ABSTRACT
This study assessed the validity and reliability of the Pandemic Coping Scale (PCS), a new brief measure of coping with pandemic-related stressors.
Methods
The PCS was administered to N = 2316 German participants during the COVID-19 pandemic. Exploratory and confirmatory factor analysis was applied among random splits of the sample. Global goodness of fit (χ2, RMSEA, SRMR, CFI, TLI), local goodness of fit (factor loadings, communalities, factor reliability, discriminant validity) and additional test quality criteria (internal consistency, item discrimination and difficulty) were evaluated for a four-factor model vs. a four-factor model combined with a second-order general factor. Convergent and divergent validity were examined by Pearson correlations of the PCS subscales with the Brief-COPE subscales; criterion validity was evaluated by correlations with wellbeing (WHO-5), depressive (PHQ-9) and anxiety symptoms (GAD-2).
Results
Exploratory factor analysis suggested a four-factor solution (‘Healthy Lifestyle’, ‘Joyful Activities’, ‘Daily Structure’, ‘Prevention Adherence’). Confirmatory factor analysis showed a sufficient global fit for both specified models which did not differ in their fit to the data. Local goodness of fit indices showed moderate to large factor loadings and good factor reliabilities except for the subscale ‘Prevention Adherence’. Internal consistencies were good for the PCS total scale (α = .83), the ‘Healthy Lifestyle’ (α = .79) and the ‘Daily Structure’ (α = .86) subscales, acceptable for ‘Joyful Activities’ (α = .60), and low for ‘Prevention Adherence’ (α = .52). The four subscales evidenced convergent and divergent validity with the Brief-COPE subscales. The subscales ‘Healthy lifestyle’, ‘Joyful activities’ and ‘Daily structure’ showed criterion validity with wellbeing, depressive and anxiety symptoms.
Conclusions
The PCS is a reliable and valid measure to assess pandemic-specific coping behavior in the domains of ‘Healthy Lifestyle’, ‘Joyful Activities’, and ‘Daily Structure’. The PCS subscale ‘Prevention Adherence’ might be improved by adding items with varying item difficulties.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is related to multiple stressors that impact the wellbeing of whole populations (Aknin et al., Citation2022). In addition to the burden of a COVID-19 infection, the lockdowns had a drastic impact on everyday life. Social physical contacts, such as friends and family gatherings, have become rare. Structuring the work and daily activities when working from home have become challenging (Chirico et al., Citation2021; Platts, Breckon, & Marshall, Citation2022). Physical activities like cycling to work have been restricted, leisure opportunities such as going to the sports club have become impossible. At the same time, activities like watching television and sitting in front of the computer have increased (Kowalsky, Farney, Kline, Hinojosa, & Creasy, Citation2021, june 23; Ong et al., Citation2020). Being at home most of the time may have promoted unhealthy eating habits (Bennett, Young, Butler, & Coe, Citation2021) and alcohol use (Acuff, Strickland, Tucker, & Murphy, Citation2022; Schmidt et al., Citation2021). The reduced social contact increased distress, loneliness, and anxiety (Beutel et al., Citation2021). To reduce psychological distress from a pandemic, it is important to understand the coping strategies people use to deal with pandemic-specific stressors and which of these strategies promote well-being.
Coping can be defined as ‘the person’s constantly changing cognitive and behavioral efforts to manage specific external or internal demands that are appraised as taxing or exceeding the person’s resources’ (Folkman, Lazarus, Dunkel-Schetter, DeLongis, & Gruen, Citation1986). The term coping usually refers to adaptive coping strategies, i.e. strategies that reduce distress and promote wellbeing and health (Taylor & Stanton, Citation2007). Engaging in exercising in response to a stressful situation might be seen as adaptive coping, as it may reduce distress and increase wellbeing. However, some coping strategies may increase distress, and in turn may be considered maladaptive. For example, smoking in response to a stressful situation could be seen as maladaptive, as it may increase distress and can harm health.
Coping with multiple pandemic-related stressors requires specific coping skills, such as adhering to physical distancing measures, establishing or adhering healthy lifestyle habits and daily structure, or actively seeking social support. Research conducted during the early phase of the COVID-19 pandemic found associations between coping and reduced anxiety and depression symptoms (Fullana, Hidalgo-Mazzei, Vieta, & Radua, Citation2020). Establishing a daily routine, following a healthy diet, and taking the opportunity to pursue hobbies were most strongly related to lower depressive symptoms (Fullana et al., Citation2020). In a general population study on relationships between coping and mental health (Shamblaw, Rumas, & Best, Citation2021), active coping and positive reframing were related to lower levels of depressive symptoms and a perceived higher quality of life.
To assess coping with the specific stressors during a pandemic or epidemic, a valid and reliable measure is needed that considers the specific demands of this extraordinary situation. According to a recently conducted meta-analysis (Kato, Citation2015), the most often used coping measures applied outside of pandemics or epidemics were the Coping Orientation to Problems Experienced (COPE; Carver, Scheier, & Weintraub, Citation1989), the Brief-COPE (Carver, Citation1997), and the Ways of Coping Questionnaire (WCQ; Folkman & Lazarus, Citation1988). During the COVID-19 pandemic, the 60-item COPE (Carver et al., Citation1989) has rarely been used, as its length makes it less feasible for online-based assessments that are required during a lockdown.
The Brief-COPE was applied during the COVID-19 pandemic in the general population (Kavčič, Avsec, & Zager Kocjan, Citation2022; Zacher & Rudolph, Citation2021) and among at-risk groups such as students (El-Monshed, El-Adl, Ali, & Loutfy, Citation2022; Sheroun et al., Citation2020). A study among students (El-Monshed et al., Citation2022) found negative associations between problem-focused coping and psychological distress, as well as positive correlations between dysfunctional coping and distress. In a general population study conducted during the early phase of the COVID-19 pandemic (Zacher & Rudolph, Citation2021), active coping, positive reframing, seeking emotional support, and religion were related to wellbeing. Unexpectedly, the two coping domains planning and humor, usually perceived as adaptive, were associated with reduced wellbeing; these coping strategies might be less adaptive during a pandemic compared to non-pandemic situations. The 66-item WCQ (Folkman & Lazarus, Citation1988) measures problem-focused and emotion-focused strategies. The WCQ has been applied in a few studies during the early phase of the COVID-19 pandemic (Özçevik Subaşi, Akça Sümengen, Şimşek, & Ocakçı, Citation2021; Salopek-Žiha et al., Citation2020). A study comparing coping of physicians and nurses found that physicians used more problem-focused strategies, while nurses used more emotion-focused strategies (Salopek-Žiha et al., Citation2020). The psychometric evaluation of the WCQ reveiled an instable factor structure (Edwards & O’Neill, Citation1998; Parker, Endler, & Bagby, Citation1993) and heterogenous internal consistencies (Lundqvist & Ahlström, Citation2006; Rexrode, Petersen, & O’Toole, Citation2008). The WCQ has been criticized to measure behavior that does not target coping with specific stressors (Ben-Porath, Waller, & Butcher, Citation1991; Stone, Greenberg, Kennedy-Moore, & Newman, Citation1991). The 48-item Coping Inventory for Stressful Situations (CISS; Endler & Parker, Citation1990, Citation1999) has been used in a few studies during the COVID-19 pandemic to measure task-, emotion- and avoidance-oriented coping during the COVID-19 pandemic. Reliability and validity of the CISS have been established (Cohan, Jang, & Stein, Citation2006; McWilliams, Cox, & Enns, Citation2003). A study using the CISS demonstrated associations between task-oriented coping and reduced levels of burnout symptoms (Di Monte, Monaco, Mariani, & Di Trani, Citation2020). Another study (Rogowska, Kuśnierz, & Bokszczanin, Citation2020) reported an unexpected positive association between task-oriented coping and anxiety symptoms. This unexpected result could be pandemic-specific, since the usual behaviors to cope with everyday stressors might lead to frustration when the situation cannot be changed (Rogowska et al., Citation2020).
In sum, several coping measures exist of which some have been used to investigate coping during the current COVID-19 pandemic. The BRIEF-COPE and the CISS have been most often used. While the findings of these studies indicate relationships between coping and relevant mental health variables such as wellbeing (Kavčič et al., Citation2022; Zacher & Rudolph, Citation2021), depression and anxiety (Rogowska et al., Citation2020), these measures have not been designed to assess coping within the specific context of a pandemic. Consequently, some researchers have stressed the need to cover the coping behaviors unique for a pandemic or an epidemic (Rahman, Issa, & Naing, Citation2020) which are not covered by the existing measures. A brief, valid and reliable measure of coping behavior during a pandemic is required that can be used to complement existing coping measures. Therefore, the aim of this study was to take a first step in this direction by assessing factorial, convergent, divergent and criterion validity and reliability of the Pandemic Coping Scale, a new brief measure of coping with stressors relevant in the context of a pandemic.
Materials and methods
Study design
For this psychometric study, cross-sectional data was drawn from the first wave of a longitudinal cohort study on stressors, coping, and symptoms of adjustment disorder during the COVID-19 pandemic (Lotzin et al., Citation2020). The data were assessed between June and September 2020. The psychometric properties of the PCS were evaluated in two separate analyses conducted on two random splits of the sample. The first analysis investigated the dimensional structure of the PCS by exploratory factor analysis (EFA). In a second analysis, we examined whether the identified dimensions could be replicated by using confirmatory factor analysis (CFA). Internal consistency, item discrimination and difficulty, convergent, divergent and criterion validity were also assessed.
Sample
Data were collected from German participants. Eligibility criteria were (1) an age of at least 18 years, and (2) the ability to understand German language. The trial was actively promoted via the internet (e.g. eBay advertisements, Facebook, interest groups), leisure and sports clubs, large companies, and clubs of senior citizens. After being informed about the study and willing to participate, participants filled out an online questionnaire. A total of N = 2316 participants agreed to take part in the survey and filled out the questions of the Pandemic Coping Scale (PCS). Ethics approval was provided by the Local Psychological Ethics Committee at the Center for Psychosocial Medicine (LPEK) at University Medical Center Hamburg-Eppendorf (LPEK-0149).
Development of the PCS
The Pandemic Coping Scale (PCS, Appendix 6) was designed as a brief self-report measure to assess coping behavior to stressors of a pandemic. The first set of items was constructed after reviewing the scientific literature on measures of coping with stressors (please see summary of measures in the introduction), the published recommendations on how to cope with daily stressors relevant for the COVID-19 pandemic (American Medical Association, Citation2020; Center for the Study of Traumatic Stress, Citation2020; Centers for Disease Control and Prevention, Citation2020; World Health Organization, Citation2020), and the research evidence on life style factors related to mental health (Walsh, Citation2011). Six domains of behavior that were likely to be affected by a pandemic or epidemic and have shown to be related to mental health (Walsh, Citation2011) were selected: preventive adherence (e.g. following the recommendations to limit the spread of the coronavirus); health lifestyle (e.g. paying attention to a healthy diet); rest (e.g. taking breaks); meaningful activities (e.g. doing something enjoyable); daily structure (e.g. maintain daily routine.); and social support (e.g. spending a good time with loved ones, friends, or pet). The domains covered by the Brief-COPE were excluded (e.g. religious involvement), so that the PCS could be used as a pandemic-specific measure in addition to this established measure. The first item set was constructed by a clinical psychologist. Items were then reviewed and refined by consensus of an expert group of professionals in the field of traumatic stress, which were members of the European Society of Traumatic Stress Studies (Lotzin et al., Citation2020). The resulting first version of the PCS included thirteen four-point items representing coping behaviors in the six identified domains. The item scaling and scoring was harmonized with the Brief-COPE. The item scores ranged from 0 to 3 (0 = ‘I have not been doing this at all’; 1 = ‘I’ve been doing this a little bit’; 2 = ‘I’ve been doing this a medium amount’; 3 = ‘I’ve been doing this a lot’). Higher scores indicated doing more of the respective behavior. Completion of the questionnaire requires about five minutes. Sociodemographic characteristics were assessed by self-constructed items (e.g. gender, age, education, household income).
Additional measures
To evaluate convergent, divergent and criterion validity of the PCS, general coping with stressors (Brief-COPE), wellbeing (WHO-5), depressive (Patient Health Questionniare, PHQ-9) and anxiety symptoms (GAD-2) were assessed.
Coping behavior
General coping was measured using the Brief-COPE (Carver, Citation1997; Knoll, Rieckmann, & Schwarzer, Citation2005). The Brief-COPE captures 14 coping strategies (Active coping, planning, instrumental support, emotional support, positive reinterpretation, acceptance, humor, and religion as functional coping strategies; and distraction, venting, self-blame, behavioral disengagement, denial, and substance use as dysfunctional coping strategies) by 28 items on four-point Likert scales (0 = ‘I have not been doing this at all’ to 3 = ‘I’ve been doing this a lot’). The Brief-COPE has indicated good psychometric properties, including good internal consistencies (Cooper, Katona, & Livingston, Citation2008) and convergent, divergent validity (Kato, Citation2015).
Well-Being
Well-being was measured using the five-item WHO Well-Being Index (WHO-5; Bech, Olsen, Kjoller, & Rasmussen, Citation2003). Respondents rated aspects of well-being within the last two weeks on six-point scales (0 = ‘At no time’ to 5 = ‘All the time’). A total score can be computed, higher values reflect higher well-being. The WHO-5 showed good psychometric properties, including good internal consistencies (Brähler, Mühlan, Albani, & Schmidt, Citation2007).
Depressive and anxiety symptoms
The five-item Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, Citation2001) was used to assess depressive symptoms. Respondents rate on four-point scales (0 = ‘not at all’ to 3 = ‘nearly every day’) whether they experienced symptoms of fatigue, loss of appetite or negative thoughts related to depression within the last two weeks. The PHQ-9 has shown criterion and construct validity (Kroenke et al., Citation2001). Anxiety symptoms were assessed with the GAD-2 (Kroenke, Spitzer, Williams, Monahan, & Löwe, Citation2007), a short two-item measure of anxiety symptoms based on the GAD-7 (Spitzer, Kroenke, Williams, & Löwe, Citation2006). Respondents rate anxiety symptoms within the last two weeks on two four-point scaled items (0 = ‘not at all’ to 3 = ‘almost every day’). The measure has shown convergent validity with the GAD-7 (Kroenke et al., Citation2007).
Data analysis
The psychometric properties of the PCS were evaluated in two separate series of analyses that were conducted in two random splits of our dataset of N = 2316 of participants, using the random generator of SPSS 22.0. The first sample was used to investigate the dimensional structure of the PCS by exploratory factor analysis (EFA). The second sample was used to examine whether the identified dimensions could be replicated by using confirmatory factor analysis (CFA). Additional test quality criteria, as well as convergent, divergent and criterion validity were also examined in the second sample.
Sample 1
Exploratory factor analysis
A sample of n = 1144 participants was used for EFA. The EFA was done following current recommendations on conducting EFA (Samuels, Citation2017). Before conducting the EFA, the bivariate correlation matrix of all PCS items was computed and inspected to detect problems with multicollinearity. The strength of correlations was determined based on Cohen’s criteria (Cohen, Citation1988): low: r = ±.10 to .29, moderate: r = ±.30 to .49, large: r = ±.50 to 1.0. Bivariate correlations of greater than r = .80 were assumed to indicate multicollinearity problems. For correlations r > .80, one of the two items was removed.
Scales were extracted based on an EFA using Maximum Likelihood (ML) as the extraction method, as this method is recommended when measures are developed to be used with other datasets in the future (Field, Citation2013). An oblimin rotation with Kaiser normalization was applied. Items with communalities of less than .20 were removed, and the EFA was re-run. The optimal number of factors was determined by the following criteria: (1) Kaiser’s criterion (eigenvalue > 1); (2) a solution of a maximum number of factors with at least two items with a loading greater than .40 and a low cross-loading. Items with factor loadings < .30 and/or cross-loadings > 75% were removed, starting with the one with the lowest absolute maximum loading on all the factors. The analyses were conducted in SPSS 22.0.
Sample 2
Confirmatory factor analysis
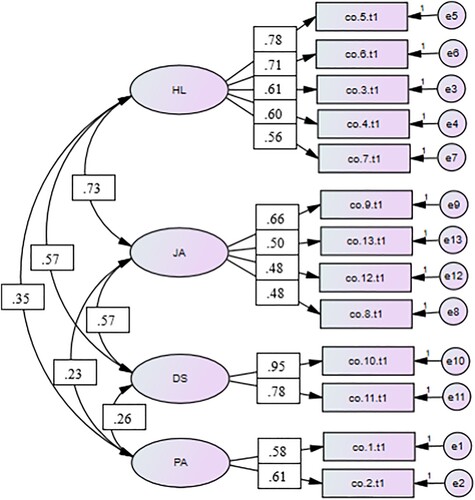
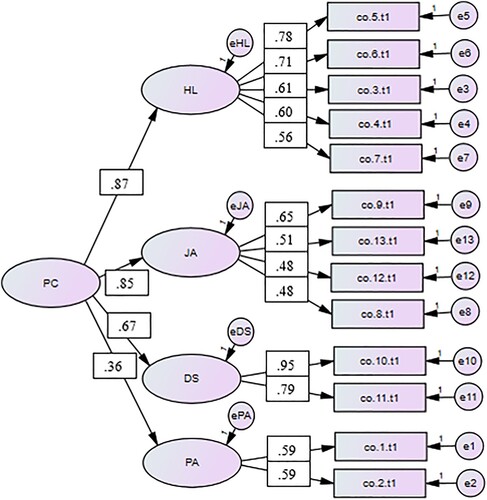
A sample of N = 1172 participants was used to conduct a CFA to test the factorial validity of the factor model obtained by the EFA. The analyses were conducted in SPSS 22.0 and AMOS. Based on the results of the EFA, two models were tested. Model 1 consisted of the 13 items as indicators for four latent factors (). Correlations between factors were expected and allowed. To examine whether all factors load on one general factor, Model 1 was extended in Model 2 by adding a second-order general factor on which the four first-order factors loaded ().
Figure 2. Factor loadings of Model 2 consisting of four first-order factors and a second-order general factor.
A CFA using the ML estimation method was applied. Normal distribution of the items as a prerequisite for ML estimations was evaluated using the skew- (γ1) and kurtosis index (γ2). |γ1| ≥ 3.0 and |γ2| ≥ 10.0 were considered as problematic (Kline, Citation2015, pp. 76–77).
Global Goodness of Fit. Based on the recommendations of Schermelleh-Engel, Moosbrugger, and Müller (Citation2003), the following cut-offs and indices were used for model evaluation: χ2 statistics and normed χ2 (χ2/df): ≤ 3 acceptable, ≤ 2 good; Root Mean Square Error of Approximation (RMSEA): ≤ .08 acceptable, ≤ .05 good; Standardized Root Mean Residual (SRMR): ≤ .10 acceptable, ≤ .05 good. The Tucker Lewis Index (TLI) and Comparative Fit Index (CFI): > .92 acceptable, according to the recommendations of Hair, Black, Babin, and Anderson (Citation2019), taking the large sample size and model complexity into account.
Local Goodness of Fit. Local fit indices were used to assess how reliable the indicators measured the latent constructs. Factor loadings of λ ≥ .50 were rated as moderate, loadings of λ ≥ .70 were rated as large (Hair et al., Citation2019). The Critical Ratio (C.R.) of ≥ |1.96| was used to assess their statistical significance. Factor communalities were considered as acceptable with λ2 ≥ .50 (Hair et al., Citation2019).
On the level of the factors, factor reliabilities (FR) were computed, with FR > .60 assumed as sufficient (Bagozzi & Yi, Citation1988). Discriminant validity was determined using the Fornell-Larcker criterion that compares the Average Variance Extracted (AVE) with the coefficient of determination (AVE > R2 of two factors; Fornell & Larcker, Citation1981).
Model Comparison. A chi-square difference test was applied to compare the fit of Model 1 and Model 2 (Δχ2 = χ2 Model 2 – χ2 Model 1 and Δdf = df Model 2 – df Model 1; Kline, Citation2015, p. 281). Because chi-square tests tend to be oversensitive in large samples (Hair, Citation2010), a conservative significance level of α = .01 was chosen.
Additional test quality criteria
The item difficulties were calculated by the mean of the items divided by the maximum item score (assumed as good if .20 ≤ P ≤ .80; Kline, Citation2013). The corrected item-total correlations was estimated as a measure of item discrimination (rit ≥ .30 rated as acceptable and rit ≥ .50 as good; Krohne et al. (Citation2007), p. 52). To evaluate internal consistency for the PCS total scale and subscales, Cronbach's α coefficients were calculated, except for the ‘Daily Structure’ and ‘Prevention Adherence’ subscales for which the Spearman-Brown coefficient was used as recommended for two-item scales (Eisinga, te Grotenhuis, & Pelzer, Citation2013).
Convergent, divergent and criterion validity
To assess convergent and divergent validity of the PCS, Pearson Product-Moment Correlation coefficients were calculated between the subscales of the PCS and the Brief-COPE. To assess concurrent criterion validity, Pearson Product-Moment Correlation coefficients were calculated between the PCS subscales and wellbeing (WHO-5), depressive symptoms (PHQ-9) and anxiety symptoms (GAD-2).
Results
Sample 1
Exploratory factor analysis
The sample included n = 1144 German adults from the general public (). The sample can be characterized as a medium to high-educated sample with varying age and income. Ages ranged between 18 and 82 years, with a mean age of 41.17 (SD = 12.79). More participants were female (n = 811, 70.9%) than male (n = 327, 28.6%), or of diverse gender (n = 6, 0.5%). Only few participants (n = 4, 0.35%) reported less than ten years of schooling; 12.8% (n = 146) completed up to thirteen years of schooling as highest education; 35.1% (n = 402) completed vocational training; 48.2% (n = 551) graduated university; and 3.58% (n = 41) completed a doctorate. One fifth of the sample (n = 251, 21.9%) classified themselves as being at risk for severe or life-threatening symptoms of COVID-19. One fifth (n = 268, 23.4%) stated to have been diagnosed with a mental disorder, of whom 8.0% (n = 92) reported to be affected by a mental disorder at the time of the assessment.
Table 1. Sociodemographic characteristics of the two study samples.
Intercorrelations ranged from r −.001 to .76. As no correlation exceeded the threshold of .80, all items were retained in the analysis. The communalities of the initial solution were greater than .20 for all items, indicating that all items could be used. The means, standard deviations and indices for skewness and kurtosis for the items are shown in . All items were approximately normally distributed, although some items showed a negative skew.
Table 2. Means, standard deviations and factor loadings for the items of the pandemic coping scale (Exploratory factor analysis, n = 1144).
The results of the EFA suggested a four-factor solution (). The factor solution was also confirmed by visual examination of the scree plot. No additional factor exceeded the threshold of an Eigenvalue of 1.0. All items had loadings > .40 on the respective factor. The four factors were named (1) ‘Healthy Lifestyle’, (2) ‘Joyful Activities’, (3) ‘Daily Structure’, and (4) ‘Prevention Adherence’. The factors accounted for 25.2% (Daily Structure), 10.8% (Healthy Lifestyle), 4.3% (Joyful Activities), and 4.4% (Prevention Adherence) of the total variance, respectively. The factor correlations ranged from r = .20 (Joyful Activities with Prevention Adherence) to r = .58 (Healthy Lifestyle with Joyful Activities). In the four-factor solution, each item had a salient loading on only one factor. No item of the rotated factor matrix cross-loaded more than 75% on another factor. The factor loadings of the 13 items ranged between .39 and .94, suggesting meaningful and practically significant factor loadings (Cudeck & O’Dell, Citation1994).
Of the six pandemic coping domains that were specified prior to the analysis (please see Measure section), the domains ‘Healthy Lifestyle’, ‘Daily Structure’, and ‘Prevention Adherence’ were identified as single factors in the EFA. The two previously specified domains ‘Meaningful Activities’ and ‘Social Activities’ loaded on one common factor, which was named ‘Joyful Activities’. The two items of the previously specified domain ‘Resting’ loaded on the ‘Healthy Lifestyle’ factor.
Sample 2
Confirmatory factor analysis
The sample included n = 1172 German adults (). The sample characteristics were similar to those of the sample used for the exploratory factor analysis and can be characterized as a medium to high-educated sample with varying age and income. Mean age was 41.19 (SD = 13.1), which ranged from 18 to 80 years. The majority of the sample was female (n = 813, 69.4%), the remaining participants were male (n = 355, 30.3%) or of diverse gender (n = 4, 0.3%). Only 0.3% (n = 3) of the sample completed less than nine years of schooling. The remaining participants completed up to thirteen years of schooling (n = 138, 11.8%), passed a vocational training (n = 416, 35.5%), graduated from university (n = 572, 48.8%) or completed a doctorate (n = 43, 3.7%). One fifth of the sample (n = 253, 21.6%) classified themselves as being at risk for severe or life-threatening symptoms of the coronavirus disease. 23.2% (n = 272) reported being diagnosed with a mental disorder; and 8.0% (n = 94) stated to be currently affected by a mental disorder. All indicators were approximately normally distributed (skew index │γ1│< 3.0 and kurtosis index |γ2| < 10.0; Appendix 1; Kline, Citation2015, pp. 76–77).
Model 1
Global Goodness of Fit. The χ2 statistics suggested a discrepancy between the theoretical model and the model implied by the observed data (χ2 (59, n = 1172) = 367, p < .001, normed χ2 = 6.22, ). The RMSEA showed an acceptable fit (RMSA = .067, p < .001, 90% CI = .060, .073), the SRMR indicated a good fit (SRMR = .043), the CFI (.926) showed an acceptable fit. However, the TLI (.902) indicated an insufficient model fit as it was lower than .92.
Table 3. Global fit indices of the confirmatory factor analysis for Model 1 and Model 2 (Confirmatory factor analysis, n = 1172).
Local Goodness of Fit. Factor loadings were moderate (λ ≥ .50) to large (λ ≥ .70), apart from smaller loadings of three indicators of the factor ‘Joyful Activities’ (Appendix 2). All factor loadings were significant (C.R. ≥ |1.96|). Only four indicators showed communalities λ2 ≥ .50 (items 5, 6, 10 and 11; Appendix 2). The factors mainly showed discriminant validity in terms of a small to medium correlation (ranging from .05 to .33, Appendix 3) except for ‘Healthy Lifestyle’ and ‘Joyful Activities’, which showed a medium correlation (r = .54). Factor reliability was considered as good with FR >.60 for all factors except for ‘Prevention Adherence’ (FR = .52, Appendix 3).
Additional test quality criteria. Item difficulties were considered as good (Appendix 4), except for the indicators of ‘Prevention Adherence’ which showed a low difficulty (P > .80). Item discrimination indices were good (rit > .50) or acceptable (rit > .30). Internal consistency was excellent for the factor ‘Daily Structure’ (α = .86), and moderate for the factor ‘Healthy Lifestyle’ (α = .79). The factors ‘Joyful Activities’ (α = .60) and ‘Prevention Adherence’ (α = .52) showed low internal consistency.
Model 2
Overall, the global and local fit indices and the test quality criteria of Model 2 were similar to those found in Model 1.
Global Goodness of Fit. The χ2 statistic referred to a statistically significant difference between the specific and observed variance-covariance matrix (χ2 (61, N = 1172) = 373.33, p < .001, normed χ2 = 6.12; ). The RMSEA showed an acceptable fit (RMSEA = .066, p < .001, 90% CI = .060, .073), the SRMR showed a good fit (SRMR = .043). While the CFI (.925) indicated an acceptable model fit, the TLI (.904) indicated an insufficient fit, as it was <.92.
Local Goodness of Fit. Factor loadings of the indicators were moderate to large, except for the items 8 and 12 of the factor ‘Joyful Activities’ (Appendix 2). The factor loadings on the second-order general factor (named ‘Pandemic Coping’) were large for ‘Healthy Lifestyle’ (λ = .87) and ‘Joyful Activities’ (λ = .85), moderate for ‘Daily Structure’ (λ = .67) and small for ‘Prevention Adherence’ (λ = .36, Appendix 2). All factor loadings were significant (C.R. ≥ |1.96|). Consistent with Model 1, communalities λ2 ≥ .50 were only found for the items 5, 6, 10 and 11 (Appendix 2). The factor reliabilities could be considered as good for the second-order general factor ‘Pandemic Coping’ (FR = .90) and for all first-order factors (FR>.60) except for ‘Prevention Adherence’ (FR = .52, Appendix 3).
Model comparison
The chi-square difference test comparing Model 1 and Model 2 showed no significant difference in their fit to the data (Δχ2 (2, n = 1172) = 6.36, p = .042).
Additional test quality criteria
Item difficulties were evaluated as good for all indicators (Appendix 4) except for the indicators of ‘Prevention Adherence’, which showed low difficulties (P > .80). Item discrimination indices concerning the second-order general factor ‘Pandemic Coping’ were evaluated as good (rit >.50) or acceptable (rit >.30), except for the indicators of ‘Prevention Adherence’. The internal consistency of the second-order general factor ‘Pandemic Coping’ was acceptable (α = .83). For the internal consistencies of the subscales, please see result section for Model 1.
Convergent, divergent and criterion validity
Correlations between the PCS subscales indicated evidence for their convergent and divergent validity, i.e. showed higher correlations with the Brief-COPE subscales measuring convergent constructs, and lower or no correlations with subscales measuring divergent constructs (Appendix 5). For example, the PCS subscale ‘Healthy lifestyle’ showed the highest correlation with the Brief-COPE subscale ‘Active Coping’, and the lowest correlation with the subscale ‘Denial’. The PCS subscales ‘Healthy lifestyle’, ‘Joyful activities’ and ‘Daily structure’ showed moderate positive correlations with wellbeing (WHO-5), moderate negative correlations with depressive symptoms (PHQ-9), and small negative correlations with anxiety symptoms (GAD-2), indicating their concurrent criterion validity. The PCS subscale ‘Prevention adherence’ did not significantly correlate with wellbeing, depressive or anxiety symptoms, indicating that this subscale were unrelated to these constructs.
Discussion
Coping with the specific stressors of a pandemic may impact physical and psychological health and well-being. This research aimed to assess the validity and reliability of the Pandemic Coping Scale (PCS, Appendix 6), a brief measure of coping with the stressors of a pandemic, in the German general population in two separate samples. In a first sample, we identified underlying factors of the PCS by using exploratory factor analysis (EFA). In a second sample, we examined whether the factor structure identified in the EFA could be replicated using confirmatory factor analysis (CFA). In the CFA, we assessed the global goodness of fit of the factor structure, the local goodness of fit and additional test quality criteria, which were evaluated in two models: a four-factor model, and a four-factor model combined with a second-order general factor. Convergent, divergent and criterion validity were also evaluated.
Factorial validity
The EFA indicated a four-factor solution (‘Healthy Lifestyle’, Joyful Activities’, ‘Daily Structure’ and ‘Prevention Adherence’), which accounted for 44.6% of the total variance. Each of the 13 items of the PCS showed salient and significant factor loadings on only one of the four factors, indicating their factorial validity.
Global fit
The four-factor solution could be replicated by applying CFA in our second sample. Most of the global fit indices (RMSEA, SRMR, CFI) showed a sufficient fit in a model with four separate factors, as well as in a model which additionally included a second-order general factor. However, the χ2 statistics of both models indicated a deviation from the observed model, consistent with earlier research showing that the χ2 test tends to be oversensitive in large samples (Hair et al., Citation2019). The comparison of the two models (four-factor model vs. a four-factor model combined with a second-order general factor) showed no difference in their fit to the data. These results suggest that a second-order general factor seems to be consistent with the data structure and may legitimize the calculation of a total score of the ‘Pandemic Coping Scale’.
Local fit
On the level of the indicators, we found that most of the factor loadings of the two tested factor models were moderate to large, except for some items of the subscale ‘Joyful Activities’. The factor loading of the items of the subscale ‘Prevention Adherence’ on the second-order general factor were also lower. The subscale ‘Joyful Activities’ was initially constructed as two separate domains, but according to our results of the EFA, the constructs of meaningful and social activities overlapped. However, these two domains may still cover separate aspects resulting in increased heterogeneity of the combined scale. This might explain the comparably small factor loadings of the items on ‘Joyful Activities’, but greater factor loadings on the second-order general factor.
On the level of the factors, we found good factor reliabilities for all first-order factors except for ‘Prevention Adherence’ for both tested models. Therefore, the indicators within each factor share enough variance to measure a similar construct. Most factors showed evidence for discriminant validity, demonstrating that the items of the subscales represent distinct constructs. These findings are in line with the results of the EFA which showed that all items loaded highly on only one factor. The subscales ‘Healthy Lifestyle’ and ‘Joyful Activities’ shared variance with each other, implying that they were not fully independent.
Additional test quality criteria
Item difficulty
Our analysis of additional test quality criteria yielded comparable results for both tested factor models for most of the assessed indices. The items of three subscales showed good item difficulties, whereas the items of ‘Prevention Adherence’ were comparably easy in both models. Consequently, this subscale may not perfectly discriminate between people with very high versus high prevention adherence scores. The scale might benefit from additional items with varying difficulties. However, the data assessment for this study took place three to six months of the start of the pandemic. It has become evident that people – after the lockdown has become an enduring condition – are less adherent to the lockdown measures. The reduced prevention adherence behavior which is measured by the subscale is likely to increase the item variance and item difficulty. Future studies using the PCS in the later phases of the pandemic are needed to further examine the item difficulties of this subscale.
Item discrimination and internal consistency
Acceptable indices for item discrimination were found for all items, with one exception: The items of the subscale ‘Prevention Adherence’ did not sufficiently discriminate between high and low scores in the second-order general factor in Model 2. Internal consistency was excellent for ‘Daily Structure’, acceptable for ‘Healthy Lifestyle’, but low for Joyful Activities’ and ‘Prevention Adherence’. Cronbach’s α increases with an increasing number of items per scale (Ponterotto & Ruckdeschel, Citation2007); the low number of indicators of the factor ‘Prevention Adherence’ might have contributed to the low internal consistency. Furthermore, calculations of Cronbach’s α are affected by the total item variance (Streiner, Citation2003). The low difficulties of both items of this scale may have restricted the item variance, which could have contributed to the low internal consistency of the factor ‘Prevention Adherence’. The lower internal consistency of ‘Joyful Activities’ might be attributable to the heterogeneity caused by the inclusion of two formerly separate domains.
Convergent, divergent and criterion validity
Intercorrelations between the four PCS subscales provided evidence for convergent and divergent validity. The PCS subscales ‘Healthy lifestyle’, ‘Joyful activities’ and ‘Daily structure’ subscales showed evidence for criterion validity, based on positive correlations with wellbeing, and negative correlations with depressive and anxiety symptoms, while such correlations could not be established for the PCS subscale ‘Prevention adherence’.
Overall, the findings of our analyses conducted in two different samples provided substantial evidence for the factorial, convergent, divergent and criterion validity, as well as reliability of the three PCS subscales ‘Daily Structure’, ‘Healthy Lifestyle’, and ‘Joyful Activities’. Our analysis also provided some evidence for the validity and reliability of the subscale ‘Prevention Adherence’. However, compared with the other subscales, ‘Prevention Adherence’ showed a lower factor reliability and a lower factor loading on the second-order general factor, lower item discrimination indices concerning the second-order general factor, lower internal consistency, and lower item difficulties. The lower factorial validity and reliability might be explained by a reduced item variance. Most of the conducted calculations are based on variance-covariance matrices; reduced item variance therefore results in lower local and lower global model fit. Alternatively, the items of this subscale might measure content that is less related to the content domains of the other three subscales. While the subscale of ‘Prevention Adherence’ includes behaviors such as informing oneself about the pandemic situation and following the recommendations, the other three subscales of the PCS focus on self-care and social contact. This could explain the smaller factor loading of ‘Prevention Adherence’ and moderate to large factor loadings of the remaining subscales on the second-order general factor. It would also explain why the items of ‘Prevention Adherence’ could distinguish between participants with high and low scores in ‘Prevention Adherence’ but could not distinguish sufficiently between participants with high and low scores in the total score of the PCS. The ‘Prevention Adherence’ scales also showed little evidence for criterion validity, i.e. significant correlations with wellbeing, depressive and anxiety symptoms. Removing the subscale of ‘Prevention Adherence’ might result in a higher internal consistency of the total score of ‘Pandemic Coping’ and would increase the homogeneity of the items. The elimination of both items could improve local and global model fit, as the two items showed reduced item variance. However, the removal of this subscale carries the risk of leaving out an important area of coping behavior that is specific for a pandemic. Alternatively, additional items measuring preventive adherence to the PCS with higher item difficulties could be added to the scale.
While several coping measures exist, these measures have not been developed to assess coping within the specific context of a pandemic. The PCS is a brief coping measure that has been specifically developed during the COVID-19 pandemic to measure coping relevant in the context of a pandemic or an epidemic. The PCS might be used in addition to established coping measures to capture the pandemic-specific coping behavior. The measured coping domains ‘Healthy Lifestyle’, ‘Joyful Activities’, ‘Daily Structure’ and ‘Prevention Adherence’ are likely to be also relevant during future pandemics or epidemics of infectious diseases that require lockdown measures, social isolation, physical distancing, or preventive actions such as wearing face masks (e.g. the SARS 2002–2003 epidemic, Anderson et al., Citation2004).
Research directions
Future studies need to examine the psychometric properties of the PCS among representative samples. The psychometric properties of the questionnaire might be further improved by adding items to the Prevention Adherence subscale and further examining its factorial validity and reliability. The strength and direction of association of the PCS with other measures of coping during a pandemic should be examined. Finally, the appropriateness of the usage of the measure should be also examined in other countries.
Strength and limitations
A strength of this study is the use of sufficiently sized samples, and the combined use of EFA and CFA in two random splits of a large sample to replicate the results obtained in EFA. A limitation is that the sample was not representative for the German general population regarding gender, income and education. The study is also limited by the use of self-report questionnaires that might have led to different results compared to observational measures of coping.
Conclusion
Overall, the findings of our analyses provide substantial empirical support for the validity and reliability of the three subscales ‘Healthy Lifestyle’, ‘Joyful Activities’, ‘Daily Structure’ of the Pandemic Coping Scale. The subscale ‘Prevention Adherence’ might benefit from further adaption and evaluation.
Ethics statement
Ethics approval was provided by the Local Psychological Ethics Committee at the Center for Psychosocial Medicine (LPEK) at University Medical Center Hamburg-Eppendorf (LPEK-0149). All participants provided informed consent before participating. The longitudinal cohort study was registered in a study registry (https://doi.org/10.17605/OSF.IO/8XHYG) before the start of the study.
Consent for publication
All authors provided their consent for publication.
Acknowledgements
We greatly thank the study team, in particular Laura Kenntemich for the data management, and Eike Neumann-Runde for his technical support in the setup of the survey. The authors thank the ESTSS COVID-19 study consortium (please see https://doi.org/10.17605/OSF.IO/8XHYG) for reviewing the PCS items. Authors’ contributions: AL designed and coordinated the study, drafted the manuscript and carried out the EFA; RK carried out the CFA and contributed to the writing of the manuscript; SB contributed to the data management and reviewed the manuscript; MB contributed to the recruitment. LK, AO, MB, and IS reviewed the manuscript. All authors read and approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data are available upon reasonable request from the first author.
Additional information
Funding
References
- Acuff, S. F., Strickland, J. C., Tucker, J. A., & Murphy, J. G. (2022, February). Changes in alcohol use during COVID-19 and associations with contextual and individual difference variables: A systematic review and meta-analysis. Psychology of Addictive Behaviors, 36(1), 1–19.
- Aknin, L. B., De Neve, J. E., Dunn, E. W., Fancourt, D. E., Goldberg, E., Helliwell, J. F., et al. (2022). Mental health during the first year of the COVID-19 pandemic: A review and recommendations for moving forward. Perspectives on Psychological Science, 17(4), 915–936. https://doi.org/10.1177/17456916211029964.
- American Medical Association (AMA). (2020). Managing mental health during COVID-19 [Internet]. Chicago, IL: American Medical Association. Retrieved from https://www.ama-assn.org/delivering-care/public-health/managing-mental-health-during-covid-19
- Anderson, R. M., Fraser, C., Ghani, A. C., Donnelly, C. A., Riley, S., Ferguson, N. M., Leung, G. M., Lam, T. H., & Hedley, A. J. (2004). Epidemiology, transmission dynamics and control of SARS: The 2002–2003 epidemic. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 359(1447), 1091–1105.
- Bagozzi, R. R., & Yi, Y. (1988). On the evaluation of structural equation models. 21.
- Bech, P., Olsen, L. R., Kjoller, M., & Rasmussen, N. K. (2003, June). Measuring well-being rather than the absence of distress symptoms: A comparison of the SF-36 mental health subscale and the WHO-five well-being scale. International Journal of Methods in Psychiatric Research, 12(2), 85–91.
- Bennett, G., Young, E., Butler, I., & Coe, S. (2021, March 4). The impact of lockdown during the COVID-19 outbreak on dietary habits in various population groups: A scoping review. Frontiers in Nutrition, 8, 626432.
- Ben-Porath, J. S., Waller, N. G., & Butcher, J. N. (1991 August). Assessment of coping: An empirical illustration of the problem of inapplicable items. Journal of Personality Assessment, 57(1), 162–176.
- Beutel, M. E., Hettich, N., Ernst, M., Schmutzer, G., Tibubos, A. N., & Braehler, E. (2021, July 22). Mental health and loneliness in the German general population during the COVID-19 pandemic compared to a representative pre-pandemic assessment. Scientific Reports, 11(1), 14946.
- Brähler, E., Mühlan, H., Albani, C., & Schmidt, S. (2007, April). Teststatistische Prüfung und Normierung der deutschen Versionen des EUROHIS-QOL Lebensqualität-Index und des WHO-5 Wohlbefindens-Index. Diagnostica, 53(2), 83–96.
- Carver, C. S. (1997). You want to measure coping but your protocol’ too long: Consider the brief cope. International Journal of Behavioral Medicine, 4(1), 92–1003.
- Carver, C. S., Scheier, M. F., & Weintraub, J. K. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56(2), 267–283.
- Center for the Study of Traumatic Stress (CSTS). (2020). Sustaining the well-being of healthcare personnel during coronavirus and other infectious disease outbreaks. [Internet]. Bethesda, MD: Uniformed Services University, Department of Psychiatry. Retrieved from https://www.cstsonline.org/assets/media/documents/CSTS_FS_Sustaining_WellBeing_of_Healthcare_Personnel_during_Infectious_Disease_Outbreaks.pdf
- Centers for Disease Control and Prevention (CDC). (2020). Coronavirus Disease 2019 (COVID-19): Stress and Coping. [Internet]. Atlanta, GA: U.S. Department of Health & Human Services. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
- Chirico, F., Zaffina, S., Di Prinzio, R. R., Giorgi, G., Ferrari, G., Capitanelli, I., … Ilesanmi, O. (2021). Working from home in the context of COVID-19: A systematic review of physical and mental health effects on teleworkers. Journal of Health and Social Sciences, 6, 319–332. https://doi.org/10.19204/2021/wrkn8.
- Cohan, S. L., Jang, K. L., & Stein, M. B. (2006, March). Confirmatory factor analysis of a short form of the coping inventory for stressful situations. Journal of Clinical Psychology, 62(3), 273–283.
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: L. Erlbaum Associates. 594 p.
- Cooper, C., Katona, C., & Livingston, G. (2008, November). Validity and reliability of the brief COPE in carers of people with dementia: The LASER-AD study. Journal of Nervous & Mental Disease, 196(11), 838–843.
- Cudeck, R., & O’Dell, L. L. (1994). Applications of standard error estimates in unrestricted factor analysis: Significance tests for factor loadings and correlations. Psychological Bulletin, 115(3), 475.
- Di Monte, C., Monaco, S., Mariani, R., & Di Trani, M. (2020, October 2). From resilience to burnout: Psychological features of Italian general practitioners during COVID-19 emergency. Frontiers in Psychology, 11, 567201.
- Edwards, J. R., & O’Neill, R. M. (1998, December). The construct validity of scores on the ways of coping questionnaire: Confirmatory analysis of alternative factor structures. Educational and Psychological Measurement, 58(6), 955–983.
- Eisinga, R., te Grotenhuis, M., & Pelzer, B. (2013). The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? International Journal of Public Health, 58(4), 637–642.
- El-Monshed, A. H., El-Adl, A. A., Ali, A. S., & Loutfy, A. (2022). University students under lockdown, the psychosocial effects and coping strategies during COVID-19 pandemic: A cross sectional study in Egypt. Journal of American College Health, 70(3), 679–690.
- Endler, N. S., & Parker, J. D. A. (1990). Coping inventory for stressful situations (CISS): Manual. Toronto: Multi-Health Systems.
- Endler, N. S., & Parker, J. D. A. (1999). Coping inventory for stressful situations (CISS): Manual (2nd ed.). Toronto: Multi-Health Systems.
- Field, A. (2013). Discovering statistics using IBM SPSS statistics. Los Angeles: Sage.
- Folkman, S., & Lazarus, R. S. (1988). Manual for the ways of coping questionnaire. Palo Alto, CA: Consulting Psychologists Press.
- Folkman, S., Lazarus, R. S., Dunkel-Schetter, C., DeLongis, A., & Gruen, R. J. (1986). Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. Journal of Personality and Social Psychology, 50(5), 992–1003.
- Fornell, C., & Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research, 18(1), 39–50.
- Fullana, M. A., Hidalgo-Mazzei, D., Vieta, E., & Radua, J. (2020). Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. Journal of Affective Disorders, 275, 80–81.
- Hair, J. F. (2010). Multivariate data analysis. Upper Saddle River, NJ: Prentice Hall.
- Hair, J. F., Jr., Black, W. C., Babin, B. J., & Anderson, R. E. (2019). Multivariate data analysis (8th ed.). Andover, Hampshire: Cengage Learning EMEA. 813 p.
- Kato, T. (2015). Frequently used coping scales: A meta-analysis. Stress and Health, 31(4), 315–323.
- Kavčič, T., Avsec, A., & Zager Kocjan, G. (2022). Coping profiles and their association with psychological functioning: A latent profile analysis of coping strategies during the COVID-19 pandemic. Personality and Individual Differences, 185, 111287.
- Kline, P. (2013). Handbook of psychological testing. Routledge. 753 p.
- Kline, R. B. (2015). Principles and practice of structural equation modeling [Internet] (4th ed.). New York: Guilford Press. Retrieved May 16, 2019, from https://ebookcentral-1proquest-1com-100f089lk0117.emedien3.sub.uni-hamburg.de/lib/subhh/reader.action?docID=4000663
- Knoll, N., Rieckmann, N., & Schwarzer, R. (2005, April). Coping as a mediator between personality and stress outcomes: A longitudinal study with cataract surgery patients. European Journal of Personality, 19(3), 229–247.
- Kowalsky, R. J., Farney, T. M., Kline, C. E., Hinojosa, J. N., & Creasy, S. A. (2021, June 23). The impact of the covid-19 pandemic on lifestyle behaviors in U.S. college students. Journal of American College Health, 23, 1–6.
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001, September). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613.
- Kroenke, K., Spitzer, R. L., Williams, J. B. W., Monahan, P. O., & Löwe, B. (2007, March 6). Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine, 146(5), 317.
- Krohne, H. W., Hock, M., Heuer, H., Rösler, F., & Tack, W. H.(Eds.) (2007).Psychologische Diagnostik: Grundlagen und Anwendungsfelder, Kohlhammer.
- Lotzin, A., Aakvaag, H., Acquarini, E., Ajdukovic, D., Ardino, V., Böttche, M., Bondjers, K., Bragesjö, M., Dragan, M., Grajewski, P., Figueiredo-Braga, M., Gelezelyte, O., Javakhishvili, J. D., Kazlauskas, E., Knefel, M., Lueger-Schuster, B., Makhashvili, N., Mooren, T., Sales, L., … Schäfer, I. (2020). Stressors, coping and symptoms of adjustment disorder in the course of the COVID-19 pandemic – study protocol of the European society for traumatic stress studies (ESTSS) pan-European study. European Journal of Psychotraumatology, 11(1), 1780832.
- Lundqvist, L. O., & Ahlström, G. (2006, May). Psychometric evaluation of the ways of coping questionnaire as applied to clinical and nonclinical groups. Journal of Psychosomatic Research, 60(5), 485–493.
- McWilliams, L. A., Cox, B. J., & Enns, M. W. (2003, December). Use of the coping inventory for stressful situations in a clinically depressed sample: Factor structure, personality correlates, and prediction of distress. Journal of Clinical Psychology, 59(12), 1371–1385.
- Ong, J. L., Lau, T. Y., Massar, S. A. A., Chong, Z. T., Ng, B. K. L., Koek, D., et al. (2020). COVID-19-related mobility reduction: Heterogenous effects on sleep and physical activity rhythms. Sleep Res Soc, zsaa179, 1–13.
- Özçevik Subaşi, D., Akça Sümengen, A., Şimşek, E., & Ocakçı, A. F. (2021, October). Healthcare workers’ anxieties and coping strategies during the COVID-19 pandemic in Turkey. Perspectives in Psychiatric Care, 57(4), 1820–1828.
- Parker, J. D., Endler, N. S., & Bagby, R. M. (1993). If it changes, it might be unstable: Examining the factor structure of the ways of coping questionnaire. Psychological Assessment, 5(3), 361–368.
- Platts, K., Breckon, J., & Marshall, E. (2022, December). Enforced home-working under lockdown and its impact on employee wellbeing: A cross-sectional study. BMC Public Health, 22(1), 199.
- Ponterotto, J. G., & Ruckdeschel, D. E. (2007). An overview of coefficient alpha and a reliability matrix for estimating adequacy of internal consistency coefficients with psychological research measures. Perceptual and Motor Skills, 105(3), 997–1014.
- Rahman, H. A., Issa, W. B., & Naing, L. (2020, September). Psychometric properties of Brief-COPE inventory among nurses [Internet]. In Review. Retrieved February 24, 2021, from https://www.researchsquare.com/article/rs-84184/v1
- Rexrode, K. R., Petersen, S., & O’Toole, S. (2008, April). The ways of coping scale: A reliability generalization study. Educational and Psychological Measurement, 68(2), 262–280.
- Rogowska, A. M., Kuśnierz, C., & Bokszczanin, A. (2020, September). Examining anxiety, life satisfaction, general health, stress and coping styles during COVID-19 pandemic in Polish sample of university students. Psychology Research and Behavior Management, 13, 797–811.
- Salopek-Žiha, D., Hlavati, M., Gvozdanović, Z., Gašić, M., Placento, H., Jakić, H., Klapan, D., & Simic, H. (2020). Differences in distress and coping with the COVID-19 stressor in nurses and physicians. Psychiatria Danubina, 32(2), 287–293.
- Samuels, P. (2017). Advice on exploratory factor analysis.
- Schermelleh-Engel, K., Moosbrugger, H., & Müller, H. (2003). Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res – Online, 8(2), 23–74.
- Schmidt, R. A., Genois, R., Jin, J., Vigo, D., Rehm, J., & Rush, B. (2021, November). The early impact of COVID-19 on the incidence, prevalence, and severity of alcohol use and other drugs: A systematic review. Drug and Alcohol Dependence, 228, 109065.
- Shamblaw, A. L., Rumas, R. L., & Best, M. W. (2021, February). Coping during the COVID-19 pandemic: Relations with mental health and quality of life. Canadian Psychology / Psychologie Canadienne, 62(1), 92–100.
- Sheroun, D., Wankhar, D. D., Devrani, A., Lissamma, P. V., Gita, S., & Chatterjee, K. (2020). A study to assess the perceived stress and coping strategies among B. Sc. Nursing students of selected colleges in Pune during COVID-19 pandemic lockdown. Int J Sci Healthc Researc, 5(2), 280–288.
- Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006, May 22). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
- Stone, A. A., Greenberg, M. A., Kennedy-Moore, E., & Newman, M. G. (1991). Self-report, situation-specific coping questionnaires: What are they measuring? Journal of Personality and Social Psychology, 61(4), 648–658.
- Streiner, D. L. (2003, February). Starting at the beginning: An introduction to coefficient alpha and internal consistency. Journal of Personality Assessment, 80(1), 99–103.
- Taylor, S. E., & Stanton, A. L. (2007, April). Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology, 3(1), 377–401.
- Walsh, R. (2011). Lifestyle and mental health. American Psychologist, 66(7), 579–592.
- World Health Organization (WHO). (2020). Mental health and psychosocial considerations during the COVID-19 outbreak. World Health Organ [Internet]. 03; Geneva. Available from: https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf
- Zacher, H., & Rudolph, C. W. (2021, January). Individual differences and changes in subjective wellbeing during the early stages of the COVID-19 pandemic. American Psychologist, 76(1), 50–62.
Appendices
Appendix 1
Means, Standard Deviations, Skewness and Kurtosis (Confirmatory Factor Analysis, n = 1172)
Appendix 2
Local Goodness of Fit Indices: Factor Loadings and Communality (Confirmatory Factor Analysis, n = 1172)
Appendix 3
Local Goodness of Fit Indices: Factor Reliabilities, Average Variance Extracted, Fornell-Larcker Criterion and Intercorrelations of the Subscales (Confirmatory Factor Analysis, n = 1172)
Appendix 4
Internal Consistency, Discrimination Index and Difficulty Index (Confirmatory Factor Analysis, n = 1172)
Appendix 5. Intercorrelations between the Pandemic Coping Scale Subscales and the Brief-COPE Subscales, and WHO-5, PHQ-9 and GAD-2 (n = 1172)
Appendix 6. Pandemic coping scale (PCS)
The following questions ask how you have sought to cope with the hardship due to the pandemic.
Please read the statements and indicate how much you have been doing this within the last four weeks to cope with the coronavirus pandemic on a scale from 0 to 3. Please tick the box that best reflects your behavior.
Table