ABSTRACT
Background
Research has demonstrated the importance of understanding risk factors for mental health and wellbeing. Less research has focused on protective factors that protect mental health and promote wellbeing in diverse contexts. Estimating structural paths from risk protective factors to psychopathology and wellbeing can inform prioritization of targeted investment in adolescent health programs that seek to modify factors that are most closely associated with mental wellbeing.
Study objective
The purpose of this study was to examine risk factors (e.g. emotional neglect, emotional abuse, physical neglect, stigma) and protective factors (e.g. community relationships, self-esteem, and autonomy) among adolescent orphans, protective associations with depression, anxiety and externalizing behaviors and promotive associations with hope, happiness, and health.
Methods
The analytic sample was collected between January and March of 2019 and included 350 adolescent orphans ages 10–15 from three districts in Tanzania. Participants completed survey interviews, 75–90 min in length, that measured risk and protective factors, psychological symptoms, and mental wellbeing measures.
Results
Results of the fitted structural equation model indicated that structural paths from protective factors to psychopathology (β = −0.53, p = 0.015) and mental wellbeing (β = 0.72, p = 0.014) outcomes were significant. Structural paths from risk factors to psychopathology (β = −0.34, p = 0.108) and mental wellbeing (β = −0.24, p = 0.405) were not significant.
Conclusion
In a sample of vulnerable youth, protective factors (e.g. community relationships, self-esteem, and autonomy) were significantly associated with reduced depression, anxiety and externalizing behaviors and increased hope, happiness, and health in a structural equation model that included risk factors (emotional neglect, emotional abuse, physical neglect). Results suggest that strong community relationships, self-esteem and autonomy may be important modifiable factors to target in intervention programs aimed at supporting adolescent mental wellbeing.
Introduction
The transition from childhood to adolescence, marked by the onset of puberty, is the beginning of a period of rapid growth and dynamic changes, not only in physical development, but also in social, emotional, and cognitive growth (Crone & Dahl, Citation2012). The Lancet Commission on Adolescent Health and Wellbeing reported a disproportionate surge in the number of adolescents globally, with adolescents representing 16% of the global population in 2018, and unprecedented expansion in low-resource settings (UNICEF, Citation2019). Investment in adolescent health is warranted and has the potential to yield a ‘triple dividend’ of health benefits for adolescents now, into adulthood, and for the next generation of children (Patton et al., Citation2016). Increases in accidents, suicides, homicide, mental disorders, substance use, eating disorders, sexually transmitted diseases and unintended pregnancy can lead to life-long negative trajectories (Patton et al., Citation2016). Mental wellbeing has been understudied in comparison with mental disorders (Sequeira et al., Citation2022; Thomas et al., Citation2020). The WHO’s constitution defines health as a ‘state of complete, physical, mental and social wellbeing and not merely the absence of disease or infirmity’ (World Health Organization, Citation2023). Risk for mental health disorders increases during mid-to-late adolescence and can have near and long-term impacts on health and wellbeing (Green et al., Citation2010). As such, adolescent mental health is a particularly important priority for early-targeted-investment during adolescence.
An estimated 47.5 million children were orphaned in 2007 in Sub-Saharan Africa (UNICEF, Citation2009). Previous research has demonstrated that exposure to stress among orphans includes adopting caretaker roles, poverty, instability in housing and school attendance, separation from siblings, vulnerability to child labor and exploitation, emotional neglect, emotional abuse, physical abuse and stigma (Ahmad et al., Citation2015; Anda et al., Citation1999; Blum et al., Citation2019; Cluver et al., Citation2009; Dube et al., Citation2006; Foster et al., Citation1997; Mersky et al., Citation2013; Michl et al., Citation2013; Ntozi & Mukiza-Gapere, Citation1995; Tsehay et al., Citation2020; Zhang et al., Citation2019). In Sub-Saharan Africa, these risk factors are associated with depression, anxiety, and externalizing behaviors that can persist into adulthood (Cherewick, Tol, et al., Citation2016; Earls et al., Citation2008; Hermenau et al., Citation2015; Meinck et al., Citation2017; Stansfeld et al., Citation2017). Adolescent orphans in Africa, in comparison to non-orphans, are more susceptible to adverse life experiences leading to an increase in risk for psychological symptoms (Doku et al., Citation2019; Hermenau et al., Citation2015; Marais et al., Citation2013; Puffer et al., Citation2012). Studies in Tanzania found that emotional and social risk factors increased psychological problems in adolescent orphans and emotional support and support of autonomy were lacking and were associated with decreased wellbeing (Kyaruzi, Citation2022; Msoka & Holroyd, Citation2018). Patterns of social behavior, emotional development, and identity formation during early adolescence can increase risk for poor health outcomes during mid-to-later adolescence gender-based violence, sexual and reproductive health outcomes or support positive mental wellbeing (Grootendorst-van Mil et al., Citation2021; McLaughlin et al., Citation2022; Pine et al., Citation2001; Schneiders et al., Citation2006).
A recent review of mental health interventions for adolescents in sub-Saharan Africa assessed 57 unique interventions, 17 of which specifically targeted orphan populations, and intervention approaches included economic-based, family strengthening, psychoeducation, cognitive behavioral therapy and interpersonal psychotherapy (Mabrouk et al., Citation2022). Additional reviews of adolescent mental health interventions recommend the implementation of programs by non-specialists within community settings such as schools and community-based organizations (Mabrouk et al., Citation2022; Sequeira et al., Citation2022). For such interventions to be effective, additional research with diverse adolescent populations is needed to understand levels of risk or protective factors and associations with psychological symptoms and wellbeing. There is a significantly smaller body of research focused on protective factors that mitigate risk and promote positive health outcomes, however, there is evidence that social emotional capacities and skills, autonomy, self-esteem, coping flexibility, social support networks, and positive caregiver and community relationships are protective for mental health (Henson et al., Citation2017; Luthar, Citation2006; Masten, Citation2009; Taylor et al., Citation2000; Triana et al., Citation2019; World Health Organization, Citation2023). Identifying protective factors and the strength of association of protective factors protecting against psychopathology and promoting wellbeing is important to informing policies and programs, particularly in contexts where traumatic experiences have already transpired.
Gaps exist in the current literature examining risk and protective factors for mental health among adolescent orphans (Jörns-Presentati et al., Citation2021). Intervention approaches targeting mental wellbeing can help to ensure vulnerable youth can contribute to society and the future stability of countries. To date, no studies to our knowledge have simultaneously evaluated risk and protective factors and associations with psychopathology and mental wellbeing. To advance future research evaluation of modifiable factors, including modifiable protective factors, is needed to guide intervention programming targeting adolescents by leveraging modifiable factors with the greatest potential impact on psychopathology and wellbeing. The WHO estimates returns of 3.5–5.7 USD for each 1 USD invested in the treatment of anxiety and depression (Meffert et al., Citation2021). Tanzania is experiencing a surge in the youth population with approximately half the population under the age of 17.5 years and 47% under the age of 15 years (MoHCDGEC, Citation2016; UNDP, Citation2017). This number is expected to double by 2055 (UNICEF, Citation2019). This youth ‘bulge’ is caused by improvements in early child morbidity and mortality; however, the substantial increase in adolescent populations also underscores the importance of addressing morbidity and mortality associated with mental health by preventing psychopathology and promoting wellbeing during adolescence (Patton et al., Citation2016).
Hypothesis
The objective of this study was to examine the association between risk and protective factors on psychopathology and mental wellbeing among adolescent orphans in Tanzania. To achieve this objective, we sought to model paths from both risk and protective latent factors to these (Tol et al., Citation2013). It was hypothesized that (1) protective factors including self-esteem, autonomy and community relationships would be positively associated with wellbeing outcomes (happiness, hope for the future and general health) and negatively associated with psychopathology (depression, anxiety and externalizing behaviors), (2) the strength of association of structural paths from protective factors to psychopathology and wellbeing outcomes would be greater than the strength of association of structural paths between risk factors to psychopathology and wellbeing outcomes. While the primary objectives of this study were to evaluate second-order latent risk and protective factors on psychopathology and wellbeing, a secondary objective was to assess the relative strength of paths from first-order latent factors to second-order latent factors. It was hypothesized that community relationships would have the strongest association with the latent protective factor, based on recent research with orphans in this context (Cherewick et al., Citation2023). It was also hypothesized that experiences of stigma would be most strongly associated with the latent risk factor, based on previous research indicating the importance of stigma in predicting mental health outcomes in orphan populations (Cluver et al., Citation2008).
Methods
Ethics approval
The study protocol was approved by the University of California Berkeley Committee for Protection of Human Subjects Institutional Review Board (IRB) – CPHS Protocol Number: 2018-01-10628; in June 2018. The primary local partner in Tanzania, Health for a Prosperous Nation (H-PON), obtained ethical clearance for these research activities from the National Institute of Medical Research, the local IRB in Tanzania (Ref. NIMR/HQ/R.8a/Vol. IX/2851 in August 2018).
Study procedures
Participants at each orphanage were read an announcement script in the local language, Swahili, and adolescents were invited to contact the orphanage guardian if they were interested in participating in the study. Before each interview, the guardian (i.e. orphanage owner) gave written consent for each youth and oral assent was obtained from each youth. Assent scripts were read aloud in Swahili, detailing the study objectives and protocol. Each youth was assigned an advocate from The Ministry of Health and Social Welfare and was informed that they could contact them for all matters of concern regarding the study before, during, or after the survey. A social welfare officer accompanied participants to most visits, and research assistants were instructed to report youth in need of support to their advocate.
After obtaining guardian consent and participant assent, each participant was provided a private place (e.g. quiet room in orphanage or outside) to complete the interview. Survey interviews were conducted by local research staff consisting of two expert trainers and 12 community facilitators. Training included topics such as research methods, CITI’s course in human subjects’ protection, survey administration, sensitivity, privacy, and consent. The survey was programed onto computer tablets and administered by a trained facilitator who read aloud each question in Swahili and recorded participant responses on the tablet. Surveys were translated from English to Swahili by bilingual research partners at H-PON. Interviews took 75–90 min. Participants were offered a break during the survey, and each received a small gift of school supplies as a token of appreciation for participation. Data were collected between January and March of 2019.
Sample selection
To examine the association between adolescent risk and mental health and wellbeing, we surveyed adolescent orphans ages 10–15. Participants were recruited in collaboration with H-PON and youth-serving orphanages. The city of Dar es Salaam has five districts: Kinondoni, Ubungo, Ilala, Temeke and Kigamboni. H-PON identified orphanages in three peri-urban districts: Ubungo, Ilala and Temeke. All orphanages with children ages 10 and older were invited and agreed to participate, with additional permission from the Ministry of Health and Social Welfare. All adolescents age 10–15 that provided assent were included in the study. Two eligible adolescents did not provide assent because they were ill, and one eligible adolescent did not want to participate. All other adolescents invited to participate provided assent and completed the survey.
Survey measures
African youth psychological assessment
The African Youth Psychological Assessment (AYPA) is a dimensional scale for measuring psychosocial adjustment in African youth (Betancourt et al., Citation2014). The scale measures internalizing and externalizing symptoms in African youth and has been previously validated and used in several East African contexts and in Tanzania (Betancourt et al., Citation2014; Cherewick, Tol, et al., Citation2016; Cherewick et al., Citation2021; Fine et al., Citation2021; O’Callaghan et al., Citation2014; Sonderegger et al., Citation2011). Subsequent analysis of the AYPA divided internalizing symptoms into two domains representing anxiety and depression (Sonderegger et al., Citation2011). summarizes the items of each subscale used to measure depression, anxiety, and externalizing behaviors. Each item was provided to the trained interviewer to ask the participant how much they experienced or felt this in the past seven days on a 4-point Likert scale (1 = ‘Never’ to 4 = ‘All the time’). Subscales were aggregated by mean with higher scores indicating greater levels of symptoms reported. The Cronbach's alpha in this sample for the full AYPA measure was 0.81 in this sample.
Table 1. African Youth Psychological Assessment (AYPA).
Douchette and Bickman's hopefulness scale
This scale was used to measure hope among adolescents ages 6–18 and has demonstrated high internal consistency in previous studies in Sub-Saharan Africa and Tanzania (α = 0.82) (Cherewick, Tol, et al., Citation2016; Doucette & Bickman, Citation2001; Mwakanyamale & Yizhen, Citation2019). The scale consists of 10 items designed to assess levels of hopefulness in the last 30 days. Each item was rated on a 3-point scale of 1 = ‘Almost never’, 2 = ‘Sometimes’ and 3 = ‘Often’. Examples of items include, ‘there are people I counted on to help out if I needed to’, ‘my life has been going well’, and ‘I was able to accomplish the things I wanted to do in my life’. Cronbach’s alpha was 0.75 in this sample and scores were aggregated by mean with higher scores indicating higher levels of hope for the future.
Childhood trauma scale
This study utilized this self-report measure to assess adverse life experiences including emotional abuse, emotional neglect, and physical neglect. The original scale included 25 items evaluated using a 5-point scale of 1 = ‘Never true’ to 5 = ‘Very often true’ and demonstrated a Cronbach's alpha ranging 0.88–0.95 (Bernstein et al., Citation2003; Mwakanyamale & Yizhen, Citation2019; Wingenfeld et al., Citation2011). We adapted the scale by reducing the 5-point response categories to dichotomous ‘yes’ or ‘no’ and removing 15 items that were identified as too sensitive for this population by the local IRB, particularly those about prior sexual assault or sexual abuse. The remaining 10 items included three domains of emotional abuse, emotional neglect, and physical neglect. Some questions asked include, ‘I lived in different households at different times’, ‘I was insulted or humiliated by someone close to me in front of other people’, and ‘I saw or heard someone beaten’. Cronbach’s alpha for this sample was 0.88. Mean scores were calculated by domain with higher scores indicating higher exposure to adverse life experiences in that domain.
Stigma
This study measured stigma on an 8-item adaptation of Williams et al.’s original 9-item ‘Everyday Discrimination Scale’, highlighting experiences of stigma or perceived discrimination in day-to-day life related to respect, courtesy, intelligence, honesty, verbal harassment, and verbal insults (Williams et al., Citation1997). This scale was introduced to participants with the prompt ‘in your day-to-day life, how often do any of the following things happen to you’. Responses were recorded on a 4-point scale (0 = ‘Never’ to 3 = ‘Always’). Examples of items include ‘You are threatened or harassed’ and ‘You are treated with less respect than other people are’. One item, ‘You receive poorer service than other people at restaurants or stores’, was removed. Cronbach’s alpha in this sample was 0.80. Scores were aggregated by mean with higher scores indicating greater experiences of stigma.
Rosenberg self-esteem scale
The study used the Rosenberg self-esteem (RSE) 10-item scale that has dichotomous response choices ‘yes’ and ‘no’ (Rosenberg, Citation2015). This measure has been used in prior studies in Tanzania and translated to Swahili (Mwakanyamale & Yizhen, Citation2019). Examples of items include ‘I feel that I have a number of good qualities’ and ‘on the whole I am satisfied with myself’. Cronbach’s alpha was 0.63 in this sample. After completing reverse-scoring on items as instructed by scale scoring instructions, scores were aggregated by mean with higher scores indicating higher levels of self-esteem.
Adolescent autonomy questionnaire
This scale was adapted to measure adolescent autonomy manifested in a young person’s ability to act, feel, and think independently (Noom et al., Citation2001). The scale aims to assess three domains of autonomy including functional (e.g. easily starting new activities), emotional (e.g. vocalizing disagreements), and attitudinal (e.g. making choices easily) autonomy. The scale consists of 15, 5 items for each domain, and were assessed on a 5-point scale (1 = ‘Very bad description of me’ to 5 = ‘Very good description of me’). Total autonomy scores were aggregated by mean with higher scores reflecting higher total autonomy. Cronbach’s alpha for the total scale was 0.61 in this sample.
Additional measures
General Health was measured by asking participants to respond to 1 item, ‘overall, how would you rate your health during the past month?’ with response options of 0 = ‘Very bad’ to 3 = ‘Very good’. Happiness was measured by asking participants to respond to one item, ‘in general, how happy do you consider yourself to be’. Community Relationships were measured with four items developed by the Tanzanian research team by adapting previously developed questions to measure community relationships in east-Africa (Cherewick, Doocy, et al., Citation2016). Participants responded with dichotomous answer choices ‘yes’ and ‘no’ to four statements: ‘I feel welcome in my community’, ‘My caregivers treat me as well as other children’, ‘I have the same opportunities and responsibilities as other children in the family/household’, and ‘I feel that I am treated like the other children in the community’. The community relationship measure was aggregated by mean, with higher scores indicating more favorable community relationships.
Data analysis
Data were analyzed using Stata Statistical Software Version 14 (StataCorp, Citation2017). Sample characteristics are presented using frequencies and means by sex. Prior to fitting the structural equation models (SEMs), forward stepwise regression models for included measure were completed to identify potential covariates (sex, age, school enrollment, age upon entering the orphanage and years spent at the orphanage). Sex was determined to be a potential confounder and was included as a covariate in the structural equation models. Next, prior to fitting the SEM, we completed first-order confirmatory factor analysis (CFA) on the latent variables comprising the second-order latent variables for Risk Factors, Protective Factors, Psychopathology and Wellbeing.
SEM, specifically a full latent variable model, was used to examine relationships between latent variables. The structural path model is consistent with previously developed conceptual models and theory identifying risk, protective and promotive path relationships to mental health outcomes (Masten, Citation2011; Masten, Citation2013; Ungar, Citation2012). The SEM was assessed for overall fit, significance of structural paths and variability of latent variables explained by observed variables. Goodness of fit was evaluated using chi-square, the root mean square error of approximation (RMSEA), the comparative fit index (CFI), the Tucker-Lewis index (TLI) and the standardized root mean residual (SRMR) (Bentler, Citation1990; Steiger & Lind, Citation1980; Tucker & Lewis, Citation1973). The following statistical criteria were used to evaluate model fit: RMSEA < 0.06; CFI > 0.90, TLI > 0.90, and SRMR < 0.08 (Kline & Santor, Citation1999). Robust cluster estimation was used to account for clustering of orphanages within each of 3 districts. The maximum likelihood method of estimation was used to estimate the SEM.
Results
Demographic characteristics
A total of 20 orphanages were involved in the study from three districts in peri-urban Dar es Salaam, Tanzania. The smallest orphanage housed 16 youth and the largest housed 160. Staffing of the orphanages ranged from 3 to 40 staff members, with registration years between 1966 and 2010. 18 of the 20 orphanages housed both boys and girls. Seven orphanages were in the Ubungo district, 9 in the Temeke district, and 4 in the Ilala district. A total of 1095 total youth of all ages resided in these orphanages, including 489 girls and 606 boys.
Of these 1095 total youth, 350 between the ages of 10 and 15 provided assent and participated in the study (). 201 girls and 149 boys were included in the analytic sample with a mean age of 12.4; SD:1.5. As expected, girls reported higher scores on the pubertal development scale with a mean score of 1.5; SD:1.2 in comparison to boys with a mean score of 0.7; SD:0.9. Most youth (92%) were currently enrolled in school. The average age that youth began care in the orphanage was 7.2 years old; SD:3.7 and on average participants had spent 5.4 years at the orphanage (SD:3.6) at the time of the study. Participants’ report of risk and protective factors, psychological symptoms, and wellbeing measures are reported in .
Table 2. Descriptive statistics of analytical sample (n = 350).
Table 3. Mean and standard deviations of measures.
Structural equation model
The measurement models for each latent variable (Risk and Protective Factors, Wellbeing and Psychological Symptoms) were selected based on previous research indicating significant relationships with mental health and wellbeing outcomes. We followed the following steps to fit the structural equation model (Hancock et al., Citation2010). We established the measurement model for each factor using CFA and evaluated fit. Results from CFA indicated adequate model fit for each factor with CFI > 094; TLI > 0.88, SRMR < 0041 and RMSEA < 0.043. (2) We estimated a CFA model with all factors in the intended SEM allowing factors to freely co-vary and evaluated model fit. Results indicated that fit indices were unsatisfactory (CFI = 085, SRMR = 0096, RMSEA = 0.084). (3) We then examined Lagrange multiplier tests of modification indices and found the omitted covariance path between risk and protective factor latent variables was significant (MI = 60.2, P > MI = 0.000; EPC = −0.746) (Sörbom, Citation1989). (4) The covariance path between risk and protective factors is theoretically supported, and thus we revised the SEM to include this covariance path and evaluated model fit. (5) We then fitted the subsequent SEM with the addition of the covariance path between risk and protective factors and evaluated model fit. Results indicated adequate model fit of the revised SEM; CFI = 0.926; RMSEA = 0.059 (90% CI [0.046; 0.073]). (6) We completed residual analyses and determined the SRMR of 0.045 and RMSEA of 0.059 met evaluation levels of 0.05 and 0.06, respectively. Further examination of residuals following the SEM supported model fit with no standardized residuals larger than 3 (in absolute value) (Barrett, Citation2007). (7) We then explored plausible sources of measurement non-invariance including testing invariance by sex and age using multi-group structural equation modeling. Multi-group SEM models failed to converge, due to inadequate sample size. Based on prior regression analyses exploring confounders indicating sex as a potential confounder, we included sex as a covariate in our final SEM.
presents the SEM for the analytical sample. Invariance by sex was tested and was insignificant. presents the standardized path coefficients and p-values for the structural paths between second-order latent variables (risk and protective factors) and second-order latent variables of psychopathology and wellbeing. Results indicate that protective factors were significantly associated with lower levels of psychological symptoms (β = −4.87, p = 0.045), and higher levels of wellbeing (β = 3.79, p = 0.048).
Figure 1. Structural equation model of Risk and Protective Factors on Psychological Symptoms and Wellbeing.
Note: CFI = 0.926; SRMR = 0.045; RMSEA = 0.059; *p < 0.05, **p < 0.01, ***p < 0.001; Sex was included as a covariate.
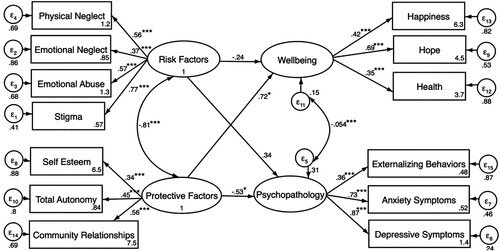
Table 4. Standardized path coefficients between risk and protective factors and mental health and wellbeing.
Paths from first-order latent factors to second-order latent factors reported in indicate important differences in the strength of association from first-order to second-order latent factors. For the Risk Factors latent factor, stigma had the highest association (γ = 0.77; p < 0.001), followed by emotional abuse (γ = 0.57, p < 0.001), physical neglect (γ = 0.56, p < 0.001), and emotional neglect (γ = 0.37, p < 0.001). For the Protective Factors latent factor, community relationships held the highest association (γ = 0.56, p < 0.001), followed by autonomy (γ = 0.45, p < 0.001), and self-esteem (γ = 0.34, p < 0.001). For the Wellbeing latent factor, hope for the future had the highest association with wellbeing (γ = 0.69, p < 0.001), followed by happiness (γ = 0.42, p < 0.001), and health (γ = 0.35, p < 0.001). For the Psychopathology latent factor, depressive symptoms had the highest path standardized path coefficient (γ = 0.87, p < 0.001), followed by anxiety symptoms (γ = 0.73, p < 0.001), and externalizing behaviors (γ = 0.36, p < 0.001),
Discussion
The aims of this study were to evaluate protective paths to lower psychological symptoms and promotive paths to mental wellbeing by examining risk and protective latent factors. Results from this study found that protective factors were significantly associated with lower psychological symptoms, and higher levels of wellbeing. Further, this study did not find a statistically significant association between risk factors and wellbeing or psychological symptoms. Orphans in Tanzania have reported higher levels of adverse life experiences with 56% reporting emotional neglect (Hermenau et al., Citation2015). Experiences of maltreatment in childhood and adolescence are an important factor in understanding the developmental etiology of psychological disorders (Hawes et al., Citation2021; Lee et al., Citation2022; Schilling et al., Citation2007). Previous research on orphans and abandoned children from five low-income countries have indicated that emotional difficulties (i.e. emotional symptoms, conduct problems, hyperactivity/inattention, and peer relationship problems) are associated with lags in cognitive development and risk for psychopathology including depression, anxiety and anti-social behaviors (Bomysoad & Francis, Citation2020; Escueta et al., Citation2014). A study of Zambian adolescents found that adolescents who experience one or more adverse life experiences including physical violence, emotional violence or community violence reported more mental distress, suicidal thoughts and attempts (Lee et al., Citation2022). These findings highlight the importance of focusing on protective factors to improve mental health in adolescent orphan populations, especially among populations faced with risk factors, like orphanhood, that have already occurred (Bachman DeSilva et al., Citation2012; Whetten et al., Citation2011).
Modeling a latent factor of risk allows the inclusion of four domains of risk including emotional neglect, emotional abuse, physical neglect, and stigma. Results from this study supported the hypothesis that stigma would have the strongest association with the latent risk factor compared to emotional abuse, physical neglect, and emotional neglect, which were also statistically significantly positively associated with the latent risk factor. Experiencing stigma and discrimination has been shown to lower self-control, increase risky or unhealthy behaviors (e.g. delinquency, fighting, substance abuse) and reduce participation in healthy behaviors (Aronson et al., Citation2013; Inzlicht et al., Citation2006; Kwaning et al., Citation2021). Experiences of stigma can lead to significantly heightened stress responses and are associated with poor sleep (e.g. quality, duration), which can have long-term effects including increased disease and mortality risk in adulthood (Inzlicht et al., Citation2006; Ong et al., Citation2017; Pascoe & Smart Richman, Citation2009). Over time, repeated experiences of stigma can become a chronic stressor. Previous research explored how social perceptions of ‘differentness’, or categorization into a group separate from the majority, can be internalized and lead to ‘self-stigma’ and worse mental health outcomes (Corrigan & Nieweglowski, Citation2021). Previous research indicates that orphans attribute experiences of stigmatization to their orphan status (Funkquist et al., Citation2007; Morantz et al., Citation2013). In this study, Tanzanian orphans may perceive their orphan status as source of stigma, and future research is needed to explore if and why orphans have differential perceptions of stigma experiences in comparison to non-orphans. Prior research with Tanzanian orphans has shown that perceived stigmatization was associated with orphan’s depression severity (Hermenau et al., Citation2015). Cultural context and social norms are important factors to consider experiences of stigma to identify potential intervention strategies that seek to reduce stigma (Koydemir & Essau, Citation2018).
The latent protective factor in this study included domains of community relationships, self-esteem, and autonomy. As hypothesized, this study found community relationships had the strongest association with the latent protective factor compared to autonomy and self-esteem, which were also statistically significantly positively associated with the latent protective factor. Previous research has identified the protective domains as significantly associated with lower psychopathology and higher mental wellbeing (Ames et al., Citation2015; Malika et al., Citation2021; Tol et al., Citation2013; Werner, Citation1992). For example, a study with aboriginal youth in Canada, identified the importance of self-esteem as a protective factor for depressive symptoms (Ames et al., Citation2015). In another study, personal autonomy was protective against the effects of hardship on mental health (Werner, Citation1992). The findings in this study indicated that positive community relationships, higher self-esteem, and greater autonomy were associated with reduced psychological symptoms and greater happiness, hope and health. Prior research has demonstrated the importance of supportive social relationships during adolescence in predicting lower psychological symptoms, externalizing symptoms, stress, depression and loneliness (Deković et al., Citation2004; Inguglia et al., Citation2015; La Greca & Harrison, Citation2005; Morrow, Citation1999; Wild et al., Citation2013).
Previous research indicates that social support, from friends, caregivers, extended family and community members has a significant, positive association with levels of hope and self-esteem (Cherewick, Doocy, et al., Citation2016; Deković et al., Citation2004; Griggs, Citation2017; Mahon & Yarcheski, Citation2017; Triana et al., Citation2019). These results align with our study findings that community relationships and self-esteem were significantly associated with protective factors. Hope was also significantly associated with wellbeing, which was positively supported by protective factors in this sample. A study in two slum settlements in Kenya of adolescents (ages 12–19) examined the relationship between adverse life events, self-esteem, and delinquency (Kabiru et al., Citation2014). One study found that adolescents who experienced adverse life events but had higher levels of self-esteem were less likely to engage in delinquent behavior (Kabiru et al., Citation2014). The ability of adolescents to form social support networks, including community relationships may vary by context and by gender. Research from the Democratic Republic of Congo found that girls had more limited freedom outside the home and greater household responsibilities preventing the formation of strong social support systems (Cherewick, Tol, et al., Citation2016). Research in university-aged students in collectivist (Pakistan) and individualist (Germany) cultural contexts found that a sense of coherence and social support was an important predictor of wellbeing, indicating that supportive relationships may be an especially valuable protective factor to leverage regardless of culture (Nosheen et al., Citation2017).
In this study, autonomy was a statistically significant domain of the latent protective factor. During adolescence, autonomy becomes increasingly important while learning to navigate a rapidly changing social world including new relationships and responsibilities. Evidence from studies of adolescent orphans from other contexts, including Ethiopia and Egypt, have demonstrated lower levels of autonomy in orphans than non-orphans (El-Gilany et al., Citation2013; Hailegiorgis et al., Citation2018). Research suggests that opportunities to practice positive risk taking can promote mental wellbeing (Allen & Loeb, Citation2015; Crone & Dahl, Citation2012). For example, research among 13–15-year-olds from the Southeastern United States indicated that developing autonomy can be protective against criminal behavior and alcohol/substance abuse up to a decade later (Allen & Loeb, Citation2015; Rutter, Citation2000; Wild et al., Citation2013). Similar results have been reported in Italian 17–26-year-olds, with higher autonomy found to be predictive of lower levels of depression (Inguglia et al., Citation2015). Cross-cultural differences, including comparative studies between collectivistic and individualistic cultures, can shape the types of autonomy appropriate for youth in a particular context. Cheng et al. (Citation2014) completed a meta-analysis on coping strategies and reported that in more individualistic societies, the importance placed on autonomy and self-consistency impacted the adaptive effect of some coping strategies, whereas in more collectivistic societies, having flexibility in use of coping strategies that were situation-dependent were more adaptive. For Tanzanian orphans, it will be important to explore differences in autonomy between orphans and non-orphans, and potential opportunities for orphans to build autonomy in ways that are socially acceptable.
Orphans in low-resource settings are a particularly vulnerable group that can benefit from interventions that focus on protective factors rather than previously encountered risk factors (Ahmad et al., Citation2015; Cluver et al., Citation2009). This study contributes to the growing body of research on modifiable protective factors that can protect against psychopathology and promote mental wellbeing during adolescence (Masten, Citation2009; Taylor et al., Citation2000). Recent studies have examined protective factors and effects on psychological health of positive peer and community relationships in mitigating risks pertaining to COVID-19 (Magson et al., Citation2021). A study in Zambia and Sierra Leone on the effects of COVID-19 on children and young people found protective factors increased resilience and were associated with lower depression and anxiety (Sharpe et al., Citation2021). Supporting coping flexibility, including engagement (social support seeking, problem solving) and disengagement strategies (distraction) for various stressors may best protect and promote mental wellbeing. A study in Tanzania comparing psychological wellbeing between orphans and non-orphans found orphans demonstrated more internalizing and externalizing symptoms than non-orphans (Hermenau et al., Citation2015; Makame et al., Citation2002). In contexts where community relationships are valued, there is an opportunity to integrate cultural assets into intervention design to leverage their protective effects (Cherewick et al., Citation2020). A study with Tanzanian orphans and non-orphans found Utu, a culturally defined collective asset representing a philosophical value system underscoring shared humanity and reciprocal acts of kindness and generosity in the community, enhances resilience to adverse life experiences and experiences of stigma and (Cherewick et al., Citation2023). Policies and intervention programs can modify protective factors to leverage the dual benefit to protect and promote mental wellbeing.
Limitations
While this study selected districts that represented diverse sociodemographic profiles, the results of this study may not be generalizable to other contexts or countries. For example, the protective association of strong community relationships with better mental health outcomes may not be present in other cultures or contexts. Rural districts may present different risk and protective factors from the peri-urban orphanages included in this study. Adolescents in this study were not randomly selected; any adolescents who provided assent were included. Future studies should consider randomly selecting adolescents from a greater diversity of geographic location and socioeconomic status to confirm these results as generalizable to all orphans in Tanzania. While the analytical approach to SEM accounted for clustering at the municipal district level, our data set did not include orphanage-level data and it is possible that effects differ between individual orphanages.
This study sought to use measures that had been previously validated in sub-Saharan Africa, however, not all measures were previously validated in Tanzania or in orphan populations. Further, a limitation was the reliance on adolescents’ self-report on measure items. It is possible that adolescents’ current mental health/wellbeing could bias their ability to accurately perceive their own mental health or the ways they are perceived by others (e.g. stigma) and therefore it is possible that adolescents with more mental health challenges have lower perceptions of self-esteem, autonomy and community relationships. Additionally, this study explored only four types of adverse life experiences comprising the latent risk factor, partly due to the sensitive age of the participants. Future studies may consider expanding the risk factors measured (e.g. sexual abuse, community violence).
This study used cross-sectional data and therefore causal associations cannot be determined. Longitudinal data would provide evidence about the direction of causal association and potential buffering effect of protective factors on risk factors. The relationships between risk and protective factors and mental health outcomes are complex and longitudinal data are needed to examine the temporal and/or reciprocal relationships between risk and protective factors on mental health. Further, longitudinal data would allow modeling relative strengths of protective and promotive paths over time and could reveal important latent class trajectories of mental health.
Conclusion
In a sample of vulnerable adolescent orphans with high exposure to adverse life experiences and experiences of stigma, protective factors were significantly associated with reduced psychological symptoms and increased mental wellbeing. Results suggest that strong community relationships, self-esteem and autonomy may be important modifiable protective factors to target for intervention programming aimed at improving adolescent mental health.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the sensitive age of the study participants (10–15-year-old). These datasets are available from the corresponding author on reasonable request. The author will vet requests to be certain that appropriate IRB approvals and data safety guidelines are in place before distribution.
Acknowledgements
The authors would like to acknowledge Health for a Prosperous Nation (H-PON) for their work in recruiting study participants, obtaining consent and assent and administering the survey questionnaire. Special thanks to the District Municipal Officers and the National Statistics Board of Tanzania for supporting this work. The authors are grateful to the National Institute of Medical Research in Tanzania (NIMRI) for approving this study. Most of all the authors would like to thank the adolescent participants for their participation in the study and their guardians and advocates for supporting participation in the study.
Authors contribution
The original study was conceived of and designed by MC. Development of survey instruments was completed by MC and PN. Data analysis and interpretation was completed by MC, EH, JL, RD. Manuscript preparation was completed by MC, RD, JL, SB, EH, PS and PN. All authors have contributed critically and significantly to drafting a final manuscript. All authors read and approved of the final manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. Research Interests include Adolescent health, global health, mental health.
Ethics statement
Institutional Review Board Statement: The study was conducted in accordance with the Declaration of Helsinki and was approved by an Institutional Review Board/Ethics committee.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Ahmad, I., Smetana, J. G., & Klimstra, T. (2015). Maternal monitoring, adolescent disclosure, and adolescent adjustment among Palestinian refugee youth in Jordan. Journal of Research on Adolescence, 25(3), 403–411. https://doi.org/10.1111/jora.12133
- Allen, J. P., & Loeb, E. L. (2015). The autonomy-connection challenge in adolescent–peer relationships. Child Development Perspectives, 9(2), 101–105. https://doi.org/10.1111/cdep.12111
- Ames, M. E., Rawana, J. S., Gentile, P., & Morgan, A. S. (2015). The protective role of optimism and self-esteem on depressive symptom pathways among Canadian aboriginal youth. Journal of Youth and Adolescence, 44(1), 142–154. https://doi.org/10.1007/s10964-013-0016-4
- Anda, R. F., Croft, J. B., Felitti, V. J., Nordenberg, D., Giles, W. H., Williamson, D. F., & Giovino, G. A. (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA, 282(17), 1652–1658. https://doi.org/10.1001/jama.282.17.1652
- Aronson, J., Burgess, D., Phelan, S. M., & Juarez, L. (2013). Unhealthy interactions: The role of stereotype threat in health disparities. American Journal of Public Health (1971), 103(1), 50–56. https://doi.org/10.2105/AJPH.2012.300828
- Bachman DeSilva, M., Skalicky, A., Beard, J., Cakwe, M., Zhuwau, T., & Simon, J. (2012). Longitudinal evaluation of the psychosocial well-being of recent orphans compared with non-orphans in a school-attending cohort in KwaZulu-natal. South Africa. International Journal of Mental Health Promotion, 14(3), 162–182. https://doi.org/10.1080/14623730.2012.733600
- Barrett, P. (2007). Structural equation modelling: Adjudging model fit. Personality and Individual Differences, 42(5), 815–824. https://doi.org/10.1016/j.paid.2006.09.018
- Bentler, P. M. (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238. https://doi.org/10.1037/0033-2909.107.2.238
- Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., Ahluvalia, T., Stokes, J., Handelsman, L., Medrano, M., Desmond, D., & Zule, W. (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect, 27(2), 169–190. https://doi.org/10.1016/S0145-2134(02)00541-0
- Betancourt, T. S., Yang, F., Bolton, P., & Normand, S. L. (2014). Developing an African youth psychosocial assessment: An application of item response theory. International Journal of Methods in Psychiatric Research, 23(2), 142–160. https://doi.org/10.1002/mpr.1420
- Blum, R. W., Li, M., & Naranjo-Rivera, G. (2019). Measuring adverse child experiences among young adolescents globally: Relationships with depressive symptoms and violence perpetration. The Journal of Adolescent Health, 65(1), 86–93. https://doi.org/10.1016/j.jadohealth.2019.01.020
- Bomysoad, R. N., & Francis, L. A. (2020). Adverse childhood experiences and mental health conditions among adolescents. Journal of Adolescent Health, 67(6), 868–870. https://doi.org/10.1016/j.jadohealth.2020.04.013
- Cheng, C., Lau, H.-P. B., & Chan, M.-P. S. (2014). Coping flexibility and psychological adjustment to stressful life changes: A meta-analytic review. Psychological Bulletin, 140(6), 1582. https://doi.org/10.1037/a0037913
- Cherewick, M., Dahl, R. E., Rubin, D., Leiferman, J. A., & Njau, P. F. (2023). Psychometric validation of the collective asset Utu: associations with coping strategies and resilience during adolescence. Global Health Research and Policy, 8(1), 15. https://doi.org/10.1186/s41256-023-00303-4.
- Cherewick, M., Doocy, S., Tol, W., Burnham, G., & Glass, N. (2016). Potentially traumatic events, coping strategies and associations with mental health and well-being measures among conflict-affected youth in eastern democratic Republic of Congo. Global Health Research and Policy, 1(1), 1–18. https://doi.org/10.1186/s41256-016-0007-6
- Cherewick, M., Lebu, S., Su, C., & Dahl, R. E. (2020). An intervention to enhance social, emotional, and identity learning for very young adolescents and support gender equity: Protocol for a pragmatic randomized controlled trial. JMIR Research Protocols, 9(12), e23071. https://doi.org/10.2196/23071
- Cherewick, M., Lebu, S., Su, C., Richards, L., Njau, P. F., & Dahl, R. E. (2021). Promoting gender equity in very young adolescents: Targeting a window of opportunity for social emotional learning and identity development. BMC Public Health, 21(1), 1–18. https://doi.org/10.1186/s12889-021-12278-3
- Cherewick, M., Tol, W., Burnham, G., Doocy, S., & Glass, N. (2016). A structural equation model of conflict-affected youth coping and resilience. Health Psychology and Behavioral Medicine, 4(1), 155–174. https://doi.org/10.1080/21642850.2016.1228458
- Cluver, L., Gardner, F., & Operario, D. (2009). Poverty and psychological health among AIDS-orphaned children in Cape Town, South Africa. AIDS Care, 21(6), 732–741. https://doi.org/10.1080/09540120802511885
- Cluver, L. D., Gardner, F., & Operario, D. (2008). Effects of stigma on the mental health of adolescents orphaned by AIDS. Journal of Adolescent Health, 42(4), 410–417. https://doi.org/10.1016/j.jadohealth.2007.09.022
- Corrigan, P. W., & Nieweglowski, K. (2021). Difference as an indicator of the self-stigma of mental illness. Journal of Mental Health, 30(4), 417–423. https://doi.org/10.1080/09638237.2019.1581351
- Crone, E. A., & Dahl, R. E. (2012). Understanding adolescence as a period of social–affective engagement and goal flexibility. Nature Reviews Neuroscience, 13(9), 636–650. https://doi.org/10.1038/nrn3313
- Deković, M., Buist, K. L., & Reitz, E. (2004). Stability and changes in problem behavior during adolescence: Latent growth analysis. Journal of Youth and Adolescence, 33(1), 1–12. https://doi.org/10.1023/A:1027305312204
- Doku, P. N., Akohene, K. M., Ananga, M. K., & Debrah, T. P. (2019). A systematic review of the mental health of orphans and vulnerable children within the context of HIV/AIDS in Africa. International Journal of Psychiatry, 4(2), 1–20. ISSN: 2475-5435.
- Doucette, A., & Bickman, L. (2001). Child adolescent measurement system (CAMS).
- Dube, S. R., Miller, J. W., Brown, D. W., Giles, W. H., Felitti, V. J., Dong, M., & Anda, R. F. (2006). Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 38(4), 444.e1–10. https://doi.org/10.1016/j.jadohealth.2005.06.006
- Earls, F., Raviola, G. J., & Carlson, M. (2008). Promoting child and adolescent mental health in the context of the HIV/AIDS pandemic with a focus on sub-Saharan Africa. Journal of Child Psychology and Psychiatry, 49(3), 295–312. https://doi.org/10.1111/j.1469-7610.2007.01864.x
- El-Gilany, A.-H., El-Bilsha, M. A., & Ibrahim, A. (2013). Gender differences in maladaptive cognitive schema in orphans in Dakahlia, Egypt. The Scientific World Journal, 2013, Article ID 373120. https://doi.org/10.1155/2013/373120.
- Escueta, M., Whetten, K., Ostermann, J., & O’Donnell, K. (2014). Adverse childhood experiences, psychosocial well-being and cognitive development among orphans and abandoned children in five low income countries. BMC International Health and Human Rights, 14(1), 1–13. https://doi.org/10.1186/1472-698X-14-6
- Fine, S. L., Malik, A., Guimond, M.-F., Nemiro, A., Temu, G., Likindikoki, S., Annan, J., & Tol, W. A. (2021). Improving mental health in low-resource settings: A feasibility randomized controlled trial of a transdiagnostic psychological intervention among Burundian refugee adolescents and their caregivers. Behaviour Research and Therapy, 145, 103944. https://doi.org/10.1016/j.brat.2021.103944
- Foster, G., Makufa, C., Drew, R., Mashumba, S., & Kambeu, S. (1997). Perceptions of children and community members concerning the circumstances of orphans in rural Zimbabwe. AIDS Care, 9(4), 391–405. https://doi.org/10.1080/713613166
- Funkquist, Å, Eriksson, B., & Muula, A. (2007). The vulnerability of orphans in Thyolo district, southern Malawi. Tanzania Journal of Health Research, 9(2), 102–109. https://doi.org/10.4314/thrb.v9i2.14311
- Green, B., Carroll, A., & Brett, A. (2010). Structured risk assessment in community forensic mental health practice. Australasian Psychiatry, 18(6), 538–541. https://doi.org/10.3109/10398562.2010.498513
- Griggs, S. (2017). Hope and mental health in young adult college students: An integrative review. Journal of Psychosocial Nursing and Mental Health Services, 55(2), 28–35. https://doi.org/10.3928/02793695-20170210-04
- Grootendorst-van Mil, N. H., Bouter, D. C., Hoogendijk, W. J. G., van Jaarsveld, S. F. L. M., Tiemeier, H., Mulder, C. L., & Roza, S. J. (2021). The iBerry study: A longitudinal cohort study of adolescents at high risk of psychopathology. European Journal of Epidemiology, 36(4), 453–464. https://doi.org/10.1007/s10654-021-00740-w
- Hailegiorgis, M. T., Berheto, T. M., Sibamo, E. L., Asseffa, N. A., Tesfa, G., & Birhanu, F. (2018). Psychological wellbeing of children at public primary schools in Jimma town: An orphan and non-orphan comparative study. PloS one, 13(4), e0195377. https://doi.org/10.1371/journal.pone.0195377
- Hancock, G. R., Mueller, R. O., & Stapleton, L. M. (2010). The reviewer's guide to quantitative methods in the social sciences. Routledge.
- Hawes, D. J., Lechowicz, M., Roach, A., Fisher, C., Doyle, F. L., Noble, S., & Dadds, M. R. (2021). Capturing the developmental timing of adverse childhood experiences: The adverse life experiences scale. The American Psychologist, 76(2), 253–267. https://doi.org/10.1037/amp0000760
- Henson, M., Sabo, S., Trujillo, A., & Teufel-Shone, N. (2017). Identifying protective factors to promote health in American Indian and Alaska native adolescents: A literature review. The Journal of Primary Prevention, 38(1-2), 5–26. https://doi.org/10.1007/s10935-016-0455-2
- Hermenau, K., Eggert, I., Landolt, M. A., & Hecker, T. (2015). Neglect and perceived stigmatization impact psychological distress of orphans in Tanzania. European Journal of Psychotraumatology, 6(1), 28617. https://doi.org/10.3402/ejpt.v6.28617
- Inguglia, C., Ingoglia, S., Liga, F., Lo Coco, A., & Lo Cricchio, M. G. (2015). Autonomy and relatedness in adolescence and emerging adulthood: Relationships with parental support and psychological distress. Journal of Adult Development, 22(1), 1–13. https://doi.org/10.1007/s10804-014-9196-8
- Inzlicht, M., McKay, L., & Aronson, J. (2006). Stigma as ego depletion: How being the target of prejudice affects self-control. Psychological Science, 17(3), 262–269. https://doi.org/10.1111/j.1467-9280.2006.01695.x
- Jörns-Presentati, A., Napp, A.-K., Dessauvagie, A. S., Stein, D. J., Jonker, D., Breet, E., Charles, W., Swart, R. L., Lahti, M., Suliman, S., Jansen, R., van den Heuvel, L. L., Seedat, S., & Groen, G. (2021). The prevalence of mental health problems in sub-Saharan adolescents: A systematic review. PLOS ONE, 16(5), e0251689. https://doi.org/10.1371/journal.pone.0251689
- Kabiru, C. W., Elung’ata, P., Mojola, S. A., & Beguy, D. (2014). Adverse life events and delinquent behavior among Kenyan adolescents: A cross-sectional study on the protective role of parental monitoring, religiosity, and self-esteem. Child and Adolescent Psychiatry and Mental Health, 8(1), 1–11. https://doi.org/10.1186/1753-2000-8-24
- Kline, R. B., & Santor, D. A. (1999). Principles & practice of structural equation modelling. Canadian Psychology, 40(4), 381. https://doi.org/10.1037/h0092500
- Koydemir, S., & Essau, C. A. (2018). Chapter 5 – anxiety and anxiety disorders in young people: A cross-cultural perspective. In M. Hodes, S. S.-F. Gau, & P. J. De Vries (Eds.), Understanding uniqueness and diversity in child and adolescent mental health (pp. 115–134). Academic Press.
- Kwaning, K., Wong, M., Dosanjh, K., Biely, C., & Dudovitz, R. (2021). Gender stigma awareness is associated with adolescent risky health behaviors. PLoS One, 16(5), e0251332. https://doi.org/10.1371/journal.pone.0251332
- Kyaruzi, E. (2022). Psychosocial wellbeing of orphaned children in selected primary schools in Tanzania. Heliyon, 8(11), e11347. https://doi.org/10.1016/j.heliyon.2022.e11347
- La Greca, A. M., & Harrison, H. M. (2005). Adolescent peer relations, friendships, and romantic relationships: Do they predict social anxiety and depression? Journal of Clinical Child and Adolescent Psychology, 34(1), 49–61. https://doi.org/10.1207/s15374424jccp3401_5
- Lee, N., Massetti, G. M., Perry, E. W., & Self-Brown, S. (2022). Adverse childhood experiences and associated mental distress and suicide risk: Results from the Zambia violence against children survey. Journal of Interpersonal Violence, 37(21–22), NP21244–NP2NP65. https://doi.org/10.1177/08862605211056726
- Luthar, S. S. (2006). Resilience in development: A synthesis of research across five decades.
- Mabrouk, A., Mbithi, G., Chongwo, E., Too, E., Sarki, A., Namuguzi, M., Atukwatse, J., Ssewanyana, D., & Abubakar, A. (2022). Mental health interventions for adolescents in sub-Saharan Africa: A scoping review. Frontiers in Psychiatry, 13, 1696. https://doi.org/10.3389/fpsyt.2022.937723
- Magson, N. R., Freeman, J. Y., Rapee, R. M., Richardson, C. E., Oar, E. L., & Fardouly, J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. https://doi.org/10.1007/s10964-020-01332-9
- Mahon, N. E., & Yarcheski, A. (2017). Parent and friend social support and adolescent hope. Clinical Nursing Research, 26(2), 224–240. https://doi.org/10.1177/1054773815619881
- Makame, V., Ani, C., & Grantham-McGregor, S. (2002). Psychological well-being of orphans in Dar El salaam, Tanzania. Acta Paediatrica, 91(4), 459–465. https://doi.org/10.1111/j.1651-2227.2002.tb01671.x
- Malika, N., Granillo, C., Irani, C., Montgomery, S., & Belliard, J. C. (2021). Chronic absenteeism: Risks and protective factors among low-income, minority children and adolescents. Journal of School Health, 91(12), 1046–1054. https://doi.org/10.1111/josh.13096
- Marais, L., Sharp, C., Pappin, M., Lenka, M., Cloete, J., Skinner, D., & Serekoane, J. (2013). Housing conditions and mental health of orphans in South Africa. Health & Place, 24, 23–29. https://doi.org/10.1016/j.healthplace.2013.08.004
- Masten, A. S. (2009). Ordinary magic: Lessons from research on resilience in human development. Education Canada, 49(3), 28–32. ISSN: ISSN-0013-1253.
- Masten, A. S. (2011). Resilience in children threatened by extreme adversity: Frameworks for research, practice, and translational synergy. Development and Psychopathology, 23(2), 493–506. https://doi.org/10.1017/S0954579411000198
- Masten, A. S. (2013). Global perspectives on resilience in children and youth. Child Development. https://doi.org/10.1111/cdev.12205
- McLaughlin, K. A., Garrad, M. C., & Somerville, L. H. (2022). What develops during emotional development? A component process approach to identifying sources of psychopathology risk in adolescence. Dialogues in Clinical Neuroscience. https://doi.org/10.31887/DCNS.2015.17.4/kmclaughlin.
- Meffert, S. M., Lawhorn, C., Ongeri, L., Bukusi, E., Campbell, H. R., Goosby, E., Bertozzi, S. M., & Kahonge, S. N. (2021). Scaling up public mental health care in sub-Saharan Africa: Insights from infectious disease. Glob Ment Health (Camb), 8, e41. https://doi.org/10.1017/gmh.2021.41
- Meinck, F., Cluver, L. D., Orkin, F. M., Kuo, C., Sharma, A. D., Hensels, I. S., & Sherr, L. (2017). Pathways from family disadvantage via abusive parenting and caregiver mental health to adolescent health risks in South Africa. Journal of Adolescent Health, 60(1), 57–64. https://doi.org/10.1016/j.jadohealth.2016.08.016
- Mersky, J. P., Topitzes, J., & Reynolds, A. (2013). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the US. Child Abuse & Neglect, 37(11), 917–925. https://doi.org/10.1016/j.chiabu.2013.07.011
- Michl, L. C., McLaughlin, K. A., Shepherd, K., & Nolen-Hoeksema, S. (2013). Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: Longitudinal evidence in early adolescents and adults. Journal of Abnormal Psychology, 122(2), 339–352. https://doi.org/10.1037/a0031994
- MoHCDGEC. 2016. Tanzania demographic and health survey and malaria indicator survey 2015-2016. Ministry of Health, Community Development Gender Elderly and Children (MoHCDGEC) Tanzania Mainland Ministry of Health - MoH. . Zanzibar National Bureau of Statistics, N.B.S. Tanzania Office of Chief Government Statistician, OCGS Zanzibar ICF.
- Morantz, G., Cole, D., Vreeman, R., Ayaya, S., Ayuku, D., & Braitstein, P. (2013). Child abuse and neglect among orphaned children and youth living in extended families in sub-Saharan Africa: What have we learned from qualitative inquiry? Vulnerable Children and Youth Studies, 8(4), 338–352. https://doi.org/10.1080/17450128.2013.764476
- Morrow, V. (1999). Conceptualising social capital in relation to the well-being of children and young people: A critical review. The Sociological Review, 47(4), 744–765. https://doi.org/10.1111/1467-954X.00194
- Msoka, A., & Holroyd, E. (2018). Children’s perspectives of their psychosocial wellbeing in Tanzanian orphanages. International Journal of Nursing and Midwifery, 10(5), 41. https://doi.org/10.5897/IJNM2017.0292
- Mwakanyamale, A. A., & Yizhen, Y. (2019). Psychological maltreatment and its relationship with self-esteem and psychological stress among adolescents in Tanzania: A community based, cross-sectional study. BMC Psychiatry, 19(1), 1–9. https://doi.org/10.1186/s12888-019-2139-y
- Noom, M., Deković, M., & Meeus, W. (2001). Conceptual analysis and measurement of adolescent autonomy. Journal of Youth and Adolescence, 30(5), 577–595. https://doi.org/10.1023/A:1010400721676
- Nosheen, A., Riaz, M. N., Malik, N. I., Yasmin, H., & Malik, S. (2017). Mental health outcomes of sense of coherence in individualistic and collectivistic culture: Moderating role of social support. Pakistan Journal of Psychological Research, 32(2).
- Ntozi, J. P., & Mukiza-Gapere, J. (1995). Care for AIDS orphans in Uganda: Findings from focus group discussions. Health Transition Review, 5, 245–252. http://www.jstor.org/stable/40652170.
- O’Callaghan, P., Branham, L., Shannon, C., Betancourt, T. S., Dempster, M., & McMullen, J. (2014). A pilot study of a family focused, psychosocial intervention with war-exposed youth at risk of attack and abduction in north-eastern democratic Republic of Congo. Child Abuse & Neglect, 38(7), 1197–1207. https://doi.org/10.1016/j.chiabu.2014.02.004
- Ong, A. D., Cerrada, C., Lee, R. A., & Williams, D. R. (2017). Stigma consciousness, racial microaggressions, and sleep disturbance among Asian Americans. Asian American Journal of Psychology, 8(1), 72. https://doi.org/10.1037/aap0000062
- Pascoe, E. A., & Smart Richman, L. (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531–554. https://doi.org/10.1037/a0016059
- Patton, G. C., Sawyer, S. M., Santelli, J. S., Ross, D. A., Afifi, R., Allen, N. B., Arora, M., Azzopardi, P., Baldwin, W., Bonell, C., Kakuma, R., Kennedy, E., Mahon, J., McGovern, T., Mokdad, A. H., Patel, V., Petroni, S., Reavley, N., Taiwo, K., … Viner, R. M. (2016). Our future: A lancet commission on adolescent health and wellbeing. The Lancet, 387(10036), 2423–2478. https://doi.org/10.1016/S0140-6736(16)00579-1
- Pine, D. S., Cohen, P., & Brook, J. S. (2001). Emotional reactivity and risk for psychopathology among adolescents. CNS Spectrums, 6(1), 27–35. https://doi.org/10.1017/S1092852900022860
- Puffer, E. S., Drabkin, A. S., Stashko, A. L., Broverman, S. A., Ogwang-Odhiambo, R. A., & Sikkema, K. J. (2012). Orphan status, HIV risk behavior, and mental health among adolescents in rural Kenya. Journal of Pediatric Psychology, 37(8), 868–878. https://doi.org/10.1093/jpepsy/jss077
- Rosenberg, M. (2015). Society and the adolescent self-image. Princeton University Press. 339 p.
- Rutter, M. (2000). Resilience reconsidered: Conceptual considerations, empirical findings, and policy implications.
- Schilling, E. A., Aseltine, R. H., & Gore, S. (2007). Adverse childhood experiences and mental health in young adults: A longitudinal survey. BMC Public Health, 7(1), 1–10. https://doi.org/10.1186/1471-2458-7-30
- Schneiders, J., Nicolson, N. A., Berkhof, J., Feron, F. J., Van Os, J., & Devries, M. W. (2006). Mood reactivity to daily negative events in early adolescence: Relationship to risk for psychopathology. Developmental Psychology, 42(3), 543. https://doi.org/10.1037/0012-1649.42.3.543
- Sequeira, M., Singh, S., Fernandes, L., Gaikwad, L., Gupta, D., Chibanda, D., & Nadkarni, A., (2022). Adolescent health series: The status of adolescent mental health research, practice and policy in sub-Saharan Africa: A narrative review. Tropical Medicine & International Health, 27(9), 758–766. https://doi.org/10.1111/tmi.13802
- Sharpe, D., Rajabi, M., Chileshe, C., Joseph, S. M., Sesay, I., Williams, J., & Sait, S. (2021). Mental health and wellbeing implications of the COVID-19 quarantine for disabled and disadvantaged children and young people: Evidence from a cross-cultural study in Zambia and Sierra Leone. BMC Psychology, 9(1), 1–15. https://doi.org/10.1186/s40359-021-00583-w
- Sonderegger, R., Rombouts, S., Ocen, B., & McKeever, R. S. (2011). Trauma rehabilitation for war-affected persons in northern Uganda: A pilot evaluation of the EMPOWER programme. British Journal of Clinical Psychology, 50(3), 234–249. https://doi.org/10.1348/014466510X511637
- Sörbom, D. (1989). Model modification. Psychometrika, 54(3), 371–384. https://doi.org/10.1007/BF02294623
- Stansfeld, S. A., Rothon, C., Das-Munshi, J., Mathews, C., Adams, A., Clark, C., & Lund, C. (2017). Exposure to violence and mental health of adolescents: South African health and well-being study. BJPsych Open, 3(5), 257–264. https://doi.org/10.1192/bjpo.bp.117.004861
- StataCorp. (2017). Stata statistical software (15th ed.). StataCorp LLC.
- Steiger, J. H., & Lind, J. C. (1980). Statistically based tests for the number of common factors. Paper presented at the Annual Meeting of the Psychometric Society, Iowa City.
- Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3), 411. https://doi.org/10.1037/0033-295X.107.3.411
- Thomas, T., Tan, M., Ahmed, Y., & Grigorenko, E. L. (2020). A systematic review and meta-analysis of interventions for orphans and vulnerable children affected by HIV/AIDS worldwide. Annals of Behavioral Medicine, 54(11), 853–866. https://doi.org/10.1093/abm/kaaa022
- Tol, W. A., Song, S., & Jordans, M. J. (2013). Annual research review: Resilience and mental health in children and adolescents living in areas of armed conflict – a systematic review of findings in low-and middle-income countries. Journal of Child Psychology and Psychiatry, 54(4), 445–460. https://doi.org/10.1111/jcpp.12053
- Triana, R., Keliat, B. A., & Sulistiowati, N. M. D. (2019). The relationship between self-esteem, family relationships and social support as the protective factors and adolescent mental health. Humanities & Social Sciences Reviews, 7(1), 41–47. https://doi.org/10.18510/hssr.2019.715
- Tsehay, M., Necho, M., & Mekonnen, W. (2020). The role of adverse childhood experience on depression symptom, prevalence, and severity among school going adolescents. Depression Research and Treatment, 2020, Article ID 5951792. https://doi.org/10.1155/2020/5951792.
- Tucker, L. R., & Lewis, C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38(1), 1–10. https://doi.org/10.1007/BF02291170
- UNDP. (2017). Tanzania human development report 2017 – social policy in the context of economic transformation. United Nations Development Programme. Tanzania Office, Economic and Social Research Foundation; 2018 2018. Report No.: 978-9976-5231-8-8.
- Ungar, M. (2012). Researching and theorizing resilience across cultures and contexts. Preventive Medicine, 55(5), 387–389. https://doi.org/10.1016/j.ypmed.2012.07.021
- UNICEF. (2009). The state of the world’s children.
- UNICEF. (2019). The state of the world’s children: Children, food and nutrition – growing well in a changing world.
- Werner, E. E. (1992). The children of Kauai: Resiliency and recovery in adolescence and adulthood. Journal of Adolescent Health, 13(4), 262–268. https://doi.org/10.1016/1054-139X(92)90157-7
- Whetten, K., Ostermann, J., Whetten, R., O'Donnell, K., Thielman, N., & Team, P. O. F. O. R. (2011). More than the loss of a parent: Potentially traumatic events among orphaned and abandoned children. Journal of Traumatic Stress, 24(2), 174–182. https://doi.org/10.1002/jts.20625
- Wild, L. G., Flisher, A. J., & Robertson, B. A. (2013). Risk and resilience in orphaned adolescents living in a community affected by AIDS. Youth & Society, 45(1), 140–162. https://doi.org/10.1177/0044118X11409256
- Williams, D. R., Yan, Y., Jackson, J. S., & Anderson, N. B. (1997). Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351. https://doi.org/10.1177/135910539700200305
- Wingenfeld, K., Schäfer, I., Terfehr, K., Grabski, H., Driessen, M., Grabe, H., Löwe, B., & Spitzer, C. (2011). [The reliable, valid and economic assessment of early traumatization: First psychometric characteristics of the German version of the adverse childhood experiences questionnaire (ACE)]. Psychotherapie, Psychosomatik, Medizinische Psychologie, 61(1), e10–e14. https://doi.org/10.1055/s-0030-1263161
- World Health Organization. (2023). Constitution of the world health organization.
- Zhang, Y., Zhang, X., Zhang, L., & Guo, C. (2019). Executive function and resilience as mediators of adolescents’ perceived stressful life events and school adjustment. Frontiers in Psychology, 10. https://doi.org/10.3389/fpsyg.2019.00446
