ABSTRACT
Background
Dialysis implies huge changes in patients’ lives. Yet, there is a need to better understand patients’ experience in the time following dialysis initiation.
Objective
The objective of this study was to investigate patients’ experience of dialysis a year after treatment initiation and the associations between patients’ discourse and their anxiety and depression symptoms.
Methods
Twenty two patients (mean age 63.4; 68% men) took part in a semi-directed interview about their experience with dialysis. Participants completed the Hospital Anxiety and Depression Scale (HADS). Interviews were analyzed using a lexicometric analysis.
Results
The analysis generated five classes: experience with nephrological care, facing loss and family relationships, family and acceptance, implementation of a new routine and making sense of the end-stage renal disease experience. Patients’ felt very passive in their experience with care. They reported the importance of integrating dialysis in their lives and the role of family support when facing treatment initiation. Depressed patients were more likely to describe their nephrological monitoring very factually and to talk about what they lost with dialysis initiation.
Conclusion
Dialysis initiation is a hard time for patients during which they face many challenges. This first year represents a time of adaptation, in which family seems essential.
Introduction
End-stage renal disease (ESRD) is the failure of kidneys to function. In France, around 84,000 patients are living with ESRD and are treated with renal replacement therapy. Among them, nearly 47,000 are undergoing a life-long treatment: dialysis. The number of patients treated by dialysis is constantly increasing (Agence de la Biomédecine, Citation2016; Vigneau et al., Citation2017). Two main types of dialysis exist: hemodialysis and peritoneal dialysis. In addition to technical differences, these two treatments differ regarding the frequency, the location and who implements these treatments. Peritoneal dialysis requires daily treatment cycles whereas hemodialysis takes place every two days. Moreover, while hemodialysis mostly takes place in dialysis units or hospital centres, peritoneal dialysis can be done at home. This implies that patients often carry out peritoneal dialysis on their own or with help from a family member (Haute Autorité de Santé [HAS], Citation2017). Dialysis is a complicated treatment and represents a huge change in patients’ lives. Besides frequent dialysis sessions usually at least 4 hours 3 times a week, patients must follow fluid/dietary restrictions, take medications and attend medical appointments (Molzahn & Butera, Citation2006). Dialysis patients are more likely to have a poor quality of life, and to be more anxious and depressed than the general population (Cukor, Coplan, Brown, Peterson, & Kimmel, Citation2008; Fukuhara et al., Citation2003). Depressive symptoms are very common at dialysis initiation (Watnick, Kirwin, Mahnensmith, & Concato, Citation2003). Moreover, quality of life at dialysis initiation predicts health outcomes (e.g. hospitalization) (Lopez Revuelta, Garcia Lopez, de Alvaro Moreno, & Alonso, Citation2004). Similarly, depression seems to predict patients’ mortality (Farrokhi, Abedi, Beyene, Kurdyak, & Jassal, Citation2014). Some authors argue that depression may be part of a normative response to ESRD (Rodin, Citation1994). Nevertheless, high levels of anxiety appear to be frequent (Yoong et al., Citation2017).
Several studies have highlighted patients’ feeling of dependence and restriction. The changes stemming from this treatment imply a search for a ‘new normal’ and the need to adapt to dialysis (Makaroff, Citation2012). Patients feel their illness changes their relationships and affects the social roles they had (Karamanidou, Weinman, & Horne, Citation2014). Patients report changes in their family life and guilt when they feel dialysis restricts their families’ activities. ESRD can also impact patients’ close ones, especially their families (Lindsay, MacGregor, & Fry, Citation2014b). Psychosocial factors play an important role in patients’ adjustment to ESRD, especially social support (Untas et al., Citation2011). Emotional support is linked to autonomy and self-esteem whereas overprotection has opposite effects (Jansen et al., Citation2014).
Diagnosis and nephrological care do not seem to affect patients much till the announcement of dialysis initiation (Desseix, Citation2011). The start of treatment represents a shocking event for patients (Schell, Patel, Steinhauser, Ammarell, & Tulsky, Citation2012). They lack preparation and report mental and physical challenges facing this new way of life. In hemodialysis, high mortality rates are observed during the first year of treatment compared to the following years (National Institutes of Health [NIH], Citation2017; Robinson et al., Citation2014). In addition, this period is marked by changes in employment status and income (Kim et al., Citation2017; van Manen et al., Citation2001). Patients also seem to perceive dialysis as an illness with its own symptoms and consequences. It represents a biographical disruption, exposing patients to their mortality (Desseix, Citation2011). In the study of Gustafsson et al. (Clarkson & Robinson, Citation2010; Karamanidou et al., Citation2014; Makaroff, Citation2012; Reid, Seymour, & Jones, Citation2016; Stringer & Baharani, Citation2012), patients were interviewed about their past, present and future with dialysis. They reported a shift from freedom to dependency, the need to adjust to a new life and the transition toward acceptance. However, this study included patients no matter the time since dialysis initiation.
Several qualitative studies (Clarkson & Robinson, Citation2010; Karamanidou et al., Citation2014; Makaroff, Citation2012; Reid et al., Citation2016; Stringer & Baharani, Citation2012) have investigated patients’ experience with dialysis in general. They highlighted the feeling of dependence/restriction and the importance of patient-professional relationships (Reid et al., Citation2016). These studies dealt with the dialysis experience at large and not specifically on dialysis onset (Lai, Loh, Mooppil, Krishnan, & Griva, Citation2012; Monaro, Stewart, & Gullick, Citation2014; Stringer & Baharani, Citation2012). So far, only three qualitative studies focused on this particular period. The first one showed how this time is marked by loss and grief. Indeed, freedom, autonomy and social life are affected by dialysis (Monaro et al., Citation2014). It used a hermeneutic method and both patients’ and family members’ interviews were analyzed together. The other two studies used methods that are not well described. They showed how distress, social support and treatment-related concerns were prominent in patients’ interviews (Lai et al., Citation2012). Moreover, after dialysis initiation few elderly participants still found their treatment acceptable (Stringer & Baharani, Citation2012). Although the first year following dialysis initiation appears to be crucial, literature on the subject is scarce.
Most qualitative studies that have been carried out have used either a form of content analysis or a method based on phenomenology (Chiaranai, Citation2016; Karamanidou et al., Citation2014; Reid et al., Citation2016; Schell et al., Citation2012; Xhulia et al., Citation2015). None of them used a lexicometric analysis. This term refers to computer-assisted methods allowing ‘formal reorganizations of text sequences and statistical analyses on the vocabulary of a text corpus’ (Lebart, Salem, & Berry, Citation1997). It allows researchers to examine both the content of participants’ discourse and their wording. Another strength of this approach is to consider quantitative data in the analysis. This seems interesting considering the rates of anxiety and depression in this population which could be related to patients’ discourse.
This qualitative study aimed to investigate patients’ experience of dialysis a year after treatment initiation through a lexicometric analysis. In other words, we wished to explore this experience through the analysis of speech patterns. We also wanted to investigate the associations between patients’ discourse and anxiety and depression symptoms.
Methods
Sample
Research participants were ESRD patients on dialysis. They were recruited in five French dialysis units located in the South-West of the country. Inclusion criteria were: having been treated by dialysis for at least a year (from twelve to fourteen months), being over 18 years old and speaking French. Patients who had had a renal transplant, a previous experience of dialysis, or cognitive problems (e.g. disoriented in time/place) were excluded.
Twenty-two patients took part in this study. Thirteen were on hemodialysis in a hospital centre, 8 were on hemodialysis in satellite units and a patient was on peritoneal dialysis. Participants ranged in age from 26 to 82 with a mean age of 63.4 years (SD = 16.9), 68% were men, 68% were in a relationship and 77% had at least one child. Regarding their professional status, 59% were retired, 27% were disabled, 14% were employed, and 5% were looking for a job. Twenty-seven per cent were on a waiting list for renal transplantation or in the process of being added on a waiting list. Fourty-five per cent changed dialysis modality/location since its beginning.
Data collection
This research is part of a larger longitudinal study that included 120 patients starting dialysis. Seventy-five of the initial patients participated to the follow-up about a year after treatment initiation. Then, patients were proposed to take part in a semi-structured interview. The first 22 participants to accept to take part in the qualitative part of the research were interviewed. A health psychologist introduced the study to each patient and gave information on the goal of the interviews. If the patient agreed to take part in the study, an informed consent was signed. Socio-demographic and medical information was collected: age, gender, marital status, professional situation, number of children, education level, condition of dialysis initiation, dialysis modality, registration on a waiting list for renal transplantation, change in dialysis modality/location. Patients were also asked to complete a questionnaire measuring depression and anxiety symptoms. Then, an interview began, with open-ended questions to encourage participants’ self-expression. The interview items are available in Box 1. The mean duration of the interviews was 50 minutes.
Pre-dialysis period
Adjustement to dialysis
Health problems and complications linked to dialysis
Changes related to dialysis
Medical monitoring
Information
Future
Depression and anxiety were measured with the Hospital Anxiety and Depression Scale (HADS) one year after dialysis initiation some days before they were interviewed (Bjelland, Dahl, Haug, & Neckelmann, Citation2002; Zigmond & Snaith, Citation1983). The French adaptation of the questionnaire has good psychometric properties (Razavi, Delvaux, Farvacques, & Robaye, Citation1989). It has been validated in a sample of dialysis patients (Untas et al., Citation2009). This allowed to categorize patients into two groups: anxious vs. non-anxious patients and depressed vs. non-depressed patients. The thresholds chosen to categorize participants’ depression and anxiety scores are: 9+ for the anxiety subscale and 7+ for the depression subscale (Bjelland et al., Citation2002).
Ethics statement
At the time of the study having an ethical approval was not mandatory for this type of research under French law. However, when we conducted our study we:
informed patients of the aims of the study;
made sure participants understood the study, what it implied and wanted to take part in it;
gave information letter about the study;
informed patients that patients of their right to withdraw from the research, they were notified that participation was anonymous, and that information was strictly confidential and would be used solely for scientific purposes;
obtained signed consent forms after approval.
Data analysis
All twenty-two interviews were transcribed. The whole corpus was 90 pages (62,467 words) long.
We proceeded to an inductive quantitative content analysis. A lexicometric analysis assisted by Iramuteq (R interface for multidimensional analysis of texts and questionnaires) software was performed on the interviews. This kind of analysis is based on an automatic analysis of speech providing a quantitative analysis of the data. Iramuteq software performs a lemmatization. This process reduces words to their lexical root, named lemmas (e.g. doing and does become do). Then, the corpus is automatically divided in Units of Context (UC) based on the number of occurrences (words) and punctuation (Reinert, Citation1983, Citation1990). We used the Alceste method developed by Reinert (Reinert, Citation1983) to conduct our analysis and executed it with Iramuteq (Ratinaud & Marchand, Citation2012). A descending hierarchical classification (DHC) classifies UCs into classes according to the distribution of words/lemmas. A chi-square indicates the strength of the association between these lemmas and their class. The DHC also includes a Correspondence Analysis (CA) performed on contingency tables showing UCs crossed with the classes of the analysis. In this analysis, grammatical words (e.g. articles, pronouns) were considered supplementary whereas content words (e.g. nouns, verbs) were active. Active forms contribute to the axes of the CA whereas supplementary forms do not. Thus, words conveying the sense of the sentences were considered in the construction of the classes by Iramuteq. The links between classes and function words (words that express grammatical relationships) were calculated by Iramuteq in a second phase. Our aim was to identify classes of meaning rather than grammatical classes. Although LM proceeded to an inductive analysis, results from such method may be influenced by the research objectives and the researchers’ assumptions and experiences (Thomas, Citation2006). That is why we wrote a short ‘intellectual equation’ (Paillé & Mucchielli, Citation2016) available as a supplementary material. The goal of this equation is to describe the author’s (LM) influences in the interpretative process (e.g. experiences, theories). Results were reviewed by the researcher who interviewed the participants (AU) in order to strengthen our analysis (Creswell & Creswell, Citation2018). AU assessed and discussed the analytic process from the raw interviews to the interpretation. She could ask questions about our analysis to enhance the accuracy of the results. This method allows for a rigorous analysis of the data without losing the strengths of a qualitative analysis.
Moreover, Iramuteq software allows to consider categorical variables in the analyses. Thus, age, gender, marital status, professional situation, number of children, education level, dialysis modality, registration on a waiting list for renal transplantation, change in dialysis modality/location, depression and anxiety were taken into account in the analyses. Indeed, the program proceeds to chi-squared associations between these variables and each class identified. This allowed to encompass the quantitative variables listed earlier.
In summary, the Reinert method reorganizes the text from its chronological order to ‘lexical worlds’. A lexical world gathers in a same cluster of words, different moments of the participants’ discourse and thought process as well as different point of views on a similar subject (Reinert, Citation1993). They are the most important traces of these perspectives. Lexicometric analyses rest upon the idea that recurrences are pertinent: the regularity of a phenomenon in the discourse is what matters most (Lejeune, Citation2010). Since our objective was to investigate these perspectives and patients’ patterns of speech, we opted for the Alceste method to explore our corpus and investigate participants’ views and ways of expressing them.
Results
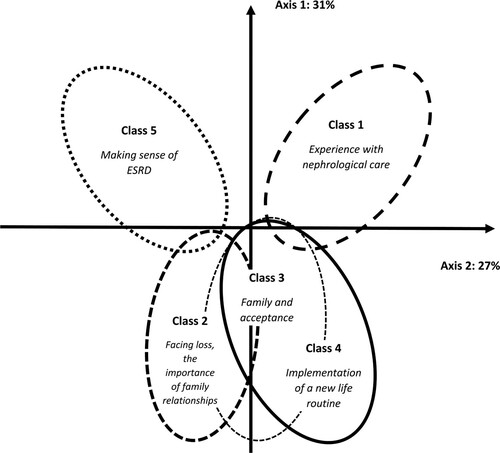
The analysis generated five classes encompassing 84% of the corpus. Sixteen per cent of the corpus could not be attached to any of the five classes. This could be due to our interview grid which allowed participants to talk openly about their experience. The dendrogram representing these classes is available in .
Figure 1. Results of the descending hierarchical classification (DHC).
*In French, these words can have two meanings, it is indicated within parentheses. N.B.: This table presents the first 17 most strongly associated active forms (p < .001) and supplementary forms (p < .05) in each class as well as the significant variables associated to them (p < .05).
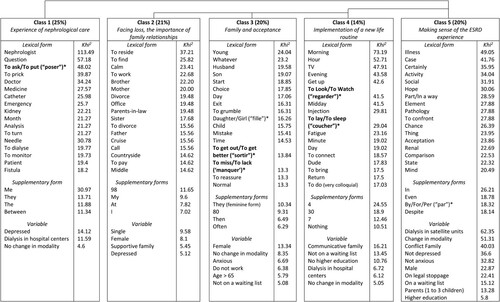
Class 1: experience with nephrological care
Class 1 encompasses 25% of the classified corpus. It deals with patients’ experience with their nephrological care before and after dialysis initiation.
‘Nephrologist’ is the word most significantly associated with class 1. Most patients report a feeling of closeness with their nephrologist due to the frequency of their meetings and the monitoring before dialysis. However, others describe their physicians with more negative terms. The word ‘nephrologist’ is associated with the words ‘ask/put’ and ‘question’. Questions have an important place within this relationship. Indeed, nephrologists are both the ones asking questions and the ones patients want to ask questions to. However, if some of patients’ questions are answered, others are left ignored.
They ask you questions […] there is a relationship which can be very nice with some of them but others are … How could I say … who do not feel concerned at all. (Andre, 70)
When I ask questions they don’t answer, they don’t spend much time with the patient, it would be normal they spend more time … (Daryl, 82)
Very few verbs are associated with this class. Apart from ‘ask’, most of the verbs either describe a passive event (‘turn’, ‘dialyse’) or refer to actions made by the staff (‘put’, ‘turn’, ‘prick’, ‘monitor’). Patients used ‘turn’ to either describe pain or movement in/by the staff. Interestingly, an indefinite pronoun roughly equivalent to ‘someone’, as well as ‘they’ and ‘me’ is associated with this class. These words are supplementary forms. Patients seem to feel passive and see professionals as an undefined entity.
They took my blood and I arrived at about 3:30 […] and at 7:00 I was at the hospital and the next day I went on dialysis. I didn’t know what was happening. (Bill, 74)
Class 1 was more represented by: patients without children, patients who were dialysing in hospital centres, who had not changed treatment modality/location and depressed patients.
Class 2: facing loss, the importance of family relationships
Class 2 encompasses 21% of the classified corpus. Words pertaining to family are linked to this class such as ‘brother’, ‘mother’, ‘parents-in-law’, ‘family’ and ‘relationship’. These words refer to both the family context within which dialysis is initiated (e.g. ‘divorce’) and how relationships are transformed following treatment initiation.
My husband is an only son, my son is an only son, you see my family stopped quickly. On my side of my family we were numerous. When we grow old, it’s like this … I, who was used to big families and big dinner parties … But now I only have one sister, that’s all. (June, 79)
When I need something, bam! It’s done because she [my sister] cares and when she was sick, well, we helped her. We get along well, we are a very very close family. (Malcolm, 69)
I am divorced, I work part-time and to cope I want to have a transplantation quickly and find a full-time job. (Julia, 43)
Indeed, for most patients, dialysis rearranged their relationships (e.g. ‘find/meet’, ‘middle’). However, their close ones support them while they face ESRD, sometimes despite distance. ‘Reside’ brings to light this notion.
I don’t want to find myself sick in the middle of healthy people. (Freddie, 67)
With my family, we didn’t see each other much. But then, with the illness and everything that happened it kind of brought us together. (Fitzgerald, 30)
Despite the role of family support during this period, dialysis remains something patients experience alone.
I come here alone, by car. It’s okay, I’ve spent my whole life [when I was a nurse] telling patients that what they can do alone, they should do it. (Amy, 56)
In addition to change in relationships, another predominant idea is the sense of loss following dialysis initiation. ‘Habit’, ‘find/meet’, ‘travel’, ‘holidays’, ‘work’ and ‘office’ highlight that patients feel they cannot do what they could do before (e.g. working). Habits they had before dialysis must be changed. Moreover, some patients describe change in their personality (e.g. ‘calm’).
When I was working, we used to go out as couples, we had barbecues … We met in the forest, hiked … Now it’s over. Some colleagues try to contact me, but I don’t want to. (Freddie, 67)
Never, never you will find your health again. (Andre, 70)
I used to always have the fidgets, now I am calmer, I read a lot. (Amy, 56)
Contrary to class 1, supplementary forms include ‘I’ and variations of ‘my’ in French. Its content is more personalized than that of class 1.
This class is associated with the following characteristics: women, single patients, without children and depressed patients.
Class 3: family and acceptance
Class 3 encompasses 20% of the classified corpus. It focuses mainly on the consequences of dialysis and the sense of limitation that comes with it.
As for class 2, many words pertaining to family are linked to this class such as ‘husband’, ‘son’, ‘daughter’ and ‘child’. Family support seems crucial when facing dialysis. Contrary to the previous class in which the words referred to extended family members, in class 3 it focuses on nuclear family.
Life is so hard, without my daughter I would stop fighting. Fortunately, I have my husband. He is amazing. (Kelly, 50)
This support can go both ways. Indeed, ‘reassure’ is associated with this class. It can refer to reassurance family members provide to patients as well as patients’ perception of their families’ need for reassurance.
[My son] is a little more reassured but there are times when he’s not well. He’s here every day at any time of the day. (June, 79)
‘Accept’ is also associated with this class. It can refer to illness acceptance or lack thereof by the patient and his/her family. ‘Exit’, ‘to get out/to get better’ also highlight this notion.
I’m under the impression that time has stopped since September. Transplantation I feel like it’s the exit door. (Amy, 56)
I think [my mother] considers I’m dead, gone. It’s not easy, yeah. She’s a nurse it can seem … And I think she still hasn’t accepted this situation, that it happens to her daughter. (Rose, 26)
‘Start’ appears in sentences in which patients describe their experience of dialysis initiation and how their perspective has changed since then.
It was a little hard at the start because [dialysis] it’s new, but it did not affect me tremendously. You have to adapt. (Colin, 80)
‘Choice’, accept’, ‘first’, ‘whatever’ and ‘normal’ highlight the difficulties for patients to accept a treatment they have no choice to follow. They report they cannot do ‘whatever’ they like anymore such as going out, for example. Dialysis and its consequences are not considered ‘normal’. The time constraints implied by dialysis, represented by ‘day’ and ‘time’, seem especially hard to overcome.
That’s why I say I have the impression to live part-time because during almost half of the week, we are not living the normal life. (Arthur, 74)
It’s a chore but we accept it yes, because we don’t have a choice but it’s still a terrible constraint, every two days … (Andre, 70)
‘To miss/to lack’ is used to describe what lacks in their medical monitoring, what they miss/lack because of ESRD (e.g. breath, hobbies) or what they do not miss. Similarly, ‘young’ appears in sentences in which patients describe their younger years or tell the problems they encounter in their monitoring because they are (not) young.
She tries to make meals, ah yes we lack this [information on nutrition], we know nothing about it. Nephrologists don’t talk about it. (Benjamin, 79)
Some people are much younger than me so I am doomed to a very long wait. (Andre, 70)
This class is associated with the following characteristics: women, older patients, patients who did not work, who never changed dialysis modality/location, who were not on a waiting list for renal transplantation and anxious patients.
Class 4: implementation of a new life routine
Class 4 encompasses 14% of the classified corpus. It deals with patients’ description of their life routine after dialysis initiation. Words such as ‘morning’, ‘tv’, ‘evening’, ‘get up’ and ‘go to bed’ appear jointly with ‘injection’, ‘connect’ and ‘machine’. This refers to the integration of dialysis in patients’ day-to-day life.
If some patients manage to adapt to their treatment, others struggle to find the right place for dialysis in their lives.
I like having friends and laughing with them. The four hours go by quickly. […] Sometimes I even go cheerfully, we laugh, everyone tells what he/she has been up to. (John, 50)
I’m never happy in the morning when I go to the dialysis centre. I get up at 5:00 am to go take the car at 6:30 and I go to sleep at 8:00 or 8:30 pm whereas before I didn’t go to bed before 11:30. (Kelly, 50)
Another idea of this class relates to the time dialysis takes in their life. ‘Hour’, ‘minute’, ‘morning’ and ‘day’ highlight this notion. Moreover, most supplementary forms are numbers (e.g. ‘4’, ‘30’, ‘7’). They often refer to time periods.
Patients are completely left to themselves. Someone should find a way to pass the time. The problem is not dialysis per se, it’s those 4 hours that are awful. (Andre, 70)
This class also deals with the difficulties of integrating dialysis in one’s day-to-day life. ‘Tiresome’, ‘have to’ and ‘hard’ show how dialysis can be a burden.
I put up with it that’s all, since I have to. It’s those three days, you feel … […] You feel a little imprisoned. (Nicky, 80)
This class is associated with the following characteristics: patients who did not pursue higher education, who were not on a waiting list for transplantation, who did not change dialysis modality/location and patients dialysing in hospital centres.
Class 5: making sense of the ESRD experience
Class 5 encompasses 20% of the corpus. It deals with patients’ attempt to make sense of what happened or will happen to them. It is significantly associated with two patients: Simon and Freddie. Therefore, some elements may not represent the whole sample.
Patients describe their illness, its consequences and their process of making sense of ESRD. Moreover, words appear to be more formal than in other classes.
‘Even’, ‘despite’, ‘currently’ and a French word roughly equivalent to ‘by/for’ (appearing in sentences like ‘for example … ’ or ‘by comparison … ’) are supplementary forms associated with this class. ‘Certainly’ and ‘example’ are active forms associated with this class. These UCs, mostly transition words, show how patients connect their experiences. By connecting these events they give sense to what happened to them.
I feel better by comparison to before dialysis, less tired. No, not much has changed although I stopped working. No, just like before […] because I avoid talking about dialysis. (John, 50)
Class 5 also includes ‘illness’, ‘case’, ‘life’, ‘state’ and ‘situation’. This class comprises very few verbs. Patients talk about their illness and what it implies for them. They explain how they see life since dialysis initiation and how they consider the future. This interpretation is strengthened by ‘acceptation’ and ‘hope’.
It’s not a dream life. It’s life. And life isn’t always perfect, so you have to accept it like this. I accept, I have accepted dialysis. I have accepted maybe, I don’t know. (Arthur, 74)
This class encompasses all the variety in patients’ ways to live and describe their experience with dialysis. Participants talk about how they cope(d) with dialysis and how they have changed since treatment initiation. Indeed, some report how they coped thanks to social support or by changing for a treatment option better suited for them, for example. They also show introspection on their psychological functioning, some report being inherently optimistic whereas others are not. This process of making sense also leads to comparisons about how they were before and after treatment initiation. ESRD made some of them rearrange their relationships, their work life and some parts of their character in a positive or negative way. Others report not much changed since dialysis initiation. The common core of this experience is ESRD.
With all the technology we have nowadays, we can cure everything. I can’t believe we can’t cure an illness … […] To my mind, I can’t admit it. (Freddie, 67)
It’s true that it’s a tiring fight […] You must maintain a certain optimism, even a will to fight. We can’t give in, we can’t let go. (Simon, 50)
‘Transplantation’ and ‘chance’ show how some patients look to the future, with or without transplantation. Some consider they are lucky to be on dialysis, to be monitored and to be in relatively good health. They compare their own experience with their close others’ facing ESRD or another illness.
I’m lucky, I still urinate a lot […]. When I talk about it with other patients, they tell me You, you still urinate, it is not the same … You can get away with more. (Robert, 47)
Patients use the word ‘thing’ to describe dialysis and its consequences. It encompasses things dialysis prevents them to do, things that add up to dialysis and things related to dialysis.
I’m becoming grumpy the littlest thing in relation to a situation … Before and after dialysis, clearly it changes a little. (Alec, 76)
I knew […] the start of dialysis would have positive outcomes even if it is something very hard to bear psychologically speaking. (Simon, 50)
Although ‘acceptation’ belonged to class 5, it is only pronounced 6 times by a single participant. Therefore, we decided not to include this element in our interpretation. This class is associated with the following characteristics: men, patients with higher education, who had children, who were on a legal work stoppage because of ESRD, patients dialysing in satellite units, who changed dialysis modality/location, who were on a waiting list for renal transplantation and non-depressed and non-anxious patients.
Links between classes
The CA graphic representation is presented in . Classes 2, 3 and 4 overlap each other revealing that loss, routine and acceptance (or lack thereof) are linked. We could hypothesize that every class of this group interacts with the other. Acceptance depends on the existence of loss and the implementation of a routine and vice versa. These three classes oppose classes 1 and 5 on the first axis. This factor represents a continuum from illness life (how patients think and experience ESRD) to life with the illness (how patients incorporate their disease in their life).
Class 1 opposes class 5 on the second axis. Class 1 focuses on the description of their monitoring and highlights a feeling of passiveness. Class 5, however, illustrates how patients make sense of their experience and how they think/feel about ESRD. This axis represents a continuum from a depersonalized description of facts to introspection.
Discussion
This study allowed to shed light on the experience of dialysis patients a year after treatment initiation. Until now, few studies have focused on this crucial period (Chilcot et al., Citation2013; Lai et al., Citation2012; Monaro et al., Citation2014; Stringer & Baharani, Citation2012). Previous studies showed that freedom and autonomy were very prominent themes in patients’ interviews. Our research showed that patients confronted to treatment initiation address similar subjects to patients who have been on dialysis for a longer time (Makaroff, Citation2012). However, we also highlighted how patients encounter very specific challenges in the period following treatment initiation. Indeed, family, illness acceptation and adaptation are very central in patients’ experience in the time following dialysis initiation. The Alceste analysis allows to take into account quantitative variables, as it has been done in similar studies (Bucci & Vanheule, Citation2018; Lelorain, Tessier, Florin, & Bonnaud-Antignac, Citation2012). However, these results should be read with caution as this is an exploratory method to investigate this kind of association. Depressed patients were more likely to talk about what they lost with dialysis initiation and to describe their nephrological monitoring very factually. Indeed, previous research has shown that depressed patients use more impersonal and truncated sentences than healthy controls (Trifu, Nemes, Bodea-Hațegan, & Cozman, Citation2017).
Our analysis encompassed 84% of the whole corpus. Although no official threshold exists to quantify a satisfying classification in lexicometric analysis, this percentage could be considered a very satisfying one. Indeed, among recent studies using a similar procedure (i.e. interviews) the percentage of classified UC ranged from 60% to 74% (Bucci & Vanheule, Citation2018; Denoual, Dargentas, Roudaut, Balez, & Sizun, Citation2016; Guzmán-Osorio, Chávez-Vallejo, Monzerrat Silvat, Parrello, & Ioro, Citation2017; Moscato & Varescon, Citation2018). We first underlined that patients do not seem to feel as actors of their own health. This hypothesis was reflected by the way participants told their experience. This result is in line with previous studies that reported a feeling of losing personhood within the clinical world and an asymmetry in power within patient-professional relationships (Lindsay et al., Citation2014; Reid et al., Citation2016). Its presence as a significant class in our analysis could be due to the questions we asked patients about their monitoring. However, it provides interesting information about patients’ care experience. The first year of dialysis is characterized by a shift in monitoring. Indeed, patients reported that nephrologists did not spend much time with them. This contrasts with their monitoring before the start of dialysis. This class is associated with patients dialysing in centres. In these centres, patients see a nephrologist every dialysis session often for a very short time (due to the number of patients the nephrologist has to see during a dialysis session). As numerous nephrologists work there, patients have to adjust to a main follow-up change which turns from a specific one with a same nephrologist (who they may know for years) before dialysis to a frequent but short follow-up during dialysis with several nephrologists. This observation seems important considering less patient-nephrologist contacts is associated with lower patient satisfaction and nephrologists concern for patients is among the most important aspects of care for patients (Plantinga et al., Citation2004; Rubin et al., Citation1997).
The second class highlighted patients’ experience of loss and the role family plays in the adaptation to this new life. It is associated with depressed patients. The sense of loss that comes with treatment initiation could be associated with depression symptoms. Professionals should pay attention to this kind of content in patients’ speech. Previous studies reported the burden of the limitations induced by dialysis (e.g. travel) (Karamanidou et al., Citation2014; Reid et al., Citation2016). Surprisingly, the dietary and fluid restrictions that go with dialysis did not appear in this analysis unlike in other studies (Lai et al., Citation2012; Palmer et al., Citation2015). Moreover, first-person singular pronouns are associated with the two classes (Class 1 and 2) linked to depression symptoms. This is congruent with previous research on the linguistic specificities of depressed patients’ language (Edwards & Holtzman, Citation2017).
The third class shows how accepting a treatment patients have no choice to follow is a challenge both for patients and their families. Indeed, the treatment also affects families’ well-being, especially in the beginning of dialysis (Monaro et al., Citation2014). This class is associated with anxious patients. We can hypothesize that the acceptance process is a source of anxiety and that patients need reassurance. Interestingly, family has a noteworthy place in two themes. This could indicate the important role family takes during this time, especially family support which seems crucial when facing treatment initiation. Patients perceive their families support them but also that this transition affects those close to them who, in turn, need support. Class 2 and 3 highlight how loss and acceptation are important elements of the experience following treatment initiation. It is interesting to notice that they are both associated with women which suggest that family may be a particularly important part of women’s experience with ESRD.
The fourth class encompasses descriptions of the new routine patients must implement and how this rhythm can be hard to find. Adjustment to life on dialysis, although quite specific to the beginning of treatment, is an ongoing process as changes in health are encountered (Reid et al., Citation2016). Our results are congruent with previous studies. The ‘abnormal normalcy’ of ESRD was highlighted in a previous literature review (Makaroff, Citation2012). The themes we identified reflect this search for normalcy by implementing a new life routine, facing loss and moving toward acceptance.
Finally, we interpreted the fifth class as an attempt to make sense of ESRD. It was associated with patients with higher education and who may be more active in their care (e.g. who changed dialysis modality/location) compared to others. Previous research has shown that people from a higher social class are more likely to speak about their experience and to engage in self-reflection (Radley, Citation2002). This class encompasses patients’ different ways to think and feel about ESRD. It brings to light how making sense of the illness and coping with it is a very individual process. The commonality between all these various experiences is ESRD. However, this class was mainly represented by two individuals. It may highlight that this reflection is not shared by every participant. Since patients can have trouble perceiving a positive future with dialysis following treatment initiation (Monaro et al., Citation2014), it could make this process harder to handle.
The classes identified in the analysis interact with one another. Class 2, 3 and 4 represent how patients consider and face this new way of life. Their links show patients’ grieving process regarding ESRD. As for the opposition between class 1 and 5, they highlight a continuum between a factual description of their care to an introspection regarding how they think and feel about their illness. While this first class is associated with several participants, class 5 is not. This could show how patients’ view of care has a predominant place in their overall experience with ESRD. It seems shared among several participants whereas introspection may not be a common process among patients or might be difficult to express or talk about in a single research interview.
This research comprises two main limitations. First, only one patient on peritoneal dialysis participated in this study. Therefore, the results presented mainly reflect patients on hemodialysis. Future research might investigate the differences in patients’ speech according to their dialysis modality. Second, some classes may have appeared because of our interview items, in particular the first class. However, our analysis allowed us to draw interesting conclusions on how patients talk about their experience.
In conclusion, this study showed that, a year after dialysis initiation, patients face challenges like those of patients who have been on dialysis for a longer time. However, they have a specific experience linked to the beginning of their treatment. Indeed, we noticed that illness acceptance, adaptation and family are predominant elements in patients’ interviews. Although decision regret is rare (7-8%), patients who report family influence on their RRT choice also report greater regret (Berkhout-Byrne et al., Citation2017; Gilman et al., Citation2017; Tan, Teo, Finkelstein, & Meng, Citation2019). This could indicate more conflictual family relations, which has been linked to patients’ mental health (Untas, Rascle, Idier, Lasseur, & Combe, Citation2012). On the other hand, supportive families could help the illness acceptance process. These results highlight the importance of caring for patients during this period.
Regarding practice implications, the first year following dialysis initiation appears to be a time of adaptation for patients. Thus, they may need particular attention regarding their informational (e.g. regarding monitoring) and emotional needs. This could help support their acceptation process. Furthermore, family should be taken into account in patients’ monitoring, especially following treatment initiation considering the crucial role they have. Family members may also face specific difficulties that should be addressed. Moreover, health professionals should be attentive to patients talking regularly about loss (e.g. things they cannot do anymore) and passiveness. This may be a sign of emotional difficulties. Moreover, results showed that their experience with care was linked with a feeling of passiveness and could be associated with depression symptoms. Therefore, it seems especially important to empower patients to be actors of their own health.
Lexicometric analysis appears to be a rich method to study patients’ speech. Indeed, it allows to investigate both what participants are talking about and how they are telling their experience. Future research could use this method to investigate patients’ experience of ESRD before and following dialysis initiation to better understand patients’ difficulties and needs.
Supplemental Material
Download MS Word (18.9 KB)Acknowledgements
This research was supported by the Fondation de France. We thank our colleagues and the patients who accepted to take part in the study for their help.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Agence de la Biomédecine. (2016). Rapport annuel du registre REIN 2016. Registre REIN, 97. doi:https://doi.org/10.1111/epp.2605
- Berkhout-Byrne, N., Gaasbeek, A., Mallat, M. J. K., Rabelink, T. J., Mooijaart, S. P., Dekker, F. W., & Van Buren, M. (2017). Regret about the decision to start dialysis: A cross-sectional Dutch national survey. Netherlands Journal of Medicine, 75(6), 225–234.
- Bjelland, I., Dahl, A. A., Haug, T. T., & Neckelmann, D. (2002). The validity of the Hospital Anxiety and Depression Scale: An updated literature review. Journal of Psychosomatic Research, 52(2), 69–77. doi:https://doi.org/10.1016/S0022-3999(01)00296-3
- Bucci, F., & Vanheule, S. (2018). Families of adult people with disability: Their experience in the use of services run by social cooperatives in Italy. International Journal of Social Welfare, 27(2), 157–167. doi:https://doi.org/10.1111/ijsw.12283
- Chiaranai, C. (2016). The lived experience of patients receiving hemodialysis treatment for end-stage renal disease. Journal of Nursing Research, 24(2), 101–108. doi:https://doi.org/10.1097/jnr.0000000000000100
- Chilcot, J., Norton, S., Wellsted, D., Davenport, A., Firth, J., & Farrington, K. (2013). Distinct depression symptom trajectories over the first year of dialysis: Associations with illness perceptions. Annals of Behavioral Medicine, 45(1), 78–88. doi:https://doi.org/10.1007/s12160-012-9410-5
- Clarkson, K. A., & Robinson, K. (2010). Life on dialysis: A lived experience. Nephrology Nursing Journal : Journal of the American Nephrology Nurses’ Association, 37(1), 29–35.
- Creswell, J. W., & Creswell, J. D. (2018). Research design: Qualitative, quantitative, and mixed methods approaches. Newbury Park: Sage.
- Cukor, D., Coplan, J., Brown, C., Peterson, R. A., & Kimmel, P. L. (2008). Course of depression and anxiety diagnosis in patients treated with hemodialysis: A 16-month follow-up. Clinical Journal of the American Society of Nephrology : CJASN, 3(6), 1752–1758. doi:https://doi.org/10.2215/CJN.01120308
- Denoual, H., Dargentas, M., Roudaut, S., Balez, R., & Sizun, J. (2016). Father’s role in supporting breastfeeding of preterm infants in the neonatal intensive care unit: A qualitative study. BMJ Open, 6(6), e010470. doi:https://doi.org/10.1136/bmjopen-2015-010470
- Desseix, A. (2011). ‘L’hémodialyse, cette maladie’. Approche anthropologique d’un amalgame. Sciences Sociales et Santé, 29(3), 41–74.
- Edwards, T., & Holtzman, N. S. (2017). A meta-analysis of correlations between depression and first person singular pronoun use. Journal of Research in Personality, 68, 63–68. doi:https://doi.org/10.1016/j.jrp.2017.02.005
- Farrokhi, F., Abedi, N., Beyene, J., Kurdyak, P., & Jassal, S. V. (2014). Association between depression and mortality in patients receiving long-term dialysis: A systematic review and meta-analysis. American Journal of Kidney Diseases, 63(4), 623–635.
- Fukuhara, S., Lopes, A. A., Bragg-Gresham, J. L., Kurokawa, K., Mapes, D. L., Akizawa, T., … Held, P. J. (2003). Health-related quality of life among dialysis patients on three continents: The dialysis outcomes and practice patterns study. Kidney International, 64(5), 1903–1910. doi:https://doi.org/10.1046/j.1523-1755.2003.00289.x
- Gilman, E. A., Feely, M. A., Hildebrandt, D., Edakkanambeth Varayil, J., Chong, E. Y., Williams, A. W., & Mueller, P. S. (2017). Do patients receiving hemodialysis regret starting dialysis? A survey of affected patients. Clinical Nephrology, 87(3), 117–123. doi:https://doi.org/10.5414/CN109030
- Guzmán-Osorio, G. M., Chávez-Vallejo, S. L., Monzerrat Silvat, G., Parrello, S., & Ioro, I. (2017). Partners of patients with a chronic disease: Narrative enquiry of hemophilia. Revista Electrónica de Psicología Iztacala, 20(2), 548–569.
- Haute Autorité de Santé [HAS]. (2017). Dialyse péritonéale et hémodialyse: Informations comparatives.
- Jansen, D. L., Rijken, M., Kaptein, A. A., Boeschoten, E. W., Dekker, F. W., & Groenewegen, P. P. (2014). The role of social support in dialysis patients’ feelings of autonomy and self-esteem: Is support more beneficial for patients with specific illness perceptions? Families, Systems, & Health, 32(3), 313–327. doi:https://doi.org/10.1037/fsh0000028
- Karamanidou, C., Weinman, J., & Horne, R. (2014). A qualitative study of treatment burden among haemodialysis recipients. Journal of Health Psychology, 19(4), 556–569. doi:https://doi.org/10.1177/1359105313475898
- Kim, M.-H., Kim, Y. C., Lee, J. P., Kim, H., Kim, D. K., Ryu, D.-R., … Kim, Y. S. (2017). Three-year income trends in Korean adults commencing hemodialysis: A prospective cohort. Nephrology. doi:https://doi.org/10.1111/nep.13065
- Lai, A. Y., Loh, A. P. P., Mooppil, N., Krishnan, D. S. P., & Griva, K. (2012). Starting on haemodialysis: A qualitative study to explore the experience and needs of incident patients. Psychology, Health & Medicine, 17(6), 674–684. doi:https://doi.org/10.1080/13548506.2012.658819
- Lebart, L., Salem, A., & Berry, L. (1997). Exploring textual data. Berlin: Springer Science & Business Media.
- Lejeune, C. (2010). Montrer, calculer, explorer, analyser. Ce que l’informatique fait (faire) à l’analyse qualitative. 18.
- Lelorain, S., Tessier, P., Florin, A., & Bonnaud-Antignac, A. (2012). Posttraumatic growth in long term breast cancer survivors: Relation to coping, social support and cognitive processing. Journal of Health Psychology, 17(5), 627–639. doi:https://doi.org/10.1177/1359105311427475
- Lindsay, H., MacGregor, C., & Fry, M. (2014). The experience of living with chronic illness for the haemodialysis patient: An interpretative phenomenological analysis. Health Sociology Review, 23(3), 232–241. doi:https://doi.org/10.1080/14461242.2014.11081976
- Lopez Revuelta, K., Garcia Lopez, F. J., de Alvaro Moreno, F., & Alonso, J. (2004). Perceived mental health at the start of dialysis as a predictor of morbidity and mortality in patients with end-stage renal disease (CALVIDIA study). Nephrology Dialysis Transplantation, 19(9), 2347–2353. doi:https://doi.org/10.1093/ndt/gfh392
- Makaroff, K. L. S. (2012). Experiences of kidney failure: A qualitative meta-synthesis. Nephrology Nursing Journal, 39(1), 21–30.
- Molzahn, A., & Butera, E. (2006). Contemporary nephrology nursing: Principles and practice.
- Monaro, S., Stewart, G., & Gullick, J. (2014). A ‘lost life’: Coming to terms with haemodialysis. Journal of Clinical Nursing, 23(21–22), 3262–3273. doi:https://doi.org/10.1111/jocn.12577
- Moscato, A., & Varescon, I. (2018). Satisfaction and difficulties of French professional home caregivers in supporting older people with Alzheimer’s disease or alcohol misuse. Health & Social Care in the Community, 26(1), 27–34. doi:https://doi.org/10.1111/hsc.12457
- National Institutes of Health [NIH]. (2017). United States renal data system annual data report.
- Paillé, P., & Mucchielli, A. (2016). L’Analyse qualitative en Sciences humaines et sociales. Malakoff: Armand Colin.
- Palmer, S. C., Hanson, C. S., Craig, J. C., Strippoli, G. F. M., Ruospo, M., Campbell, K., … Tong, A. (2015). Dietary and fluid restrictions in CKD: A thematic synthesis of patient views from qualitative studies. American Journal of Kidney Diseases : The Official Journal of the National Kidney Foundation, 65(4), 559–573. doi:https://doi.org/10.1053/j.ajkd.2014.09.012
- Plantinga, L. C., Fink, N. E., Sadler, J. H., Levey, A. S., Levin, N. W., Rubin, H. R., … Powe, N. R. (2004). Frequency of patient-physician contact and patient outcomes in hemodialysis care. Journal of the American Society of Nephrology : JASN, 15(1), 210–218. doi:https://doi.org/10.1097/01.ASN.0000106101.48237.9D
- Radley, A. (2002). Worlds of illness. London: Routledge.
- Ratinaud, P., & Marchand, P. (2012). Application de la méthode ALCESTE aux « gros » corpus et stabilité des « mondes lexicaux »: Analyse du « CableGate » avec IRAMUTEQ. 10.
- Razavi, D., Delvaux, N., Farvacques, C., & Robaye, E. (1989). Validation de la version française du H.A.D.S. dans une population de patients cancéreux hospitalisés. Revue de Psychologie Appliquée (Paris), 39(4), 295–307.
- Reid, C., Seymour, J., & Jones, C. (2016). A thematic synthesis of the experiences of adults living with hemodialysis. Clinical Journal of the American Society of Nephrology, 11(7), 1206–1218. doi:https://doi.org/10.2215/CJN.10561015
- Reinert, M. (1983). Une méthode de classification descendante hiérarchique: Application à l’analyse lexicale par contexte. Les Cahiers de L’Analyse Des Données, 8(2), 187–198.
- Reinert, M. (1990). Alceste une méthodologie d’analyse des données textuelles et une application: Aurelia De Gerard De Nerval. Bulletin de Méthodologie Sociologique, 26. doi:https://doi.org/10.1177/075910639002600103
- Reinert, M. (1993). Les ‘mondes lexicaux’ et leur ‘logique” à travers l’analyse statistique d’un corpus de récits de cauchemars. Langage & Société, 66(1), 5–39. doi:https://doi.org/10.3406/lsoc.1993.2632
- Robinson, B. M., Zhang, J., Morgenstern, H., Bradbury, B. D., Ng, L. J., McCullough, K. P., … Pisoni, R. L. (2014). Worldwide, mortality risk is high soon after initiation of hemodialysis. Kidney International, 85(1), 158–165. doi:https://doi.org/10.1038/ki.2013.252
- Rodin, G. (1994). Depression in patients with end-stage renal disease: Psychopathology or normative response? Advances in Renal Replacement Therapy, 1(3), 219–227. doi:https://doi.org/10.1016/S1073-4449(12)80004-5
- Rubin, H. R., Jenckes, M., Fink, N. E., Meyer, K., Wu, A. W., Bass, E. B., … Powe, N. R. (1997). Patient’s view of dialysis care: Development of a taxonomy and rating of importance of different aspects of care. American Journal of Kidney Diseases, 30(6), 793–801. doi:https://doi.org/10.1016/S0272-6386(97)90084-6
- Schell, J. O., Patel, U. D., Steinhauser, K. E., Ammarell, N., & Tulsky, J. A. (2012). Discussions of the kidney disease trajectory by elderly patients and nephrologists: A qualitative study. American Journal of Kidney Diseases, 59(4), 495–503. doi:https://doi.org/10.1053/j.ajkd.2011.11.023
- Stringer, S., & Baharani, J. (2012). Why did I start dialysis? A qualitative study on views and expectations from an elderly cohort of patients with end-stage renal failure starting haemodialysis in the United Kingdom. International Urology and Nephrology, 44(1), 295–300. doi:https://doi.org/10.1007/s11255-011-0045-4
- Tan, E. G. F., Teo, I., Finkelstein, E. A., & Meng, C. C. (2019). Determinants of regret in elderly dialysis patients. Nephrology, 24(6), 622–629. doi:https://doi.org/10.1111/nep.13400
- Thomas, D. R. (2006). A general inductive approach for analyzing qualitative evaluation data. American Journal of Evaluation, 27(2), 237–246. doi:https://doi.org/10.1177/1098214005283748
- Trifu, R. N., Nemes, B., Bodea-Hațegan, C., & Cozman, D. (2017). Linguistic indicators of language in major depressive disorder (MDD). An evidence based research. Journal of Evidence-Based Psychotherapies, 17(1), 105–128. doi:https://doi.org/10.24193/jebp.2017.1.7
- Untas, A., Aguirrezabal, M., Chauveau, P., Leguen, E., Combe, C., & Rascle, N. (2009). Anxiété et dépression en hémodialyse: Validation de l’Hospital Anxiety and Depression Scale (HADS). Nephrologie et Therapeutique, 5(3), 193–200. doi:https://doi.org/10.1016/j.nephro.2009.01.007
- Untas, A., Rascle, N., Idier, L., Lasseur, C., & Combe, C. (2012). Family relations, mental health and adherence to nutritional guidelines in patients facing dialysis initiation. Psychology & Health, 27(7), 753–766. doi:https://doi.org/10.1080/08870446.2011.574699
- Untas, A., Thumma, J., Rascle, N., Rayner, H., Mapes, D., Lopes, A. A., … Combe, C. (2011). The associations of social support and other psychosocial factors with mortality and quality of life in the dialysis outcomes and practice patterns study. Clinical Journal of the American Society of Nephrology : CJASN, 6(1), 142–152.
- van Manen, J. G., Korevaar, J. C., Dekker, F. W., Reuselaars, M. C., Boeschotem, E. W., & Krediet, R. T. (2001). Changes in employment status in end-stage renal disease patients in their first year of dialysis. Peritoneal Dialysis International, 21(6), 595–601.
- Vigneau, C., Kolko, A., Stengel, B., Jacquelinet, C., Landais, P., Rieu, P., … Couchoud, C. (2017). Ten-years trends in renal replacement therapy for end-stage renal disease in mainland France: Lessons from the French Renal Epidemiology and Information Network (REIN) registry. Nephrologie et Therapeutique, 13(4), 228–235. doi:https://doi.org/10.1016/j.nephro.2016.07.453
- Watnick, S., Kirwin, P., Mahnensmith, R., & Concato, J. (2003). The prevalence and treatment of depression among patients starting dialysis. American Journal of Kidney Diseases, 41(1), 105–110. doi:https://doi.org/10.1053/ajkd.2003.50029
- Xhulia, D., Gerta, J., Dajana, Z., Koutelekos, I., Vasilopoulou, C., Skopelitou, M., & Polikandrioti, M. (2015). Needs of hemodialysis patients and factors affecting them. Global Journal of Health Science, 8(6), 109–120. doi:https://doi.org/10.5539/gjhs.v8n6p109
- Yoong, R., Mooppil, N., Khoo, E., Newman, S., Lee, V., Kang, A. W. C., & Griva, K. (2017). Prevalence and determinants of anxiety and depression in end stage renal disease (ESRD). A comparison between ESRD patients with and without coexisting diabetes mellitus. Journal of Psychosomatic Research, 94, 68–72. doi:https://doi.org/10.1016/J.JPSYCHORES.2017.01.009
- Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. doi:https://doi.org/10.1111/j.1600-0447.1983.tb09716.x