (Basel). 2019:11. doi:10.3390/CANCERS11040564.
- Mensurado S, Rei M, Lança T, Ioannou M, Gonçalves-Sousa N, Kubo H, Malissen M, Papayannopoulos V, Serre K, Silva-Santos B. Tumor-associated neutrophils suppress pro-tumoral IL-17+ γδ T cells through induction of oxidative stress. PLoS Biol. 2018;16:e2004990.
- Blaisdell A, Crequer A, Columbus D, Daikoku T, Mittal K, Dey SK, Erlebacher A. Neutrophils oppose uterine epithelial carcinogenesis via debridement of hypoxic tumor cells graphical abstract HHS public access. Cancer Cell. 2015;28:785–799.
- Finisguerra V, Di Conza G, Di Matteo M, Serneels J, Costa S, Thompson AAR, Wauters E, Walmsley S, Prenen H, Granot Z, et al. MET is required for the recruitment of anti-tumoural neutrophils. Nature. 2015;522:349–353.
- Granot Z, Henke E, Comen EA, King TA, Norton L, Benezra R. Tumor entrained neutrophils inhibit seeding in the premetastatic lung. Cancer Cell. 2011;20:300–314.
- Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Worthen GS, Albelda SM. Polarization of tumor-associated neutrophil (TAN) phenotype by TGF-β: “N1” versus “N2” TAN. Cancer. 2010;16:183–194.
- Reglero-real N, Leukocyte Trafficking : time to Take Time Seriously, 273–275 (2019).
- Uhl B, Vadlau Y, Zuchtriegel G, Nekolla K, Sharaf K, Gaertner F, Massberg S, Krombach F, Reichel CA. Aged neutrophils contribute to the first line of defense in the acute inflammatory response.Blood. 2018;128:2327–2338.
- Vafadarnejad E, Rizzo G, Krampert L, Arampatzi P, Nugroho VA, Schulz D, Roesch M, Alayrac P, Vilar J, Silvestre J-S, et al., Time-resolved single-cell transcriptomics uncovers dynamics of cardiac neutrophil diversity in murine myocardial infarction. bioRxiv, 738005 (2019).
- Grayson PC, Sloan JM, Niles JL, Monach PA, Merkel PA. Antineutrophil cytoplasmic antibodies, autoimmune neutropenia, and vasculitis. Semin Arthritis Rheum. 2011;41:424–433.
- Little MA, Al-Ani B, Ren S, Al-Nuaimi H, Leite M, Alpers CE, Savage CO, Duffield JS. Anti-proteinase 3 anti-neutrophil cytoplasm autoantibodies recapitulate systemic vasculitis in mice with a humanized immune system. PLoS One. 2012:7. doi:10.1371/journal.pone.0028626.
- Vorobjeva NV, Chernyak BV. NETosis: molecular mechanisms, role in physiology and pathology. Biochem. 2020;85:1178–1190.
- Lee KH, Kronbichler A, Park DDY, Park YM, Moon H, Kim H, Choi JH, Choi YS, Shim S, Lyu IS, et al. Neutrophil extracellular traps (NETs) in autoimmune diseases: A comprehensive review. Autoimmun Rev. 2017;16:1160–1173.
- Nakazawa D, Masuda S, Tomaru U, Ishizu A. Pathogenesis and therapeutic interventions for ANCA-associated vasculitis. Nat Rev Rheumatol. 2019;15:91–101.
