ABSTRACT
Objectives
This study aimed (1) to determine the psychometric properties of a Thai version of the Maslach Burnout Inventory–Human Services Survey for Medical Personnel (MBI-HSS [MP]) and (2) to examine the mean scores of burnout and associated factors during the COVID-19 pandemic.
Methods
Forward and back translations of the MBI-HSS (MP) questionnaire were performed. The Thai version was subsequently completed by 682 Thai physicians and nurses who worked during the COVID-19 pandemic. Exploratory factor analysis was performed on the first subsample (n = 341) by conducting Kaiser Mayer-Olkin sampling adequacy measurement and Bartlett’s test of sphericity whereas confirmatory factor analysis (CFA) was performed on the second subsample (n = 341) using fit indices of the normed chi-square (χ2/df), the comparative fit index, the Tucker–Lewis index, and the root mean square error of approximation. This version’s internal consistency was investigated using Cronbach’s alpha coefficient. Demographic profiles were evaluated with descriptive and analytical statistics.
Results
The Thai version of the MBI-HSS (MP) displayed good psychometric characteristics, as the Cronbach’s alpha values of the 3 burnout factors ranged from 0.843 to 0.945. The CFA also showed good fit indices (χ2/df = 4.473; P < 0.001; RMSEA = 0.075 (95%CI = 0.055-0.079); CFI = 0.946; and TLI = 0.936). The physicians’ mean EE, DP, and PA scores were 25.28 ± 13.27, 7.15 ± 6.11, and 36.83 ± 8.13, respectively, whereas The nurses’ mean EE, DP, and PA scores were 23.10 ± 14.14, 4.43 ± 5.06, and 35.67 ± 10.24, respectively. Healthcare professionals who were younger, single, had fewer years of practice, and had more working hours per week tended to express more burnout scores.
Conclusions
The Thai version of the MBI-HSS (MP) demonstrates good psychometric properties in assessing burnout among healthcare professionals. Several factors may be pivotal in intensifying burnout.
Introduction
Burnout, a psychological syndrome occurring in response to chronic stress in the workplace (Maslach & Leiter, Citation2016), comprises 3 key dimensions. They are emotional exhaustion (loss of energy, depletion, and fatigue), depersonalization/cynicism (negative attitude toward clients, detachment, and withdrawal), and reduced personal accomplishment (reduced productivity and inability to cope) (Maslach & Leiter, Citation2016).
Before the pandemic of COVID-19, burnout had already been prevalent among physicians as a national survey reported that physicians were more likely to experience symptoms of burnout (37.9%) than the general population (27.8%) (Shanafelt et al., Citation2012). Physicians who had to work at the frontline care access, worked longer hours, and struggled with work-life integration tended to be at greater risk of burnout (Shanafelt et al., Citation2012). Burnout not only had an impact on healthcare providers’ well-being but was also correlated to medical error and clinical behaviors as well as loss of productivity (Reith, Citation2018).
Since 2020, a significant number of healthcare workers providing health services during the COVID-19 pandemic have experienced burnout due to exposure to various psychosocial stressors (Ulfa et al., Citation2021) and changes caused by the COVID-19 situation (Baptista et al., Citation2021; Denning et al., Citation2021; Khasne et al., Citation2020). Fear of COVID-19 could also directly and indirectly influence work stress, emotional exhaustion, and depersonalization among healthcare personnel (Ahorsu et al., Citation2022). Additionally, burnout in physicians and nurses may result from increased service demand and inadequate resources, changed work practices, prolonged wearing of protective equipment, and working in an unfamiliar environment (Denning et al., Citation2021).
During the COVID-19 pandemic, the prevalence of burnout among healthcare workers ranged between 6.0% and 90.4% (Meira-Silva et al., Citation2022; Nishimura et al., Citation2021; Tang et al., Citation2022). The broad range may be due to variations across studies in the burnout measurement tools, burnout definitions, and cutoff values used (Meira-Silva et al., Citation2022; Tang et al., Citation2022). Therefore, a well-accepted assessment tool specifically developed and culturally adapted for investigating burnout among Thai medical personnel is needed.
Burnout assessment instruments
The Maslach Burnout Inventory (MBI) is one of the most widely used measures for assessing dimensions of burnout in organizational psychiatry and psychology research (María Diaz Vizcaya et al., Citation2023). It was developed to assess the 3 dimensions of burnout and has been translated into many languages (Maslach & Leiter, Citation2016). MBI versions have been developed for a range of occupations. The MBI–Human Services Survey (MBI-HSS), the original version, extensively assesses burnout in workers who serve other people, while the MBI–General Survey (MBI-GS) measures burnout in people working in nonhuman service areas (Rotenstein et al., Citation2018). The MBI-HSS for Medical Personnel (MBI-HSS [MP]) was specifically developed to measure burnout in medical professionals. It has been translated into several languages (Lin et al., Citation2022). The MBI-HSS has been translated into the Thai language since 1989 and was tested for reliability (Summawart, Citation1989). Cronbach’s alpha coefficient of each domain was between 0.65 and 0.92 (Summawart, Citation1989). However, the previous study was done only among nurses and only in one hospital so the result may not represent different groups of healthcare professionals or other clinical settings. Moreover, the MBI-HSS (MP), which is more specific to medical personnel, has not been translated into the Thai language yet.
Factors associated with burnout
Burnout among healthcare workers during the COVID-19 pandemic has been attributed to increased workloads, long working hours, younger age (Kunno et al., Citation2022), few years of experience (Amanullah & Shankar, Citation2020; Galanis et al., Citation2021; Jakovljevic et al., Citation2021), and perception of stress (Joshi & Sharma, Citation2020). Being a frontline worker, ie, a member of a medical team directly caring for patients with COVID-19 infections, has been linked with an increase in the burnout rate (Lasalvia et al., Citation2021; Ulbrichtova et al., Citation2022) and, conversely, a decrease in the rate (Wu et al., Citation2020). It has been postulated that the decreased rate could be due to a greater sense of control among frontline workers than among those working in traditional wards (Wu et al., Citation2020). Therefore, the relationship between being a frontline healthcare worker and burnout remains controversial (Meira-Silva et al., Citation2022). In Thailand, burnout among medical staff during the COVID-19 pandemic was common (25.9%) and was associated with female sex (Kunno et al., Citation2022). However, other factors have yet to be studied extensively.
Our study had the following 2 aims:
To determine the psychometric properties of the Thai version of the MBI-HSS (MP) among physicians and nurses in Thailand
To examine the associated burnout factors in these groups of healthcare professionals during the pandemic.
Materials and methods
Translation
We obtained permission from Mind Garden, Inc., the copyright owner of the Maslach Burnout Inventory, to use, translate and culturally adapt the MBI-HSS (MP) into a Thai version. Two independent bilingual translators translated the MBI-HSS (MP) from the English version into 2 separate Thai versions. While the first translator was familiar with burnout content, the second was unaware of the MBI. A third translator then worked with the first 2 translators to resolve ambiguities and discrepancies in words and meanings. After that, 2 other independent translators back-translated the draft Thai version into English. The original English version was compared with the back-translated versions. Following discussion, the research team reached a consensus on the prefinal Thai version of the MBI-HSS (MP). The questionnaire was then administered to 10 medical professionals to probe how well they understood each item and how they responded. Appropriate revisions were made to the questionnaire before field testing began.
Study design and sampling method
An online cross-sectional survey was distributed to members of the Medical Association of Thailand, the Thailand Nursing and Midwifery Council, and several colleges governed by the Medical Council of Thailand. Their members included Thai physicians and nurses working in various clinical settings during the COVID-19 pandemic (August 2020–February 2022). Questionnaires that were not wholly answered and potential participants who declined to join the study were excluded.
Ethical considerations
Participants in this study were volunteers and were anonymous. Before this research began, the Siriraj Institutional Review Board approved its protocol (Si-350/2020).
Measurements
The MBI-HSS (MP)
Burnout was measured using the MBI-HSS (MP). It comprises 22 items categorized into 3 scales: emotional exhaustion (EE), depersonalization (DP), and lack of personal accomplishment (PA). The items are scored on a 7-point Likert scale (0 = never; 6 = every day) (Lin et al., Citation2022).The Perceived Stress Scale
The Thai version of the Perceived Stress Scale (PSS) was used to estimate to what degree individuals perceive their life as uncontrollable, unpredictable, and overloading. This reliable and valid instrument consists of 10 items. All are scored on a 5-point Likert scale (0 = never; 4 = very often) (Wongpakaran & Wongpakaran, Citation2010). Total scores range from 0 to 40.
The reliability of the Thai version of PSS found in our study was assessed by Cronbach’s alpha with values of 0.876.
Analysis
The sample size was calculated with a formula that used an alpha value of 0.05 and an estimated probability (P) value of 0.50. The calculated sample sizes were 374 and 299 for physicians and nurses, respectively (Hamed et al., Citation2020; Wang et al., Citation2020). To minimize the risk of a nonresponse rate and missing data, an additional 5% was allocated for sample recruitment.
The total sample was randomly and equally divided into two distinct and equivalent subsamples using computerized randomization in which exploratory factor analysis (EFA) was performed on the first sample (n = 341) whereas confirmatory factor analysis (CFA) was performed on the second sample (n = 341).
The EFA was performed on the first sample. This process was adapted for use with the ordinal data using polychoric correlation, and was conducted using the FACTOR software (version 12.2). To test factorability, we conducted Kaiser Mayer-Olkin (KMO) sampling adequacy measurement and Bartlett’s test of sphericity using the first sample. The KMO value ranged from 0.00 to 1.00. The KMO value of equal to or greater than 0.70 was desired (Lloret et al., Citation2017). Bartlett’s test of sphericity was utilized to ensure that variables and factors did not overlap and should yield a significant level of P < 0.05 to permit factorial analysis. The parallel analysis would be performed using unweighted least squares (ULS) as the estimation method followed by a direct oblimin rotation used for determining the number of factors (Horn, Citation1965).
The CFA was performed on the second sample analysis in MPLUS v. 7 software (Muthén & Muthén, Citation1998). We analyzed Mardia's (Citation1970) multivariate asymmetry skewness and kurtosis (Mardia, Citation1970). If the assumption of multivariate normality was violated and ordinal response data, we used the diagonally robust weighted least squares (WLSMV) estimation approach.
The CFA was carried out to confirm its structure validity by using fit indices of the normed chi-square (χ2/df), the comparative fit index (CFI), the Tucker–Lewis index (TLI), and the root mean square error of approximation (RMSEA). The model fit was considered adequate for CFI and TLI values greater than 0.9, whereas RMSEA values less than 0.08 suggested a suitable fit (Li et al., Citation2022).
The internal consistency of the Thai version of the MBI-HSS (MP) was investigated using Cronbach’s alpha coefficient.
Regarding demographic data, descriptive and analytical statistics were performed using IBM SPSS Statistics for Windows, version 24 (IBM Corp, Armonk, NY, USA.) Means and standard deviations (SDs) were calculated for continuous variables, while numbers and percentages were used for categorical variables. The relationship between the MBI-HSS (MP) assessments and PSS scores was examined by Pearson correlation coefficients. Statistical significance was set at a P value of less than 0.05. The independent t-tests and analysis of variance were used to test the relationship between MBI-HSS (MP) scores and demographic profiles.
Results
In all, 682 online questionnaires were returned by 381 physicians and 301 nurses. This represented a response rate of 28.72%.
Demographic profiles of physicians and nurses and perceptions of burnout
Most physicians were female (65.1%; ), aged between 30 and 39 (56.2%), single (55.6%), and specialists (79%) with 11–20 years of clinical experience (41.2%). They often worked more than 50 h per week (42.9%) and were typically not frontline workers (69.3%). Of the 381 physicians, 46.2% (n = 176) considered that they had burnout symptoms, and 47.2% believed that the COVID-19 pandemic might be the current primary cause of their burnout.
Table 2. Exploratory factor analysis of the Thai version of MBI-HSS (MP) (N = 341).
The majority of nurses were female (93.7%), aged over 50 (30.2%), and married (45.5%). They typically had more than 20 years of practice (49.2%), worked for 40–50 h per week (63.2%), and were not frontline workers (70.4%). Nearly half (45%) perceived themselves as having burnout, and 43.7% thought the pandemic might cause burnout in nurses ().
Table 1. Baseline characteristics of physicians and nurses.
Exploratory factor analysis
The KMO coefficient value in the first sample was 0.896 indicating factorability and Bartlett’s test of sphericity yielded a significant level of P < 0.001, χ2/df = 3820.4/231. displays the mean score, standard deviation (SD), skewness, kurtosis, corrected item-total correlation of each item with its factor and factor loading of the 3-factor extracted from the parallel analysis (Supplementary 1) with eigenvalues > 1 and cumulative explain variance 68.06% based on the analysis factor formed emotional exhaustion factor (9 items), depersonalization (5 items) and lack of personal accomplishment (8 items). The Cronbach’s alphas of EE, PA, and DP were 0.945, 0.847, and 0.843, respectively. The corrected item-total correlations of each item with its factor were all positive, ranging from 0.39 to 0.86 of the Thai version of the MBI-HSS (MP). The polychoric correlation matrix is available in (Supplementary 2).
Confirmatory factor analyses
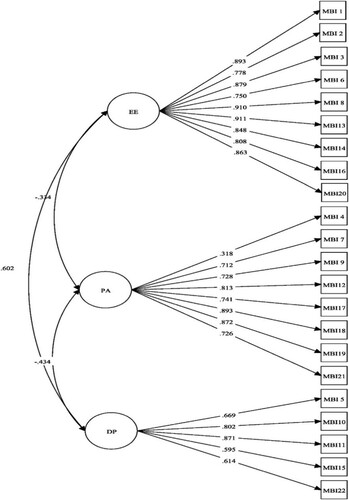
The analysis of ia's (1970) multivariate asymmetry skewness and kurtosis reported the kurtosis coefficient value was 655.686 (P < 0.001) implying the violation of the assumption of multivariate normality. Therefore, we performed CFA with the WLSMV estimation approach. The 3-factor structure of the MBI-HSS (MP) was evaluated through confirmatory factor analysis, which showed good fit indices for the Thai version (χ2/df = 4.473; P < 0.001; RMSEA = 0.075 (95%CI = 0.055-0.079); CFI = 0.946; and TLI = 0.936). The path diagram in indicates that the standardized coefficients of the relationship between factors and items ranged from 0.318 to 0.911.
Relationships between stress, demographic profiles, and MBI-HSS (MP) subscale scores in physicians
The physicians’ mean EE, DP, and PA scores were 25.28 ± 13.27, 7.15 ± 6.11, and 36.83 ± 8.13, respectively.
reveals that the mean EE and DP scores were significantly higher for participants who were younger than 30 years, were single, had 3 or fewer years of practice, and worked over 50 h per week (P < 0.05). Physicians who perceived that they had burnout had higher EE and DP scores but lower PA scores than their counterparts (P < 0.001). The mean scores of the MBI-HSS (MP) subscales for the frontline and nonfrontline healthcare professionals did not differ significantly. However, the mean PA scores were significantly higher for physicians who were aged over 50, were specialists, and had been working for more than 20 years ().
Table 3. Univariate analysis of MBI-HSS (MP) scores in relation to the demographic profiles of physicians.
The mean score for the Thai version of the PSS was 16.42 ± 6.87. The PSS score was positively correlated with the mean scores of EE (r = 0.72; P < 0.001) and DP (r = 0.44; P < 0.001). Conversely, the PSS score was significantly negatively correlated with the mean scores of PA (r = −0.61; P < 0.001).
Relationship between stress, demographic profiles, and MBI-HSS (MP) subscale scores in nurses
The nurses’ mean EE, DP, and PA scores were 23.10 ± 14.14, 4.43 ± 5.06, and 35.67 ± 10.24, respectively.
The mean EE and DP scores were significantly higher for nurses who were younger than 30, were single, and worked more than 50 h per week. Nurses who perceived themselves as having burnout showed significantly higher EE and DP scores but lower PA scores than those who did not feel burned out ().
Table 4. Univariate analysis of MBI-HSS (MP) scores in relation to the demographic profiles of nurses.
The mean DP score was higher for frontline nurses than for nonfrontline nurses (P < 0.002). However, the mean scores of the other burnout dimensions of the 2 groups did not differ significantly.
The nurses’ mean PSS score was 15.06 ± 6.49 and was positively correlated with MBI-HSS (MP) subscale scores for EE (r = 0.58; P < 0.001) and DP (r = 0.49; P < 0.001). However, the PSS score was negatively correlated with the PA score (r = −0.51; P < 0.001).
Discussion
Burnout among healthcare professionals was reported to be highest among physicians and nurses (Ghahramani et al., Citation2021). However, there is a lack of psychometric studies on the MBI-HSS (MP) (Lin et al., Citation2022). The current investigation represents the first psychometric study of the MBI-HSS (MP) in Southeast Asia. It is also the first study to demonstrate the validity and reliability of the Thai version of the MBI-HSS (MP).
Psychometric properties of the MBI-HSS (MP)
The Cronbach’s alpha reliability values of the 3 burnout factors evaluated by the MBI-HSS (MP) were 0.945, 0.847, and 0.843. Given that Cronbach’s coefficient values exceeding 0.7 indicate acceptability (Li et al., Citation2022), the MBI-HSS (MP) is a reliable means of assessing burnout in Thai medical personnel. This means that all 22 items of the MBI-HSS (MP) fitted all 3 burnout dimensions (EE, DP, and PA). Our findings are similar to those of an Iranian study at the item and scale levels (Lin et al., Citation2022).
As to structural validity, the confirmatory factor analysis revealed that the 3-factor model had a good fit. Two indicator values (CFI and TLI) were > 0.9, while the RMSEA value was < 0.08. These results confirmed that the 3 themes were distinguishable and conceptually intercorrelated. Stress was positively correlated with the EE and DP subscales but was negatively correlated with PA. These findings correspond with other studies that indicated that physicians and nurses suffering from burnout experience some degree of stress and have reduced confidence in their abilities (Johnson et al., Citation2020; Morgantini et al., Citation2020). Our results support that stress contributes to burnout and align with research that found a moderate correlation between work-related burnout and PSS scores (Hayes et al., Citation2021).
Burnout among healthcare providers during the COVID-19 pandemic
The results of the current study determined the average scores for the 3 burnout dimensions and the related factors among doctors and nurses. Our findings are consistent with other research: older participants who were specialized and had extensive work experience expressed a larger sense of PA than younger, single participants who worked longer hours and had less work experience (Baptista et al., Citation2021; Ferry et al., Citation2021; Galanis et al., Citation2021; Khasne et al., Citation2020). This disparity could be because younger healthcare providers had to work during an emerging infectious disease situation (COVID-19) despite having limited clinical experience dealing with extreme events and possibly a lower level of specialized training (Abdelhafiz et al., Citation2020; Ferry et al., Citation2021; Galanis et al., Citation2021). Longer work hours can be emotionally draining, especially for individuals on overnight shifts (Abdelhafiz et al., Citation2020). Furthermore, the finding that married healthcare workers reported less burnout than single workers is consistent with a study (Elghazally et al., Citation2021) that proposed that married health personnel might receive emotional support from their partners.
The influence of the sex of medical personnel on burnout is inconsistent across studies. Similar to some previous studies (Dinibutun, Citation2020; Zakaria et al., Citation2021), our study found no significant difference in the burnout scores of males and females. However, some other studies reported that females had a higher burnout rate. Those researchers hypothesized that the increased rate resulted from a dual role in executing domestic responsibilities alongside working in the medical field (Baptista et al., Citation2021; Khasne et al., Citation2020).
The present study highlighted that physicians and nurses who perceived themselves as having burnout were found to have higher EE and DP scores but lower PA scores upon assessment by the MBI-HSS (MP). Since many healthcare providers know they might have psychological distress, potential strategies to prevent, address, and reduce burnout should be provided in the workplace (Sharifi et al., Citation2021). Prior studies also supported the importance of developing strategies to improve resilience which can help each individual to cope with perceived job stress and burnout (Rashnuodi et al., Citation2022; Wu et al., Citation2022).
Burnout among frontline and nonfrontline healthcare workers
Many recent studies have demonstrated that frontline workers were at risk of burnout during the COVID-19 pandemic since they had to face difficulties managing patients with infection (Babamiri et al., Citation2022; Lasalvia et al., Citation2021). On the other hand, some studies found that burnout was also prevalent among nonfrontline health providers (Ghahramani et al., Citation2021; Wu et al., Citation2020).
One study demonstrated that the number of days spent directly providing care to patients with COVID-19 infections was significantly correlated with feelings of DP among nurses (Jiménez-Fernández et al., Citation2022). While the frontline nurses in our study tended to express symptoms of DP more than the nonfrontline workers, there were no significant differences in the 3 burnout scores of physicians who worked on the front line and those who did not. Hence, dealing directly with patients with COVID-19 infection may not be an isolated predictor of burnout. Other factors might also be related to occupational burnout, for example, time pressures, workplace stress, anxiety, a sense of not being in control, and inadequate coping strategies (Etesam et al., Citation2021; Ghahramani et al., Citation2021; Jiménez-Fernández et al., Citation2022; Wu et al., Citation2020).
Strengths, limitations, and suggested further research
A core strength of this study is that the Thai version of the MBI-HSS (MP) can be used in a Thai cultural setting. This is because the questionnaire was developed through cross-cultural adaptation. In addition, the psychometric findings indicated good internal consistency. The Cronbach’s alpha values of all dimensions of burnout were comparable to the Persian version of the MBI-HSS (MP) (range = 0.733–0.844) (Lin et al., Citation2022).
However, there are several limitations. First, previous studies on the psychometric properties of the MBI-HSS (MP) are limited; some studies are not available in English, making it difficult to compare results. This study was also conducted during several COVID-19 waves between 2020 and 2022. There were peaks and troughs in COVID-19 cases and periods when COVID-19 was under control. Consequently, it is unclear whether the COVID-19 situation directly caused burnout in medical personnel. Furthermore, there may have been a selection bias since medical personnel who felt highly distressed or not too distressed may have declined to participate.
Moving forward, it is recommended that prospective studies be undertaken to explore the sources and progression of burnout and its consequences on work performance and patient care. Burnout among other medical personnel is also an important issue to be investigated. Moreover, the effectiveness of individual and organizational interventions should be explored.
Implications
The study findings could help healthcare professionals become more aware of their psychological well-being. Interventions should focus on the individual and organizational levels to improve the management of workloads, enhance feelings of control, build clinical competence, and provide adequate support to health workers. It is also vital to develop specific strategies, such as enhancing personal resilience, to help medical personnel cope with burnout and stress, especially for those who are already aware that they might have burnout and work stress and ready to get help.
Conclusions
The Thai version of the MBI-HSS (MP) demonstrates good psychometric properties regarding internal consistency and validity. This Thai version of the MBI presents promising potential to assess burnout syndrome among physicians and nurses in Thailand. It could also benefit researchers and healthcare professionals in gaining insights into burnout among this population, especially during exceptional circumstances such as the COVID-19 pandemic.
Authors’ contributions
Study design, manuscript revising and approving: K.W., W.R., P.Pariwatcharakul, and P.Pukrittayakamee.
Conceptualization, data collection, interpretation of data and manuscript drafting: K.W.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Siriraj Institutional Review Board. See details under Methods.
Supplemental Material
Download MS Word (14.2 KB)Supplemental Material
Download MS Word (12.8 KB)Acknowledgement
The authors thank Mrs Lakkana Thongchot, Ms Naratip Sa-nguanpanich, Ms Sirinda Chanpen, and Ms Aree Singlamphong, our research assistants, for their contributions to this project. The authors also thank the Medical Association of Thailand, the Thailand Nursing and Midwifery Council, the colleges governed by the Medical Council of Thailand, Dr. Chonnakarn Jatchavala, and Mr. Thanayot Sumalrot for their kind help.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data underpinning the results can be obtained on reasonable request.
Additional information
Funding
References
- Abdelhafiz, A. S., Ali, A., Ziady, H. H., Maaly, A. M., Alorabi, M., & Sultan, E. A. (2020). Prevalence, associated factors, and consequences of burnout among Egyptian physicians during COVID-19 pandemic. Frontiers in Public Health, 8, 590190. https://doi.org/10.3389/fpubh.2020.590190
- Ahorsu, D. K., Lin, C.-Y., Marznaki, Z. H., & Pakpour, A. H. (2022). The association between fear of COVID-19 and mental health: The mediating roles of burnout and job stress among emergency nursing staff. Nursing Open, 9(2), 1147–1154. https://doi.org/10.1002/nop2.1154
- Amanullah, S., & Shankar, R. R. (2020). The Impact of COVID-19 on physician burnout globally: A review. Healthcare, 8(4), 421. https://doi.org/10.3390/healthcare8040421
- Babamiri, M., Bashirian, S., Khazaei, S., Sohrabi, M. S., Heidarimoghadam, R., Mortezapoor, A., & Zareian, S. (2022). Burnout and mental health of COVID-19 frontline healthcare workers: Results from an online survey. Iran Journal of Psychiatry, 17(2), 136–143.
- Baptista, S., Teixeira, A., Castro, L., Cunha, M., Serrão, C., Rodrigues, A., & Duarte, I. (2021). Physician burnout in primary care during the COVID-19 pandemic: A cross-sectional study in Portugal. Journal of Primary Care & Community Health, 12, 215013272110084. https://doi.org/10.1177/21501327211008437
- Denning, M., Denning, M., Goh, E. T., Tan, B., Kanneganti, A., Almonte, M., Scott, A., Martin, G., Clarke, J., Sounderajah, V., Markar, S., Przybylowicz, J., Chan, Y. H., Sia, C.-H., Chua, Y. X., Sim, K., Lim, L., Tan, L., Tan, M., … Kinross, J. (2021). Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: A multinational cross-sectional study. PLoS ONE, 16(4), e0238666. https://doi.org/10.1371/journal.pone.0238666
- Dinibutun, S. R. (2020). Factors associated with burnout among physicians: An evaluation during a period of COVID-19 pandemic. Journal of Healthcare Leadership, 12, 85–94. https://doi.org/10.2147/JHL.S270440
- Elghazally, S. A., Alkarn, A. F., Elkhayat, H., Ibrahim, A. K., & Elkhayat, M. R. (2021). Burnout impact of COVID-19 pandemic on health-care professionals at Assiut University Hospitals, 2020. International Journal of Environmental Research and Public Health, 18(10), 5368. https://doi.org/10.3390/ijerph18105368
- Etesam, F., Akhlaghi, M., Vahabi, Z., Akbarpour, S., & Sadeghian, M. H. (2021). Comparative study of occupational burnout and job stress of frontline and non-frontline healthcare workers in hospital wards during COVID-19 pandemic. Iran Journal of Public Health, 50(7), 1428–1435.
- Ferry, A. V., Wereski, R., Strachan, F. E., & Mills, N. L. (2021). Predictors of UK healthcare worker burnout during the COVID-19 pandemic. QJM: An International Journal of Medicine, 114, 374–380. https://doi.org/10.1093/qjmed/hcab065
- Galanis, P., Vraka, I., Fragkou, D., Bilali, A., & Kaitelidou, D. (2021). Nurses' burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Advanced Nursing, 77(8), 3286–3302. https://doi.org/10.1111/jan.14839
- Ghahramani, S., Lankarani, K. B., Yousefi, M., Heydari, K., Shahabi, S., & Azmand, S. (2021). A systematic review and meta-analysis of burnout among healthcare workers during COVID-19. Frontiers in Psychiatry, 12, 758849. https://doi.org/10.3389/fpsyt.2021.758849
- Hamed, R. A., Abd Elaziz, S. Y., & Ahmed, A. S. (2020). Prevalence and predictors of burnout syndrome, post-traumatic stress disorder, depression, and anxiety in nursing staff in various departments. Middle East Current Psychiatry, 27(1), 36. https://doi.org/10.1186/s43045-020-00044-x
- Hayes, S. W., Priestley, J. L., Moore, B. A., & Ray, H. E. (2021). Perceived stress, work-related burnout, and working from home before and during COVID-19: An examination of workers in the United States. SAGE Open, 4, 215824402110581. https://doi.org/10.1177/21582440211058193
- Horn, J. L. (1965). A rationale and test for the number of factors in factor analysis. Psychometrika, 30(2), 179–185. https://doi.org/10.1007/BF02289447
- Jakovljevic, B., Stojanovic, K., Nikolic Turnic, T., & Jakovljevic, V. L. (2021). Burnout of physicians, pharmacists and nurses in the course of the COVID-19 pandemic: A Serbian cross-sectional questionnaire study. International Journal of Environmental Research and Public Health, 18(16), 8728. https://doi.org/10.3390/ijerph18168728
- Jiménez-Fernández, R., Corral-Liria, I., Trevissón-Redondo, B., Lopez-Lopez, D., Losa-Iglesias, M., & Becerro-de-Bengoa-Vallejo, R. (2022). Burnout, resilience and psychological flexibility in frontline nurses during the acute phase of the COVID-19 pandemic (2020) in Madrid, Spain. Journal of Nursing Management, 30(7), 2549–2556. https://doi.org/10.1111/jonm.13778
- Johnson, A. R., Jayappa, R., James, M., Kulnu, A., Kovayil, R., & Joseph, B. (2020). Do Low self-esteem and high stress lead to burnout Among health-care workers? Evidence from a tertiary hospital in Bangalore, India. Safety and Health at Work, 11(3), 347–352. https://doi.org/10.1016/j.shaw.2020.05.009
- Joshi, G., & Sharma, G. (2020). Burnout: A risk factor amongst mental health professionals during COVID-19. Asian Journal of Psychiatry, 54, 102300. https://doi.org/10.1016/j.ajp.2020.102300
- Khasne, R. W., Dhakulkar, B. S., Mahajan, H. C., & Kulkarni, A. P. (2020). Burnout among healthcare workers during COVID-19 pandemic in India: Results of a questionnaire-based survey. Indian Journal of Critical Care Medicine, 24(8), 664–671. https://doi.org/10.5005/jp-journals-10071-23518
- Kunno, J., Supawattanabodee, B., Sumanasrethakul, C., Wiriyasirivaj, B., & Yubonpunt, P. (2022). Burnout prevalence and contributing factors among healthcare workers during the COVID-19 pandemic: A cross-sectional survey study in an urban community in Thailand. PLoS ONE, 17(8), e0269421. https://doi.org/10.1371/journal.pone.0269421
- Lasalvia, A., Amaddeo, F., Porru, S., Carta, A., Tardivo, S., Bovo, C., Ruggeri, M., & Bonetto, C. (2021). Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: A cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open, 11(1), e045127. https://doi.org/10.1136/bmjopen-2020-045127
- Li, W., Yu, H., Li, B., Zhang, Y., & Fu, M. (2022). The transcultural adaptation and validation of the Chinese version of the attitudes toward recognizing early and noticeable deterioration scale. Frontiers in Psychology, 13, 1062949. https://doi.org/10.3389/fpsyg.2022.1062949
- Lin, C.-Y., Alimoradi, Z., Griffiths, M. D., & Pakpour, A. H. (2022). Psychometric properties of the Maslach Burnout Inventory for Medical Personnel (MBI-HSS-MP). Heliyon, 8, e08868. https://doi.org/10.1016/j.heliyon.2022.e08868
- Lloret, S., Ferreres, A., Hernández, A., & Tomás, I. (2017). El análisis factorial exploratorio de los ítems: análisis guiado según los datos empíricos y el software. Anales de Psicología, 33(2), 417–432. https://doi.org/10.6018/analesps.33.2.270211
- Mardia, K. V. (1970). Measures of multivariate skewness and kurtosis with applications. Biometrika, 57(3), 519–530. https://doi.org/10.1093/biomet/57.3.519
- María Diaz Vizcaya, R., José Rodríguez Rivas, M., Mariño Méndez, H., Teresa Alvés Pérez, M., & López Castro, J. (2023). Euro-Burn I: Assessment of burnout syndrome in health workers in a Mediterranean country during the SARS-CoV-2 pandemic. The International Journal of Social Psychiatry, 25, 1–14. https://doi.org/10.1177/00207640231174364
- Maslach, C., & Leiter, M. P. (2016). Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry, 15(2), 103–111. https://doi.org/10.1002/wps.20311
- Meira-Silva, V. S. T., Freire, A. C. T. N., Zinezzi, D. P., Ribeiro, F. C. R., Coutinho, G. D., Lima, I. M. B., Crispi, I. C., Porto, J. D., Silva1, L. G. P., Miranda, L. H. A., Zurita, M. G. F., Belerique, V. H. R., & Bandoli, Y. T. (2022). Burnout syndrome in healthcare workers during the COVID-19 pandemic: a systematic review. Revista Brasileira de Medicina do Trabalho, 20(1), 122–131. https://doi.org/10.47626/1679-4435-2022-849
- Morgantini, L. A., Naha, U., Wang, H., Francavilla, S., Acar, Ö., Flores, J. M., Crivellaro, S., Moreira, D., Abern, M., Eklund, M., Vigneswaran, H. T., & Weine, S. M. (2020). Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS ONE, 15(9), e0238217. https://doi.org/10.1371/journal.pone.0238217
- Muthén, L., & Muthén, B. (1998). Mplus user’s guide, 7th Ed Los Angeles. Muthén & Muthén.
- Nishimura, Y., Miyoshi, T., Hagiya, H., Kosaki, Y., & Otsuka, F. (2021). Burnout of healthcare workers amid the COVID-19 pandemic: A Japanese cross-sectional survey. International Journal of Environmental Research and Public Health, 18(5), 2434. https://doi.org/10.3390/ijerph18052434
- Rashnuodi, P., Nourollahi-Darabad, M., Afshari, D., Shirali, G., Amiri, A., Rotkhali, E., & Shabgard, Z. (2022). The effect of resilience indicators on the job stress level among nurses: A predictor study. Asian Journal of Social Health and Behavior, 5(3), 138–145. https://doi.org/10.4103/shb.shb_4_22
- Reith, T. P. (2018). Burnout in United States healthcare professionals: A narrative review. Cureus, 10(12), e3681. http://doi.org/10.7759/cureus.3681
- Rotenstein, L. S., Torre, M., Ramos, M. A., Rosales, R. C., Guille, C., Sen, S., & Mata, D. A. (2018). Prevalence of burnout among physicians: A systematic review. JAMA, 320(11), 1131–1150. https://doi.org/10.1001/jama.2018.12777
- Shanafelt, T. D., Boone, S., Tan, L., Dyrbye, L. N., Sotile, W., Satele, D., West, C. P., Sloan, J., & Oreskovich, M. R. (2012). Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Archives of Internal Medicine, 172(18), 1377–1385. https://doi.org/10.1001/archinternmed.2012.3199
- Sharifi, M., Asadi-Pooya, A. A., & Mousavi-Roknabadi, R. S. (2021). Burnout among healthcare providers of COVID-19; a systematic review of epidemiology and recommendations. Arch Acad Emerg Med, 9(1), e7. https://doi.org/10.22037/aaem.v9i1.1004
- Summawart, S. (1989). Burnout among the staff nurses in Ramathibodi Hospital. Mahidol University. http://mulinet11.li.mahidol.ac.th/e-thesis/scan/18486.pdf
- Tang, R., Feng, O., Chong, J. J., & Wang, A. (2022). Evaluating the impact of coronavirus disease on burnout among healthcare workers using Maslach Burnout Inventory tool: A systematic review. Proceedings of Singapore Healthcare, 31, 201010582211173. https://doi.org/10.1177/20101058221117390
- Ulbrichtova, R., Svihrova, V., Tatarkova, M., Svihra, J., Novak, M., & Hudeckova, H. (2022). Prevalence of burnout syndrome in COVID-19 and non-COVID-19 units in university hospital: A cross-sectional study. International Journal of Environmental Research and Public Health, 19(19), 12664. https://doi.org/10.3390/ijerph191912664
- Ulfa, M., Azuma, M., & Steiner, A. (2021). Burnout status of healthcare workers in the world during the peak period of the COVID-19 pandemic. Frontiers in Psychology, 13, 952783. https://doi.org/10.3389/fpsyg.2022.952783
- Wang, J., Wang, W., Laureys, S., & Di, H. (2020). Burnout syndrome in healthcare professionals who care for patients with prolonged disorders of consciousness: a cross-sectional survey. BMC Health Services Research, 20(1), 841. https://doi.org/10.1186/s12913-020-05694-5
- Wongpakaran, N., & Wongpakaran, T. (2010). The Thai version of the PSS-10: An Investigation of its psychometric properties. BioPsychoSocial Medicine, 4(6), 6–6. https://doi.org/10.1186/1751-0759-4-6
- Wu, Y., Wang, J., Luo, C., Hu, S., Lin, X., Anderson, A. E., Bruera, E., Yang, X., Wei, S., & Qian, Y. (2020). A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. Journal of Pain and Symptom Management, 60(1), e60–e65. https://doi.org/10.1016/j.jpainsymman.2020.04.008
- Wu, Y.-P., Ahorsu, D. K., Chen, J.-S., Lin, C.-Y., Lee, C.-H., & Griffiths, M. D. (2022). The role of demographic factors, mindfulness and perceived stress in resilience among nurses: A cross sectional study. Journal of Nursing Management, 30(7), 3093–3101. https://doi.org/10.1111/jonm.13715
- Zakaria, M. I., Remeli, R., Ahmad Shahamir, M. F., Md Yusuf, M. H., Azizah Ariffin, M. A., & Noor Azhar, A. M. (2021). Assessment of burnout among emergency medicine healthcare workers in a teaching hospital in Malaysia during COVID-19 pandemic. Hong Kong Journal of Emergency Medicine, 28(4), 254–259. https://doi.org/10.1177/1024907921989499