ABSTRACT
Background: The impact of cancer extends beyond treatment and evaluating the adverse psychological effects in survivors is important. We examined: (1) the relationship between diagnosis, relapse, and subjective well-being using a short and a holistic measure of well-being, including comparisons between our sample and established norms; (2) if reported physical symptoms were related to components of subjective well-being; and (3) if increased psychological flexibility predicted overall subjective well-being.
Methods: In total, 316 survivors completed online questionnaires to assess cancer, physical health (Edmonton Symptom Assessment Scale-R; ESAS-R), subjective well-being (Comprehensive Inventory of Thriving; CIT; Satisfaction with Life Scale; SWLS) and psychological flexibility (Comprehensive Assessment of Acceptance and Commitment Therapy).
Results: Relative to ESAS-R cut-points (Oldenmenger et al., 2013), participants reported only moderate levels of tiredness and slightly elevated drowsiness, depression, and anxiety; participants reported more problems with psychological health. SWLS scores were lower than published norms (M = 18.23, SD = 8.23) and a relapse was associated with the lowest SWLS scores (M = 16.95, SD = 7.72). There were differences in thriving between participants and age-matched norms (Su et al., 2014). Participants reported lower community involvement, respect, engagement with activities, skill mastery, sense of accomplishment, self-worth, self-efficacy, autonomy, purpose, optimism, subjective well-being, and positive emotions coupled with higher loneliness and negative emotions. In regression analysis, two components of psychological flexibility, Openness to Experience, t = 2.50, p < 0.13, β = −0.18, and Valued Action, t = 7.08, p < 0.001, β = −0.47, predicted 28.8% of the variability in total CIT scores, beyond the effects of demographic and disease characteristics and reported physical symptoms.
Conclusion: Cancer is an isolating experience, with the adverse psychological effects that impact subjective well-being continuing after the cessation of physical symptoms. Specific components of psychological flexibility may explain some variability in thriving beyond disease characteristics and may inform psychological intervention after diagnosis.
Each year approximately 1 in 6 deaths result from cancer, making cancer the second leading cause of death worldwide (WHO, Citation2021). According to the Canadian Cancer Society (Citation2019), almost 50% of Canadians will receive a cancer diagnosis in their lifetime. New medical interventions decreased cancer-related deaths for both males and females, with 63% of people expected to survive more than five years (Brenner et al., Citation2020). The ‘cancer experience’ extends beyond diagnosis, treatment, and end of life care. Because an increasing number of patients become cancer survivors, researchers should focus on the complex interplay of physical and psychological factors that impact the long-term effect of a cancer diagnosis on overall physical and psychological health.
Psychological health in individuals with a previous cancer diagnosis is defined by having distress or lack of distress, coupled with levels of ‘positive well-being and psychological growth’ (Andrykowski et al., Citation2008). This definition extends the importance of psychological health beyond a specific mental health diagnosis. Psychological health in cancer survivors is relevant not only during treatment and immediately following diagnosis but also in the years after treatment. Psychological health of survivors may include anxiety and feelings of hopelessness related to fear of relapse, which can lead to lower psychological health and more serious mental health challenges (Andrykowski et al., Citation2008). When cancer and mental health problems, such as depression and anxiety, co-occur, mortality rates are increased and reported quality of life decreases (Pinquart & Duberstein, Citation2010; Yi & Syrjala, Citation2017).
Psychological and physical well-being
An individual’s sense of well-being involves assessing physical and psychological factors (Diener et al., Citation1985). Many medical symptoms, such as depression and pain, are affected by both physical (i.e. serotonin levels, injury) and psychological (i.e. lowered social interactions, personality) variables. In general, health-related quality of life is an objective measure that includes an assessment of overall physical and emotional functioning, social engagement, emotional well-being, energy levels, fatigue, pain, and general health perceptions (Hays & Morales, Citation2001). Quality of life questionnaires ask patients to rate symptoms and include questions such as, During the past week, have you had trouble sleeping? or Did you feel tense? These questionnaires are modified for specific diseases; for example, a cancer quality of life scale includes cancer-specific questions (i.e. You worried your family members were at risk of getting cancer) in addition to questions focused on specific symptoms. In general, quality of life focuses on physical symptoms or limitations in activities of daily life.
Subjective well-being encompasses cognitive (assessment of life circumstances) and emotional (assessment of positive/negative emotions) factors (Tay et al., Citation2015) that is related to psychological health. Subjective well-being involves the interplay of many factors, including the perception of happiness, social connectivity, and employment satisfaction. Health-related quality of life encompasses overall physical (energy, fatigue, pain, etc.) and psychological functioning (social, emotional well-being), as well as general health perceptions (Hays & Morales, Citation2001). Measures of subjective well-being focus on the overall perception of one’s life, with specific measures focused on the subjective experience of ‘happiness’. Inventories measuring subjective well-being inventory might include items such as, Overall, I am happy with my life, or I feel good most of the time and generally focus on the overall assessment of specific areas of one’s life (including Personal Autonomy, Mastery of Skills, Social Connectivity, Positive and Negative Emotionality; see Su et al., Citation2014). In short, measures of subjective well-being ask how much respondents are bothered or impacted by aspects of their life and thus measure how they currently ‘feel’. An individual may have poor physical health and yet still report that they are happy with their life and adjust their expectations based on their limitations while still being satisfied overall.
Although there are moderate associations between quality of life and satisfaction with life (SWL), researchers consistently report that high health-related quality of life does not necessarily predict satisfaction with life. Health researchers often focus on specific mental health problems (i.e. anxiety, depression) to examine if psychological symptomatology is co-morbid with specific medical conditions and associated symptoms (limited mobility, pain, nausea). Examining these specific mental health problems may not give us the whole picture of an individual's overall psychological health (Andrykowski et al., Citation2008). In this study, we examined both reported physical symptoms which is an objective measure of HRQL and subjective well-being using a brief and a holistic measure to capture psychological health.
Although the cancer journey begins at diagnosis, it does not typically end after treatment, with psychological effects that can last for years after diagnosis. It is important to consider how outcome factors, such as SWL, change as time passes. For example, cancer patients often report moderate to moderately high loneliness levels, which increase with time since the initial diagnosis (Deckx et al., Citation2014). It is possible that it is not only passing time that influences SWL, but events and experiences that occur across different times. Lorenzo-Seva et al. (Citation2019) found that cancer survivors had slightly elevated SWL scores compared to healthy controls, with many participants endorsing the statement ‘life has given them a second chance’. Using a large sample of cancer survivors (N = 6,389) who completed questionnaires over three periods spanning 20 years, Ellis et al. (Citation2019) found lowered satisfaction with health and sex life, but satisfaction with all other domains remained the same or improved suggesting satisfaction with all aspects of life may not always decrease after a cancer diagnosis. Thus, we examined how specific aspects of subjective well-being, such as overall satisfaction, relationships, engagement, and autonomy, varied after a cancer diagnosis.
Can increased psychological flexibility improve psychological health?
A cancer diagnosis can cause severe psychological distress and, for some individuals, change how they perceive and cope with their life circumstances (Boykin et al., Citation2020). These negative changes impact overall psychological health during diagnosis, treatment, and recovery. Psychological flexibility (PF; Francis et al., Citation2016; Swash et al., Citation2017) is a modifiable factor defined by how people focus on present circumstances and prioritise thoughts, emotions, and behaviours aligned with personal values and goals. PF allows individuals to engage with their trauma and increase self-awareness to prevent their diagnosis from defining their sense of self (Boykin et al., Citation2020). Integrating aspects of PF into daily life may help an individual focus on the present and more effectively cope with trauma (Droutman et al., Citation2018).
According to Swash et al. (Citation2017), PF can be improved through Acceptance and Commitment Therapy (ACT), which increases resilience and focuses on teaching individuals how to prevent negative thoughts and feelings from becoming a central part of one’s personality. Considering this evidence-based method used to improve PF, it is important to understand how it relates to specific outcomes in this population and which components of PF are related to positive outcomes such as increased subjective well-being. Resiliency represents an individual's ability to adapt in a positive way to challenging experiences (Bonanno, Citation2004). PF and resiliency share commonalities in their focus on values-based actions despite obstacles, however, PF also includes components of cognitive diffusion, mindfulness, and identity. Unlike Cognitive Behavioural Therapy (CBT), the ACT process is not focused on eliminating or changing negative thoughts; instead, an individual may have persistent negative thoughts and yet be able to interact flexibly with both positive and negative inner experiences to live a life that is in line with their core values (Kashdan & Rottenberg, Citation2010). This value-based action is beneficial to individuals living with chronic conditions such as pain (Wicksell et al., Citation2008) and autoimmune disorders (Hebert & Best, Citation2021).
Research suggests that ACT can help cancer patients increase their overall PF, effectively lowering physical and psychological symptoms (Hulbert-Williams et al., Citation2015). Francis et al. (Citation2016) and Swash et al. (Citation2017) reported that increased psychological flexibility is associated with lower levels of psychological distress and higher quality of life. Given these positive effects, this practice can help cancer patients reduce psychological distress, including depression, anxiety, hopelessness, and suicidal ideation. A recent systematic review concluded that ACT can be a useful component in the future of cancer care by improving depression symptoms, anxiety, stress, fear, and improve overall quality of life (Li et al., Citation2021). Research supports its use both in late-stage ovarian cancer survivors (Rost et al., Citation2012) and in group settings for cancer survivors transitioning from the treatment phase to the post-treatment phase (Arch & Mitchell, Citation2016). An extensive meta-analysis published in early 2021 shows that ACT presented both in-person and through telephone-based delivery is efficacious at decreasing overall distress in individuals who have received a cancer diagnosis. In this meta-analysis, the number of treatment weeks ranged from 4–12, with longer iterations yielding more positive outcomes. Younger individuals were more likely to benefit from this type of intervention; however, the method it was delivered (in person, group, online) did not significantly impact the outcomes (Li et al., Citation2021). By fostering acceptance and creating more conscious, present, and flexible approaches to psychological experiences, ACT can help cancer survivors navigate their return to everyday life despite the fear of the unknown, anxieties, and depression symptoms. These short, flexible intervention styles are adaptable to challenges individuals may encounter after a cancer diagnosis, including fatigue and reduced mobility. Improving psychological flexibility may help individuals with a cancer diagnosis accept both positive and negative emotions without identifying them as ‘good’ or ‘bad’. Perhaps most importantly it can foster diffusion (e.g. move from ‘I am a cancer patient/diseased’ to ‘I am a person with a cancer diagnosis’) and focus on identifying their core values and learning to live their lives in line with those values despite obstacles.
Thus far, research has failed to include adequate analyses on which components of psychological flexibility are most salient to those who have received a cancer diagnosis. Considering diminished physical and mental resources a client may have after a cancer diagnosis it may be valuable for clinicians to narrow their focus in therapy that are most useful to this specific population. In many ways, ACT is a framework for approaching other forms of therapy, including CBT (Hayes et al., Citation2006) and understanding the relationships between the components of psychological flexibility and subjective well-being can help inform clinical judgment.
Purpose of the current study
The current study was part of a more extensive study designed to examine how cancer affects psychological health at diagnosis, during treatment, and during recovery and remission. In the current study, our objectives were to examine (1) how having a previous cancer diagnosis and relapse relates to subjective well-being, including how the current sample’s subjective well-being compares to established norms; (2) how reported physical symptoms are related to components of subjective well-being in this sample, and (3) the positive predictive qualities of psychological flexibility, the targeted outcome of ACT, on overall subjective well-being beyond reported physical symptoms, demographics, and diagnosis variables (time since diagnosis, relapse). Additionally, we were interested in examining how time since diagnosis relates to psychological health; specifically, we were interested in determining whether reported physical and psychological health was different depending on the time that reportedly passed since diagnosis.
Method
Recruitment
Participants were recruited from ‘private/closed’ Facebook support groups. These support groups are open to individuals who have received a cancer diagnosis in the past or are supporting someone who has received a cancer diagnosis. These groups often have administrators who also have a history of cancer diagnosis. Advertisements were posted in various Facebook groups and participants were offered a chance to win an Amazon gift card for their participation. Participants who were over the age of 18 and reported having a previous cancer diagnosis were invited to take part in the survey. Survey responses were collected using Qualtrics, which is a secure online survey tool. This pool of participants is representative of a group of individuals who have received a cancer diagnosis in the past, are a part of these online support communities, and have the capacity to complete the survey independently.
Materials
Given the long-term physical effects of cancer and its treatment, the completed questionnaire package included measures to assess physical symptoms with the Edmonton Symptom Assessment Scale (ESAS; Chang et al., Citation2000), satisfaction with life with the Satisfaction with Life Scale (SWLS; Diener et al., Citation1985) and thriving with the Comprehensive Inventory of Thriving (CIT; Su et al., Citation2014), which both measure subjective well-being, and PF measured using the Comprehensive Assessment of Acceptance and Commitment Therapy Processes (CompACT; Francis et al., Citation2016). Using these measures, we will focus on overall psychological (Diener et al., Citation1985; Su et al., Citation2014) and physical well-being (Aaronson et al., Citation1993; Chang et al., Citation2000) in individuals who have had a cancer diagnosis.
Edmonton Symptom Assessment Scale (ESAS-R; Chang et al., Citation2000)
This scale is a 9-item questionnaire that uses a 12-point rating scale. This questionnaire has nine symptoms (pain, activity, nausea, depression, anxiety, drowsiness, lack of appetite, well-being, and shortness of breath) that the individual rates on a scale from 0 (none) to 11 (worst possible). This scale has been widely used in over 20 languages in the last 25 years and has sound psychometric properties. Specifically, the ESAS-R has high internal validity (Cronbach Alpha, .79), test-retest validity (r = .85 from day 2–7) and shows convergent validity with pain scales (Hui & Bruera, Citation2017). The sum of the nine scores becomes the individual's ESAS-R distress score, and a higher score indicates multiple symptoms. The ESAS-R has an overall Cronbach alpha of .79 and test-retest coefficients ranging from .86 to .97 (Chang et al., Citation2000). In the current study, we used only the physical symptom subscale scores. The reliability of this measure was high when the overall distress score that includes all items was used, Cronbach’s alpha = .87.
Satisfaction with Life Scale (SWLS; Diener et al., Citation1985)
The SWLS is a five-item questionnaire that uses questions such as ‘I am satisfied with my life,’ which are scaled on a 7-point Likert-type scale ranging from strongly disagree to strongly agree. The SWLS has a possible range of 5–35, with higher scores indicating higher satisfaction. The Cronbach alpha was found to be .87, while the test-retest coefficient was .82 (Diener et al., Citation1985). In the current study, the reliability of this measure was high, Cronbach’s alpha = .91. According to Diener, scores greater than 25 indicate high satisfaction in all areas of life. Scores between 20 and 24 show a general satisfaction with life, with some domains that are perceived as needing improvement. Individuals who score less than 20 are dissatisfied with at least one area of their life; individuals with chronic illness typically report lower than average life satisfaction. Including the SWLS in this study allowed us to compare our sample to published norms on the total score which is not available with the Comprehensive Inventory of Thriving scale, an instrument that provides more breadth to our assessment of well-being.
Comprehensive Inventory of Thriving (CIT; Su et al., Citation2014)
The CIT is a 54-item questionnaire with a 5-point Likert scale ranging from strongly disagree to strongly agree. This measure has 18 subscales, used to measure the broad concept of well-being and thriving. Each of the 18 subscales assesses an aspect of positive functioning, characterised by seven dimensions of psychological health (i.e. supportive and enriching relationships, interest in daily activities, feelings of meaning and purpose in life, a sense of accomplishment, subjective well-being, feelings of control and autonomy, and optimism). The CIT has been reported as having internally consistent scores, with alpha coefficients ranging from .71 to .96, and this measure was also reported as having good test-retest reliability (r = .57 to r = .83) over the span of four months. The CIT has demonstrated good convergent validity with other measures of psychological well-being (Flourishing Scale, Satisfaction with Life, Life Orientation Test, Core Self-Evaluation Scales). This holistic view of well-being not only predicts positive functioning and health outcomes beyond other measures of well-being, but also shows higher incremental validity when predicting objective and self-reported health outcomes. In the current study the reliability of all subscales ranged from .70–.91.
Acceptance and Commitment Therapy Processes (CompACT; Francis et al., Citation2016)
The CompACT uses a 23-item questionnaire that measures an individual’s ability to be psychologically flexible using a 7-point scale from 1 (strongly disagree) to 7 (strongly agree). The CompACT includes three interrelated but distinguishable subscales that contain both negative and positively framed statements; Openness to Experience (e.g. Thoughts are just thoughts- they don’t control what I do.); Behavioural Awareness (e.g. I rush through meaningful activities without being really attentive to them.); and, Valued Action (e.g. I can identify the things that really matter to me in life and pursue them.) that are measured on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree).
The Cronbach alpha for this measure was found to be .91, showing good reliability and high concurrent and convergent validity. In the current study, the reliability of only two of the three subscales of the CompACT were high: Behavioural Awareness Cronbach’s alpha = .84 and Openness to Experience Cronbach’s alpha = .88. The Cronbach’s alpha for Valued Action was acceptable at .57.
Procedure
The University of New Brunswick Research Ethics Board (REB 013-2019) reviewed and approved this project. All data were collected using Qualtrics, which allows for the secure collection of online questionnaire data. Data was collected between April 2019 and March 2020; data collection ended prior to the start of the COVID-19 pandemic. After reading preliminary information and signing an informed consent form, participants completed the questionnaire package. Demographic and disease specific questions were always presented first. The other questionnaires were presented in randomised order. All measures were provided in English. After completing the questionnaire package, participants had the opportunity to sign up to be included in a random draw for a gift card.
Data analysis strategy
Prior to conducting data analysis, the data were examined to identify outliers and missing values. Participants who did not complete more than 20% of items on any given measure were excluded and their scale scores were not included in relevant analyses. Participants were retained for analyses of the measures for which they completed at least 80% of the items. Participants who did not complete the demographics questionnaires were excluded. Prior to data collection, a power analysis was conducted using G-Power to determine adequate sample size. Given the current sample size (N = 316) and a medium effect size (f2 = .15) the achieved power was .99. We tested the assumptions underlying all statistical tests (i.e. normality, linearity). To examine how a cancer diagnosis impacts physical and psychological health (Research Objective 1 and 2), descriptive statistics for the overall sample were calculated and t-tests were used to compare the sample scores to published norms. Comparing our results with the published norms gives us a numerical representation of how our sample of individuals with a cancer diagnosis compare to samples drawn from the general population. Pearson Product Moment Correlation Coefficients were used to assess the association between time since diagnosis and variables associated with psychological health. To explore the unique predictive relationship that psychological flexibility and severity of reported physical symptoms has on overall Thriving (subjective well-being) beyond demographics (sex, age) and disease characteristics (time since diagnosis, relapse), a hierarchical linear regression predicting Thriving was conducted (Research Objective 3).
Results
Participants
In total, 316 participants completed the questionnaire package (67% female). In this sample, the females were slightly younger than the males, Mfemale = 52.49, SD = 13.26 vs. Mmale = 56.02, SD = 12.47. Individuals reported that, on average, it had been 6.55 years since diagnosis (SD = 8.01), and the average age at diagnosis was 46.32 years. A summary of the reported cancer types, relapse, and prognosis is provided in . In total, 83 participants (23.7%) reported a relapse, with almost 80% of relapses occurring within two years of treatment. Most participants reported cancer treatments; 233 had surgery, 176 had radiation therapy, 220 had chemotherapy, 32 had hormone therapy, 43 reported treatments with another form of anti-cancer drugs, 20 were treated through naturopathic or homeopathic methods, and 23 used cannabis-related treatments. Participants were able to select multiple treatment types. In this study we were interested in subjective well-being and quality of life after cancer. In this sample, these variables were similar, regardless of cancer stage at diagnosis and prognosis. A relapse was associated with lower wellness and thus, where appropriate, relapse was considered in statistical tests. Most participants were in a long-term relationship (65% were married), 10.3% were divorced, and 10% were single. Although participants from many countries completed the questionnaire package, most participants lived in the United States (n = 189; 54%) or Canada (n = 60; 17.1%).
Table 1. Summary of cancer types reported by participants (N = 350).
Research question 1: psychological health in cancer patients
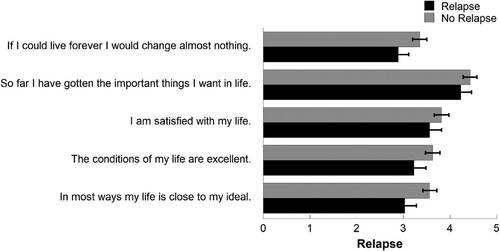
To assess our first objective, the average SWLS scores of individuals with a cancer diagnosis were compared to published norms (see Diener, Citation2006). In this sample, the average SWLS was 18.23, indicating slight dissatisfaction with life. Specifically, 55.6% had scores less than 20, 16.2% were between 20 and 24, and 28.2% reported SWLS scores above 25. Further, shows the average SWLS scores for each item by relapse. Although scores for individuals who have relapsed were lower on each question, the overlap of the confidence intervals indicate that the differences in scores did not represent statistically significant differences (see ). This was important to investigate if there was a significant difference between these subgroups in this population because there was concern that a relapse would impact overall SWLS scores. Interestingly, the correlation between SWLS and years since diagnosis was not statistically significant (r = −.01), indicating that, for this sample, life satisfaction did change as the reported time since diagnosis increased. Although the lowest SWLS were reported by respondents who reported a relapse (M = 16.95, SD = 7.72), these scores were not statistically lower than individuals with a single diagnosis.
Figure 1. Mean scores (standard error) on Satisfaction with Life Scale items as a function of cancer relapse.
The CIT provides a multifaceted measurement of positive functioning and recognises that individuals who thrive do well in different areas of life. presents the mean subscale scores for the current sample (overall and by time since diagnosis) and includes the published norms for individuals between 40 and 59 years (Su et al., Citation2014; http://labs.psychology.illinois.edu/~ediener/CIT_BIT.html). Overall, participants with a cancer diagnosis had lower scores on most CIT subscales. shows the subscales with significant differences from the norms with effect sizes noted. All effect sizes were small or very small except for engagement (Cohen’s d = .58) and Negative Feelings (Cohen’s d = .97). Further, a correlational analysis indicated that time since diagnosis was not associated with most thriving subscales. Although CIT-Engagement scores were higher in the years reported after diagnosis, r = .15, p = .04, CIT-Respect decreased, r = −.18, p = .01. The lower perceived respect of individuals who had survived more than five years post diagnosis suggests that the effects of a cancer diagnosis are cumulative and extend beyond the period of initial diagnosis and treatment. In addition, a series of t-tests were conducted to examine if a cancer relapse was associated with lower thriving scores. Except for individuals who had a relapse, who reported significantly higher average support, t(218) = 2.41, p = .02, thriving subscale scores were not related to the cancer relapse variable.
Table 2. Mean scores (standard deviation) on the comprehensive inventory of thriving subscales. T-tests were done to examine differences between the overall sample means and CIT norms (Su et al., Citation2014).
Physical well-being in individuals diagnosed with cancer
To address our second objective, we used the Edmonton Symptom Assessment Scale (ESAS-R) to assess physical and psychological symptoms. Scores on ESAS-R range from 0 (no suffering) to 10 (worst possible suffering) and are commonly used to describe how specific symptoms affect daily life. Correlations between the ESAS-R subscales and CIT: Thriving and CompACT subscales are reported in . Overall, as expected, there were statistically significant inverse correlations between CIT subscale scores and all aspects of ESAS-R physical and psychological health. Further, greater CompACT scores were associated with less severe physical and psychological symptoms. These correlations were moderate to large and were all significant at the p < . 01 level.
Table 3. Correlations between the Edmonton Symptom Assessment Scale (ESAS-R) subscales and variables of interest.
presents the published cut-off points indicating symptom severity and the potential need for follow-up care (Oldenmenger et al., Citation2013) and the means of our participants for each ESAS-R item. Overall, current participants reported mild to moderate ESAS-R symptoms. Interestingly, individuals who reported a cancer relapse did not report more problems on any of the ESAS-R symptoms and had a total distress score that was not significantly higher than individuals who did not report a relapse (M = 3.32 vs. 3.39, F = .033, p = .86). Further, correlational analyses indicated no statistically significant associations with any ESAS-R scores and time since diagnosis, indicating that ESAS-R scores were stable over time.
Table 4. Mean (standard deviation) scores on the ESAS-R of the current sample as a function of time since diagnosis. Oldenmenger et al. (Citation2013) cut-off points are included for comparison purposes.
The influence of psychological flexibility
A hierarchical linear regression was conducted to examine how psychological flexibility was related to subjective well-being beyond the effects of physical health. For this analysis, the total score on the CIT was calculated and used as the criterion variable. Biological sex, age, years since diagnosis, and relapse (yes, no) were entered in Block 1. The ESAS-R subscale scores related to physical health (pain, tiredness, drowsiness, nausea, lack of appetite, shortness of breath) were entered in Block 2, and CompACT subscales were entered in Block 3. The overall model was statistically significant, F(13, 173) = 20.88, p < .001, and accounted for 62.2% of the variability in Thriving (see ). Block 1 was not statistically significant (p = .95), indicating that neither basic demographic nor cancer-related variables accounted for significant variance. Block two variables contributed significantly to the model (R2 change = 33.2%), with Tiredness (lack of energy) emerging as a significant predictor, t = −3.78, p < 0.001, β = −0.38 . In Block 3, an additional 28.6% of the variability was accounted for, with Openness to Experience, t = 2.50, p = .03, β = −.18, and Valued Action, t = 7.08, p < .001, β = −.47, contributing to the model.
Table 5. Summary of the hierarchical regression analysis for predicting thriving (N = 173).
Discussion
Overall, current results suggest that the psychological effects of a cancer diagnosis extend beyond the period of initial treatment. We found that survivors’ average satisfaction with life and psychological thriving was somewhat lower than published norms with the largest differences seen in the Engagement and Negative Feelings subscales of the Comprehensive Inventory of Thriving (see Diener, Citation2006; Diener et al., Citation1985; Su et al., Citation2014). The Comprehensive Inventory of Thriving includes subscales to provide a more detailed assessment of different aspects of psychological health, including relationship satisfaction, skill mastery, autonomy, and emotionality. Compared to age norms published by Su et al. (Citation2014), survivors reported lower community support, respect, social engagement, higher loneliness, and more negative emotions. Likely due to their lower community support and tendency to not engage in social activities, survivors reported less skill mastery and had a lower sense of accomplishment, self-efficacy, and self-worth than individuals who have not faced a cancer diagnosis. Overall, the participants who reported having a previous cancer diagnosis reported lower subjective well-being compared to norms. This result was not surprising. This study aimed to further examine variability within this sample; a cancer diagnosis is not a modifiable factor, however psychological factors such as psychological flexibility may be modifiable and were associated with increased well-being.
As would be expected, individuals who reported a relapse had similar (and lower) psychological health than survivors who had a single diagnosis. Further, analyses indicated that overall reported psychological health did not change based on the reported years since diagnosis, suggesting that the psychological consequences of a cancer diagnosis are often present at all stages, even after the cessation of treatment. These results extend the findings of Schumacher et al. (Citation2013) who reported long-lasting psychological distress, specifically anxiety, in survivors. Although Schmacher et al. did not find lower subjective well-being in the years after treatment, the differences could be due to the composition of the sample; 42% of Schumacher et al.’s participants were within four years of diagnosis, compared with approximately 64% of the current sample. Thus, it is possible that with a broader time frame results would differ. Overall, the current results suggest that, relative to normative samples, psychological health is lower in cancer survivors at all points after diagnosis.
In the current study, participant’s ESAS-R scores (Chang et al., Citation2000) were indicative of mild to moderate physical symptoms (Oldenmenger et al., Citation2013). Symptom severity did not vary based on the reported time since initial diagnosis. Further, and contrary to expectations, a disease relapse was not associated with increased reported symptom severity. As expected, we found moderate correlations between physical symptoms and psychological health. Our results replicated Avis et al. (Citation2005) who reported that, in the years after treatment, regardless of physical health improvements, levels of psychological distress do not necessarily improve (Avis et al., Citation2005). Even though survivors reported only mild to moderate medical symptoms (see ; Oldenmenger et al., Citation2013), they reported lower subjective well-being (satisfaction with life, psychological thriving) than normative samples (Diener et al., Citation1985; Su et al., Citation2014). These findings support large-scale studies that highlight direct and indirect links between physical and psychological wellness (see Ohrnberger et al., Citation2017). Ohrnberger and colleagues used a mediation model and reported that the relations between psychological and physical health are mediated by lifestyle factors, including increased physical activity and social connections.
The benefits of psychological flexibility
We focused on how the components of psychological flexibility are related to overall psychological thriving in the years that follow a cancer diagnosis. Current results indicate moderate correlations between psychological flexibility and physical and psychological symptoms, which replicate the meta-analysis conducted by Hayes et al. (Citation2006) suggested that the change process that occurs through ACT by increasing psychological flexibility is related to positive physical and psychological outcomes. In addition to higher psychological distress, cancer survivors report a variety of concerns, including fear of recurrence (van de Wal et al., Citation2016), worries about the health of family members (Avis et al., Citation2005), and side effects of treatment (i.e. urinary and bowel incontinence; Chambers et al., Citation2017). The way individuals approach their lives and engage with their environments dramatically impacts their overall well-being despite the effects of inevitable variables, such as the passing of time, cancer relapse, or severity of physical ailments related to health. ACT aims to increase psychological flexibility through targeting three specific areas: Openness to Experience; Valued Action; and Behavioural Awareness (Soo et al., Citation2011).
In the regression model predicting overall thriving, we found that demographic variables (age, sex) and disease related variables (time since diagnosis, relapse) did not contribute significantly to the model. Further, after controlling for disease and demographic variables, the only physical variable contributing to the model was ESAS-R: Tiredness (lack of energy), which suggests a significant physical barrier for individuals. Tiredness is a symptom of many medical illnesses and psychological ailments. It can often be challenging to tease apart which tiredness (lack of energy) results from physical conditions and which components are related to psychological distress. Despite the contribution of tiredness, it is important to note that drowsiness/sleepiness was not a significant contributor to this model. Patient perspectives on the ESAS-R have indicated that there are physical and psychological components to both descriptors, leading to some confusion about how to differentiate these two symptoms (Watanabe et al., Citation2009).
In this study, Openness to Experience and Valued Action significantly predicted overall thriving beyond demographic, cancer, and physical symptom variables. Openness to Experience is defined by one’s ability to accept all positive and negative thoughts without attaching a positive or negative label to them. ACT therapy programmes focuses on this ability and teaches individuals to discriminate between constructive and non-constructive thoughts. Skills such as these encourage individuals to change their focus from using maladaptive problem-solving coping strategies to descriptive-engaged styles of coping (Soo et al., Citation2011). Cognitive defusion is defined by the ability to be aware of thoughts while not trying to change them. Cognitive defusion involves the acceptance of both positive and negative emotions and in this state, individuals do not focus on the modification or labelling of any thought process. The development of cognitive defusion skills has the potential to help survivors manage fears of relapse, sickness, and death. This non-judgemental process could help break the common cycle of rumination. When thoughts are allowed to occur without conscious effort to change the ‘bad’ thought, the negative impact on well-being is diminished. Our results indicate that, when demographic and physical symptom variables were controlled, Openness to Experience predicted approximately four percent of the overall variability in psychological thriving, providing potential clinical utility of this concept.
Moving forward with life activities that bring meaning and value to one’s life is highly related to thriving. This model is even more significant in the relationship between Valued Action, which accounted for almost 24% of the variability in psychological thriving. This component of Psychological Flexibility measures the degree to which an individual can identify their core values and can live life in line with those values, even when obstacles are present. ACT guides an individual through identifying their values and helps them objectively evaluate how their actions align with those values in all quadrants of their life. This component of Psychological Flexibility is also an important part of resiliency. Bonanno (Citation2004) describes a resilient individual as one who may not show a reduction in symptoms or negative life experiences but that they are showing signs of thriving or ‘doing well’. This study highlights the importance of these skills in a population that has been faced with mortality and physical difficulties.
Behavioural Awareness, which was not a significant predictor in current models, is a component of psychological flexibility that embodies present moment mindfulness. Current results suggest that in this population, openness to all internal experiences is a more salient predictor of thriving than being present in the moment and not rushing through meaningful activities. Although an essential component of mindfulness, it is possible that focusing on the present moment is not enough to improve psychological outcomes after a cancer diagnosis. After a cancer diagnosis, there are many periods where anxiety and the potential for bad news are inevitable; individuals who can experience these negative thoughts and emotions without judgement and do not work to suppress them may report better psychological outcomes both immediately after a cancer diagnosis and as the years pass in their remission. Previous research has indicated that ACT therapy models that incorporate all three aspects of psychological flexibility improve well-being; this research highlights the aspects of psychological flexibility that may be most important to target when working with individuals who have received a cancer diagnosis.
Clinical utility of results
The results of the current study highlight the ACT processes, specifically openness to experience and valued action, are significantly related to subjective well-being after cancer. Individuals enter therapy with different levels of PF; some individuals may have high levels of PF without exposure to formal ACT-based approaches. Individuals may find some of the pillars of flexibility more challenging to foster than others. Further, it is possible that someone may be inflexible, but because they never faced difficult life circumstances that require a higher level of flexibility, they may not have experienced a subjective level of distress linked to this inflexibility.
ACT is a psychological intervention and daily functioning approach that can be considered a transdiagnostic intervention to promote overall positive personal growth (Luoma, Hayes, & Walser, Citation2007). Each ACT process is targeted in therapy differently. For example, values are defined using a visual representation of a bullseye that allows clients map their alignment with their values in four areas of life (relationships, leisure, health/personal growth, and work/school). In this process, individuals also have a chance to identify a barrier to living their life in a way that is fully aligned with their personal values. When helping individuals defuse their inner experiences, ACT draws upon the use of metaphors that help them visualise and defuse their thoughts, so they can see them just as thoughts without needing to hold them true.
Although ACT provides skills, techniques, and metaphors, there is not a specific set of tangible skills to attain, but rather, ACT is a way of approaching life in a psychologically flexible way. This research suggests that for cancer survivors, being open to positive and negative experiences and engaging in behaviours that move them toward a values-based life are valuable additions to creating an individualised therapeutic approach.
Limitations and directions for future research
Although this research reveals some meaningful relationships between physical and psychological outcomes after a cancer diagnosis, it is important to note limitations. This sample was a non-probability, convenience sample. As is typical of questionnaire research, there was an unequal balance of males and females, affecting the generalizability of results. This sample was not gender balanced which limited our ability to conduct gender-based analyses. Although gender was controlled for, when possible, this is a limitation of the study because controlling for gender does not allow us to examine if differences exist based on sex or gender. Future research could explore how the sex and gender of survivors affect variables, such as psychological flexibility and social connectedness, that are associated with overall psychological health. Highlighting resources that focus on concerns specific to males or females could inform the development of programmes or therapeutic interventions that take differences such as these into account.
We collected from an online sample of individuals who self-reported a previous cancer diagnosis and were a part of a cancer support group. General distress may be higher among these individuals, explaining mild physical symptoms and lower psychological health. Further, the self-report design of this study does not allow for objective classification of patients based on the stage of cancer or actual prognosis; however, we would argue that subjective levels of physical distress are also a valid measurement of an individual’s perceived distress. We would suggest that future researchers recruit survivors from sites that focus on specific interests rather than survivor support. A broader sample would allow the generalisation of the current results to the wider population of cancer survivors. In future research, using a more controlled sample and using a longitudinal design would expand these findings.
Finally, in future studies, to reduce extraneous variables such as location, inclusion in a support group, treatment type, quality of medical care, and geographic location, researchers could recruit survivors from a single clinic (or region). The inclusion of qualitative methodologies would allow for a more nuanced examination of the concerns of survivors. Current participants likely had varied medical care and healthcare providers; for example, participants in the United States of America have a vastly different healthcare system than patients in Canada. Thus, future research should focus on mixed methods analyses to explore differences associated with health care systems and psychological concerns. Given the mean 6.55 years since initial diagnosis, it is important to note that many confounding life variables could have occurred between diagnosis and questionnaire completion. In this study the sample is compared to population norms which does indicate lower psychological wellness than normative samples.
Future research should also examine the components of psychological flexibility in individuals with a previous cancer diagnosis more closely. Researchers could further investigate these relationships in large scale studies of individuals with a previous cancer diagnosis such as Ohrnberger et al. (Citation2017) who used mediation models to examine factors related to wellness in more depth in general populations. This study shows that the Openness to Experience and Valued Action components of psychological flexibility are related to higher levels of thriving. It would be interesting to investigate the impacts of Behavioural Awareness in this population to investigate if its inclusion has positive impacts on other outcomes, has a neutral impact, or if it is potentially detrimental to the therapeutic process.
Conclusions
In the past, health professionals and researchers have focused primarily on the impact of cancer on physical health. Given recent medical advances, novel treatments have been developed that improve long term survival. Thus, many survivors eventually return to everyday activities at some point after treatment. Traditionally, the goal of many patients and their medical team have focused on getting through treatment and return to ‘normal’ life. Research does show that ACT can help improve psychological health in individuals with chronic conditions (Wicksell et al., Citation2008) and is efficacious in cancer patients (González-Fernández & Fernández-Rodríguez, Citation2019). This research helps isolate the components of ACT that can be emphasised in treatment for individuals who had received a cancer diagnosis regardless of how long it has been since it was received. With this knowledge researchers can begin to examine which components of psychological flexibility should be a focus in therapy for this population. For example, considering that Valued Action is such a significant predictor of subjective well-being, a clinician may choose to start with identifying values helping their client balance their values circle by engaging in more behaviours that are in line with these values.
Although the psychological effects of diagnosis and treatment are not as immediately necessary, their importance increases in the months and years after diagnosis and treatment. This increased awareness of how psychological health impacts health highlights the importance of the current study. Our goal was to understand the complex relationship between physical and psychological health to, ultimately, provide information that will help clinicians and future researchers find ways to improve the life satisfaction of cancer patients and survivors.
Ethics statement
The Ethics statement is the Institutional review board statement/informed consent statement.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by an Institutional Review Board/Ethics committee. See details under Methods.
Informed consent
The project was reviewed by the University of New Brunswick Ethics Board (REB 013-2019) and confirms to the standards set for in the Canadian Tricouncil Policy on Research Ethics. All participants completed an informed consent form prior to data collection. The informed consent form explained that participation was voluntary and that participants could skip any questions that they did not want to answer and could terminate their participation that any time. Participants were informed that their data was both anonymous and confidential.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., Filiberti, A., Flechtner, H., Fleishman, S. B., de Haes, J. C. J. M., Kaasa, S., Klee, M., Osoba, D., Razavi, D., Rofe, P. B., Schraub, S., Sneeuw, K., Sullivan, M., & Takeda, F. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. JNCI: Journal of the National Cancer Institute, 85(5), 365–376. http://doi.org/10.1093/jnci/85.5.365
- Andrykowski, M. A., Lykins, E., & Floyd, A. (2008). Psychological health in cancer survivors. Seminars in Oncology Nursing, 24(3), 193–201. https://doi.org/10.1016/j.soncn.2008.05.007
- Arch, J. J., & Mitchell, J. L. (2016). An Acceptance and Commitment Therapy (ACT) group intervention for cancer survivors experiencing anxiety at re-entry: ACT intervention for anxious cancer survivors. Psycho-Oncology, 25(5), 610–615. https://doi.org/10.1002/pon.3890
- Avis, N. E., Smith, K. W., McGraw, S., Smith, R. G., Petronis, V. M., & Carver, C. S. (2005). Assessing Quality of Life in Adult Cancer Survivors (QLACS). Quality of Life Research, 14(4), 1007–1023. http://doi.org/10.1007/s11136-004-2147-2
- Bonanno, G. A. (2004). Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist, 59(1), 20. https://doi.org/10.1037/0003-066X.59.1.20
- Boykin, D. M., Anyanwu, J., Calvin, K., & Orcutt, H. K. (2020). The moderating effect of psychological flexibility on event centrality in determining trauma outcomes. Psychological Trauma: Theory, Research, Practice, and Policy, 12(2), 193–199. https://doi.org/10.1037/tra0000490
- Brenner, D. R., Weir, H. K., Demers, A. A., Ellison, L. F., Louzado, C., Shaw, A., Turner, D., Woods, R. R., & Smith, L. M. for the Canadian Cancer Statistics Advisory Committee (2020). Projected estimates of cancer in Canada in 2020. Canadian Medical Association Journal, 192(9), E199–E205. https://doi.org/10.1503/cmaj.191292
- Canadian Cancer Society. (2019). Cancer statistics at a glance. https://www.cancer.ca/en/cancerinformation/cancer-101/cancer-statistics-at-a-glance/?region=on.
- Chambers, S. K., Ng, S. K., Baade, P., Aitken, J. F., Hyde, M. K., Wittert, G., Frydenberg, M., & Dunn, J. (2017). Trajectories of quality of life, life satisfaction, and psychological adjustment after prostate cancer. Psycho-Oncology, 26(10), 1576–1585. https://doi.org/10.1002/pon.4342
- Chang, V. T., Hwang, S. S., & Feuerman, M. (2000). Validation of the Edmonton symptom assessment scale. Cancer: Interdisciplinary International Journal of the American Cancer Society, 88(9), 2164–2171. https://doi.org/10.1002/(SICI)1097-0142(20000501)88:9<2164:AID-CNCR24>3.0.CO;2-5
- Deckx, L., van den Akker, M., & Buntinx, F. (2014). Risk factors for loneliness in patients with cancer: A systematic literature review and meta-analysis. European Journal of Oncology Nursing, 18(5), 466–477. https://doi.org/10.1016/j.ejon.2014.05.002
- Diener, E. D. (2006). Understanding satisfaction with life scores. http://labs.psychology.illinois.edu/~ediener/SWLS.html
- Diener, E. D., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75. https://doi.org/10.1207/s15327752jpa4901_13
- Droutman, V., Golub, I., Oganesyan, A., & Read, S. (2018). Development and initial validation of the Adolescent and Adult Mindfulness Scale (AAMS). Personality and Individual Differences, 123, 34–43. https://doi.org/10.1016/j.paid.2017.10.037
- Ellis, E. M., Nelson, W. L., & Ferrer, R. A. (2019). Trajectories of current and predicted satisfaction with one’s life following a cancer diagnosis. Annals of Behavioral Medicine, 53(2), 158–168. https://doi.org/10.1093/abm/kay025
- Francis, A. W., Dawson, D. L., & Golijani-Moghaddam, N. (2016). The development and validation of the Comprehensive Assessment of Acceptance and Commitment Therapy processes (CompACT). Published in the Journal of Contextual Behavioral Science, https://doi.org/10.1016/j.jcbs.2016.05.003
- González-Fernández, S., & Fernández-Rodríguez, C. (2019). Acceptance and commitment therapy in cancer: Review of applications and findings. Behavioral Medicine, 45(3), 255–269. https://doi.org/10.1080/08964289.2018.1452713
- Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. https://doi.org/10.1016/j.brat.2005.06.006
- Hays, R. D., & Morales, L. S. (2001). The RAND-36 measure of health-related quality of life. Annals of Medicine, 33(5), 350–357. https://doi.org/10.3109/07853890109002089
- Hebert, K., & Best, L. A. (2021). Factors contributing to wellbeing: Comparing functional somatic symptom disorders and well-defined autoimmune disorders. In C. Pracana & M. Wang (Eds.), Psychological applications and trends (pp. 269–281). inScience Press.
- Hui, D., & Bruera, E. (2017). The Edmonton symptom assessment system 25 years later: Past, present, and future developments. Journal of Pain and Symptom Management, 53(3), 630–643. https://doi.org/10.1016/j.jpainsymman.2016.10.370
- Hulbert-Williams, N. J., Storey, L., & Wilson, K. G. (2015). Psychological interventions for patients with cancer: Psychological flexibility and the potential utility of Acceptance and Commitment Therapy. European Journal of Cancer Care, 24(1), 15–27. https://doi.org/10.1111/ecc.12223
- Kashdan, T. B., & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30(7), 865–878. doi:10.1016/j.cpr.2010.03.001
- Li, Z., Li, Y., Guo, L., Li, M., & Yang, K. (2021). Effectiveness of acceptance and commitment therapy for mental illness in cancer patients: A systematic review and meta-analysis of randomised controlled trials. International Journal of Clinical Practice, 75(6), e13982. https://doi.org/10.1111/ijcp.13982
- Lorenzo-Seva, U., Calderon, C., Ferrando, P. J., Mar Muñoz, M., Beato, C., Ghanem, I., Castelo, B., Carmona-Bayonas, A., Hernández, R., & Jiménez-Fonseca, P. (2019). Psychometric properties and factorial analysis of invariance of the Satisfaction With Life Scale (SWLS) in cancer patients. Quality of Life Research, 28(5), 1255–1264. https://doi.org/10.1007/s11136-019-02106-y
- Luoma, J. B., Hayes, S. C., & Walser, R. D. (2007). Learning ACT: An acceptance and commitment therapy skills-training manual for therapists. New Harbinger Publications.
- Ohrnberger, J., Fichera, E., & Sutton, M. (2017). The dynamics of physical and mental health in the older population. The Journal of the Economics of Ageing, 9, 52–62. https://doi.org/10.1016/j.socscimed.2017.11.008
- Oldenmenger, W. H., Pleun, J., de Klerk, C., & van der Rijt, C. C. (2013). Cut points on 0–10 numeric rating scales for symptoms included in the Edmonton Symptom Assessment Scale in cancer patients: A systematic review. Journal of Pain and Symptom Management, 45(6), 1083–1093. https://doi.org/10.1016/j.jpainsymman.2012.06.007
- Pinquart, M., & Duberstein, P. R. (2010). Depression and cancer mortality: A meta-analysis. Psychological Medicine, 40(11), 1797–1810. https://doi.org/10.1017/S0033291709992285
- Rost, A. D., Wilson, K., Buchanan, E., Hildebrandt, M. J., & Mutch, D. (2012). Improving psychological adjustment among late-stage ovarian cancer patients: Examining the role of avoidance in treatment. Cognitive and Behavioral Practice, 19(4), 508–517. https://doi.org/10.1016/j.cbpra.2012.01.003
- Schumacher, J. R., Palta, M., LoConte, N. K., Trentham-Dietz, A., Witt, W. P., Heidrich, S. M., & Smith, M. A. (2013). Characterizing the psychological distress response before and after a cancer diagnosis. Journal of Behavioral Medicine, 36(6), 591–600. https://doi.org/10.1007/s10865-012-9453-x
- Soo, C., Tate, R. L., & Lane-Brown, A. (2011). A systematic review of Acceptance and Commitment Therapy (ACT) for managing anxiety: Applicability for people with acquired brain injury? Brain Impairment, 12(1), 54–70. https://doi.org/10.1375/brim.12.1.54
- Su, R., Tay, L., & Diener, E. (2014). The development and validation of Comprehensive Inventory of Thriving (CIT) and Brief Inventory of Thriving (BIT). Applied Psychology: Health and Well-Being, 6(3), 251–279. https://doi.org/10.1111/aphw.12027
- Sullivan, G. M., & Feinn, R. (2012). Using effect size-or why the P value is not enough. Journal of Graduate Medical Education, 4(3), 279–282. https://doi.org/10.4300/JGME-D-12-00156.1
- Swash, B., Bramwell, R., & Hulbert-Williams, N. J. (2017). Unmet psychosocial supportive care needs and psychological distress in haematological cancer survivors: The moderating role of psychological flexibility. Journal of Contextual Behavioral Science, 6(2), 187–194. https://doi.org/10.1016/j.jcbs.2017.02.005
- Tay, L., Kuykendall, L., & Diener, E. (2015). Satisfaction and happiness–the bright side of quality of life. In W. Glatzer (Ed.), Global handbook of quality of life (pp. 839–853). Springer.
- van de Wal, M., van Oort, I., Schouten, J., Thewes, B., Gielissen, M., & Prins, J. (2016). Fear of cancer recurrence in prostate cancer survivors. Acta Oncologica, 55(7), 821–827. https://doi.org/10.3109/0284186x.2016.1150607
- Watanabe, S., Nekolaichuk, C., Beaumont, C., & Mawani, A. (2009). The Edmonton symptom assessment system—what do patients think? Supportive Care in Cancer, 17(6), 675–683. https://doi.org/10.1007/s00520-008-0522-1
- Wicksell, R. K., Ahlqvist, J., Bring, A., Melin, L., & Olsson, G. L. (2008). Can exposure and acceptance strategies improve functioning and life satisfaction in people with chronic pain and Whiplash-Associated Disorders (WAD)? A randomized controlled trial. Cognitive Behaviour Therapy, 37(3), 169–182. https://doi.org/10.1080/16506070802078970
- World Health Organization. (2021, March 3). Cancer. Retrieved March 20, 2021, from https://www.who.int/news-room/fact-sheets/detail/cancer
- Yi, J. C., & Syrjala, K. L. (2017). Anxiety and depression in cancer survivors. The Medical Clinics of North America, 101(6), 1099–1113. https://doi.org/10.1016/j.mcna.2017.06.005
