ABSTRACT
Firefighting is recognised as a profession where health and well-being can be affected by a variety of occupational factors, such as physical, thermal, and chemical stressors. Along with the risks intuitively associated with the fire service, however, psychosocial stress has begun to attract attention as another variable deserving of consideration. Indeed, long-term exposure to work-related psychosocial stress has been linked with poor health outcomes in many workers; however, despite this association, very little has been done to examine how such stressors become biologically embedded in firefighters. To help facilitate research into how psychosocial stress can affect health-related outcomes in the fire service, we propose a framework centered on the notion of allostatic load. First, we reviewed the occupational characteristics that may generate psychosocial stress within firefighters before introducing allostatic load (that is, dysregulation across various physiological systems caused by the need to manage ongoing stressors). Next, we provided a summary of how allostatic load can be measured and touched on the framework's utility for studying the cumulative effects of work-related stress on firefighter health. After this, factors that may influence the steps leading from stress exposure to health outcomes were discussed; in particular, we commented upon how research in this area should consider specific non-modifiable (age, sex, and ethnicity) and modifiable (psychosocial resources and behavioural habits) factors. Finally, we presented methodological barriers and opportunities that may arise when using the allostatic load framework with this professional group. By introducing the framework, we hope to provide a tool that may be used by those interested in stress-health research in firefighters to build the evidence needed to inform primary prevention measures.
General orientation and objectives
Work-related psychosocial stress, an enduring threat to health and wellbeing, has commanded growing attention in recent decades. In firefighting, as with many occupations, stress often results from work events and characteristics, including social interactions, that produce psychological strain (Ganster & Rosen, Citation2013). Such stressors may appear through a constellation of day-to-day job experiences, like job demands, interpersonal relationships, and work environment/culture (An et al., Citation2015; Payne & Kinman, Citation2019; Saijo et al., Citation2007), and can place workers at elevated risk for reduced job performance and adverse behavioural and health outcomes (Igboanugo et al., Citation2021; Isaac & Buchanan, Citation2021).
Given the rise in adverse health outcomes (such as short – and long-term disability and chronic illnesses) and the implications to public safety, there is an urgent need to address workplace stressors that impact the health and wellbeing of firefighters. However, despite mounting evidence suggesting a significant association between psychosocial stress and adverse health outcomes, the underlying process still eludes our full comprehension. Due to the complicated nature of the stress-health relationship, a theory-driven framework will provide the best approach to elucidating this phenomenon. One possibility that needs to be considered in this regard is the allostatic load (AL) model (McEwen & Stellar, Citation1993), which offers an innovative and reliable framework for investigating and understanding the cumulative biological imprint of chronic psychosocial stress exposure in firefighters.
As a result, our primary goals will be to introduce the AL framework and explore its practicality in guiding scientific inquiry into psychosocial stress and adverse health-related outcomes in the fire service. To meet our objectives, the article will proceed as follows. First, the various type of stressors commonly reported by firefighters will be identified, with special attention placed on those of a psychosocial nature. Next, a summary of work-related psychosocial stressors and the steps leading from them to adverse health outcomes in firefighters will be provided. Third, the AL model will be introduced, and the framework's utility for studying work-related stress and its cumulative effect on firefighter health and wellbeing will be outlined. After this, we will describe factors that may play a significant role in the stress-AL-health outcome relationship. Finally, we will discuss methodological barriers and opportunities that may arise when applying the AL framework within this professional group. Ethics approval was not required to review published/publicly reported literature.
Types of stressors experienced by firefighters
Stressors prevalent among firefighters can be grouped into two main categories: physical and psychosocial. In addition to physical stress from fire suppression, firefighters often endure injury from structural collapse, equipment failure, and exposure to contaminants from combustion products. Also, since firefighters respond to medical emergencies and disasters, they may experience additional physical stressors that threaten personal safety, such as needlesticks, patient violence, and respiratory diseases (Durand et al., Citation2021; Fisher & Etches, Citation2003).
Further, some of what firefighters experience may enter the realm of traumatic stress, which includes cases where the perceived magnitude of a physical and/or psychosocial stressor exceeds a severity threshold. Characteristics that may foster the likelihood of an exposure crossing the traumatic threshold include witnessing the injury, or death of victims, or fellow firefighters and the experience of dealing with victims of fire, accidents, and natural disasters (Fisher & Abrahamson, Citation2002; Fisher & Etches, Citation2003). As might be reasonably expected, a traumatic level of stress experience can place a firefighter at higher risk of post-traumatic stress injury (Salleh et al., Citation2020) and vicarious trauma [i.e. stress emanating from exposure to a traumatised person (Fisher & Etches, Citation2003)].
Due to decades of research, there is considerable evidence about the nature and prevalence of physical, traumatic, and environmental stressors and their consequences [see reviews by Barr et al. (Barr et al., Citation2010), Guidotti & Clough (Guidotti & Clough, Citation1992), and Orr et al. (Orr et al., Citation2019) for more details], primarily because of their clear link with health-related outcomes such as musculoskeletal, respiratory, and traumatic stress disorders (Guidotti, Citation1992; Jahnke et al., Citation2016; Mustajbegovic et al., Citation2001). Consequently, great strides have been made in developing policies, training procedures, and protective equipment to mitigate the impact of physical and traumatic stressors on firefighters. Unfortunately, a similar degree of progress has not been achieved for the other main type of stress experienced by these workers.
Firefighters have a unique work schedule, often consisting of a traditional 24-hour shift followed by two days off; however, in exceptional cases, 24-hour shifts may extend beyond the allocated schedule (Choi et al., Citation2016). During their shifts, firefighters often face frequent emergency alarms that may promote a hypervigilant state with readiness for potential danger. In other instances, especially on a slow day, their time at work may become boring (Murphy et al., Citation1999). Regardless of its variability, over time, such shift characteristics may lead to varying levels of stimulation, causing sleep disorders, fatigue, and anxiety (Barger et al., Citation2009; Haddock et al., Citation2013; Murphy et al., Citation1999). In addition, work-life balance and marital satisfaction may suffer because of the unusual work schedule and extended work hours (Shreffler et al., Citation2011).
Further, most firefighting work environments in North America and other parts of the world employ a paramilitary leadership style with a ‘chain of command’ structure (Murphy et al., Citation1999). Such a leadership style may inadvertently create challenges in communication leading to interpersonal conflicts, power struggles, insubordination with leadership, or, in worst-case scenarios, result in an authoritative and ‘toxic’ work environment (Beaton & Murphy, Citation1993). In addition, the paramilitary environment may encourage the sort of bravado that exposes firefighters to risk-taking and fatal mistakes (Fisher & Etches, Citation2003). Since firefighters depend on the leadership and combined effort of their entire platoon (Driessen, Citation2002, p.5), there is often an expectation of bravery and commitment from each team member. The downside of such expectation is the possibility that firefighters struggling with job demands, or other issues, may choose not to seek help, or speak out for fear of stigmatisation, or being ostracised (Banes, Citation2014; Beaton & Murphy, Citation1993).
In addition, various factors that complicate the work environment of firefighters have begun to emerge. As noted, firefighters, especially in urban areas, have observed increased job demands along with role conflicts and ambiguity, due to their growing involvement in emergency medical services and other activities outside the usual scope of firefighting. As a result, in addition to fire-suppression skills, many firefighters must be well-versed in life-saving techniques that require time urgency, decision-making readiness, and exposure to harmful situations (Murphy et al., Citation1999). Furthermore, changing demographics, rapid urbanisation, and climate change have placed additional demands on time, effort, and capacity. Despite the increase in job demands often experienced, pay and benefits have not always grown in a matching fashion, leading to effort-reward imbalance, job security concerns, and burnout (Ângelo & Chambel, Citation2013; Lourel et al., Citation2008; Rajabi et al., Citation2020).
The enduring impact of psychosocial stress on firefighters
Due to the likelihood of repeated exposure to work-related psychosocial stressors, the possibility that firefighters may experience a high risk of adverse physiological, mental health, and behavioural changes is not surprising (Fisher & Etches, Citation2003; Igboanugo et al., Citation2021). That is, going along with the increased risk of occupational injuries caused by physical stressors, many firefighters may also be burdened by exposure to psychosocial stressors (acute and chronic) that can increase their risk of cardiovascular disorders, musculoskeletal difficulties, undesirable mental health outcomes (like burnout and depression), and harmful coping behaviours, like alcohol dependency (Igboanugo et al., Citation2021).
At the organisational level, stress-related adverse health outcomes may take shape as increased rates of absenteeism, sick days, long-term disability, labour-management disputes, and early retirements (Fisher & Etches, Citation2003). In addition, poor job performance, an inability to attract and retain firefighters, and increased healthcare costs from managing stress-related disorders are potential consequences of these health outcomes that may also place the public at risk.
The allostatic load framework: biological embedding of workplace psychosocial stress
In response to stressful stimuli, a set of highly interrelated adaptive processes are activated, allowing the body to respond to the challenge (McEwen & Wingfield, Citation2003). The two most notable stress response systems are the hypothalamic–pituitary–adrenal gland (HPA) axis and the sympathetic-adrenal medullary (SAM) system (Chrousos, Citation2009; McEwen, Citation1998). Stimulating the HPA axis and the SAM system leads to the release of vital hormones (such as cortisol and catecholamines), which are responsible for maintaining the fundamental stability of the most important physiological systems. For example, by generating and redistributing energy resources through a cascade of events in different, but interconnected systems, cortisol and catecholamines enable the body to respond to a challenge by maintaining essential metabolism and body temperature (Chrousos, Citation2009; Godoy et al., Citation2018).
By working to create conditions that will help support those systems responsible for homeostasis (i.e. those physiological parameters necessary for life), cortisol and catecholamines are primary mediators of a process that has come to be known as ‘allostasis’ (Godoy et al., Citation2018; Sterling & Eyer, Citation1988). Allostasis may be imagined as the varied and often inter-connected physiological changes initiated by the primary mediators that influence downstream-level changes governing homeostasis to ensure the greatest degree of organism-level stability in the face of changing circumstances (Juster et al., Citation2010; Sterling & Eyer, Citation1988).
The various physiological changes caused by the primary mediators underlying allostasis were refined throughout evolution to play a beneficial role in improving adaptation and performance in the face of environmental demands, such as those presented by stressors (Juster et al., Citation2010). However, chronic activation of these allostatic changes may lead to the gradual dysregulation of many physiological systems that sets the stage for eventual ‘wear and tear’ (Juster et al., Citation2010). Put simply, continued attempts by the body to maintain stability in the face of changing circumstances over the long term has a biological cost, which has been framed as ‘allostatic load’ (McEwen & Stellar, Citation1993). Importantly, given the current discussion, the AL model may provide an account of how the physiological changes that begin with exposure to various stressors experienced throughout life can culminate in adverse health outcomes (Carbone et al., Citation2022; McEwen, Citation2000).
McEwen and Seeman (McEwen & Seeman, Citation1999), in their seminal work on the stress-AL relationship, detailed the steps by which high AL culminates in disease. At first, frequent stressors, or chronic exposure to stress burdens the body's adaptive and regulatory systems. Subsequently, the chronic activation of allostasis leads to a series of pathophysiological states representing altered response patterns, including the inability to properly extinguish the physiological stress response, even after the stressor is gone. Finally, due to overuse, or maladaptation, such failure to adapt results in dysregulated biological systems that eventually succumb to disease states (Ganster & Rosen, Citation2013; McEwen, Citation1998).
Measuring allostatic load
By considering multisystem stress biomarkers, the AL model allows us to quantify the cumulative ‘wear and tear’ on the body when adaptive systems are repeatedly required to operate in a manner beyond what may be regarded as typical (Singer et al., Citation2004). In selecting how to measure AL, consideration is given to the synergistic effect of various biomarkers involved with the stress response and/or predictive of long-term physiologic dysregulation, or pathological states (Bizik et al., Citation2013; Edes et al., Citation2018); the compilation of these biomarkers form the AL index (or ALI). At least 11 algorithmic formulations for arriving at the ALI score exist; however, the original scoring algorithm, the risk quartile count method (Seeman et al., Citation1997), remains the most frequently used (Juster et al., Citation2010; McLoughlin et al., Citation2020). In the risk quartile count method, the sample's distribution of a biomarker is used to establish risk categories (i.e. the upper, or lower 25th percentile, as appropriate), and these thresholds are then used to characterise recorded values (Bizik et al., Citation2013; McLoughlin et al., Citation2020). In particular, values falling within a high-risk quartile are assigned a score of ‘1’, whereas all others are scored as zero; after this, the ALI is then determined by simply summing the scores from each biomarker (Bizik et al., Citation2013). Regardless of the combination of factors used to determine the ALI, the summary measure of AL is a greater predictor of long-term health than any individual biomarker (Karlamangla et al., Citation2002; Seeman et al., Citation2001).
Given the theoretical construct of allostatic load, the experience of stress over time would be expected to increase one's ALI. Importantly, such a notion is supported by evidence from both cross-sectional (Mair et al., Citation2011; Mauss & Jarczok, Citation2021) and longitudinal (Clark et al., Citation2007; Glei et al., Citation2007; Piazza et al., Citation2019; Upchurch et al., Citation2015) investigations that strongly suggest psychosocial stress is linked to increased AL scores in the general population. Moreover, along with evidence supporting the link between psychosocial stress and high AL, extant research affirms that high AL can increase risk of adverse health outcomes. For example, among the earliest attempts at operationalising AL, Seeman et al. (Seeman et al., Citation1997) compiled an index of 10 biomarkers to show high ALI correlated significantly with poor health status, including adverse cognitive function. Additionally, several recent literature reviews have documented evidence linking elevated AL to adverse health outcomes, including psychiatric conditions, cardiovascular disease, and all-cause mortality (Beckie, Citation2012; Guidi et al., Citation2021; Juster et al., Citation2010).
Work-related psychosocial stress and allostatic load
Current evidence points to a strong link between psychosocial stress and significant neurologic and somatic dysregulation in the form of high AL (McLoughlin et al., Citation2021; Theall et al., Citation2012). As a result, the growing application of the AL model to reveal the cumulative consequence of job strain in working populations should not be surprising. For example, work-related psychosocial stressors (such as effort-reward imbalance and high job demands) have been positively associated with AL (Bellingrath et al., Citation2009; de Castro et al., Citation2010; Mauss et al., Citation2015; Mauss et al., Citation2016; Schnorpfeil et al., Citation2003; Sun et al., Citation2007). Based on the compelling evidence linking AL and adverse health outcomes in the general population (workers in particular), there is a strong likelihood that work-related stressors elevate the risk for chronic disease in firefighters through a pathway that involves AL.
Applying the allostatic load framework to investigate work-related psychosocial stress within the fire service
The utility and value of subjective stress measures, for example, self-report questionnaires, have been widely debated (Brown et al., Citation2016), and concerns regarding their reliability and validity have been highlighted as potential limitations (see for psychosocial stress assessments commonly used with firefighters). For example, recall bias may limit self-report accuracy in capturing past events (Slavich, Citation2016). Alternatively, some studies have focused on the effect of work-related stress on physiological biomarkers, for example, cortisol (Teixeira et al., Citation2022), heart rate variability (Pluntke et al., Citation2019; Yook, Citation2019), and blood pressure (Choi et al., Citation2016; Kaur et al., Citation2014). Although informative, the assessment of single biomarkers provides limited information on the multi-systemic changes that coincide with stress-related disorders (Juster, Russell, et al., Citation2016). Although both approaches (self-report and specific biomarkers) play vital roles in stress-outcome assessment, when used individually, they may fall short of elucidating how work-related stress affects firefighters (Ganster & Rosen, Citation2013). For this reason, an approach that provides a more comprehensive stress-outcome assessment, especially within the work environment, is essential.
Table 1 . Alphabetical listing of assessment tools commonly used to measure psychosocial stress among firefighters.
An additional challenge to understanding how work-related psychosocial stress leads to adverse health outcomes stems from the Healthy Worker Effect [HWE; a reduction in morbidity and mortality in workers compared to the general population; (Li & Sung, Citation1999)], which may be particularly evident in professions (like firefighting) that have strict recruitment and retention criteria (Choi, Citation2000). That is, recruiting healthy, resilient firefighters lacking comorbidity is typical among fire departments. However, the AL model may offer an attractive solution, since changes within multiple systems can be identified with the ALI even when firefighters appear to be fine, or perceive their health to be satisfactory. In other words, the AL model may be sufficiently sensitive to systemic health changes in an otherwise healthy professional group and permit greater accuracy during comparison with other first responders, or the general population.
As well, because AL serves as a multisystem indicator of chronic physiological dysfunction, the framework presents a viable approach to chronic disease prevention among firefighters. Since computing the AL index informs our understanding of the cumulative changes in one's physiological status over time, AL may serve as a biological warning system that identifies systems undergoing clinically relevant change, or deterioration (Juster, Russell, et al., Citation2016). Additionally, since measuring AL allows individuals at risk of adverse health outcomes to be identified, the measure provides a valuable opportunity to address prevailing stressors and lessen their health-related consequences.
Primary and secondary variables for consideration in the proposed firefighter AL framework
In addition to the primary variables of interest within the framework (i.e. work-related psychosocial stress, allostatic load, and firefighter health), factors influencing the associations between the model's primary variables need to be considered. In particular, previous studies have revealed that AL may be influenced by various factors that enter into the model as secondary variables (Gustafsson et al., Citation2014). Indeed, the sequence of events leading from adaptive stress response to AL and the development of adverse health outcomes is dynamic and may be influenced by both modifiable and non-modifiable secondary variables. According to the current literature, non-modifiable factors linked with AL that may be relevant when investigating firefighters include age, sex, and ethnicity (Beckie, Citation2012).
Non-modifiable secondary variables
Age and allostatic load
Compelling evidence shows that AL consistently increases with age (Beckie, Citation2012; Crimmins et al., Citation2003; Seeman et al., Citation2001). For example, in the earliest application of the AL framework, Seeman and colleagues determined, by following members of the MacArthur Cohort of Successful Agers, that AL increased significantly with age (Seeman et al., Citation1997). Similarly, a cross-sectional study which used a sample of adults aged 20 to 80, observed that AL scores rose in a non-linear pattern with age (Crimmins et al., Citation2003). That is, AL rose slowly beginning at age 25, with a surging rise after 35 till age 65, and then a plateau afterwards. Additionally, evidence supports a rise in AL with age in working populations (Schnorpfeil et al., Citation2003; Sun et al., Citation2007). Of course, the age-AL relationship is expected, given that the multi-systemic change in physiology captured by AL reflects the gradual change in the body's function over one's lifespan (Guidi et al., Citation2021; Read & Grundy, Citation2014).
In addition to the increase in AL that coincides with age, as experienced firefighters rise through the ranks and are accorded more responsibilities, they may endure more frequent, or intense work-related psychosocial stress events, with mounting physiological costs as their career progresses (Goh et al., Citation2020; Regehr et al., Citation2003). Thus, given that firefighters spend considerable time on the job and that many retire past the age of fifty-five (King, Citation2011), both age and length of service should be considered when investigating work-related psychosocial stress among these workers, especially to allow age – and cohort-related effects on AL to be distinguished.
Biological sex, gender roles, and allostatic load
Biological sex and psychosocial gender roles may independently, or synergistically influence AL (Juster et al., Citation2016; Juster & Lupien, Citation2012; Kerr et al., Citation2020). With regards to biological sex, previous research looking into either specific occupational groups, or across the general population suggests that higher AL is more often found in men (Kerr et al., Citation2020; Mauss et al., Citation2015; Schnorpfeil et al., Citation2003). For example, Schnorpfeil et al. (Citation2003) reported higher mean AL scores (r = 0.13, p = .02) for men (M = 3.29, SD = 2.28) than women (M = 2.43, SD = 1.70) in a sample of 324 industrial workers. A variety of factors could be responsible for the observed sex-based difference; most notable among them could be the immuno-, cardio-, and neuroprotective effects from estrogen benefitting women and the greater biological responsivity to stress that men tend to exhibit (McEwen, Citation2000; Yang & Kozloski, Citation2011).
Along with sex, Juster and Lupien (Juster & Lupien, Citation2012) highlight the importance of gender roles in the stress-AL paradigm. Gender roles are often driven by an individual's perception of their maleness-femaleness and are reflected in the degree to which they adopt masculine and/or feminine-typical behaviours; for example, masculinity is often associated with an assertive and competitive perspective on social interactions, while femininity is typically viewed as taking shape in an approach that may be described as more nurturing and sensitive (Juster et al., Citation2016; Kerr et al., Citation2020). Notably, while investigating gender roles and AL in a sample of workers, Juster and Lupien (Juster & Lupien, Citation2012) revealed that traits associated with masculinity predicted higher AL, unlike those typically associated with feminity, regardless of biological sex.
Firefighting remains an overwhelmingly male profession, with men comprising about 95% of the population in the US (ZIPPIA, Citation2022) and Canada (P-SEC, Citation2021). Often, women who have joined the fire service are subjected to a hyper-masculine environment that requires acculturation. At the same time, they must navigate gender-influenced attitudes and work patterns to earn respect from their male counterparts (Sinden et al., Citation2013). Such experiences, coupled with their minority status in a male-dominated occupation, may reasonably be expected to create conditions wherein female firefighters develop higher AL than their male colleagues. Hence, along with providing a more nuanced and deeper understanding of the stress-AL relationship, there is likely to be significant value for organisations in applying sex – and gender-based analysis when utilising the AL framework to investigate firefighter health.
Ethnicity and allostatic load
Ethnicity has previously been shown to influence AL either independently, or along with other variables such as education level and socioeconomic status (Beckie, Citation2012). Since ethnic minorities often experience discrimination more than their counterparts, such inimical events may contribute to AL and its adverse health outcomes (Peek et al., Citation2010). For example, a study with US adults showed that Black individuals, especially Black women, were at least 1.5 times more likely to record higher mean AL scores (≥4) than Whites after accounting for age and poverty (Geronimus et al., Citation2006). Unfavourable socioeconomic conditions, system-level discrimination, a comparative lack of available psychosocial resources, and the burden of intersectionality (i.e. bearing more than one marginalised designation, particularly among Black women) may help explain the observed connection between ethnicity and AL (Chyu & Upchurch, Citation2011; Geronimus et al., Citation2006; Tobin et al., Citation2021; Upchurch et al., Citation2015).
In the United States, the demographic make-up for most fire stations typically consists of white (non-Hispanic) men, with other racial-ethnic groups clearly in the minority (ZIPPIA, Citation2022). As elucidated earlier, the minority status of an ethnic group may contribute to additional stressful experiences that follow from discriminatory practices within the workplace (Arbona et al., Citation2017; Deitch et al., Citation2003; Yoder & Aniakudo, Citation1997). For this reason, considering ethnicity while investigating firefighters, especially in urban areas, is necessary to fully understand how workplaces may be a source of stress, the sort of variations present in AL among certain ethnic groups, and the complex interactions that the stress-AL relationship can have with other variables (for example, the availability of psychosocial resources like social and administrative support).
Modifiable secondary variables
Along with the variables noted earlier, several modifiable factors have displayed varying degrees of association with AL among firefighters, such as psychosocial coping resources and health-related behaviours like physical activity, eating habits, and alcohol intake (Schneiderman et al., Citation2005; Suvarna et al., Citation2020).
Psychosocial resources and allostatic load
Psychosocial resources constitute personal and relational factors that provide intrinsic support for mental and physical health (Wiley et al., Citation2017). Such resources may take shape at the individual level (e.g. self-efficacy), or through interpersonal interactions such as social relationships (Wiley et al., Citation2017). Indeed, psychosocial resources may either prevent stress via proactive coping and promulgating healthy behaviours, or moderate the response to a stressor by attenuating its effect; regardless, the result will be to reduce the physiological imprint left by stressors (Aspinwall & Taylor, Citation1997; Haly, Citation2009; Wiley et al., Citation2017).
Given that social support has been shown to enhance resilience amongst firefighters by providing perceived acceptance and camaraderie, which can cushion the effect of stress exposure in these workers, this psychosocial resource may act as an essential variable influencing the accumulation of AL (Beaton & Murphy, Citation1993; Regehr, Citation2009; Regehr et al., Citation2003). Also, previous work with firefighters has shown that self-efficacy and resilience are essential coping resources for overcoming work-related stressors and their outcomes (Makara-Studzińska et al., Citation2019). Specifically, both resources buffer the effect of stress via behavioural self-regulation (i.e. impulse control and reorientation towards healthy coping choices) (Igboanugo et al., Citation2021; Makara-Studzińska et al., Citation2019). In sum, since psychosocial resources can act as protective factors in the stress-outcome relationship, considering them when investigating AL within firefighters would be quite informative.
Behavioural habits and allostatic load
Increased physical activity has been linked to reduced psychosocial stress experience and response, with subsequent dampening of HPA axis reactivity and cortisol release (Klaperski et al., Citation2013; Milani & Lavie, Citation2009; Rimmele et al., Citation2007). Empirical evidence also indicates a significant reduction in AL and its metabolic and cardiovascular outcomes with increased participation in physical activity, irrespective of demography (i.e. sex, race, and age) (Gay et al., Citation2015; Petrovic et al., Citation2016; Upchurch, Rainisch, et al., Citation2015).
Firefighters are generally encouraged to participate in physical activity, especially between calls while on duty, to maintain the aerobic fitness, muscular strength, and endurance required for their jobs (Pawlak et al., Citation2015). Indeed, their participation in voluntary physical activities and the need to meet the fitness guidelines required for firefighting may play a vital protective role against AL in this group. As a result, there is considerable value in accounting for the potential influence of physical activity on the stress-AL relationship in firefighters. Additionally, given the assumption of higher fitness levels amongst firefighters, which is a likely contributor to the ‘healthy worker effect’, considering the effect that physical activity may have on AL will provide a more nuanced assessment of the impact that stress may have on firefighter health.
Unhealthy eating habits, such as consumption of food and beverages high in salt, fat, or sugar, contribute to (abdominal) obesity (Paradis et al., Citation2009) and have been linked to elevated AL and outcomes such as cardiovascular disease (Mattei et al., Citation2011; van Draanen et al., Citation2018). Further, evidence suggests that individuals crave and consume comfort foods (i.e. high-fat and sugary meals/snacks) to cope with work-related stress (Suvarna et al., Citation2020).
Notably, evidence shows firefighters gravitate toward fatty, sugary, and calorie-dense carbohydrate meals, contributing to the growing obesity rates observed among this population of workers (Della et al., Citation2019; López-Bermudo & Gómez-Landero, Citation2021; Muegge et al., Citation2018; Yang et al., Citation2014). For example, Lopez-Bermudo and Gomez-Landero (López-Bermudo & Gómez-Landero, Citation2021) report that within a sample of 28 firefighters, 35% consumed more snacks during their shifts compared to their days off, while 40% reported indulging in unhealthy snacks like pastries. Factors contributing to unhealthy eating habits among firefighters may be psychosocial (collegial influence, lifestyle choices), physiological (boredom snacking, stress eating), or related to the work environment (firehouse eating culture, shift work) (Della et al., Citation2019; Muegge et al., Citation2018). Therefore, based on the available evidence, eating habits among firefighters should be included as part of any investigation into the relationship between work-related stress and AL.
Regarding alcohol use, definite conclusions about its effect on AL are yet to be made. That is, some studies have recorded a beneficial effect of moderate alcohol intake (1–21 units/week for men and 1–14 units/week for women; 1 unit = 10 g of pure alcohol) against AL in men and women (Gallo et al., Citation2011; Petrovic et al., Citation2016). In contrast, Crimmins et al. (Crimmins et al., Citation2009) found no association between alcohol consumption and AL. Within the fire service, alcohol is often consumed for social and coping reasons (Jahnke et al., Citation2014). Unfortunately, problematic alcohol use is prevalent among firefighters; for instance, Haddock et al. (Haddock et al., Citation2012) and Piazza-Gardner et al. (Piazza-Gardner et al., Citation2014) both revealed high levels of binge-drinking over the past month (56%, n = 656 and 34%, n = 160, respectively). Based on the prevalence of problematic alcohol use, attention must be directed to measuring alcohol consumption and considering its potential role in the effect that work-related psychosocial stress may have upon AL in firefighters.
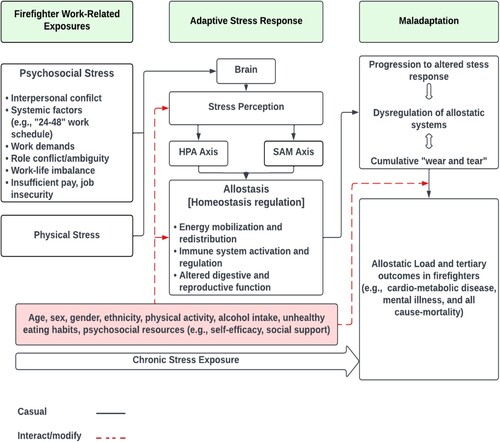
illustrates the framework proposed for studying work-related stress exposure, AL, and health outcomes in firefighters.
Figure 1 . A diagram illustrating the framework for work-related stress exposure, allostatic load build-up, and potential adverse health outcomes in firefighters.
Challenges and opportunities
Despite the AL framework's advantages, certain challenges are present. For example, some physiological variables measured for the AL index can require significant effort, financial investment, and skill. Indeed, collecting specific biomarkers can require invasive techniques that require expertise and a more stringent ethical review process. In particular, blood collection for parameters like cortisol often requires specialised techniques and professional oversight. However, recent technological and analytical advances have created opportunities to measure less invasive parameters (such as monitoring heart-rate variability with wearable devices, or measuring hair cortisol concentration).
An additional challenge related to data collection that cannot be overlooked concerns sample processing times and compliance issues. That is, the time needed to process collected samples may be prolonged depending on study type (cross-sectional, or longitudinal), sample size, and the number of retrieved parameters. For example, some biological samples (e.g. blood) may require unique storage processes, whereas others (such as hair) may require specific steps to be followed to isolate the compound of interest (i.e. cortisol). In some instances, considerable time may be spent on such processes, creating logistical challenges. In addition, the measurement frequency of specific physiological parameters (e.g. cortisol assessment in saliva) may burden participants and carry a potential risk of issues with compliance. A related obstacle to data collection that must be considered concerns the busy, often unpredictable, work schedule firefighters follow, which may affect participation and attrition.
A challenge related to interpreting findings from the AL model is the potential lack of agreement between self-report measures of perceived stress and the AL index (Brown et al., Citation2016). A handful of reasons may account for such psychophysiological discordance. One possibility is that individuals may perceive their stress levels as manageable, and this is especially the case with firefighters who, by the nature of their job and workplace culture, often exhibit composure and resiliency; however, the biomarkers used to compose an ALI may capture stress and physiological dysregulation beyond individual awareness. Also, the lack of agreement could arise from assessment deficiencies that render some self-report measures unable to faithfully capture stress experiences compared to assessments based on the AL model (Brown et al., Citation2016). Finally, when considering the timeframe reflected in each assessment, self-report measures often focus on the time around the measurement, whereas the ALI captures the cumulative effect of changes that may have occurred over more extended periods.
Despite the points noted, various opportunities abound with the AL framework. First, applying the AL model within firefighter research will prove useful in identifying (i) stressful aspects of their psychosocial environment, (ii) factors that may either build, or weaken resiliency, and (iii) the progressive impact of stress on their health. Also, continued application of the model will help reveal the specific physiological biomarkers that can best capture the progression of stress-related chronic conditions prevalent in firefighters, such as cardiovascular disease.
Furthermore, ensuing research from the application of the AL model will provide greater interest for empirical inquiry into firefighters and other first responders (e.g. police) that may illuminate other aspects of their social and environmental stress experience, including those outside the workplace. Additionally, such research should serve to motivate further work to investigate the interaction of occupation-specific factors such as geographical (urban vs rural) firefighting location, rank, and years of service with psychosocial stress and health outcomes among firefighters.
Finally, the AL framework offers a reasonable action window to target AL's antecedents to prevent adverse health outcomes for firefighters. With such an opportunity, relevant stakeholders, including epidemiologists, occupational health experts, and policymakers, may obtain the information needed to design interventions, create policies, and allocate resources that improve the health and wellbeing of firefighters.
Conclusions and recommendations for future research
Firefighters are an essential group of public servants who place their lives at risk for the safety of others, so protecting their health and wellbeing, while being an important goal on its own, will also yield much broader benefits. Hence, understanding more about AL and its associated adverse health outcomes within this professional group deserves urgent research consideration.
Having outlined compelling evidence highlighting the utility of the AL model in elucidating the complex stress-disease relationship, applying the framework in addressing psychosocial antecedents of stress and their related consequences among firefighters should appear as a natural next step. The utilisation of the AL model in firefighter research should include experimental investigations and observational studies, especially the longitudinal type, that consider various contextual and interacting factors to provide a comprehensive understanding of the health implications of AL in these workers.
As interest grows and the operationalisation of the AL framework gains momentum, there should be a consolidation in retrieving biomarkers, development of improved analytical equipment, and standardisation of the AL biomarkers used to determine the cumulative physiological consequences of stress within firefighters. Such knowledge would help advance biobehavioural research and practice, and assist in developing health-promoting interventions that seek to improve the health and wellbeing of firefighters and other first-responders.
Ethics Statement
The study was exempted from the University of Waterloo Office of Research Ethics; see details under General Orientation and Objectives.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- An, S., Chung, Y. K., Kim, B. H., Kwak, K. M., Son, J., Koo, J., Ju, Y. S., & Kwon, Y. J. (2015). The effect of organisational system on self-rated depression in a panel of male municipal firefighters. Annals of Occupational and Environmental Medicine, 27(1), 1–7. https://doi.org/10.1186/s40557-014-0044-x
- Ângelo, R. P., & Chambel, M. J. (2013). The reciprocal relationship between work characteristics and employee burnout and engagement: A longitudinal study of firefighters. Stress and Health, 31(2), 106–114. https://doi.org/10.1002/smi.2532
- Arbona, C., Pao, C., Long, A., & Olvera, N. (2017). Perceived stress in black and latino male firefighters: Associations with risk and protective factors. Ethnicity & Disease, 27(4), 421–428. https://doi.org/10.18865/ed.27.4.421
- Aspinwall, L. G., & Taylor, S. E. (1997). A stitch in time: Self-regulation and proactive coping. Psychological Bulletin, 121(3), 417–436. https://doi.org/10.1037/0033-2909.121.3.417
- Banes, C. (2014). Firefighters’ cardiovascular risk behaviors. Effective Interventions and Cultural Congruence. Work Heal Saf, 62(1), 27–35.
- Barger, L. K., Lockley, S. W., Rajaratnam, S. M. W., & Landrigan, C. P. (2009). Neurobehavioral, health, and safety consequences associated with shift work in safety-sensitive professions. Current Neurology and Neuroscience Reports, 9(2), 155–164. https://doi.org/10.1007/s11910-009-0024-7
- Barr, D., Gregson, W., & Reilly, T. (2010). The thermal ergonomics of firefighting reviewed. Applied Ergonomics, 41(1), 161–172. Available from: https://doi.org/10.1016/j.apergo.2009.07.001.
- Beaton, R., & Murphy, S. A. (1993). Sources of occupational stress among firefighter/EMTs and firefighter/paramedics and correlations with job-related outcomes. Prehospital and Disaster Medicine, 8(02), 140–150. https://doi.org/10.1017/S1049023X00040218
- Beckie, T. M. (2012). A systematic review of allostatic load, health, and health disparities. Biological Research for Nursing, 14(4), 311–346. https://doi.org/10.1177/1099800412455688
- Bellingrath, S., Weigl, T., & Kudielka, B. M. (2009). Chronic work stress and exhaustion is associated with higher allostastic load in female school teachers. Stress, 12(1), 37–48. https://doi.org/10.1080/10253890802042041
- Bizik, G., Picard, M., Nijjar, R., Tourjman, V., McEwen, B. S., Lupien, S. J., & Juster, R. P. (2013). Allostatic load as a tool for monitoring physiological dysregulations and comorbidities in patients with severe mental illnesses. Harvard Review of Psychiatry, 21(6), 296–313. https://doi.org/10.1097/HRP.0000000000000012
- Brown, T. N., Turner, R. J., & Moore, T. R. (2016). The multidimensionality of health: Associations between allostatic load and self-report health measures in a community epidemiologic study. Health Sociology Review, 25(3), 272–287. https://doi.org/10.1080/14461242.2016.1184989.
- Carbone, J. T., Clift, J., & Alexander, N. (2022). Measuring allostatic load: Approaches and limitations to algorithm creation. Journal of Psychosomatic Research, 163(September), 111050. https://doi.org/10.1016/j.jpsychores.2022.111050.
- Chang, S., Koh, S., Kang, D., Kim, S., Kang, M., Lee, C., Chung, J. J., Cho, J. J., Son, M., Chae, C. H., & Kim, J. W. (2005). Developing an occupational stress scale for Korean employees. Korean Journal of Occupational and Environmental Medicine, 17(4), 297–317. https://doi.org/10.35371/kjoem.2005.17.4.297
- Choi, B. (2000). A technique to Re-assess epidemiologic evidence in light of the healthy worker effect: The case of firefighting and heart disease. Journal of Occupational and Environmental Medicine, 42(10), 1021–1034. https://doi.org/10.1097/00043764-200010000-00009
- Choi, B., Schnall, P., & Dobson, M. (2016). Twenty-four-hour work shifts, increased job demands, and elevated blood pressure in professional firefighters. International Archives of Occupational and Environmental Health, 89(7), 1111–1125. https://doi.org/10.1007/s00420-016-1151-5
- Chrousos, G. P. (2009). Stress and disorders of the stress system. Nature Reviews Endocrinology, 5(7), 374–381. Available from: https://doi.org/10.1038/nrendo.2009.106.
- Chyu, L., & Upchurch, D. M. (2011). Racial and ethnic patterns of allostatic load among adult women in the United States: Findings from the national health and nutrition examination survey 1999-2004. Journal of Women's Health, 20(4), 575–583. https://doi.org/10.1089/jwh.2010.2170
- Clark, M. S., Bond, M. J., & Hecker, J. R., (2007). Environmental stress, psychological stress and allostatic load. Psychology, Health & Medicine, 12(1), 18–30. https://doi.org/10.1080/13548500500429338
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. https://doi.org/10.2307/2136404
- Crimmins, E. M., Johnston, M., Hayward, M., & Seeman, T. (2003). Age differences in allostatic load: An index of physiological dysregulation. Experimental Gerontology, 38(7), 731–734. https://doi.org/10.1016/S0531-5565(03)00099-8
- Crimmins, E. M., Kim, J. K., & Seeman, T. E. (2009). Poverty and biological risk: The earlier "aging" of the poor. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 64A(2), 286–292. https://doi.org/10.1093/gerona/gln010
- de Castro, A., Voss, J., Ruppin, A., Dominguez, C., & Seixas, N. (2010). Stressors among latino day laborers a pilot study examining allostatic load. American Association Occupational Health Nurses, 58(5), 185–196.
- Deitch, E. A., Barsky, A., Butz, R. M., Chan, S., Brief, A. P., & Bradley, J. C. (2003). Subtle yet significant: The existence and impact of everyday racial discrimination in the workplace. Human Relations, 56(11), 1299–1324. https://doi.org/10.1177/00187267035611002
- Della, T. S., Wild, P., Dorribo, V., Amati, F., & Danuser, B. (2019). Eating habits of professional firefighters. Journal of Occupational & Environmental Medicine, 61(5), E183–E190. https://doi.org/10.1097/JOM.0000000000001565
- Driessen, J. (2002). Crew cohesion, wildland fire transition, and fatalities. Washington DC: United States Department of Agriculture, Forest Service, Technology and Development Program. TE02P16.
- Durand, G. A., de Laval, F., de Bonet D’Oléon, A., Le Flem, F. X., Morin, Y., Badaut, C., Grard, G., Brossier, C., Fossier, M., Dia., A., & Letois, F. (2021). COVID-19 outbreak among French firefighters, Marseille, France, 2020. Eurosurveillance, 26(41), 1–9. https://doi.org/10.2807/1560-7917.ES.2021.26.41.2001676.
- Edes, A. N., Wolfe, B. A., & Crews, D. E. (2018). Evaluating allostatic load: A new approach to measuring long-term stress in wildlife. Journal of Zoo and Wildlife Medicine, 49(2), 272–282. https://doi.org/10.1638/2016-0070.1
- Fisher, P., & Abrahamson, K. (2002). When working hurts: Stress, burnout & trauma in human, emergency, and health services. Spectrum Press.
- Fisher, P., & Etches, B. (2003). A comprehensive approach to workplace stress & trauma in fire-fighting. International Association of Firefighters 17th Redmond Symposium [Internet], 1–7. Available from: http://www.fisherandassociates.org/pdf/Firefighters_03.pdf
- Gallo, L. C., Jiménez, J. A., Shivpuri, S., De Los Monteros K, E., & Mills, P. J. (2011). Domains of chronic stress, lifestyle factors, and allostatic load in middle-aged Mexican-American women. Annals of Behavioral Medicine, 41(1), 21–31. https://doi.org/10.1007/s12160-010-9233-1
- Ganster, D. C., & Rosen, C. C. (2013). Work stress and employee health: A multidisciplinary review. Journal of Management [Internet], 39(5), 1085–1122. http://jom.sagepub.com.ezproxy.ecu.edu.au/content/39/5/1085.full.pdf+html
- Gay, J. L., Salinas, J. J., Buchner, D. M., Mirza, S., Kohl, H. W., Fisher-Hoch, S. P., & McCormick, J.B. (2015). Meeting physical activity guidelines is associated with lower allostatic load and inflammation in Mexican Americans. Journal of Immigrant and Minority Health, 17(2), 574–581. https://doi.org/10.1007/s10903-013-9950-1
- Geronimus, A. T., Hicken, M., Keene, D., & Bound, J. (2006). ““Weathering” and Age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health, 96(5), 826–833. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1470581/pdf/0960826.pdf
- Gilbert, M., & Samra, J. (2010). Guarding minds @ work: A workplace guide to psychological safety and health. Can Benefits Compens Dig, 28(4), 10–12.
- Glei, D. A., Goldman, N., Chuang, Y. L., & Weinstein, M. (2007). Do chronic stressors lead to physiological dysregulation? Testing the theory of allostatic load. Psychosomatic Medicine, 69(8), 769–776. https://doi.org/10.1097/PSY.0b013e318157cba6
- Godoy, L. D., Rossignoli, M. T., Delfino-Pereira, P., Garcia-Cairasco, N., & de Lima Umeoka, E. H. (2018). A comprehensive overview on stress neurobiology: Basic concepts and clinical implications. Frontiers in Behavioral Neuroscience [Internet], 12(July), 1–23. https://www.frontiersin.org/article/10.3389fnbeh.2018.00127/full
- Goh, K. K., Jou, S., Lu, M., Yeh, L.-C., Kao, Y.-F., Liu, C.-M., & Kan, B. L. (2020). Younger, more senior, and most vulnerable? Interaction effects of age and job seniority on psychological distress and quality of life among firefighters. Psychological Trauma: Theory, Research, Practice, and Policy, 13(1), 56–65. https://doi.org/10.1037/tra0000662.
- Guidi, J., Sonino, N., & Fava, A. (2021). Allostatic load and Its impact on health: A systematic review. Psychotherapy and Psychosomatics, 90(1), 11–27. https://doi.org/10.1159/000510696
- Guidotti, T. L. (1992). Human factors in firefighting: Ergonomic-, cardiopulmonary-, and psychogenic stress-related issues. International Archives of Occupational and Environmental Health, 64(1), 1–12. https://doi.org/10.1007/BF00625945
- Guidotti, T. L., & Clough, V. M. (1992). Occupational health concerns of firefighting. Annual Review of Public Health, 13(1), 151–171. https://doi.org/10.1146/annurev.pu.13.050192.001055
- Gustafsson, P. E., Sebastian, M. S., Janlert, U., Theorell, T., Westerlund, H., & Hammarström, A. (2014). Life-Course accumulation of neighborhood disadvantage and allostatic load: Empirical integration of three social determinants of health frameworks. American Journal of Public Health, 104(5), 904–910. https://doi.org/10.2105/AJPH.2013.301707
- Haddock, C., Jahnke, S. A., Poston, W. S. C., Jitnarin, N., Kaipust, C. M., Tuley, B., & Hyder, M. L. (2012). Alcohol use among firefighters in the central United States. Occupational Medicine, 62(8), 661–664. https://doi.org/10.1093/occmed/kqs162
- Haddock, C., Poston, W. S. C., Jitnarin, N., & Jahnke, S. A. (2013). Excessive daytime sleepiness in firefighters in the Central United States. Journal of Occupational & Environmental Medicine, 55(4), 416–423. https://doi.org/10.1097/JOM.0b013e31827cbb0b
- Haly, M. K. (2009). A review of contemporary research on the relationship between occupational stress and social support: Where are we now? Australian and New Zealand Journal of Organizational Psychology, 2(August 2009), 44–63.
- Hurrell, J., & McLaney, M. (1988). Exposure to job stress: A new psychometric instrument. Scandinavian Journal of Work Environment & Health, 14, 27–28.
- Igboanugo, S., Bigelow, P. L., & Mielke, J. G. (2021). Health outcomes of psychosocial stress within firefighters: A systematic review of the research landscape. Journal of Occupational Health, 63(1), e12219–e12241. https://doi.org/10.1002/1348-9585.12219.
- Isaac, G. M., & Buchanan, M. J. (2021). Extinguishing stigma among firefighters: An examination of stress, social support, and help-seeking attitudes. Psychology (savannah, Ga ), 12(03), 349–373. https://doi.org/10.4236/psych.2021.123023
- Jahnke, S. A., Carlos, W. S., & Haddock, C. K. (2016). Firefighting and mental health: Experiences of repeated exposure to trauma. work, 53(4), 737–744. https://doi.org/10.3233/WOR-162255
- Jahnke, S. A., Poston, W., & Haddock, C. (2014). Perceptions of alcohol use among US firefighters. Journal of Substance Abuse and Alcoholism, 2(2), 1012–1019.
- Juster, R.-P., & Lupien, S. (2012). A sex- and gender-based analysis of allostatic load and physical complaints. Gender Medicine, 9(6), 511–523. https://doi.org/10.1016/j.genm.2012.10.008.
- Juster, R.-P., McEwen, B. S., & Lupien, S. J. (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews, 35(1), 2–16. https://doi.org/10.1016/j.neubiorev.2009.10.002.
- Juster, R.-P., Pruessner, J. C., Desrochers, A. B., Bourdon, O., Durand, N., Wan, N., Tourjman, V., Kouassi, E., Lesage, A., & Lupien, S.J. (2016). Sex and gender roles in relation to mental health and allostatic load. Psychosomatic Medicine, 78(7), 788–804. https://doi.org/10.1097/PSY.0000000000000351
- Juster, R.-P., Russell, J. J., Almeida, D., & Picard, M. (2016). Allostatic load and comorbidities: A mitochondrial, epigenetic, and evolutionary perspective. Development and Psychopathology, 28(2016), 1117–1146. https://doi.org/10.1017/S0954579416000730
- Karasek, R., Amick, B., Kawakami, N., Brisson, C., Houtman, I., & Bongers, P. (1998). The Job content questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial Job characteristics. Journal of Occupational Health Psychology, 3(4), 322–355. https://doi.org/10.1037/1076-8998.3.4.322
- Karlamangla, A. S., Singer, B. H., Mcewen, B. S., Rowe, J. W., & Seeman, T. E. (2002). Allostatic load as a predictor of functional decline. Journal of Clinical Epidemiology, 55(7), 696–710. https://doi.org/10.1016/S0895-4356(02)00399-2
- Kaur, H., Luckhaupt, S. E., Li, J., Alterman, T., & Calvert, G. M. (2014). Workplace psychosocial factors associated with hypertension in the U.S. Workforce: A cross-sectional study based on the 2010 national health interview survey. American Journal of Industrial Medicine, 57(9), 1011–1021. https://doi.org/10.1002/ajim.22345
- Kerr, P., Kheloui, S., Rossi, M., Désilets, M., & Juster, R. P. (2020). Allostatic load and women’s brain health: A systematic review. Frontiers in Neuroendocrinology, 59(July), 100858. https://doi.org/10.1016/j.yfrne.2020.100858.
- Kimbrel, N. A., Steffen, L. E., Meyer, E. C., Kruse, M. I., Knight, J. A., Zimering, R. T., & Gulliver, S.B. (2011). A revised measure of occupational stress for firefighters: Psychometric properties and relationship to posttraumatic stress disorder, depression, and substance abuse. Psychological Services, 8(4), 294–306. http://doi.apa.org/getdoi.cfm?doi=10.1037a0025845
- King, L. (2011). Mandatory retirement. Firefighting in Canada [Internet]. https://www.firefightingincanada.com/mandatory-retirement-8648/
- Klaperski, S., von Dawans, B., Heinrichs, M., & Fuchs, R. (2013). Does the level of physical exercise affect physiological and psychological responses to psychosocial stress in women? Psychology of Sport and Exercise, 14(2), 266–274. https://doi.org/10.1016/j.psychsport.2012.11.003.
- Kristensen, T. S., Hannerz, H., Høgh, A., Borg, V., & Scandinavian, S. (2005). The Copenhagen psychosocial questionnaire—a tool for the assessment and improvement of the psychosocial work environment. Scandinavian Journal of Work, Environment & Health, 31(6), 438–449. https://doi.org/10.5271/sjweh.948
- Li, C. Y., & Sung, F. C. (1999). A review of the healthy worker effect in occupational epidemiology. Occupational Medicine, 49(4), 225–229. https://doi.org/10.1093/occmed/49.4.225
- López-Bermudo, L., & Gómez-Landero, L. A. (2021). Healthy habits in firefighters: Assessment in shift days versus days off. Journal of Occupational & Environmental Medicine, 63(9), e580–e585. https://doi.org/10.1097/JOM.0000000000002289
- Lourel, M., Abdellaoui, S., Chevaleyre, S., & Paltrier, M. (2008). Relationships between psychological job demands, job control and burnout among firefighters. North American Journal of Psychology, 10(3), 489–495.
- Mair, C. A., Cutchin, M. P., & Kristen Peek, M. (2011). Allostatic load in an environmental riskscape: The role of stressors and gender. Health & Place, 17(4), 978–987. https://doi.org/10.1016/j.healthplace.2011.03.009.
- Makara-Studzińska, M., Golonka, K., & Izydorczyk, B. (2019). Self-efficacy as a moderator between stress and professional burnout in firefighters. International Journal of Environmental Research and Public Health, 16(2). https://doi.org/10.3390/ijerph16020183
- Mattei, J., Noel, S. E., & Tucker, K. L. (2011). A meat, processed meat, and French fries dietary pattern is associated with high allostatic load in puerto rican older adults. Journal of the American Dietetic Association, 111(10), 1498–1506. https://doi.org/10.1016/j.jada.2011.07.006.
- Mauss, D., & Jarczok, M. N. (2021). The streamlined allostatic load index is associated with perceived stress in life – findings from the MIDUS study. Stress, 24(4), 404–412. https://doi.org/10.1080/10253890.2020.1869935.
- Mauss, D., Jarczok, M. N., & Fischer, J. E. (2015). A streamlined approach for assessing the allostatic load index in industrial employees. Stress, 18(4), 475–483. https://doi.org/10.3109/10253890.2015.1040987
- Mauss, D., Jarczok, M. N., & Fischer, J. E. (2016). The streamlined allostatic load index: A replication of study results. Stress, 19(6), 553–558. https://doi.org/10.1080/10253890.2016.1219718
- McEwen, B. S. (1998). Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences, 33–44. https://doi.org/10.1111/j.1749-6632.1998.tb09546.x
- McEwen, B. S. (2000). Allostasis and allostatic load implications for neuropsychopharmacology. Neuropsychopharmacology, 22(2), 108–124. https://doi.org/10.1016/S0893-133X(99)00129-3
- McEwen, B. S., & Seeman, T. E. (1999). Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences, 896(1), 30–47. https://doi.org/10.1111/j.1749-6632.1999.tb08103.x
- McEwen, B. S., & Stellar, E. (1993). Stress and the individual. Archives of Internal Medicine, 153(18), 2093–2101. https://doi.org/10.1001/archinte.1993.00410180039004
- McEwen, B. S., & Wingfield, J. C. (2003). The concept of allostasis in biology and biomedicine. Hormones and Behavior, 43(1), 2–15. https://doi.org/10.1016/S0018-506X(02)00024-7
- McLoughlin, S., Kenny, R. A., & McCrory, C. (2020). Does the choice of allostatic load scoring algorithm matter for predicting age-related health outcomes? Psychoneuroendocrinology, 120(April), 104789. https://doi.org/10.1016/j.psyneuen.2020.104789.
- McLoughlin, S., Kenny, R. A., & McCrory, C. (2021). Psychosocial adversity and allostatic load burden in midlife and older ages. Health Psychology, 40(7), 468–471. https://doi.org/10.1037/hea0001098
- Milani R. V., & Lavie, C. J. (2009). Reducing psychosocial stress: A novel mechanism of improving survival from exercise training. The American Journal of Medicine, 122(10), 931–938. https://doi.org/10.1016/j.amjmed.2009.03.028.
- Muegge, C. M., Kleinschmidt, V. M., Johnson, K., Sotos-Prieto, M., Moffatt, S., Beverly, E., Korre, M., & Kales, S. N. (2018). Focus groups to inform a nutrition intervention for career firefighters. Clinical Nutrition and Metabolism, 1(2), 1–5. https://doi.org/10.15761/CNM.1000108
- Murphy, S. A., Beaton, R. D., Pike, K. C., & Johnson, L. C. (1999). Occupational stressors, stress responses, and alcohol consumption among professional firefighters: A prospective, longitudinal analysis. International Journal of Stress Management, 6(3), 179–196. https://doi.org/10.1023/A:1021934725246
- Mustajbegovic, J., Zuskin, E., Schachter, E. N., Kern, J., Vrcic-keglevic, M., & Heimer, S. (2001). Respiratory function in active firefighters. American Journal of Industrial Medicine, 40(1), 55–62. https://doi.org/10.1002/ajim.1071
- Orr, R., Simas, V., Canetti, E., & Schram, B. (2019). A profile of injuries sustained by firefighters: A critical review. International Journal of Environmental Research & Public Health, 16(20), 3931–3951. https://doi.org/10.3390/ijerph16203931
- Paradis, A. M., Godin, G., Pérusse, L., & Vohl, M. C. (2009). Associations between dietary patterns and obesity phenotypes. International Journal of Obesity, 33(12), 1419–1426. https://doi.org/10.1038/ijo.2009.179
- Pawlak, R., Clasey, J. L., Palmer, T., Symons, T. B., & Abel, M. G. (2015). The effect of a novel tactical training program on physical fitness and occupational performance in firefighters. Journal of Strength and Conditioning Research, 29(3), 578–588. https://doi.org/10.1519/JSC.0000000000000663
- Payne, N., & Kinman, G. (2019). Job demands, resources and work-related well-being in UK firefighters. Occupational Medicine, 69(8–9), 604–609. https://doi.org/10.1093/occmed/kqz167
- Peek, K. M., Cutchin, M. P., Salinas, J. J., Sheffield, K. M., Eschbach, K., Stowe, R. P., & Goodwin, J. S. (2010). Allostatic load among non-hispanic whites, non-hispanic blacks, and people of Mexican origin: Effects of ethnicity, nativity, and acculturation. American Journal of Public Health, 100(5), 940–946. https://doi.org/10.2105/AJPH.2007.129312
- Petrovic, D., Pivin, E., Ponte, B., Dhayat, N., Pruijm, M., Ehret, G., Ackermann, D., Guessous, I., Younes, S. E., Pechere-Bertschi, A. & Vogt, B. (2016). Sociodemographic, behavioral and genetic determinants of allostatic load in a Swiss population-based study. Psychoneuroendocrinology, 67, 76–85. https://doi.org/10.1016/j.psyneuen.2016.02.003.
- Piazza, J. R., Stawski, R. S., & Sheffler, J. L. (2019). Age, daily stress processes, and allostatic load: A longitudinal study. Journal of Aging and Health, 31(9), 1671–1691. https://doi.org/10.1177/0898264318788493
- Piazza-Gardner, A. K., Barry, A. E., Chaney, E., Dodd, V., Weiler, R., & Delisle, A. (2014). Covariates of alcohol consumption among career firefighters. Occupational Medicine, 64(8), 580–582. https://doi.org/10.1093/occmed/kqu124
- Pluntke, U., Gerke, S., Sridhar, A., Weiss, J., & Michel, B. (2019). Evaluation and classification of physical and psychological stress in firefighters using heart rate variability. 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), (pp. 2207-2212). 2019 Jul 23.
- P-SEC. (2021). Women firefighters [Internet]. Psycho-Social Ethnography of the Commonplace (P-SEC) research group. https://p-sec.org/en/project/women-firefighters/
- Rajabi, F., Molaeifar, H., Jahangiri, M., Taheri, S., Banaee, S., & Farhadi, P. (2020). Occupational stressors among firefighters: Application of multi-criteria decision making (MCDM)Techniques. Heliyon, 6(4), e03820. https://doi.org/10.1016/j.heliyon.2020.e03820.
- Read, S., & Grundy, E. (2014). Allostatic load and health in the older population of England. Psychosomatic Medicine, 76(7), 490–496. https://doi.org/10.1097/PSY.0000000000000083
- Regehr, C. (2009). Social support as a mediator of psychological distress in firefighters. The Irish Journal of Psychology, 30(1–2), 87–98. https://doi.org/10.1080/03033910.2009.10446300
- Regehr, C., Hill, J., Knott, T., & Sault, B. (2003). Social support, self-efficacy and trauma in new recruits and experienced firefighters. Stress and Health, 19(4), 189–193. https://doi.org/10.1002/smi.974
- Rimmele, U., Zellweger, B. C., Marti, B., Seiler, R., Mohiyeddini, C., Ehlert, U., & Heinrichs, M. (2007). Trained men show lower cortisol, heart rate and psychological responses to psychosocial stress compared with untrained men. Psychoneuroendocrinology, 32(6), 627–635. https://doi.org/10.1016/j.psyneuen.2007.04.005
- Saijo, Y., Ueno, T., & Hashimoto, Y. (2007). Job stress and depressive symptoms among Japanese fire fighters. American Journal of Industrial Medicine, 50(6), 470–480. https://doi.org/10.1002/ajim.20460
- Salleh, M. N. M., Ismail, H., & Yusoff, H. (2020). Prevalence and predictors for post-traumatic stress disorder. Int J Public Heal Res, 10(1), 1183–1194.
- Schneiderman, N., Ironson, G., & Siegel, S. D. (2005). Stress and health: Psychological, behavioral, and biological determinants. Annual Review of Clinical Psychology, 1(1), 607–628. https://doi.org/10.1146/annurev.clinpsy.1.102803.144141
- Schnorpfeil, P., Noll, A., Schulze, R., Ehlert, U., Frey, K., & Fischer, J. E. (2003). Allostatic load and work conditions. Social Science & Medicine, 57(4), 647–656. https://doi.org/10.1016/S0277-9536(02)00407-0
- Schuhmann, B. B., Henderson, S. N., Black, R. A., Van Hasselt, V. B., Klimley Margres, K., Masias E, V., & LeDuc, T. J. (2022). A behavioral-analytic model for assessing stress in firefighters. Behavior Modification, 46(2), 267–293. https://doi.org/10.1177/0145445520986137
- Seeman, T. E., Mcewen, B. S., Rowe, J. W., & Singer, B. H. (2001). Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences, 98(8). https://doi.org/10.1073/pnas.081072698
- Seeman, T. E., Singer, B. H., Rowe, J. W., Horwitz, R. I., & Mcewen, B. S. (1997). Price of adaptation—allostatic load and Its health consequences. Archives of Internal Medicine, 157(19), 2259–2268. https://doi.org/10.1001/archinte.1997.00440400111013
- Shreffler, K., Meadows, M., & Davis, K. (2011). Firefighting and fathering: Work-family conflict, parenting stress, and satisfaction with parenting and child behavior. Fathering: A Journal of Theory, Research, and Practice About Men as Fathers, 9(2), 169–188. https://doi.org/10.3149/fth.0902.169
- Siegrist, J., Starke, D., Chandola, T., Godin, I., Marmot, M., Niedhammer, I., & Peter, R. (2004). The measurement of effort–reward imbalance at work: European comparisons. Social Science & Medicine, 58(8), 1483–1499. https://doi.org/10.1016/S0277-9536(03)00351-4
- Sinden, K., MacDermid, J., Buckman, S., Davis, B., Matthews, T., & Viola, C. (2013). A qualitative study on the experiences of female firefighters. Work, 45(1), 97–105. https://doi.org/10.3233/WOR-121549
- Singer, B. H., Ryff, C. D., & Allostasis, S. T. (2004). Homeostasis, and the costs of physiological adaptation. In: Operationalizing allostatic load In J schulkin (pp. 113–149). Cambridge University Press.
- Slavich, G. M. (2016). Life stress and health. Teaching of Psychology, 43(4), 346–355. https://doi.org/10.1177/0098628316662768
- Spielberger, C., & Reheiser, E. (1994). The job stress survey: Measuring gender differences in occupational stress. Journal of Social Behavior and Personality, 9(2), 199–218.
- Sterling, P., & Eyer, J. (1988). Allostasis: A new paradigm to explain arousal pathology. Handb Life Stress Cogn Heal [Internet], September, 629–649. http://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=846297
- Sun, J., Wang, S., Zhang, J. Q., & Li, W. (2007). Assessing the cumulative effects of stress: The association between job stress and allostatic load in a large sample of Chinese employees. Work & Stress, 21(4), 333–347. https://doi.org/10.1080/02678370701742748
- Suvarna, B., Suvarna, A., Sarnyai, Z., Phillips, R., Juster, R., & Mcdermott, B. (2020). Health risk behaviours and allostatic load: A systematic review. Neuroscience & Biobehavioral Reviews, 108(October 2019), 694–711. https://doi.org/10.1016/j.neubiorev.2019.12.020.
- Teixeira, T., Santos, B. J., Bustos, J., & Guedes, J. (2022). Cortisol as a biomarker of work-related stress in firefighters: A systematic review. Occupational Environmental Safest Health III, 406(Nov 13), 234–247.
- Theall, K. P., Drury, S. S., & Shirtcliff, E. A. (2012). Cumulative neighborhood risk of psychosocial stress and allostatic load in adolescents. American Journal of Epidemiology, 176(SUPPL. 7), S164–S174.
- Tobin, C. S. T., Erving, C. L., & Barve, A. (2021). Race and SES differences in psychosocial resources: Implications for social stress theory. Social Psychology Quarterly, 84(1), 1–25. https://doi.org/10.1177/0190272520961379
- Upchurch, D. M., Rainisch, B. W., & Chyu, L. (2015). Greater leisure time physical activity is associated with lower allostatic load in white, black, and Mexican American midlife women: Findings from the national health and nutrition examination survey, 1999 through 2004. Women's Health Issues, 25(6), 680–687. https://doi.org/10.1016/j.whi.2015.07.002.
- Upchurch, D. M., Stein, J., Greendale, G. A., Chyu, L., Tseng, C.-H., Huang, M.-H., Lewis, T. T., Kravitz, H. M., & Seeman, T. (2015). A longitudinal investigation of race, socioeconomic status, and psychosocial mediators of allostatic load in midlife women. Psychosomatic Medicine, 77(4), 402–412. https://doi.org/10.1097/PSY.0000000000000175
- van Draanen, J., Prelip, M., & Upchurch, D. M. (2018). Consumption of fast food, sugar-sweetened beverages, artificially-sweetened beverages and allostatic load among young adults. Preventive Medicine Reports, 10(October 2017), 212–217. https://doi.org/10.1016/j.pmedr.2017.11.004.
- Wiley, J. F., Bei, B., Clinical, D., Bower, J. E., & Stanton, A. L. (2017). Relationship of psychosocial resources With allostatic load: A systematic review. Psychosomatic Medicine, 79(April), 283–292. https://doi.org/10.1097/PSY.0000000000000395
- Yang, J., Farioli, A., Korre, M., & Kales, S. N. (2014). Modified Mediterranean diet score and cardiovascular risk in a North American working population. PLoS One, 9(2), e87539.
- Yang, Y., & Kozloski, M. (2011). Sex differences in Age trajectories of physiological dysregulation: Inflammation, metabolic syndrome, and allostatic load. The Journals of Gerontology: Series A, 66A(5), 493–500. https://doi.org/10.1093/gerona/glr003
- Yoder, J., & Aniakudo, P. (1997). “Outsider within” the firehouse. Subordination and difference in the social interactions of African American women firefighters. Gender & Society, 11(3), 324–341. https://doi.org/10.1177/089124397011003004
- Yook, Y. S. (2019). Firefighters’ occupational stress and its correlations with cardiorespiratory fitness, arterial stiffness, heart rate variability, and sleep quality. PLoS One, 14(12), 1–9.
- ZIPPIA. (2022). Fireman demographics and statistics in the US [Internet]. ZIPPIA. The career expert. https://www.zippia.com/fireman-jobs/demographics/
