ABSTRACT
Objective
The COVID-19 pandemic has affected how people go about their daily lives, often in various and substantial ways. This study aims to prospectively evaluate the changes in social participation during the COVID-19 pandemic in persons with a high risk for a severe COVID-19 course in Germany.
Methods
A paper-pencil-based survey was conducted starting at March 2021. Participants filled out questionnaires at four time points based on their COVID-19 vaccination status: before COVID-19 vaccination, one month, six months and twelve months after COVID-19 vaccination. Social participation measures included the Pandemic Social Participation Questionnaire (PSP-Q) and the Index for measuring participation restrictions (IMET). Repeated measures ANOVA and paired t-test were used to test for changes between time-points. Repeated measures correlation was used to assess the relationship between social participation and local COVID-19 incidences.
Results
Data from 245 participants was analyzed before and one month after COVID-19 vaccination. In addition, data from 156 participants was analyzed at time points one, six and twelve months after COVID-19. PSP-Q and IMET scores changed significantly after participants received a COVID-19 vaccination. Between one month and twelve months after vaccination, social participation improved significantly measured by PSP-Q. Social participation was negatively correlated with regional COVID-19 incidences before and after COVID-19 vaccination. Social participation was positively correlated with COVID-19 incidences between one month and twelve months after COVID-19 vaccination.
Conclusions
Social participation improved in persons with a high risk for a severe COVID-19 course during the pandemic. The local COVID-19 incidence showed a negative association with social participation only until the fall of 2021 when it was used as the sole metric to regulate COVID-19 protective measures. Although our data describes the trends in social participation, further studies are needed to identify the influencing factors for the observed increase in social participation.
1. Introduction
In the beginning of 2020, the newly evolved severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spread over the world (Wang et al., Citation2020). Until now, the Coronavirus disease 2019 (COVID-19) has caused millions of deaths worldwide. Despite the availability of efficient vaccines in and less harmful virus variants like delta and omicron should not obscure the fact that COVID-19 is still a threat as it may cause long-lasting impairments (Long COVID). Various research has highlighted that certain pre-existing conditions or higher age are associated with an increased risk for severe or even fatal cause of COVID-19 (Richardson et al., Citation2020; Sudre et al., Citation2021). This includes immunocompromised people, e.g. who received a solid organ transplant, with rheumatological diseases or with a malignant hematologic disease. These persons are at particular risk for a fatal cause due to the impairment of their immune system (Akalin et al., Citation2020; Galmiche et al., Citation2022; Gianfrancesco et al., Citation2020; He et al., Citation2020; Nair et al., Citation2020; Pereira et al., Citation2020; Webb et al., Citation2020). In addition, some medications that lead to immunosuppression, advanced age and oncologic/hematologic diseases are associated with lower or absent formation of antibodies to COVID-19 and a higher risk of SARS-CoV-2 infection after COVID-19 vaccination (Arregocés-Castillo et al., Citation2022; Fendler et al., Citation2022; Lee et al., Citation2022; Shen et al., Citation2022).
The uncertainty towards the risk of infection even after receiving a vaccination and subsequently applied individual measures to prevent infection may have negatively impacted social participation and mental health of people with a high risk for a severe COVID-19 course. Regardless of this risk, research has shown that the COVID-19 pandemic including lockdowns and restrictions impacted significantly the social lives of many (Karing, Citation2021; Wessels et al., Citation2022). There were two ‘lockdowns’ in Germany in which businesses and services deemed ‘non-essential’ were closed (including schools and kindergartens). Furthermore, authorities restricted gatherings, e.g. individuals may only have contact with a certain number of other people outside their own household. The first lockdown took place for three weeks from 22 March 2020. After that, the non-essential stores and services were reopened depending on the regional COVID-19 incidence. The second lockdown was implemented on December 16th, 2020, until March 03rd, 2021. Thereafter, measures were released in regions with a 7-day COVID-19 incidence of less than 50 per 100,000 inhabitants (Bundesregierung, Citation2021). Beginning 22 November 2021, in addition to COVID-19 incidence, ICU bed occupancy, and COVID-19 hospitalization rates were used as metrics to guide regional COVID-19 measures. As a result, people spent larger part of their day at home with less contact to others (Karing, Citation2021; Wessels et al., Citation2022), doing homeschooling (Dietrich et al., Citation2021), performing work at home office (Schmid et al., Citation2021). Also, the usage of digital tools that help to maintain social participation despite lockdowns and restrictions (Bürgel et al., Citation2023; Skulmowski & Rey, Citation2020).
Social participation was used as an outcome measure during the COVID-19 pandemic comparing the time points before and after the pandemic and various time points during the pandemic. A decline in social participation during the pandemic compared to before the pandemic could be observed (Im Ryu et al., Citation2022; Mergel & Schützwohl, Citation2021). During the pandemic home confinement impacted social participation negatively (Ammar et al., Citation2020). Also, a reduction in social participation was observed in longitudinal studies during the pandemic in older adults (Gough et al., Citation2023; Mergel & Schützwohl, Citation2021; Morrison et al., Citation2022; Noguchi et al., Citation2021). The decrease in social participation was during the pandemic was associated with a decrease in social participation and the onset of depressive symptoms (Morrison et al., Citation2022; Noguchi et al., Citation2021). Older adults are largely the focus of social participation studies because they are at high risk for severe COVID-19 progression. Other at-risk groups, such as immunosuppressed individuals or individuals with hematologic/oncologic diseases, are rarely included in studies on social participation, although they have been associated with impaired social participation (Guida et al., Citation2020; Prihodova et al., Citation2015; Su et al., Citation2022). All studies conducted so far during the pandemic collected data at the onset of the pandemic in 2020, but the pandemic situation changed over time with, for example, the introduction of COVID-19 vaccination, SARS-CoV-2 virus variants, and media coverage on COVID-19. In addition, due to the novelty of the pandemic situation, the available social participation instruments at the onset of the pandemic did not fully account for pandemic-related impairments and researchers used newly developed or modified instruments. However, these were validated (Schröder et al., Citation2022).
As the risk and risk perception for a severe COVID-19 infection changed during the pandemic this study explores the social participation of persons with a high risk for a severe COVID-19 longitudinal. The following hypotheses were tested:
H1: Social participation improves after an individual receives COVID-19 immunization compared to before.
As studies reported that COVID-19 immunization in non-immunocompromised people is associated with a perception of being protected (Caserotti et al., Citation2021; Graffigna et al., Citation2020; Hilverda & Vollmann, Citation2021) an increase in social participation after vaccination among immunocompromised individuals is plausible. It is important to note that some of the COVID-19 vaccines are less effective for this vulnerable group than for the general population.
H2: Social participation is associated with pandemic factors (COVID-19 incidence and booster vaccination).
COVID-19 incidence rates in Germany during the study period were considered an metric to guide authorities in applying measures to mitigate the spread of the virus. These results e.g. in restriction of gatherings that might have impacted social participation (Änderungen, Citation2021; Bundesärztekammer, Citation2021). Moreover, an additional booster vaccination against COVID-19 was recommended by the Standing Committee on Vaccination (STIKO) in winter 2021 to maintain protection after basic immunization. This could further increase the perceived protection in individuals with immunosuppression (Adams et al., Citation2022; King et al., Citation2021). Hence, we hypothesize that these factors are associated with social participation.
H3: Mental health improves after COVID-19 vaccination compared to before the vaccination.
Previous studies indicate an association between social participation and mental health (Chiao et al., Citation2011; Ding et al., Citation2022; Douglas et al., Citation2017). As COVID-19 vaccination has been shown to reduce pandemic-related anxiety (Chourpiliadis et al., Citation2023), we hypothesize that COVID-19 vaccination will improve mental health.
H4: Changes in social participation differ across sociodemographic (gender, age, city resident size, domestic situation) and medical factors (comorbidities and degree of disability).
Because risk and risk perception for a severe COVID-19 course also differ among sociodemographic factors (Booth et al., Citation2021; Cipolletta et al., Citation2022; Kowsar et al., Citation2023), we hypothesize that changes in social participation during the COVID-19 pandemic are also associated with certain sociodemographic factors.
2. Methods
2.1. Research design and study participants
This study is part of the longitudinal, prospective, two-center COVID-19 Contact-Immune study (CoCo Immune study) conducted in Germany’s Federal State Lower Saxony (Dopfer-Jablonka et al., Citation2022). Beginning in March 2021 participants were eligible if they were (1) 18 years or older, (2) able to provide informed consent, (3) had knowledge of German language and (4) had a high risk of a severe COVID-19 course (a) due to regular intake of an immunosuppressive medication (b), current or former (up to 5 years) myeloid or lymphatic disease without anti-CD20 directed therapy or solid tumor under checkpoint inhibition or (c) due to older age (80 years or older). Exclusion criteria included refusal/inability to provide informed consent, (2) contraindication to blood testing, (3) inability to declare consent.
Multiple recruitment strategies were used. At first, potential participants were informed by local media reports, posters and leaflets in general practices, mass vaccination sites, and hospitals in the Federal State of Lower Saxony. Interested participants who contacted the study team and were eligible were subsequently enrolled in the study. In addition, individuals that attended the outpatient clinics of the Department of Rheumatology and Immunology of the Hannover Medical School or the Department of Hematology and Medical Oncology of the University Medical Center Göttingen and met our inclusion criteria were enrolled. Thus, this study is based on a pragmatic non-random sample (real-life sample).
Due to the COVID-19 pandemic, the entire study was conducted in a contact-minimized manner. Enrollment in the study and obtaining consent from participants were performed by either video teleconference call, phone call, or in person, whichever participants preferred. Study materials were mailed to participants with prepaid return envelopes. Study participants returned questionnaires independently to the study team by mail. All participants were informed that all required preventive measures should be taken and all regulations should be followed as proposed by governmental sites. Additional information regarding the CoCo Immune study can be gathered from the study protocol (Dopfer-Jablonka et al., Citation2022).
2.2. Variables
2.2.1. Pandemic social participation questionnaire (PSP-Q)
Social participation is a broad term and can be defined as an individual’s involvement in activities providing interaction with others in community life and in important shared spaces (Levasseur et al., Citation2022). It is highly personalized and based on individual priorities, motivations and interests. Thus, quantifying social participation can be challenging. Social participation can be measured either using data about actual participation in community-based activities (e.g. counting how often a person is involved in activities) (Noguchi et al., Citation2021) or using questionnaires reflecting the current social participation of the person (Howrey & Hand, Citation2019; Schröder et al., Citation2022). Social participation is a modifiable determinant of health and is positively associated with positive health outcomes. Health-related quality of life, loneliness, well-being and outcomes like mortality, physical and mental health are all associated with social participation whereby a higher social participation is associated with positive health outcomes (Douglas et al., Citation2017; Fain et al., Citation2022; Levasseur et al., Citation2010; Takagi et al., Citation2013).
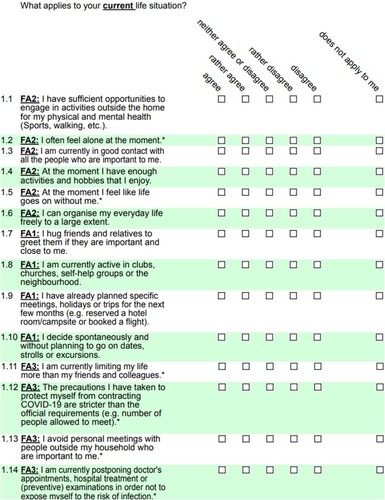
The primary measure used in this study was the PSP-Q (Schröder et al., Citation2022). The PSP-Q was developed during the first year of the pandemic to reflect social participation during the COVID-19 pandemic. It consists of 14 items and can be subdivided into three subscales reflecting well-being (6 items), active social participation (4 items) and restrictions (4 items). Each item is a statement which is rated on a five-point Likert-scale ranging from 1 = strongly agree to 5 = strongly disagree. When the statement does not concern the person filling in the questionnaire ‘not applicable’ can be chosen instead of the Likert-scale (Figure A1). To calculate the score of the measure negative items are reversed and summed up. Statements rated as ‘not applicable’ are depending on the pooling of the item rated as either ‘strongly disagree’ or ‘strongly agree’. The purpose of this is that aspects of social life that do not apply to a particular person cannot be considered a priori as lacking or impaired social participation. Higher scores indicate a higher social participation with scores ranging between 14 and 70. The questionnaire was validated with baseline data from the CoCo Immune study in German language (Schröder et al., Citation2022).
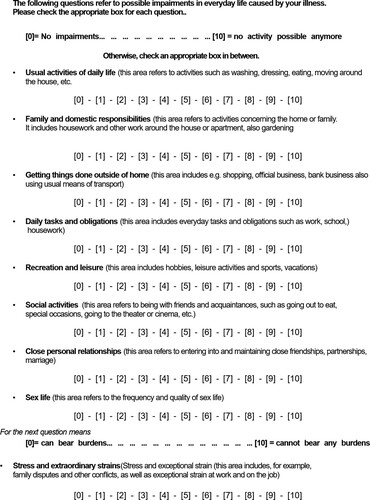
2.2.2. Index for measuring participation restriction (IMET)
The IMET is a unidimensional measure and reflects restrictions of social participation with 9 items (Takagi et al., Citation2013). Each item is rated on a 11-point Likert-scale where 0 represents no restrictions of social participation and 10 the highest restrictions possible (Figure A2). The IMET is based on the International Classification of Functioning, Disability and Health (ICF) and was primarily used in rehabilitative science in persons with chronic diseases (Deck et al., Citation2011; Citation2015; Takagi et al., Citation2013). Each item of the IMET represents one domain of participation based on the ICF classification. The IMET was validated in German language only. The IMET is used in various studies to measure social participation (Deck et al., Citation2015; Hueppe et al., Citation2014; Mergel & Schützwohl, Citation2021; Schützwohl & Mergel, Citation2020). Mergel & Schützwohl used the IMET in the general population and persons with a mental disorder to assess changes of social participation before and during the pandemic with a longitudinal study design (Mergel & Schützwohl, Citation2021; Schützwohl & Mergel, Citation2020).
2.2.3. Patient health questionnaire-4 (PHQ-4)
The PHQ-4 is an ultra-short four item scale used to screen for depression and anxiety symptoms (Löwe et al., Citation2010; Tillinger, Citation2015). The PHQ-4 consists of the two subscales ‘Patient Health Questionnaire-2’ (PHQ-2) and ‘Generalized Anxiety Disorder Scale-2’ (GAD-2). Each subscale is represented by two items, and each is rated on a four-point Likert-scale (0-3). An overall psychological distress sum score ranging between 0 and 12 can be calculated. Higher scores indicate higher anxiety and depression symptoms with values ≥3 on either subscale or values ≥6 on the overall indicating symptoms of clinically relevant anxiety or depression symptoms (Tillinger, Citation2015). Compared to the Brief Symptom Inventory, the PHQ-4 has a specificity of 94.5% and sensitivity of 51.6% with a high reliability (Kerper et al., Citation2014).
2.2.4. Pandemic-specific variables
Pandemic-specific variables include when a participant received their COVID-19 immunizations (including booster shots), daily COVID-19 incidence in the county Göttingen, Lower Saxony, Germany. County Göttingen was chosen as most participants were recruited there.
Data regarding the booster dose against COVID-19 were extracted if available from an additional telephone follow-up. COVID-19 incidence rates per 100,000 residents were retrieved from the national Institute for Public Health (Robert Koch-Institut) (Robert Koch-Institut, Citation2023). Telephone follow-up was conducted between December 7th 2021 and January 24th 2022. A full COVID-19 vaccination was defined as 14 days after two vaccination shots (BNT162b2 (Polack et al., Citation2020), mRNA-1273 (Baden et al., Citation2021) or AZD1222 (Voysey et al., Citation2021)) or after one in case Ad26.COV2.S (Sadoff et al., Citation2021) was used. An additional vaccination shot against COVID-19 was defined as booster vaccination.
2.2.5. Participants’ characteristics
As participant characteristics sociodemographic factors sex, age, school education, city resident size and domestic situation were included. Age was collected in years and categorized in <40 years, 40–65 years and older than 65 years. School education was based on secondary school and classified in low (no or low secondary school diploma), medium (intermediate secondary school diploma) and high (college preparatory). City resident size was collected categorized (<5000; 5000–20,000; 20,000–100,000; > 100,000). To assess participants’ domestic situation, we asked whether they are parenting, single parent, living alone and/or providing nursing care to relatives. Additionally, medical variables were collected describing the participants’ risk group for a severe COVID-19 course (80 + years, immunosuppressed and/or active oncological treatment) and comorbidities and degree of impairment (0% no impairment; 20–49% low impairment; 50–74% moderate impairment; 75–100% severe impairment). The degree of impairment is based on the German social law measuring physical, mental and social impairments (Sozialgesetzbuch, Citation2022). Degree of impairment varies between 0% and 100% while persons above 20% are eligible for disability assistance and may receive additional benefits. All sociodemographic characteristics were collected in the baseline questionnaire.
2.3. Time points
This study includes two separate analyses, depending upon the vaccination status at baseline and completeness of data at the studied time points. First, participants were grouped depending on whether they were fully vaccinated (at least 14 days after two vaccination shots or after one in case the COVID-19 Vaccine Janssen was used) or not at baseline. Participants who were not fully vaccinated at baseline were examined at the time points before complete vaccination (T0) and 1 month after complete vaccination (T1). Participants who were already fully vaccinated at baseline were excluded from this analysis.
Second, we performed an analysis of the participants who completed all questionnaires at all post-vaccination time points. Data were collected at the following time points: 1 month (T1), 6 months (T2) and 12 months after complete vaccination (T3). Because we examined only the time points after COVID-19 vaccination in this analysis, all participants with complete time series data sets were included in the analysis, regardless of their vaccination status at baseline.
2.4. Statistical analysis
For the statistical analysis, recruited participants were excluded if they did not complete the whole IMET and PSP-Q questionnaires for the analyzed timepoints. Sociodemographic and medical participant characteristics were reported for each of the two analyzed time periods. Data was reported with number of participants in each variable and corresponding proportion. Changes in measures and their subscales over time are tested using either a paired t-test when comparing two time points or one-way repeated measures analysis of variance when comparing three time points as the differences between the time points of all measures are approximately normally distributed. Analysis of the subscales can provide insight into which of the dimensions are changing in a multidimensional construct. Normal distribution of the differences between the time points was checked with Quantile-Quantile plots and histograms. A Bonferroni corrected post-hoc t-test is performed when testing more than two time points. The effect sizes Hedges g and ηp2 are calculated when changes between two or more than two timepoints are compared, respectively. Values of 0.2, 0.5 and 0.8 for Hedges G and values of 0.01, 0.06 and 0.14 for ηp2 are interpreted as a small, medium and large effect size, respectively (Cohen, Citation1988). When testing changes in subscales of the measure the p-values are adjusted using Bonferroni method according to the number of subscales included in the tested instrument. COVID-19 incidences will be tested for an association with social participation using repeated correlation measures. According to Cohen, a correlation coefficient of 0.1, 0.3 and 0.5 is interpreted as a small, moderate, and strong association between two variables (Cohen, Citation1988). A possible influence of the booster vaccination on changes in social participation will be tested using a t-test for two independent samples between participants with and without booster vaccination. Changes in social participation will be tested between sociodemographic and medical factors using an independent t-test when comparing two groups and one-way analysis of variance when comparing more than two groups.
All statistical analyses and data visualizations were performed using R Version 4.2.2 with the packages ggplot2 (Hadley, Citation2016), rstatix (Kassambara, Citation2022) and rmcorr (Bakdash & Marusich, Citation2017).
2.5. Research ethics
The study received approval from the responsible ethics boards of Hannover Medical School (9948_BO_K_2021) and University Medical Center Göttingen (29/3/21). The study is registered in the German register for clinical trials (DRKS00023972).
3. Results
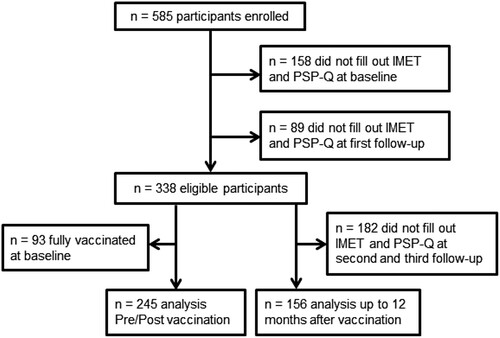
In the study, 585 participants were enrolled from which 338 filled out the PSP-Q and IMET completely. From the 338 participants, 93 were fully vaccinated at baseline. In total 245 participants were included which were not vaccinated at the beginning of the study and fully completed the IMET and PSP-Q questionnaire before and 1 month after basic vaccination. 156 participants completed all IMET and PSP-Q items for the time points 1 month after vaccination, 6 months after vaccination and 12 months after vaccination ().
Figure 1. Flowchart.
3.1. Participants’ characteristics
Most of the enrolled participants in both analyzed time periods were women between 40–65 years (Pre/Post vaccination: n = 141 (57.6%); T1-T2-T3: n = 100 (64.1%)) and had a high secondary school education (Pre/Post vaccination: n = 127 (51.8%); T1-T2-T3: n = 80 (51.3%)). About one-fifth of the participants in both cohorts were parenting at least on child (Pre/Post vaccination: n = 54 (22.0%); T1-T2-T3: n = 27 (17.3%)) and about one-fifth of the participants were living alone (Pre/Post vaccination: n = 53 (21.6%); T1-T2-T3: n = 26 (16.7%)). Most frequent comorbidities were hypertension (Pre/Post vaccination: n = 85 (34.7%); T1-T2-T3: n = 60 (38.5%)), followed by depressive disorder (Pre/Post vaccination: n = 23 (9.4%); T1-T2-T3: n = 14 (9.0%)) and diabetes type 2 (Pre/Post vaccination: n = 15 (6.1%); T1-T2-T3: n = 10 (6.4%)) in both groups. The most common COVID-19 risk groups were immunosuppressed (Pre/Post vaccination: n = 165 (67.3%); T1-T2-T3: n = 101 (64.7%)) followed by participants undergoing an active oncological treatment (Pre/Post vaccination: n = 141 (35.1%); T1-T2-T3: n = 100 (39.7%)) and participants 80 years or older (Pre/Post vaccination: n = 4 (1.6%); T1-T2-T3: n = 10 (6.4%)). All participants’ characteristics can be found in stratified after the analyzed time points ().
Table 1. Participants characteristics.
Participants of the pre/post vaccination cohort completed the T0 questionnaire between March 3rd 2021 and August 18th 2021 (median: April 15th 2021) and the T1 questionnaire between March 27th 2021 and September 14th 2021 (median June 29th 2021). Participants of the T1 – T2 – T3 cohort completed the questionnaires between March 31st and September 28th (median: June 27th 2021), June 10th 2021 and February 19th 2022 (median: November 23th 2021) and between August 29th 2021 and September 20th 2022 (median: May 24th 2022), respectively.
3.2. Social participation and mental health after COVID-19 vaccination
In line with our hypothesis H1 social participation increased significantly after the vaccination in both the PSP-Q and IMET (). Investigating the subscales of both measures the subscales ‘Well-being’ and ‘Restrictions’ of the PSP-Q showed a significant change while IMET showed significant changes in the domains ‘Getting things done outside of home’, ‘Recreation and leisure’, ‘Social activities’ and ‘Close personal relationships’ between both time points. Thereby, a medium effect according to Hedges g was shown for the PSP-Q for the subscale ‘restrictions’ (Hedges g: 0.51, 95% CI [0.41; 0.61]) and for the IMET for ‘social activities’ (Hedges G: −0.60, 95% [−0.75; −0.44]). All other significant subscales showed a small effect (Hedges G < 0.50) before and after vaccination. Mental health measured with the PHQ-4, including the GAD-2 and PHQ-2 did not change before and after COVID-19 vaccination significantly contradicting hypothesis H3.
Table 2. Mean scores and differences before and one month after COVID-19 vaccination for all included measures.
Confirming our hypothesis H2 local COVID-19 incidence rates were negatively correlated with social participation. The IMET showed a small correlation whereby the PSP-Q showed a moderate correlation with the local COVID-19 incidence rate. The subscale ‘Restrictions’ of the PSP-Q had the highest correlation with the local COVID-19 incidence rates with a correlation coefficient of r = −0.57 which can be interpreted as a strong association ().
Table 3. Correlations between social participation before and 1 month after COVID-19 vaccination with COVID-19 incidence in the county Göttingen.
3.3. Social participation and mental health up to 12 months after vaccination
When comparing social participation up to 12 months after vaccination across three time points, a significant increase was observed in the PSP-Q and its subscales (). Post-hoc analysis revealed significant increase between the timepoints T1 – T3 and T2 – T3 of the PSP-Q. These significant changes were also found in the subscales ‘Active social participation’ and ‘Restriction’. The subscale ‘Well-being’ showed only a significant change between the timepoints T2 – T3. The IMET did not change significantly between the three time points, but the subdomain ‘Social activities’ showed a significant change with a small effect size between the time points T1 – T3 and T2 – T3. The scales measuring anxiety and depression symptoms did not change significantly over time.
Table 4. Mean scores and differences 1 month, 6 months and 12 months after COVID-19 vaccination for all included measures.
The incidence of the county Göttingen had a small significant positive correlation with the PSP-Q measure and the subscale ‘Active social participation’. The IMET and other subscales had a non-significant or negligible correlation with the COVID-19 incidence (). The incidence of the county Göttingen is shown in with the IMET and PSP-Q scores for each participant and the three timepoints after COVID-19 vaccination ().
Figure 2. Median and mean change of social participation after COVID-19 vaccination. Blue triangle: mean score and median date for each time point; purple line: secondary Y-Axis (Incidence per 100,000 residents [county Göttingen]).
![Figure 2. Median and mean change of social participation after COVID-19 vaccination. Blue triangle: mean score and median date for each time point; purple line: secondary Y-Axis (Incidence per 100,000 residents [county Göttingen]).](/cms/asset/17857623-b6e3-415b-8613-d2fbb4505245/rhpb_a_2249534_f0002_oc.jpg)
Table 5. Correlations between social participation 1 month, 6 months and 12 months after COVID-19 vaccination with COVID-19 incidence in the county Göttingen.
114 out of 156 participants were reached during follow-up regarding their booster vaccination. Between fully vaccinated participants who got an additional vaccination shot against COVID-19 between T1 and T2 (n = 43) and participants which did not get an additional vaccination shot (n = 71) no difference between the change of social participation measured with the PSP-Q (t(112) = −1.10, p = 0.27) and IMET (t(112) = −0.77, p = 0.44) was observed contradicting our hypothesis H2.
3.4. Association of participants’ characteristics with social participation changes
PSP-Q changes showed differences significant differences in the variables age (p = 0.04) and the comorbidity heart failure (p = 0.01) in line with hypothesis H4. Participants under 40 years showed a higher PSP-Q improvement (M = 7.59, SD = 6.61) compared to participants between 40 and 65 years (M = 2.96, SD = 8.72) and above 65 years (M = 2.32, SD = 9.23). Participants with the comorbidity heart failure (M = −10.00, SD = 11.14) showed a worsening between T1 and T3 compared to participants without heart failure (M = 3.61, SD = 8.55). The IMET did not change significantly between sociodemographic and medical factors up to 12 months after vaccination (Appendix – ).
4. Discussion
4.1. Summary of main findings
This study investigated the social participation before a COVID-19 vaccination and up to 12 months after a COVID-19 vaccination among people with a particular higher risk for a severe or even fatal course of COVID-19. Confirming with our hypothesis H1 social participation increased one month after COVID-19 vaccination significantly. The subscale of the PSP-Q representing pandemic-related restrictions due to the COVID-19 pandemic and the domain ‘Social activities’ of the IMET showed the highest effect sizes. An increased social participation was correlated with lower COVID-19 incidence before and one month after vaccination confirming with our hypothesis H2. Contradicting our hypothesis H3 mental health did not change one month after COVID-19 vaccination. After participants received a vaccination, the social participation increased using the PSP-Q even with the highest COVID-19 incidence levels measured during the pandemic. Changes in social participation between 1 and 12 months after COVID-19 vaccination differed between age groups and the comorbidity heart failure confirm our hypothesis H4 that the change in social participation differs between participant characteristics.
The reasons for a change in social participation can be manifold. One possible reason could be a change in risk perception during the pandemic. Schneider et al. (Citation2021) showed that a change in risk perception can be partly explained by an individualistic worldview, experience with the virus, trust in government and science, and personal risk (Schneider et al., Citation2021). Also, an increase in protective behaviors that can influence social participation could be observed with increasing risk perception. Qualitative studies may provide deeper insight into factors influencing risk perception during the COVID-19 pandemic. In a qualitative study from the United Kingdom, Hanna et al. (Citation2023) showed that people’s different views regarding COVID-19 emergence, transmission, and health consequences were partially inconsistent with the scientific consensus, and subjects themselves reported being overwhelmed by the abundance of information (Hanna et al., Citation2023). Also, subjects at high risk for severe COVID-19 disease estimated their individual risk to be low. An overestimation of the efficacy of COVID-19 vaccination may be present in our study, causing subjects who perceived their risk to be low to disregard protective behaviors. This could explain the increase in social participation. Already positive information about the existence of an effective vaccination against COVID-19 led to a lower willingness to adhere to protective measures in Sweden (Andersson et al., Citation2021). Another aspect could be a so-called pandemic fatigue, which is also influenced by risk perception. According to the WHO, pandemic fatigue describes a demotivation to follow the recommended protective measures over time (CitationWHO). Wu et al. (Citation2023) observed a sharp increase in pandemic fatigue after the start of the COVID-19 vaccination campaign (Wu et al., Citation2023).
This is to our knowledge the first study using the PSP-Q in a longitudinal study design. Therefore, the statistical effect size and change of the score cannot be compared with other studies or related to a clinically significant outcome. IMET norm data show that our cohort has a twice as high IMET score representing higher restrictions compared to persons between 50 and 59 years old (Deck et al., Citation2015). Mergel & Schützwohl used the individual IMET items before the first COVID-19 lockdown in Germany during the first lockdown and after relaxation of restrictions in normal population (Mergel & Schützwohl, Citation2021). The item ‘Social activities’ significantly declines during the lockdown and increases after the relaxation of the restrictions. Our study cohort showed a smaller increase in social participation in the item ‘Social activities’ before and after COVID-19 vaccination. Even 12 months after vaccination the item score is higher compared to a pre-pandemic population described in the literature. This could be due to the fact that our cohorts consist of persons with a high risk for a severe COVID-19 course including oncological patients and immunosuppressed participants which often have progressive chronic diseases. Therefore, a higher baseline of social participation restriction due to the underlying condition can be assumed. Similar to the findings of Mergel & Schützwohl in our cohort the items ‘Usual activities of daily life’, ‘Family and domestic responsibilities’, ‘Sex life’ and ‘Stress and extraordinary strain’ did not change significantly. The IMET score in our study can also be compared to persons with specific chronic conditions. Hüppe et al. collected IMET scores in persons with self-assessed need for a rehabilitation regarding their inflammatory bowel disease before the pandemic. Patients in this randomized trial had a mean IMET score of 34.68 in the rehabilitation group and 32.79 in the control group (Hüppe et al., Citation2020). The IMET score of our cohort about 33.31 before the COVID-19 vaccination is comparable to the patients with chronic bowel disease from Hüppe et al. (Hüppe et al., Citation2020).
COVID-19 incidence was between T0 and T1 negatively correlated with social participation. As social participation increased, the COVID-19 incidences decreased. After the vaccination up to 12 months COVID-19 incidence was positively correlated with social participation. One possible explanation for these contradicting results could be the perception of the severity of COVID-19 in the general population which may have changed during the pandemic with increasing vaccination rate over time in Germany, and with a dominance of delta (Florensa et al., Citation2022) and omicron (Hyams et al., Citation2023) SARS-CoV-2 variants that cause less severe courses. Another aspect could be pandemic fatigue where persons gradually over time are demotivated to follow recommended behaviors to minimize infection spread (Haktanir et al., Citation2022; Masten & Motti-Stefanidi, Citation2020). Also overall COVID-19 incidences were used as the only benchmark for regulating COVID-19 restrictions in Germany until 21st November 2021 (Änderungen, Citation2021; Bundesärztekammer, Citation2021). Another possible reason why COVID-19 incidences were not negatively correlated with social participation could be the changed benchmark for regulating COVID-19 restrictions. From 22nd November, 2021 a method containing the local COVID-19 hospitalization incidence rates, occupancy of intensive care beds was used in addition to COVID-19 incidence rates (Änderungen, Citation2021; Bundesärztekammer, Citation2021).
The mental health of the participants in our study did not change at any time point. Other studies were contradictory on changes in mental health during the pandemic. Costa et al. found a worsening of depressive, anxious and stress-related symptoms in the second home confinement (February 2021) compared with the home confinement in March 2020 in the Portuguese general population, while during the second home confinement, the COVID-19-related deaths were manifold compared to the first home confinement period (Costa et al., Citation2022; John Hopkins University, Citation2023). Self-reported mental health problems of three meta-analyses including longitudinal studies indicate small effect sizes during the COVID-19 pandemic compared to before the pandemic with high heterogeneity between the included studies (Patel et al., Citation2022; Prati & Mancini, Citation2021; Robinson et al., Citation2022). However, studies investigating vulnerable populations (e.g. older adults or persons with chronic conditions) showed higher mental health burden and loneliness compared to the general population (Deimel et al., Citation2022; Luchetti et al., Citation2020; Robinson et al., Citation2022).
4.2. Limitations
This study comes with several limitations. The sample is not representative of all persons with a high risk for a severe COVID-19 course in Germany. Included participants were mostly woman, had a high school education, were taking immunosuppressive medication and were proficient in the German language. Participants were recruited using a non-random convenience sample. Participants who did not send back their questionnaires or had incomplete data of the included measures were excluded from the statistical analysis. Also, not all participants were reached during the telephone follow-up to ask for a booster vaccination. Therefore, the results may be influenced by a selection and loss to follow-up bias. In addition, participants with limited or no knowledge of German were not included because the IMET and PSP-Q are validated only in German, which may underrepresent participants with migration status.
Participant data were collected at different time points because not all participants were recruited at the same time. Because of factors like governmental COVID-19 measures (e.g. lockdowns), virus variants or seasonal trends (weather, contagious disease) the social participation could have been influenced. Medical factors like disease progression/regression or changes in treatment could also influence the social participation. Because correlations were used to test for an association between social participation and local COVID-19 incidence we cannot imply any effects or causation. Additionally, only persons who wanted or were vaccinated were included in the study. A study design that included non-vaccinated persons would allow us to gain more information on the effect of the vaccination. However, requiring persons for a high risk for a severe COVID-19 course would neither have been feasible nor ethically appropriate.
5. Conclusions
Social participation increased after one month after basic COVID-19 vaccination and kept increasing for the next 12 months in persons with a high risk for a severe COVID-19 course regardless of the local COVID-19 incidence. The underlying reason for the change in social participation like risk perception and attitudes should be focused on by further research. Qualitative research could be useful to understand the change process more in-depth.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by an Institutional Ethics committee. See details under Methods.
Informed consent statement
Written informed consent was obtained from all participants involved in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The datasets generated and analyzed during the current study are not publicly available in accordance with the decision of the involved Research Ethics Boards but are available from the corresponding author on reasonable request within a data-sharing agreement.
Additional information
Funding
References
- Adams, K., Rhoads, J. P., Surie, D., Gaglani, M., Ginde, A. A., McNeal, T., Talbot, H. K., Casey, J. D., Zepeski, A., Shapiro, N. I., Gibbs, K. W., Files, D. C., Hager, D. N., Frosch, A. E., Exline, M. C., Mohamed, A., Johnson, N. J., Steingrub, J. S., Peltan, I. D., ..., Self, W. H. (2022). Vaccine effectiveness of primary series and booster doses against Covid-19 associated hospital admissions in the United States: Living test negative design study. BMJ, 379, e072065. https://doi.org/10.1136/bmj-2022-072065
- Akalin, E., Azzi, Y., Bartash, R., Seethamraju, H., Parides, M., Hemmige, V., Ross, M., Forest, S., Goldstein, Y. D., Ajaimy, M., Liriano—Ward, L., Pynadath, C., Loarte—Campos, P., Nandigam, P. B., Graham, J., Le, M., Rocca, J., & Kinkhabwala, M. (2020). Covid-19 and kidney transplantation. New England Journal of Medicine, 382(25), 2475–2477. https://doi.org/10.1056/NEJMc2011117
- Ammar, A., Chtourou, H., Boukhris, O., Trabelsi, K., Masmoudi, L., Brach, M., Bouaziz, B., Bentlage, E., How, D., Ahmed, M., Mueller, P., Mueller, N., Hsouna, H., Aloui, A., Hammouda, O., Paineiras—Domingos, L. L., Braakman—Jansen, A., Wrede, C., Bastoni, S., ..., Hoekelmann, A. (2020). COVID-19 Home confinement negatively impacts social participation and life satisfaction: A worldwide multicenter study. International Journal of Environmental Research and Public Health, 17. https://doi.org/10.3390/ijerph17176237
- Andersson, O., Campos-Mercade, P., Meier, A. N., & Wengström, E. (2021). Anticipation of COVID-19 vaccines reduces willingness to socially distance. Journal of Health Economics, 80, 102530. https://doi.org/10.1016/j.jhealeco.2021.102530
- Änderungen. (2021). Änderungen des Infektionsschutzgesetztes.
- Arregocés-Castillo, L., Fernández-Niño, J., Rojas-Botero, M., Palacios-Clavijo, A., Galvis-Pedraza, M., Rincón-Medrano, L., Pinto-Álvarez, M., Ruiz-Gómez, F., & Trejo-Valdivia, B. (2022). Effectiveness of COVID-19 vaccines in older adults in Colombia: A retrospective, population-based study of the ESPERANZA cohort. The Lancet Healthy Longevity, 3(4), e242–e252. https://doi.org/10.1016/S2666-7568(22)00035-6
- Baden, L. R., El Sahly, H. M., Essink, B., Kotloff, K., Frey, S., Novak, R., Diemert, D., Spector, S. A., Rouphael, N., Creech, C. B., McGettigan, J., Khetan, S., Segall, N., Solis, J., Brosz, A., Fierro, C., Schwartz, H., Neuzil, K., Corey, L, ..., Zaks, T. (2021). Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. New England Journal of Medicine, 384(5), 403–416. https://doi.org/10.1056/NEJMoa2035389
- Bakdash, J. Z., & Marusich, L. R. (2017). Repeated measures correlation. Frontiers in Psychology, 8, 456. https://doi.org/10.3389/fpsyg.2017.00456
- Booth, A., Reed, A. B., Ponzo, S., Yassaee, A., Aral, M., Plans, D., Labrique, A., & Mohan, D. (2021). Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis. PLoS One, 16(3), e0247461. https://doi.org/10.1371/journal.pone.0247461
- Bundesärztekammer. (2021). Stellungnahme der Bundesärztekammer, Berlin. Retrieved on 3 January 2023. https://www.bundesaerztekammer.de/fileadmin/user_upload/_old-files/downloads/pdf-Ordner/Stellungnahmen/AEnderungsantrag_IfSG_28a_SN_BAEK_26082021_final.pdf
- Bundesregierung. 2021. Videoschaltkonferenz der Bundeskanzlerin mit den Regierungschefinnen und Regierungschefs der Länder am 3. März 2021, 2021. Retrieved on 19 April 2023. https://www.bundesregierung.de/resource/blob/974430/1872054/66dba48b5b63d8817615d11edaaed849/2021-03-03-mpk-data.pdf?download=1
- Bürgel, T. R., Hiebl, M. R. W., & Pielsticker, D. I. (2023). Digitalization and entrepreneurial firms’ resilience to pandemic crises: Evidence from COVID-19 and the German Mittelstand. Technological Forecasting and Social Change, 186, 122135. https://doi.org/10.1016/j.techfore.2022.122135
- Caserotti, M., Girardi, P., Rubaltelli, E., Tasso, A., Lotto, L., & Gavaruzzi, T. (2021). Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Social Science & Medicine, 272, 113688. https://doi.org/10.1016/j.socscimed.2021.113688
- Chiao, C., Weng, L.-J., & Botticello, A. L. (2011). Social participation reduces depressive symptoms among older adults: An 18-year longitudinal analysis in Taiwan. BMC Public Health, 11(1), 292. https://doi.org/10.1186/1471-2458-11-292
- Chourpiliadis, C., Lovik, A., Kähler, A. K., Valdimarsdóttir, U. A., Frans, E. M., Nyberg, F., Sullivan, P. F., & Fang, F. (2023). Short-term improvement of mental health after a COVID-19 vaccination. PLoS One, 18(2), e0280587. https://doi.org/10.1371/journal.pone.0280587
- Cipolletta, S., Andreghetti, G. R., & Mioni, G. (2022). Risk perception towards COVID-19: A systematic review and qualitative synthesis. International Journal of Environmental Research and Public Health, 19(8). https://doi.org/10.3390/ijerph19084649
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Routledge. ISBN 9780203771587.
- Costa, A. D., Fernandes, A., Ferreira, S., Couto, B., Machado-Sousa, M., Moreira, P., Morgado, P., & Picó-Pérez, M. (2022). How long does adaption last for? An update on the psychological impact of the confinement in Portugal. International Journal of Environmental Research and Public Health, 19. https://doi.org/10.3390/ijerph19042243
- Deck, R., Mittag, O., Hüppe, A., Muche-Borowski, C., & Raspe, H. (2011). IMET – Index zur Messung von Einschränkungen der Teilhabe.
- Deck, R., Walther, A. L., Staupendahl, A., & Katalinic, A. (2015). Einschränkungen der Teilhabe in der Bevölkerung – Normdaten für den IMET auf der Basis eines Bevölkerungssurveys in Norddeutschland. Rehabilitation (Stuttg), 54(06|6), 402–408. https://doi.org/10.1055/s-0035-1559670
- Deimel, D., Köhler, T., Dyba, J., Graf, N., & Firk, C. (2022). Mental health of Covid-19 risk groups during the first Covid-19 lockdown in Germany: A cross-sectional study. BMC Public Health, 22(1), 1187. https://doi.org/10.1186/s12889-022-13593-z
- Dietrich, H., Patzina, A., & Lerche, A. (2021). Social inequality in the homeschooling efforts of German high school students during a school closing period. European Societies, 23(sup1), S348–S369. https://doi.org/10.1080/14616696.2020.1826556
- Ding, Y., Chen, L., & Zhang, Z. (2022). The relationship between social participation and depressive symptoms among Chinese middle-aged and older adults: A cross-lagged panel analysis. Frontiers in Public Health, 10, 996606. https://doi.org/10.3389/fpubh.2022.996606
- Dopfer-Jablonka, A., Steffens, S., Müller, F., Mikuteit, M., Niewolik, J., Cossmann, A., Stankov, M. V., Behrens, G. M. N., Hummers, E., Heesen, G., Schröder, D., Roder, S., Klawonn, F., Vahldiek, K., Hasenkamp, J., Kallusky, J., Falk, C. S., Overbeck, T. R., & Heinemann, S. (2022). SARS-CoV-2-specific immune responses in elderly and immunosuppressed participants and patients with hematologic disease or checkpoint inhibition in solid tumors: Study protocol of the prospective, observational CoCo immune study. BMC Infectious Diseases, 22(1), 403. https://doi.org/10.1186/s12879-022-07347-w
- Douglas, H., Georgiou, A., & Westbrook, J. (2017). Social participation as an indicator of successful aging: An overview of concepts and their associations with health. Australian Health Review, 41(4), 455–462. https://doi.org/10.1071/AH16038
- Fain, R. S., Hayat, S. A., Luben, R., Abdul Pari, A. A., & Yip, J. L. Y. (2022). Effects of social participation and physical activity on all-cause mortality among older adults in Norfolk, England: An investigation of the EPIC-Norfolk study. Public Health, 202, 58–64. https://doi.org/10.1016/j.puhe.2021.10.017
- Fendler, A., Vries, E. G. E. d., GeurtsvanKessel, C. H., Haanen, J. B., Wörmann, B., Turajlic, S., & Lilienfeld-Toal, M. v. (2022). COVID-19 vaccines in patients with cancer: Immunogenicity, efficacy and safety. Nature Reviews Clinical Oncology, 19(6), 385–401. https://doi.org/10.1038/s41571-022-00610-8
- Florensa, D., Mateo, J., Spaimoc, R., Miret, C., Godoy, S., Solsona, F., & Godoy, P. (2022). Severity of COVID-19 cases in the months of predominance of the Alpha and Delta variants. Scientific Reports, 12(1), 15456. https://doi.org/10.1038/s41598-022-19125-4
- Galmiche, S., Luong Nguyen, L. B., Tartour, E., Lamballerie, X. d., Wittkop, L., Loubet, P., & Launay, O. (2022). Immunological and clinical efficacy of COVID-19 vaccines in immunocompromised populations: A systematic review. Clinical Microbiology and Infection, 28(2), 163–177. https://doi.org/10.1016/j.cmi.2021.09.036
- Gianfrancesco, M., Hyrich, K. L., Al—Adely, S., Carmona, L., Danila, M. I., Gossec, L., Izadi, Z., Jacobsohn, L., Katz, P., Lawson—Tovey, S., Mateus, E. F., Rush, S., Schmajuk, G., Simard, J., Strangfeld, A., Trupin, L., Wysham, K. D., Bhana, S., Costello, W., ..., Robinson, P. C. (2020). Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease: Data from the COVID-19 global rheumatology alliance physician-reported registry. Annals of the Rheumatic Diseases, 79(7), 859–866. https://doi.org/10.1136/annrheumdis-2020-217871
- Gough, C., Barr, C., Lewis, L. K., Hutchinson, C., Maeder, A., & George, S. (2023). Older adults’ community participation, physical activity, and social interactions during and following COVID-19 restrictions in Australia: A mixed methods approach. BMC Public Health, 23(1), 172. https://doi.org/10.1186/s12889-023-15093-0
- Graffigna, G., Palamenghi, L., Boccia, S., & Barello, S. (2020). Relationship between citizens’ health engagement and intention to take the COVID-19 vaccine in Italy: A mediation analysis. Vaccines (Basel), 8. https://doi.org/10.3390/vaccines8040576
- Guida, J. L., Holt, C. L., Dallal, C. M., He, X., Gold, R., & Liu, H. (2020). Social relationships and functional impairment in aging cancer survivors: A longitudinal social network study. The Gerontologist, 60(4), 607–616. https://doi.org/10.1093/geront/gnz051
- Hadley, W. (2016). Ggplot2: Elegrant graphics for data analysis, Second edition. Springer. ISBN 978-3-319-24277-4.
- Haktanir, A., Can, N., Seki, T., Kurnaz, M. F., & Dilmaç, B. (2022). Do we experience pandemic fatigue? Current state, predictors, and prevention. Current Psychology, 41(10), 7314–7325. https://doi.org/10.1007/s12144-021-02397-w
- Hanna, K., Clarke, P., Woolfall, K., Hassan, S., Abba, K., Hajj, T. E., Deja, E., Ahmed, S., Joseph, N., Ring, A., Allen, G., Byrne, P., & Gabbay, M. (2023). The perception of risk in contracting and spreading COVID-19 amongst individuals, households and vulnerable groups in England: A longitudinal qualitative study. BMC Public Health, 23(1), 653. https://doi.org/10.1186/s12889-023-15439-8
- He, W., Chen, L [Lei], Chen, L [Li], Yuan, G., Fang, Y., Chen, W., Di Wu, Liang, B., Lu, X., Ma, Y., Li, L., Wang, H., Chen, Z., Li, Q., & Gale, R. P. (2020). COVID-19 in persons with haematological cancers. Leukemia, 34(6), 1637–1645. https://doi.org/10.1038/s41375-020-0836-7
- Hilverda, F., & Vollmann, M. (2021). The role of risk perception in students’ COVID-19 vaccine uptake: A longitudinal study. Vaccines (Basel), 10. https://doi.org/10.3390/vaccines10010022
- Howrey, B. T., & Hand, C. L. (2019). Measuring social participation in the health and retirement study. The Gerontologist, 59, e415–e423. https://doi.org/10.1093/geront/gny094
- Hueppe, A., Langbrandtner, J., & Raspe, H. (2014). Inviting patients with inflammatory bowel disease to active involvement in their own care: A randomized controlled trial. Inflammatory Bowel Diseases, 20, 1057–1069. https://doi.org/10.1097/MIB.0000000000000044
- Hüppe, A., Langbrandtner, J., Lill, C., & Raspe, H. (2020). The effectiveness of actively induced medical rehabilitation in chronic inflammatory bowel disease. Deutsches Ärzteblatt International, 117, 89–96. https://doi.org/10.3238/arztebl.2020.0089
- Hyams, C., Challen, R., Marlow, R., Nguyen, J., Begier, E., Southern, J., King, J., Morley, A., Kinney, J., Clout, M., Oliver, J., Gray, S., Ellsbury, G., Maskell, N., Jodar, L., Gessner, B., McLaughlin, J., Danon, L., & Finn, A. (2023). Severity of omicron (B.1.1.529) and delta (B.1.617.2) SARS-CoV-2 infection among hospitalised adults: A prospective cohort study in Bristol, United Kingdom. The Lancet Regional Health - Europe, 25, 100556. https://doi.org/10.1016/j.lanepe.2022.100556
- Im Ryu, S., Park, Y.-H., Kim, J., Huh, I., Chang, S. J., Jang, S.-N., & Noh, E.-Y. (2022). Impact of COVID-19 on the social relationships and mental health of older adults living alone: A two-year prospective cohort study. PLoS One, 17, e0270260. https://doi.org/10.1371/journal.pone.0270260
- John Hopkins University. (2023). COVID-19 dashboard: By the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html (accessed on 14 January 2023)
- Karing, C. (2021). Prevalence and predictors of anxiety, depression and stress among university students during the period of the first lockdown in Germany. Journal of Affective Disorders Reports, 5, 100174. https://doi.org/10.1016/j.jadr.2021.100174
- Kassambara, A. (2022). rstatix.
- Kerper, L. F., Spies, C. D., Tillinger, J., Wegscheider, K., Salz, A.-L., Weiss-Gerlach, E., Neumann, T., & Krampe, H. (2014). Screening for depression, anxiety, and general psychological distress in pre-operative surgical patients: A psychometric analysis of the patient health questionnaire 4 (Phq-4). Clinical Health Promotion – Research and Best Practice for Patients, Staff and Community, 4(1), 5–14. https://doi.org/10.29102/clinhp.14002
- King, K., Vygen-Bonnet, S., Burchard, G.-D., Heininger, U., Kremer, K., Wiedermann, U., & Bogdan, C. (2021). STIKO-Empfehlung zur COVID-19-Impfung bei Personen mit Immundefizienz (ID) 2021. https://doi.org/10.25646/9083.2.
- Kowsar, R., Rahimi, A. M., Sroka, M., Mansouri, A., Sadeghi, K., Bonakdar, E., Kateb, S. F., & Mahdavi, A. H. (2023). Risk of mortality in COVID-19 patients: A meta- and network analysis. Scientific Reports, 13(1), 2138. https://doi.org/10.1038/s41598-023-29364-8
- Lee, A. R. Y. B., Wong, S. Y., Chai, L. Y. A., Lee, S. C., Lee, M. X., Muthiah, M. D., Tay, S. H., Teo, C. B., Tan, B. K. J., Chan, Y. H., Sundar, R., & Soon, Y. Y. (2022). Efficacy of covid-19 vaccines in immunocompromised patients: Systematic review and meta-analysis. BMJ, 376, e068632. https://doi.org/10.1136/bmj-2021-068632
- Levasseur, M., Desrosiers, J., & Whiteneck, G. (2010). Accomplishment level and satisfaction with social participation of older adults: Association with quality of life and best correlates. Quality of Life Research, 19(5), 665–675. https://doi.org/10.1007/s11136-010-9633-5
- Levasseur, M., Lussier-Therrien, M., Biron, M. L., Raymond, É, Castonguay, J., Naud, D., Fortier, M., Sévigny, A., Houde, S., & Tremblay, L. (2022). Scoping study of definitions of social participation: Update and co-construction of an interdisciplinary consensual definition. Age and Ageing, 51(2). https://doi.org/10.1093/ageing/afab215
- Löwe, B., Wahl, I., Rose, M., Spitzer, C., Glaesmer, H., Wingenfeld, K., Schneider, A., & Brähler, E. (2010). A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders, 122(1-2), 86–95. https://doi.org/10.1016/j.jad.2009.06.019
- Luchetti, M., Lee, J. H., Aschwanden, D., Sesker, A., Strickhouser, J. E., Terracciano, A., & Sutin, A. R. (2020). The trajectory of loneliness in response to COVID-19. American Psychologist, 75(7), 897–908. https://doi.org/10.1037/amp0000690
- Masten, A. S., & Motti-Stefanidi, F. (2020). Multisystem resilience for children and youth in disaster: Reflections in the context of COVID-19. Adversity and Resilience Science, 1(2), 95–106. https://doi.org/10.1007/s42844-020-00010-w
- Mergel, E., & Schützwohl, M. (2021). A longitudinal study on the COVID-19 pandemic and its divergent effects on social participation and mental health across different study groups with and without mental disorders. Social Psychiatry and Psychiatric Epidemiology, 56(8), 1459–1468. https://doi.org/10.1007/s00127-021-02025-9
- Morrison, L., McDonough, M., Won, S., Matsune, A. J., & Hewson, J. (2022). Older adults’ physical activity and social participation during COVID-19. Activities, Adaptation & Aging, 46(4), 320–342. https://doi.org/10.1080/01924788.2022.2094658
- Nair, V., Jandovitz, N., Hirsch, J. S., Nair, G., Abate, M., Bhaskaran, M., Grodstein, E., Berlinrut, I., Hirschwerk, D., Cohen, S. L., Davidson, K. W., Dominello, A. J., Osorio, G. A., Richardson, S., Teperman, L. W., & Molmenti, E. P. (2020). COVID-19 in kidney transplant recipients. American Journal of Transplantation, 20(7), 1819–1825. https://doi.org/10.1111/ajt.15967
- Noguchi, T., Hayashi, T., Kubo, Y., Tomiyama, N., Ochi, A., & Hayashi, H. (2021). Association between decreased social participation and depressive symptom onset among community-dwelling older adults: A longitudinal study during the COVID-19 pandemic. The Journal of Nutrition, Health & Aging, 25(9), 1070–1075. https://doi.org/10.1007/s12603-021-1674-7
- Patel, K., Robertson, E., Kwong, A. S. F., Griffith, G. J., Willan, K., Green, M. J., Di Gessa, G., Huggins, C. F., McElroy, E., Thompson, E. J., Maddock, J., Niedzwiedz, C. L., Henderson, M., Richards, M., Steptoe, A., Ploubidis, G. B., Moltrecht, B., Booth, C., Fitzsimons, E., ..., Katikireddi, S. V. (2022). Psychological distress before and during the COVID-19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Network Open, 5(4), e227629. https://doi.org/10.1001/jamanetworkopen.2022.7629
- Pereira, M. R., Mohan, S., Cohen, D. J., Husain, S. A., Dube, G. K., Ratner, L. E., Arcasoy, S., Aversa, M. M., Benvenuto, L. J., Dadhania, D. M., Kapur, S., Dove, L. M., Brown, R. S., Rosenblatt, R. E., Samstein, B., Uriel, N., Farr, M. A., Satlin, M., Small, C. B., ..., Verna, E. C. (2020). COVID-19 in solid organ transplant recipients: Initial report from the US epicenter. American Journal of Transplantation, 20(7), 1800–1808. https://doi.org/10.1111/ajt.15941
- Polack, F. P., Thomas, S. J., Kitchin, N., Absalon, J., Gurtman, A., Lockhart, S., Perez, J. L., Pérez Marc, G., Moreira, E. D., Zerbini, C., Bailey, R., Swanson, K. A., Roychoudhury, S., Koury, K., Li, P., Kalina, W. V., Cooper, D., Frenck, R. W., Hammitt, L. L., ..., Gruber, W. C. (2020). Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. New England Journal of Medicine, 383(27), 2603–2615. https://doi.org/10.1056/NEJMoa2034577
- Prati, G., & Mancini, A. D. (2021). The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. https://doi.org/10.1017/S0033291721000015
- Prihodova, L., Nagyova, I., Rosenberger, J., Roland, R., Majernikova, M., Groothoff, J. W., & van Dijk, J. P. (2015). Social participation after kidney transplantation as a predictor of graft loss and mortality over 10 years: A longitudinal study. Transplantation, 99(3), 568–575. https://doi.org/10.1097/TP.0000000000000347
- Richardson, S., Hirsch, J. S., Narasimhan, M., Crawford, J. M., McGinn, T., Davidson, K. W., Barnaby, D. P., Becker, L. B., Chelico, J. D., Cohen, S. L., Cookingham, J., Coppa, K., Diefenbach, M. A., Dominello, A. J., Duer-Hefele, J., Falzon, L., Gitlin, J., Hajizadeh, N., Harvin, T. G., ..., Zanos, T. P. (2020). Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA, 323(20), 2052–2059. https://doi.org/10.1001/jama.2020.6775
- Robert Koch-Institut. (2023). 7-Tage-Inzidenzen nach Bundesländern und Kreisen (fixierte Werte) sowie 7-Tage-Inzidenz der hospitalisierten COVID-19-Fälle nach Bundesländern (fixierte Werte). https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Daten/Fallzahlen_Kum_Tab.html (accessed on 13 January 2023)
- Robinson, E., Sutin, A. R., Daly, M., & Jones, A. (2022). A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders, 296, 567–576. https://doi.org/10.1016/j.jad.2021.09.098
- Sadoff, J., Gray, G., an Vandebosch, Cárdenas, V., Shukarev, G., Grinsztejn, B., Goepfert, P. A., Truyers, C., Fennema, H., Spiessens, B., Offergeld, K., Scheper, G., Taylor, K. L., Robb, M. L., Treanor, J., Barouch, D. H., Stoddard, J., Ryser, M. F., Marovich, M. A., ..., Douoguih, M. (2021). Safety and efficacy of single-dose Ad26.COV2.S vaccine against COVID-19. New England Journal of Medicine, 384(23), 2187–2201. https://doi.org/10.1056/NEJMoa2101544
- Schmid, L., Wörn, J., Hank, K., Sawatzki, B., & Walper, S. (2021). Changes in employment and relationship satisfaction in times of the COVID-19 pandemic: Evidence from the German family panel. European Societies, 23(sup1), S743–S758. https://doi.org/10.1080/14616696.2020.1836385
- Schneider, C. R., Dryhurst, S., Kerr, J., Freeman, A. L. J., Recchia, G., Spiegelhalter, D., & van der Linden, S. (2021). COVID-19 risk perception: A longitudinal analysis of its predictors and associations with health protective behaviours in the United Kingdom. Journal of Risk Research, 24(3-4), 294–313. https://doi.org/10.1080/13669877.2021.1890637
- Schröder, D., Heesen, G., Heinemann, S., Hummers, E., Jablonka, A., Steffens, S., Mikuteit, M., Niewolik, J., Overbeck, T. R., Kallusky, J., et al. (2022). Development and validation of a questionnaire to assess social participation of high risk-adults in Germany during the COVID-19 pandemic. Frontiers in Public Health, 10, 831087. https://doi.org/10.3389/fpubh.2022.831087
- Schützwohl, M., & Mergel, E. (2020). Teilhabemöglichkeit, Partizipation, Inklusion und psychisches Befinden im Zusammenhang mit Ausgangsbeschränkungen aufgrund SARS-CoV-2. Psychiatrische Praxis, 47(06|6), 308–318. https://doi.org/10.1055/a-1202-2427
- Shen, C., Risk, M., Schiopu, E., Hayek, S. S., Xie, T., Holevinski, L., Akin, C., Freed, G., & Zhao, L. (2022). Efficacy of COVID-19 vaccines in patients taking immunosuppressants. Annals of the Rheumatic Diseases, 81(6), 875–880. https://doi.org/10.1136/annrheumdis-2021-222045
- Skulmowski, A., & Rey, G. D. (2020). COVID-19 as an accelerator for digitalization at a German university: Establishing hybrid campuses in times of crisis. Human Behavior and Emerging Technologies, 2(3), 212–216. https://doi.org/10.1002/hbe2.201
- Sozialgesetzbuch. (2022). Sozialgesetzbuch neuntes Buch, §152: SGB IX §152, 2022.
- Su, S., Marrie, R. A., & Bernstein, C. N. (2022). Factors associated with social participation in persons living with inflammatory bowel disease. Journal of the Canadian Association of Gastroenterology, 5(2), 59–67. https://doi.org/10.1093/jcag/gwab022
- Sudre, C. H., Murray, B., Varsavsky, T., Graham, M. S., Penfold, R. S., Bowyer, R. C., Pujol, J. C., Klaser, K., Antonelli, M., Canas, L. S., Molteni, E., Modat, M., Jorge Cardoso, M., May, A., Ganesh, S., Davies, R., Nguyen, L. H., Drew, D. A., Astley, C. M., ..., Steves, C. J. (2021). Attributes and predictors of long COVID. Nature Medicine, 27(4), 626–631. https://doi.org/10.1038/s41591-021-01292-y
- Takagi, D., Kondo, K., & Kawachi, I. (2013). Social participation and mental health: Moderating effects of gender, social role and rurality. BMC Public Health, 13(1), 701. https://doi.org/10.1186/1471-2458-13-701
- Tillinger, J. (2015). Der PHQ-4 zur Messung von Depressivität und Angst bei operativen Patienten der Anästhesieambulanz; Charité – Universitätsmedizin Berlin.
- Voysey, M., Clemens, S. A. C., Madhi, S. A., Weckx, L. Y., Folegatti, P. M., Aley, P. K., Angus, B., Baillie, V. L., Barnabas, S. L., Bhorat, Q. E., Bibi, S., Briner, C., Cicconi, P., Collins, A. M., Colin-Jones, R., Cutland, C. L., Darton, T. C., Dheda, K., Duncan, C. J. A., ..., Pollard, A. J. (2021). Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. The Lancet, 397(10269), 99–111. https://doi.org/10.1016/S0140-6736(20)32661-1
- Wang, C., Horby, P. W., Hayden, F. G., & Gao, G. F. (2020). A novel coronavirus outbreak of global health concern. The Lancet, 395(10223), 470–473. https://doi.org/10.1016/S0140-6736(20)30185-9
- Webb, G. J., Moon, A. M., Barnes, E., Barritt, A. S., & Marjot, T. (2020). Determining risk factors for mortality in liver transplant patients with COVID-19. The Lancet Gastroenterology & Hepatology, 5(7), 643–644. https://doi.org/10.1016/S2468-1253(20)30125-4
- Wessels, M., Utegaliyev, N., Bernhard, C., Welsch, R., Oberfeld, D., Thönes, S., & Castell, C. v. (2022). Adapting to the pandemic: Longitudinal effects of social restrictions on time perception and boredom during the Covid-19 pandemic in Germany. Scientific Reports, 12(1), 1863. https://doi.org/10.1038/s41598-022-05495-2
- WHO. WHO/Europe discusses how to deal with pandemic fatigue. https://www.who.int/news-room/feature-stories/detail/who-europe-discusses-how-to-deal-with-pandemic-fatigue
- Wu, X., Lu, Y., & Jiang, B. (2023). Built environment factors moderate pandemic fatigue in social distance during the COVID-19 pandemic: A nationwide longitudinal study in the United States. Landscape and Urban Planning, 233, 104690. https://doi.org/10.1016/j.landurbplan.2023.104690
Appendix
Table A1. PSP-Q and IMET changes (mean and SD) between T1-T3 stratified between sociodemographic and medical factors.
Figure A1. PSP-Q English translation. *indicates reversed pooled items; FA1: well-being participation; FA2: active social participation; FA3: restrictions.