ABSTRACT
Background
Clinical similarities between chronic fatigue syndrome and idiopathic intracranial hypertension, supported by measurements of intracranial pressure, invite suggestions that they may be connected, the first representing a mild version of the second. Yet, if this is to be the basis for a structural explanation for chronic fatigue syndrome, it already seems incomplete, failing to explain cases where disability seems disproportionate. Is there some other confounding variable?
Purpose
To refine, in this theoretical paper, an earlier model connecting chronic fatigue syndrome with idiopathic intracranial hypertension to allow for a cerebrospinal fluid (CSF) leak.
Model
In this model, the primary structural problem is acquired obstruction to cranial venous outflow. This obstruction can take different forms, may be intermittent and subtle, and even be mistaken for normal venous anatomy, yet would be the driving force behind a tendency towards increased intracranial pressure. This chronic elevation of intracranial pressure stresses the dural membrane maintaining the integrity of the subarachnoid space, which can rupture at a weak point, allowing CSF to leak away and intracranial pressure to fall. The clinical manifestation of this disorder is the product of the severity of cranial venous outflow compromise and of the competing forces on intracranial pressure. In some instances, a CSF leak will mitigate the effects of venous compromise, in others it will compound it, producing a disease spectrum ranging through idiopathic intracranial hypertension, chronic fatigue syndrome, fibromyalgia, and spontaneous intracranial hypotension.
Conclusion
In chronic fatigue syndrome a normal intracranial pressure does not exclude significant physiological disturbance.
Introduction
In folklore, and often observed by healthcare providers, is that patients attempting to diagnose their own unexplained symptoms, find resonance with a wide range of diagnoses. Conventional wisdom puts this down to the power of suggestion. But are these patients really so easily led? Many unexplained medical conditions have multiple overlapping symptoms, including symptoms that seem unaccountably peculiar. Might some of them simply be different manifestations of the same underlying problem? We have explored this idea with respect to chronic fatigue syndrome and idiopathic intracranial hypertension (IIH), with results that seem to indicate the first as a mild form of the second [Citation1,Citation2]. More recently another group has found similar with fibromyalgia [Citation3]. Though open to debate [Citation4], a third group has now recorded dilatation of the optic nerve sheaths and descent of the cerebellar tonsils on MRI as evidence of raised intracranial pressure in a large majority of patients with myalgic encephalomyelitis/chronic fatigue syndrome [Citation5].
Some patients with chronic fatigue or fibromyalgia, however, are so severely affected, that it is difficult to conceive of their condition as the mild form of any illness. This paper refines a model developed in earlier work to take account of these observations [Citation6].
Idiopathic intracranial hypertension and chronic fatigue syndrome
Chronic fatigue syndrome is a condition of unknown cause, characterised by disabling lethargy, which develops spontaneously in either sex, at almost any age, giving symptoms that can last for years. Diagnosis is based on self-reported symptoms. There are no physical signs and no confirmatory laboratory tests [Citation7,Citation8]
Idiopathic intracranial hypertension (IIH) is a condition of raised intracranial pressure of unknown cause, characterised by headache and visual symptoms, arising spontaneously in either sex, at almost any age, giving symptoms that can last for years. The only clinical signs are those of raised intracranial pressure, of which papilloedema is the most important. Blindness is a complication [Citation9].
To suggest a connection based on any of the shared characteristics above might seem facile at first sight and, indeed, differentiating between these two conditions is so little considered a problem that neither features in the differential diagnosis of the other. Yet the primary symptom of one – headache or fatigue – is frequent in the other, and many others – cognitive, memory and mood disturbances, difficulty concentrating, dizziness, anxiety, myalgias and arthralgias – are common to both [Citation10,Citation11,Citation12]. Moreover, some patients with IIH do not have papilloedema, so called IIH without papilloedema (IIHWOP), in which case visual disturbance may be minimal and clinical signs absent [Citation13].
IIHWOP seems to be a milder form of IIH, not only with the relative absence of visual disturbance but with average intracranial pressures lower than the syndrome in full [Citation14]. It is also regarded as a rare variant of IIH, an epidemiological quirk that more probably represents a failure of diagnosis than a true reflection of its prevalence, the explanation lying in the nature of these patients’ symptoms and whether they might trigger investigation of intracranial pressure [Citation6]. Thus, patients with IIHWOP are likely to experience headache and the other multiple symptoms that accompany IIH (described above) but not the key symptom of impending visual loss which alerts the physician to the diagnosis. These other symptoms are not generally of a kind that invites investigation by lumbar puncture, but they are symptoms that would form the basis for a diagnosis of chronic fatigue syndrome [Citation7,Citation8].
It is almost inevitable, therefore, that cases of IIH will be missed in patients who are diagnosed with chronic fatigue syndrome and, pursuing this hypothesis, two independent groups, the first looking at chronic fatigue syndrome and the second at fibromyalgia, have now shown that these patients have average intracranial pressures in the high normal range with some patients unequivocally falling into the category of IIHWOP. Both groups also found that bringing down intracranial pressure by draining cerebrospinal fluid brought about an improvement in symptoms, not just headache but fatigue and pain [Citation2,Citation3].
A key additional finding in these studies was that the symptomatic improvement with lumbar puncture was experienced not only in patients with unequivocally high intracranial pressure, but also in patients whose pressures would be regarded as well within the normal range. This suggests not only that IIHWOP is being missed in chronic fatigue syndrome (and fibromyalgia) but that they are related, with chronic fatigue/fibromyalgia representing IIHWOP in milder form. IIH, therefore, could be regarded as a disorder of intracranial pressure on a spectrum, with the severest form represented by the syndrome in full, an intermediate form by IIHWOP and the mildest form by chronic fatigue/fibromyalgia [Citation6].
Idiopathic intracranial hypertension, spontaneous intracranial hypotension and chronic fatigue syndrome
This construct, however, whilst providing a framework to understand chronic fatigue in terms of an organic disorder of intracranial pressure, does not necessarily advance understanding of the aetiology of the disorder itself. Moreover, it leaves unexplained cases of chronic fatigue or fibromyalgia whose severity cannot be reconciled with a model that places them at the mild end of a disease spectrum.
Spontaneous intracranial hypotension is a disorder of low intracranial pressure caused by the spontaneous development of a cerebrospinal fluid (CSF) leak [Citation15]. The condition implies either a weakness in the dural membrane or a normal dural membrane rupturing under undue pressure. There is an association with some connective tissue disorders but increasingly the condition is being viewed as a complication of IIH, this providing explanation of instances when CSF pressure seems inappropriately high and fostering use of alternative nomenclature, specifically CSF depletion syndrome [Citation15,Citation16]. Surgical repair of a CSF leak which has developed spontaneously can tip a patient into intracranial hypertension, for example. Patients with IIH can present with CSF leaks, or they may develop CSF leaks during the course of their illness [Citation17,Citation18].
The signature complaint of spontaneous intracranial hypotension is headache, worse when upright and relieved by recumbency, in some instances grossly debilitating and accompanied structural changes easily detected on radiological imaging. In other instances, however, the syndrome is more subtle and the postural component to headache is not evident or headache may be absent altogether [Citation15]. Moreover, the other symptoms that accompany intracranial hypotension, including neck pain, blurred vision, nausea, vomiting, dizziness, noise and light hypersensitivity, cognitive problems, apathy and fatigue, do not, by themselves, easily suggest the correct diagnosis, and when neurological examination is normal and there are no abnormal radiological findings, patients may be undiagnosed or diagnosed with non-specific psychological symptoms for years [Citation15,Citation19].
As with IIHWOP, the symptom overlap between spontaneous intracranial hypotension and chronic fatigue syndrome can make them indistinguishable, even in the extent to which either condition may render a patient bedridden. As with IIHWOP, therefore, cases of spontaneous intracranial hypotension will probably be missed in patients who are diagnosed with chronic fatigue syndrome. Moreover, this would not be a chance occurrence but a reflection of the connection between chronic fatigue syndrome and IIH.
Not all patients with IIH who develop a CSF leak deteriorate as a result and, indeed, severe cases can be palliated by repeated lumbar puncture or CSF diversion procedures. Patients with IIH who develop an overt CSF leak in the form of intermittent CSF rhinorrhoea, or post nasal drip, often experience a change in symptoms during or after a period of discharge, either an improvement or a deterioration, sometimes one followed by the other, mirroring the common experience of patients after lumbar puncture. Indeed, it is probable that many patients with IIH reach a symptomatic equilibrium with a CSF leak, overt or occult, fortunate if this resolves visual symptoms and headache, unfortunate if it precipitates a syndrome of CSF depletion that can give origin to symptoms – enforced recumbency, dementia, coma – far more severe than those of the parent condition [Citation15,Citation18,Citation19].
This now suggests a more complete model for chronic fatigue syndrome/fibromyalgia. Specifically, that they are conditions of raised intracranial pressure, no different from IIH except that for the most part, they represent the mild end of the disease spectrum. In some cases, however, the underlying disorder of intracranial pressure will be more severe but modulated by CSF leak, the leak itself unrecognised, sometimes palliating the underlying disorder and at other times responsible for grossly debilitating symptoms. Papilloedema, being a sign of raised intracranial pressure, would be absent.
Idiopathic intracranial hypertension, spontaneous intracranial hypotension and cranial venous outflow obstruction
This modified construct would bind chronic fatigue syndrome to IIH but does not fully resolve the underlying cause. However, it does suggest that there is probably some force driving the condition other than a mismatch between CSF production and CSF absorption, this being one of three candidate causal mechanisms discussed in the literature [Citation20]. Of the other two, idiopathic brain swelling remains purely theoretical; intracranial venous hypertension from obstruction to cranial venous outflow has been the focus of much research [Citation21,Citation22,Citation23].
Regarding venous hypertension, the connection with intracranial pressure is undisputed, superior vena cava obstruction or venous sinus thrombosis, for example, well known causes of raised intracranial pressure, the latter sometimes responsible for a clinical syndrome indistinguishable from IIH. This has raised questions as to whether unrecognised obstruction to cranial venous outflow is responsible for other cases of IIH and in the last few years it has become apparent that narrowings at the anterior ends of both transverse sinuses are usual in this condition, accompanied by high pressures in the venous sinuses upstream [Citation21,Citation22]. This has not provided the solution, however, since raised intracranial pressure, itself, will compress the transverse sinuses and it is difficult to be certain to what extent these narrowings are the cause or effect of raised intracranial pressure [Citation23]. Nevertheless, dilating them up with a stent can bring down intracranial pressure and ameliorate symptoms [Citation24,Citation25,Citation26].
Such cause or effect considerations do not apply if there is extracranial venous outflow obstruction and recently cases of (otherwise) idiopathic intracranial hypertension have been described caused by narrowing of the jugular veins between the styloid processes and the transverse processes of the C1 vertebra, with treatment of the venous narrowings bringing resolution of the clinical syndrome [Citation27,Citation28,Citation29,Citation30]. At the other end of the spectrum, we have reported cases of spontaneous intracranial hypotension caused by narrowing of the jugular veins at the same level, whose symptoms also resolved following treatment directed at the venous stenoses [Citation31,Citation32]. In these cases, taking jugular venous obstruction as the underlying cause of intracranial hypotension, then a procedure (for example, jugular venous stenting) that would normally be expected to reduce intracranial pressure, allowed the CSF leak to heal and intracranial pressure to revert to normal.
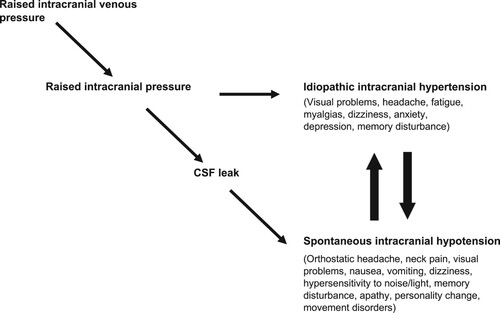
The same pathological process – extracranial obstruction to cranial venous outflow, therefore, can be responsible for syndromes of high or low intracranial pressure, each with their own constellation of overlapping symptoms, depending on whether or not there develops a CSF leak ().
Figure 1. Obstruction to cranial venous outflow causes a rise in intracranial venous pressures leading to a rise in intracranial pressure and the syndrome of IIH. If a CSF leak develops before IIH becomes evident then the physiological disturbance manifests as spontaneous intracranial hypotension (SIH). IIH and SIH have multiple overlapping symptoms and patients may reach an equilibrium position between them, or may cycle between one and the other, reflecting opposing forces on intracranial pressure.
Idiopathic intracranial hypertension, spontaneous intracranial hypotension, cranial venous outflow obstruction and chronic fatigue syndrome
If cranial venous outflow obstruction can be responsible for highly symptomatic cases of raised intracranial pressure or severe intracranial hypotension, then there will also be cases where venous compromise is less pronounced, the measurable physiological disturbance less severe, and the clinical manifestation of this disturbance more subtle. Furthermore, symptoms in such cases will likely be redolent of IIH, as will be what can be measured in terms of intracranial pressure and response to lumbar puncture [Citation33].
Narrowing of the jugular veins between the styloid processes and the C1 transverse processes may be subtle and does not always cause IIH ‘in full’, for example [Citation28]. Zilani et al. [Citation34] were struck by how minor seemed the physiological disturbance that gave symptoms in a patient with tumour obstruction to a jugular foramen. We have shown how damage to non-dominant cranial venous outflow tracts during posterior fossa surgery can be responsible for moderately increased intracranial pressure or CSF leaks, depending on the circumstances, giving chronic non-specific symptoms, including headache and fatigue, prolonged over many years [Citation35]. We have also described a patient presenting with headaches, fatigue and recurring episodes of confusion and epistaxis, these last related to posture, in whom there was very marked asymmetry of cranial venous outflow. Intracranial pressure was normal in the resting supine position but increased markedly with compression of the dominant jugular vein, this associated with exacerbation of symptoms. Increasing the capacity of non-dominant venous drainage by stenting the non-dominant transverse sinus brought about a very substantial clinical improvement, including resolution of symptoms related to posture [Citation36].
Conclusion
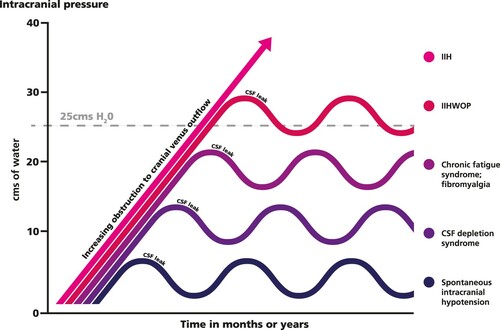
We suggest, therefore, that cranial venous outflow obstruction can take different forms, may be intermittent and subtle, and even mistaken as part of normal variant anatomy, yet be the driving force behind a disorder of intracranial pressure in which pressure may be high, normal or low, depending on the nature and severity of venous compromise and whether or not it is complicated by a CSF leak (). We suggest that the clinical manifestation of this disorder will reflect, not just intracranial pressure, but also the underlying venous obstruction, and is represented by a spectrum which includes chronic fatigue syndrome, fibromyalgia, spontaneous intracranial hypotension and IIH. We suspect that a similar mechanism may be operative in other medically unexplained syndromes.
Figure 2. Pictorial representation of the forces on intracranial pressure generated by obstruction to cranial venous outflow and the subsequent development of a CSF leak. Depending on the site and degree of venous obstruction and the compensating or overcompensating effects of CSF depletion, patients will manifest at different points on the IIH spectrum. A normal intracranial pressure, therefore, does not exclude significant physiological disturbance. IIH : idiopathic intracranial hypertension; IIHWOP: idiopathic intracranial hypertension without papilloedema.
Acknowledgements
The authors are very grateful to Professor Andrew Lever, Academic Department of Medicine, Addenbrooke’s Hospital, Cambridge, UK, for his involvement in this project.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
J Nicholas P. Higgins
J Nicholas P. Higgins is a consultant in diagnostic and interventional neuroradiology at Addenbooke’s Hospital, Cambridge, UK. He has considerable experience treating vascular disorders of the brain, head and neck, from which evolved a research interest in disorders of cerebral venous outflow, their relationship to disorders of intracranial pressure and how these might manifest in clinical practice.
John D. Pickard
John D. Pickard is professor emeritus of neurosurgery in the Department of Clinical Neurosciences of University of Cambridge, UK. He is the honorary director of the National Institute for Health Research’s Healthcare Technology Cooperative (HTC) for brain injury. His research has focused on advancing the care of patients with acute brain injury, hydrocephalus and prolonged disorders of consciousness. He served as president of the Society of British Neurological Surgeons from 2006 to 2008.
References
- Higgins N, Pickard J, Lever A. Looking for idiopathic intracranial hypertension in patients with chronic fatigue syndrome. J Obs Pain Med. 2013;1:28–35.
- Higgins N, Pickard J, Lever A. Lumbar puncture, chronic fatigue syndrome and idiopathic intracranial hypertension: a cross-sectional study. JRSM Short Rep. 2013;4(12).
- Hulens M, Rasschaert R, Dankaerts W, et al. Spinal fluid evacuation may provide temporary relief for patients with unexplained widespread pain and fibromyalgia. Med Hypotheses. 2018;118:55–58.
- Chen BS, Meyer BI, Saindane AM, et al. Prevalence of incidentally detected Signs of Intracranial Hypertension on magnetic resonance imaging and their association with papilledema. JAMA Neurol. 2021;78(6):718–725.
- Bragée B, Michos A, Drum B, et al. Signs of Intracranial Hypertension, hypermobility, and craniocervical obstructions in patients with myalgic encephalomyelitis/chronic fatigue syndrome. Front Neurol. 2020;11:828.
- Higgins JNP, Pickard JD, Lever AML. Chronic fatigue syndrome and idiopathic intracranial hypertension: different manifestations of the same disorder of intracranial pressure? Med Hypotheses. 2017;105:6–9.
- Fukuda K, Straus SE, Hickie I, et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International chronic fatigue syndrome study group. Ann Intern Med. 1994;121(12):953–959.
- Carruthers BM, van de Sande MI, De Meirleir KL, et al. Myalgic encephalomyelitis: International consensus criteria. J Intern Med. 2011;270(4):327–338.
- Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013;81(13):1159–1165.
- Round R, Keane JR. The minor symptoms of increased intracranial pressure: 101 patients with benign intracranial hypertension. Neurology. 1988;38(9):1461–1464.
- Kleinschmidt JJ, Digre KB, Hanover R. Idiopathic intracranial hypertension: relationship to depression, anxiety, and quality of life. Neurology. 2000;54(2):319–324.
- Hulens M, Rasschaert R, Vansant G, et al. The link between idiopathic intracranial hypertension, fibromyalgia, and chronic fatigue syndrome: exploration of a shared pathophysiology. J Pain Res. 2018;11:3129–3140. Published 2018 Dec 10.
- Marcelis J, Silberstein SD. Idiopathic intracranial hypertension without papilledema. Arch Neurol. 1991 Apr;48(4):392–399.
- Digre KB, Nakamoto BK, Warner JE, et al. A comparison of idiopathic intracranial hypertension with and without papilledema. Headache. 2009;49(2):185–193.
- Mokri B. Spontaneous low pressure, low CSF volume headaches: spontaneous CSF leaks. Headache. 2013;53(7):1034–1053.
- Bidot S, Levy JM, Saindane AM, et al. Do most patients with a spontaneous cerebrospinal fluid leak have idiopathic intracranial hypertension? J Neuroophthalmol. 2019;39(4):487–495.
- Schlosser RJ, Woodworth BA, Wilensky EM, et al. Spontaneous cerebrospinal fluid leaks: a variant of benign intracranial hypertension. Ann Otol Rhinol Laryngol. 2006;115(7):495–500.
- Pérez MA, Bialer OY, Bruce BB, et al. Primary spontaneous cerebrospinal fluid leaks and idiopathic intracranial hypertension. J Neuroophthalmol. 2013;33(4):330–337.
- Schievink WI. Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol. 2003;60(12):1713–1718.
- Sussman JD, Sarkies N, Pickard JD. Benign intracranial hypertension. Pseudotumour cerebri: idiopathic intracranial hypertension. Adv Tech Stand Neurosurg. 1998;24:261–305. PMID:10050215.
- Karahalios DG, Rekate HL, Khayata MH, et al. Elevated intracranial venous pressure as a universal mechanism in pseudotumor cerebri of varying etiologies. Neurology. 1996;46(1):198–202.
- King JO, Mitchell PJ, Thomson KR, et al. Cerebral venography and manometry in idiopathic intracranial hypertension. Neurology. 1995;45(12):2224–2228.
- King JO, Mitchell PJ, Thomson KR, et al. Manometry combined with cervical puncture in idiopathic intracranial hypertension. Neurology. 2002;58(1):26–30.
- Higgins JN, Owler BK, Cousins C, et al. Venous sinus stenting for refractory benign intracranial hypertension. Lancet. 2002;359(9302):228–230.
- Higgins JN, Cousins C, Owler BK, et al. Idiopathic intracranial hypertension: 12 cases treated by venous sinus stenting. J Neurol Neurosurg Psychiatry. 2003;74(12):1662–1666.
- Leishangthem L, SirDeshpande P, Dua D, et al. Dural venous sinus stenting for idiopathic intracranial hypertension: An updated review. J Neuroradiol. 2019;46(2):148–154.
- Dashti SR, Nakaji P, Hu YC, et al. Styloidogenic jugular venous compression syndrome: diagnosis and treatment: case report. Neurosurgery. 2012;70(3):E795–E799.
- Higgins JN, Garnett MR, Pickard JD, et al. An evaluation of styloidectomy as an adjunct or alternative to jugular stenting in idiopathic intracranial hypertension and disturbances of cranial venous outflow. J Neurol Surg B Skull Base. 2017;78(2):158–163.
- Zhou D, Meng R, Zhang X, et al. Intracranial hypertension induced by internal jugular vein stenosis can be resolved by stenting. Eur J Neurol. 2018;25(2):365–e13.
- Li M, Sun Y, Chan CC, et al. Internal jugular vein stenosis associated with elongated styloid process: five case reports and literature review. BMC Neurol. 2019;19(112).
- Higgins JN, Axon PR, Macfarlane R. Spontaneous intracranial hypotension complicated by subdural effusions treated by surgical relief of cranial venous outflow obstruction. J Neurol Surg Rep. 2020;81(4):e59–e65.
- Higgins N, Trivedi R, Greenwood R, et al. Brain slump caused by jugular venous stenoses treated by stenting: A hypothesis to link spontaneous intracranial hypotension with idiopathic intracranial hypertension. J Neurol Surg Rep. 2015;76(1):e188–e193.
- Higgins N, Pickard J, Lever A. Borderline intracranial hypertension manifesting as chronic fatigue syndrome Treated by venous sinus stenting. J Neurol Surg Rep. 2015;76(2):e244–e247.
- Zilani G, Pereira EA, Baig F, et al. Venoplasty and stenting of a jugular foramen meningioma. Br J Neurosurg. 2009;23(05):557–560.
- Higgins JN, Macfarlane R, Axon PR, et al. Headache, cerebrospinal fluid leaks, and pseudomeningoceles after resection of vestibular schwannomas: efficacy of venous sinus stenting suggests cranial venous outflow compromise as a unifying pathophysiological mechanism. J Neurol Surg B Skull Base. 2019;80(6):640–647.
- Higgins JN, Pickard JD, Hall F. Stent mediated redistribution of cerebral venous outflow in the treatment of severe intractable headache: a case report. J Obs Pain Med. 2014;1(3). ISSN 2047–0800.
