ABSTRACT
Background
Physical activity referral schemes have been used extensively as one pathway to support behaviour change in people with long term conditions. Best practice guidance, across countries, recommend that schemes use behaviour change practices. The effectiveness of these schemes is inconsistent, yet, little is known about the implementation of specific approaches, or what influences practitioner’s delivery. This article provides a narrative review of evidence exploring the implementation of behaviour change practices in physical activity referral schemes.
Methods
An electronic search of three databases (PubMed, Scopus, Google Scholar) was undertaken. A menu of iterative techniques was also applied from the CLUSTER approach to increase coverage.
Results
A total of 45 eligible articles was included covering diverse research designs. Enduring issues with the literature pertain to the insufficient emphasis on implementation, a conflation of behaviour change practice, and an inconsistency of scheme components. Against this backdrop, diverse factors within practitioner, attendee, partnership, work environment, and organisational domains influence the implementation of behaviour change practices.
Conclusion
The translation of behaviour change practices to applied physical activity settings must tend to the multilevel factors which have the potential to influence the quality of behaviour change implementation.
Introduction
Physical activity (PA) has consistently been shown to improve health and wellbeing (Myers et al., Citation2015; Rhodes et al., Citation2017; Wood et al., Citation2022). Physical Activity Referral Schemes (PARS) originated in the United Kingdom in the 1990s and typically involve a physician referral of inactive individuals who are at risk of, or have, a chronic health condition to an exercise specialist, for a time-limited programme in leisure settings, to support long-term activity levels. Those who are eligible normally present with cardiometabolic, low level metal health, musculoskeletal, or respiratory disorders (Dugdill et al., Citation2005).
There was a rapid expansion of PARS across Scandinavia and Central Europe after their inception (Arsenijevic & Groot, Citation2017), and later augmented versions received widespread attention in Canada and the United States of America (Thompson et al., Citation2020). Despite the popularity of PARS, evidence continues to demonstrate equivocal improvements to PA and modifiable risk factors (Pavey et al., Citation2011; Prior et al., Citation2019; Rowley et al., Citation2018; Taylor et al., Citation2020). Across countries, best practice guidance recognises the need for exercise practitioners to utilise behaviour change practices to maximise PA improvements (Lobelo et al., Citation2014; Raustorp & Sundberg, Citation2014; National Institute for Health and Care Excellence [NICE], Citation2014). Behaviour change practices are viewed as a suite of techniques including goal setting, self-monitoring, education, reviews, feedback, action planning, relapse prevention plans, and facilitating social support, which should be tailored based on individual needs (NICE, Citation2014). In addition, practice should adopt a psychological theory of behaviour change and use a communication style to maximise motivation (Department of Health [DOH], Citation2001).
Despite this commitment to behaviour change practice, there is a paucity of research examining the delivery of behaviour change practices, and programmes are underreported (Oliver et al., Citation2016; Shore et al., Citation2019; Stevens et al., Citation2022). Without understanding the quality of practice, a rejection of a programme’s effectiveness may be made when ‘the programme itself is inadequate in terms of design or delivery’ (Green, Citation2000). Therefore, researching the ingredients to support the uptake of behaviour practices in exercise professionals is paramount (Stevens et al., Citation2022).
Nonetheless, the translation of evidence to practice is non-linear, unpredictable, and contingent on practitioner competencies and ‘situational judgment’ (Greenhalgh, Citation2018). Specifically, the complexities of PARS delivery have been highlighted including issues with conceptualisation, integration with the medical agendas, and the contested nature of schemes (Henderson et al., Citation2018). The challenges to PARS resonate with wider literature pertaining to community based PA interventions which are typically pragmatic, heterogeneous, lacking a clear theoretical underpinning, and have poor evaluation processes (Ashdown-Franks et al., Citation2022; Hawkes et al., Citation2022; Henderson et al., Citation2018; Oliver et al., Citation2016). Furthermore, across disciplines, the interest in behaviour change practices has soared but, like PARS, the emphasis on implementation is underdeveloped impinging robust learning about the application of behavioural science in applied settings (Luszczynska, Citation2020).
Despite a strong commitment to implementing behaviour change practices in PARS, the benefits have been underwhelming, creating a chasm between intention and outcome. The potential of implementation research in exercise settings to advance the field has been noted (Czosnek et al., Citation2020). Implementation science is a member of a consortium of fields examining the spread and uptake of research findings (Toms et al., Citation2019). Although implementation science provides an apparatus to understand the knowledge-to-practice gap, at the time of writing this review the authors could not locate an evidence synthesis exploring the implementation of behaviour change practices in PARS. The objective of the current review was therefore to provide an interpretive critique of literature examining the implementation of behaviour change practices in PARS, to advance knowledge to explain this chasm.
Table 1. Topic based search terms and arrangement of Boolean operators for the narrative review.
Table 2. Inclusion and exclusion criteria for citation screening.
Methods
A narrative review was undertaken, but the approach was also informed by pragmatic suggestions for reviewing evidence for complex interventions (Booth et al., Citation2013).
Literature search strategy
Two electronic databases, Pubmed and Scopus, were systematically searched to initially identify citations (Falagas et al., Citation2008) (April 2021). Search terms were orientated around three areas namely implementation, behaviour change practice, and PARS. ().
Due to the specific interest in the implementation of behaviour change practices, the search was undertaken using only the title field. Nevertheless, to mitigate any omissions, two supplementary approaches were undertaken. Firstly, an electronic search was repeated across three databases (PubMed, Scopus, Google Scholar) (October 2021) using only the PARS terms. Secondly, berrypicking, pursuing related projects, and following automated citation suggestions on publisher websites were used from the CLUSTER approach to increase the scope of the citation retrieval (Booth et al., Citation2013). The CLUSTER approach is deemed complementary to topic-based searches especially when examining context dependent phenomena and implementation (). The approach involves utilising a ‘pearl’ citation and then mining other relevant citations/authors/projects in an evolving manner through interrelated work.
Figure 1. The stages adopted during the integrative review.
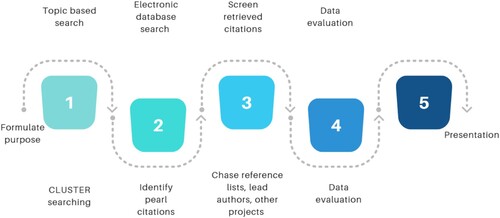
Figure 2. PRISMA flowchart outlining the study selection process based on relevance and ability to answer the research question.

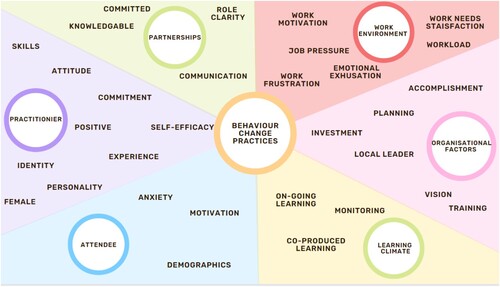
Figure 3. A visual representation of the narrative synthesis element of the review.
Eligibility criteria
There were no limits on study design, yet, to balance the levels of comprehensiveness with relevance, several filters were adopted (). Citations were only included if they were in English, peer reviewed, and had a label related to PARS. Manuscripts were included from 2001 onwards, as the English quality standards were published in 2001 and explicitly outlined the need for behaviour change practices (DOH, Citation2001). Grey literature was not used as the goal was to appraise the academic coverage of behaviour change implementation in exercise settings explicitly. Schemes that were undertaken outside of community settings, with special populations and specialist staff, were omitted as they represent settings not typical of PARS.
Study selection
The initial database search yielded 1461 citations, yet only three of 23 relevant citations explicitly examined implementation, either lived experience of implementation attempts or assessing fidelity to delivery style or behaviour change technique frameworks. A subsequent search using only the PARS labels yielded 10,800 citations, increasing the scope of the search. This subsequent search, and CLUSTER techniques, provided 22 additional citations and 316 duplicates were omitted. When titles were retrieved but did not have all elements of the search terms, they were read to appraise their relevance. The trimming process created a total of 45 manuscripts for review ().
Analysis and synthesis
Descriptive information for each paper was extracted and stored in a Microsoft Excel matrix. All screened manuscripts were also uploaded to NVivo 12 for detailed analysis and analytical memoing (Toronto & Remington, Citation2020). A constant comparison approach was adopted, which involved contrasting each emerging theme to consider refinements, consolidation, or new insights (Whittemore & Knafl, Citation2005).
Data reduction involved organising data, from open coding, into subcategories to unpick critical insights (Cronin & George, Citation2020). Lower order themes were generated when information was deemed relevant to the review question. Each new inductive label was cross-checked with previous subcategories to see if it could reside within existing nodes. Data segments were given a new label if they conflicted previous lower order themes or provided new insight. Once coding was completed, subcategories were checked for overlap and lower order themes were grouped under higher level themes. Data display was an ongoing process and handwritten mind maps allowed the processing of reoccurring areas of interest (Whittemore & Knafl, Citation2005). Due to the nature of the field, the themes were not restricted to the barriers and facilitators of implementation but also included critiques and juxtapositions between research traditions.
Results
A descriptive overview of the included manuscripts can be found as a supplementary file. The results are presented as a critical interpretive overview of the field showcasing the current limitations that exist, followed by a narrative summary of the factors which influence the implementation of behaviour change practices by PARS practitioners ().
The current limitations noted in the literature
Implementation processes not considered
Research outlined that the predictors of behaviour change practices are largely unknown (Raposo et al., Citation2020; Sánchez-Oliva et al., Citation2021; Shore et al., Citation2022; Silva et al., Citation2017; Stacey et al., Citation2010). Furthermore, despite some manuscripts having implementation in their title, many prioritised health outcomes without considering how variations in implementation may influence success/failure (Andersen et al., Citation2019; Balducci et al., Citation2019; Blom et al., Citation2020; Galbraith et al., Citation2021; Gallegos-Carrillo et al., Citation2017; James et al., Citation2017b; Mazzoni et al., Citation2020; O’brien et al., Citation2021; Sjöling et al., Citation2011; Sørensen et al., Citation2008; Spence et al., Citation2022; Williamson et al., Citation2015; Yang et al., Citation2015).
Authors outlined the need for more process evaluations and highlighted a lack of implementation exploration. A small body of evidence did outline that the monitoring of implementation is currently not aligned with best practice, stunting knowledge on how behaviour change practices can be implemented (Beck et al., Citation2016; Czosnek et al., Citation2021; Dineen, Bean, et al. Citation2021; Lambert et al., Citation2017; Moore et al., Citation2013; O’Shea et al., Citation2016; Purdy et al., Citation2022; Quested et al., Citation2017; Smith et al., Citation2021). Although many manuscripts failed to consider the design and delivery of the intervention, others had a strong theoretical base (Williamson et al., Citation2015). Nevertheless, the exploration of how logic models, theoretical underpinning, or training was translated to practice was lacking, and there was limited research appraising the acceptability of scheme components to practitioners (Czosnek et al., Citation2021; Quested et al., Citation2017).
A general concern was the subjective measurement of implementation. When implementation was considered, practice was approximated through self-report surveys (Dineen et al., Citation2022; Raposo et al., Citation2020; Sánchez-Oliva et al., Citation2021; Silva et al., Citation2017), notes from practitioners (Mazzoni et al., Citation2020), or checklists (Dineen, Banser, et al. Citation2021; Dineen, Bean, et al. Citation2021). This is prudent given that objective data about delivery demonstrated poor convergence with self-reported data (Lambert et al., Citation2017).
The current mechanistic view of behaviour change practices
Behaviour change practice was largely conflated to a menu of techniques misrepresenting optimal care (Rowley et al., Citation2021; Shore et al., Citation2022; Silva et al., Citation2017). One study did critique the conflation of behaviour change practice (Gagnon et al., Citation2018), however, despite their initial critique, their own checklist may underrepresent the relational aspects of practice.
Elsewhere authors conceptualised practice as solely educational (Gallegos-Carrillo et al., Citation2017; O’brien et al., Citation2021; Williamson et al., Citation2015), demonstrating a one-dimensional view of practice. One study mentioned supervision without detailing practices (Williamson et al., Citation2015), whilst another study referred to the use of motivational interviewing without defining what practitioners were envisaged to deliver (Hoekstra, van Offenbeek, et al. Citation2017b). Lastly, in a intervention development study, practice was reduced to the provision of ‘behavioural support’ and a list of techniques (Reale et al., Citation2021).
The distinction between the scheme elements was not clear and many authors did not disaggregate between the exercise component and behavioural support. Where implementation was assessed, it referred to the implementation of the exercise intervention and not specific behaviour change practices, diluting the emphasis on behaviour change practices (Grimmett et al., Citation2021; Purdy et al., Citation2022; Wurz et al., Citation2021).
There was a small body of work that recognised the complexity of behaviour change practice, which contrasted with the dominant paradigm. Quested and colleagues (Citation2017) highlighted that practice requires adaptation and collaboration with individuals and, as such, there is no exact formula for optimal behaviour change practice. Czosnek and her co-authors (2021) also explained that tailoring practice is fundamental for behaviour change practice. Therefore, the core components of practice, or minimal expectations of delivery, must be established, which is currently not addressed in the literature.
The biomedical dominance
A contributing factor to the conflation of behaviour change practice may be the dominance of the biomedical model. Gray (Citation2019) argued that the current viewpoint of exercise may lead to a diminished value of professional wisdom, the experiential art of supporting people, and the phenomenological aspects of health.
The biomedical model was noted throughout the reviewed manuscripts and research gave primacy to dispensing exercise and measuring safety, adherence, and clinical outcomes. The current culture privileges changing clinical outcomes over supporting the implementation of behaviour change practices (Buckley et al., Citation2018; Rowley et al., Citation2021). As Gray (Citation2019) notes, this creates expectations about practice and can shape practitioner’s identity. There was an enduring priority to use the consultation to collect medical data which impinged on other consultation elements (Moore et al., Citation2011). The biomedical model was further illustrated in the work by Gustavsson and colleagues where many stakeholders viewed the scheme as a written exercise programme alone despite the Swedish model being underscored by person-centred care and having five components.
Diversity of scheme components
There was no consistency for any PARS elements creating issues with the operation of schemes. Much of the reviewed literature deviated from the core tenets of PARS and lacked consistency in relation to staffing, inclusion criteria, and intervention content (O’Brien et al., Citation2021). Scheme content fluctuated from PA counselling, exercise alone, or a combination of both. Attendees included those with, and without, long-term conditions and schemes were led by an array of professionals including exercise physiologists, exercise scientists, fitness staff, physical therapists, sports therapists, kinesiologists, and physiotherapists.
The duration of programmes had no clear pattern and ranged from three weeks (Dineen et al., Citation2022) to three years (Balducci et al., Citation2019). Some schemes were underpinned by social cognitive theories (Carr et al., Citation2021; Duda et al., Citation2014; Galbraith et al., Citation2021; Gallegos-Carrillo et al., Citation2017; James et al., Citation2017; Rogers et al., Citation2015; Smith et al., Citation2021; Yang et al., Citation2015), some were guided by motivational interviewing (Blom et al., Citation2020; Carr et al., Citation2021; Dineen, Banser, et al. Citation2021; Galbraith et al., Citation2021; Hoekstra, van Offenbeek, et al. Citation2017b; Moore et al., Citation2013; O’Halloran et al., Citation2014; Wurz et al., Citation2021; Sjöling et al., Citation2011) and others had no outline of their behavioural content. Some settings utilised outdoor PA (Blom et al., Citation2020), sport (Dineen et al., Citation2022), group work (James et al., Citation2017; Rogers et al., Citation2015; Smith et al., Citation2021; Sørensen et al., Citation2008), and online options (Williamson et al., Citation2015).
Many manuscripts had settings not reflective of real-life PARS which may complicate the evidence. For example, in the work of Sørensen and colleagues (Citation2008), participants had to be willing to pay for care, be motivated to change, and staff nominated themselves for training. Likewise in Gagnon et al. (Citation2018) only the highest ranked university students were used as practitioners. Lastly, in the work of Hoekstra and colleagues (Citation2017b), the inclusion criterion stipulated that organisations had to be willing to implement and continue the programme, invest in the programme, and comply with the research procedures for the entirety of the project. The diversity in how PARS are defined creates an array of contextual factors making implementation research difficult as the literature is largely incomparable.
Factors influencing the implementation of behaviour change practices
Attendee characteristics
Attendees often arrived at leisure settings anxious and feeling out of place due to the intimating environment. It was postulated that behaviour change practice is more difficult under these circumstances (Quested et al., Citation2017), as practice must focus on reassurance instead of behaviour change (Shore et al., Citation2022). Working with hesitant attendees altered the practitioner’s beliefs about their ability to support change (Reale et al., Citation2021). The attendee’s unease, and the subsequent lack of optimism about the likelihood of behaviour change from practitioners, was magnified when attendees received no prior communication from medical staff about the scheme, and where consultations were short (Reale et al., Citation2021; Shore et al., Citation2022). Practitioners valued booster training to develop skills to deal with less motivated individuals (Carr et al., Citation2021). The level of attendee motivation also augmented the degree of work motivation, frustration, and desire to work in PARS. Retention of attendees was greater in high socioeconomic, English speaking, and well-educated groups, potentially verifying this relationship (Duda et al., Citation2014; Purdy et al., Citation2022).
Practitioner characteristics
In settings where practitioners perceived behaviour change practices as compatible with the organisational agenda, implementation was more likely. Applying behaviour change approaches, and seeing their impact, also had a reinforcing effect on their attitudes (Dineen et al., Citation2022; Moore et al., Citation2012). Conversely, where staff perceived they already implement behaviour change practices, or viewed the consultation as solely about information gathering, adoption was hindered (Buckley et al., Citation2018; Moore et al., Citation2012).
The training norms prioritise a medical lens which may lead to deep-rooted ideas about professional duties (Gray, Citation2019; Raposo et al., Citation2020). In addition, it was shown that as self-efficacy increased, the value of behavioural approaches also increased, highlighting a feedback loop between value, engagement, practice, and subsequent self-efficacy (Dineen et al., Citation2022; Reale et al., Citation2021). Tendency to react to organisational pressure, may also explain the variation in the implementation of behaviour change practices (Raposo et al., Citation2020). This was demonstrated when organisational pressure decreased the perceived importance of behaviour change practice (Duda et al., Citation2014). Conversely, it was shown that personal commitment to support attendees superseded the organisational pressure to secure gym memberships (Shore et al., Citation2022). Several authors outlined that positive, committed, and enthusiastic practitioners were associated with envisaged, and actual, implementation (Dineen et al., Citation2022; Hoekstra, Hettinga, et al. Citation2017a; Shore et al., Citation2022)
One manuscript also discussed how a positive and committed practitioner can spread innovations to colleagues by altering practice norms. In addition, one manuscript demonstrated that women, and those with greater than eight years’ experience, were more likely to implement behaviour change practices (Raposo et al., Citation2020). Having an accreditation may also improve the medical professional’s trust in PARS and the clarity of duties for each profession (Reale et al., Citation2021).
Work environment
Where practitioners perceived the work environment to be ‘needs supportive’, emotional exhaustion was decreased, feelings of personal accomplishment were increased, and implementation was more likely (Sánchez-Oliva et al., Citation2021; Silva et al., Citation2017). Opportunities to contribute to the organisational agenda, continuing professional development, and feeling heard were common ways ‘needs satisfaction’ was achieved (Silva et al., Citation2017).
It is also noted that behaviour change practice is emotionally taxing and fatigue may influence the quality of practice (Dineen et al., Citation2022). This was corroborated elsewhere, where a high workload, overrunning consultations, and working beyond capacity increased stress (Dineen et al., Citation2022). In combination with the taxing nature of the role, it was noted that where the organisation was controlling, and practitioners felt powerless, emotional exhaustion was magnified and autonomous motivation decreased (Raposo et al., Citation2020; Silva et al., Citation2017). The level of job pressure was also linked to needs frustration and poor implementation (Sánchez-Oliva et al., Citation2021). Lastly, practitioners who worked greater than 20 hours a week were less likely to employ behaviour change practices (Sánchez-Oliva et al., Citation2021).
Organisational factors
The providers of PARS must invest, and provide sustainable investment, to increase penetration of behaviour change practices (Purdy et al., Citation2022; Hoekstra, Hettinga, et al. Citation2017a; Smith et al., Citation2021). Where the organisation undertook inclusive planning it increased awareness, importance, needs satisfaction of staff, and produced an intervention which met the needs of the attendees and employees (Buckley et al., Citation2018; Dineen et al., Citation2022). When the core elements of the programme were made explicit, it also supported practitioners to adapt non-essential aspects whilst retaining essential elements (Purdy et al., Citation2022).
Organisations can support implementation by creating accessible policies and practice guidelines. There also needs to be ongoing communication and support on how to convert guidelines into practice (Gustavsson et al., Citation2018; Reale et al., Citation2021). Increased options for attendees must be offered in scheme polices, as gym settings, and limited choice for attendees, decreased adherence and made implementation more difficult (Carr et al., Citation2021; Shore et al., Citation2022).
The role of training to support implementation was widespread and ongoing training provided direction, enhanced skill development, knowledge, altered attitudes, and decreased drift/decay. The typical training provision of two days was seen as inadequate to support implementation (Moore et al., Citation2012).
The current understanding of the training provided to PARS practitioners is underexplored (Quested et al., Citation2017; Shore et al., Citation2022; Wurz et al., Citation2021). Furthermore, current exercise qualifications do not equip practitioners to undertake behaviour change practices (Gustavsson et al., Citation2018; Reale et al., Citation2021). It was shown that exercise practitioners do not integrate knowledge through a medical lens thus there is a need for organisations to provide expert guidance, self-reflection, refreshers, peer support, and rehearsal of skills to overcome the industry drawbacks (Gray, Citation2019; Reale et al., Citation2021; Stacey et al., Citation2010).
Local leadership supported implementation by providing expert advice, peer support, championing, allocating resources, responding to local issues, monitoring, and issuing feedback. Leaders need to be credible, respected, have influence on senior management, and have the capacity to undertake planning (Dineen et al., Citation2022). The quality of relationships, feelings of support and personal capability, spread of workforce champions, practice expectations, and communication of updates about practice are under the direct control of the leader (Dineen et al., Citation2022; Gustavsson et al., Citation2018; Hoekstra, Hettinga, et al. Citation2017a; Raposo et al., Citation2020).
Implementation was higher in organisations that had an explicit vision and strategy to support implementation. It was suggested that local commitment contextualises innovation and allows local procedures to align with the vison. An alignment to a vision facilitates intensification of practice, whereas the use of controlling practices by the organisation creates a precedent, and practitioners treat attendees in the same way (Raposo et al., Citation2020).
Partnerships
The partnership between the exercise and medical professions was a consistent theme purported to support implementation. Communication and collaboration were important to provide local ownership of the scheme, shared advocacy, recognition, and acceptance (Purdy et al., Citation2022; Caperchione et al., Citation2021; Hoekstra, van Offenbeek, et al. Citation2017b). A committed and enthusiastic physician is important to champion behaviour change practices. It was also highlighted that physician support, and their utilisation of behaviour change practices, provided credibility and ensured attendees were more receptive to behaviour change practices (Caperchione et al., Citation2021; Carr et al., Citation2021). Yet there is a disjoint, and physicians do not often advocate or maximise the teachable moment (Caperchione et al., Citation2021; Gustavsson et al., Citation2018). This was also seen where practitioners had to ‘sell exercise’ as attendees came without any information about the scheme, hampering implementation (Shore et al., Citation2022). Physicians did not feel behaviour change was within their duty and the distinction between roles in PARS is lacking (Caperchione et al., Citation2021; Gustavsson et al., Citation2018).
Learning climate
Typical investment in evaluation and quality improvement is poor in PARS (Buckley et al., Citation2018; Lambert et al., Citation2017; Spence et al., Citation2022). Nevertheless, the importance of ongoing learning was highlighted as fundamental for implementation. Firstly, for exercise practitioners developing a co-learning climate was more appealing and acceptable than issuing academic information (Stacey et al., Citation2010). Secondly, iterative planning with stakeholders increased engagement, critical thinking, problem solving, ownership, and created acceptable programme structures (Buckley et al., Citation2018; Dineen et al., Citation2022; Hoekstra, van Offenbeek, et al., Citation2017b; Reale et al., Citation2021; Smith et al., Citation2021; Wurz et al., Citation2021). Thirdly, behaviour change is not a formulaic practice and meetings provided the opportunity to enhance context-specific learning and practitioner motivation. Ongoing meetings also supported the sharing of challenges, lessons learnt, and cemented a community of practice (Grimmett et al., Citation2021).
Explicit monitoring supported implementation by accumulating evidence engendering greater confidence in PARS (Gustavsson et al., Citation2018; Purdy et al., Citation2022) and reinforced practitioner behaviour. The periodic evaluation of practice, and access to learning materials, were deemed beneficial for implementation (Beck et al., Citation2016; Dineen et al., Citation2022; Gagnon et al., Citation2018; Shore et al., Citation2022; Wurz et al., Citation2021; Hoekstra, Hettinga, et al. Citation2017a). Formative evaluation and feedback improved memory and stimulated reflection, postulated to enhance implementation. The presence of programme manuals/booklets was also seen to enhance delivery, break down attendee barriers, contextualise care, and guide behaviour change practice. A commitment to self-reflection and access to expert guidance was paramount and envisaged to increase self-efficacy and skill development (Gustavsson et al., Citation2018; Moore et al., Citation2013; Smith et al., Citation2021).
Discussion
Although behavioural science is acknowledged as fundamental to PARS, the complexity of behaviour change practice is still evolving (Borek et al., Citation2019; Hagger et al., Citation2020; McEwan et al., Citation2019), and research focusing on implementation is lacking (Luszczynska, Citation2020). Specifically in PARS, there is a paucity of research exploring the implementation of practices and literature continues to privilege testing the efficacy of PARS, from an exercise standpoint, and its role in risk factor management, largely ignoring the role of behavioural science.
The dominant biomedical paradigm, highlighted in the current review, is incongruent with the implementation of behaviour change practices and has implications for training, evaluation, funding, and attendee satisfaction. There seems to be an artificial view of what behaviour change practice entails, and many conceptualise practice as a list of pre-set techniques, hampering practitioner’s ability to support behaviour change in naturalistic settings. The current review suggests that greater attention must be placed on quality improvement through a congruent lens. Authors have highlighted how a biomedical lens hinders the implementation of behaviour change practices as it dampens attendee autonomy and creates a power differential (Moore et al., Citation2017). Nonetheless, if there was a greater adherence to a biomedical model, it could operate in clinical settings, with specialist staff, to decrease the immediate risk of mortality, as in the case of cancer prehabilitation (Jones et al., Citation2021; Moore et al., Citation2021). Alternatively, schemes should shed the ‘prescription’ model and conceptualise PARS as predominately about long-term PA changes. At present PARS retains a biomedical format, but practice does not/is unable to operate within a clinical exercise remit which creates issues. Due to this tension physicians are dissuaded to trust schemes as they lack applied health professional regulation, are not integrated in medical pathways, and are assessed on outcomes which they are not designed to address (Shore et al., Citation2021). The implementation of PA policy requires a proactive definition of practice and engagement with implementation science (Lobczowska et al., Citation2022; Toomey et al., Citation2020).
The current synthesis provides useful information about prudent reported factors that may influence the implementation of behaviour change practices in PARS. The review was however unable to comment on details that were not reported, or how the various features noted exert their influence, which is common in implementation science (Sarkies et al., Citation2022). The measurement of behaviour change practices through surveys, in this narrative review, is a reflection on what practitioners envisage they do, instead of capturing their responses in naturalistic settings. This must be treated with caution as practitioners subjective ideas about their practice may not accurately represent what is delivered (Lambert et al., Citation2017).
A separate issue is the diverse settings noted and the lack of recognition that these settings may augment implementation. Many of the manuscripts involved physiotherapists, integration in medical environments, and intense research trials which are not typical of PARS. Authors in implementation science corroborate the concerns articulated above, as extensive research planning, funding, and academic support may augment the implementation climate (Braithwaite et al., Citation2018). In addition, across implementation research, there is a lack of information about the influence of contextual factors in applied settings which is stunting knowledge about how and why implementation is achieved in a variety of settings (Dryden-Palmer et al., Citation2020).
The current review collated a menu of factors that influence the implementation of behaviour change practice in PARS. This review is timely given the interesting attention on implementation science in exercise settings (Czosnek et al., Citation2020), the recognition that exercise specialists are largely under researched (Stevens et al., Citation2022), and the continued appetite for exercise specialists to be integrated with medical professionals (Maiorana et al., Citation2018; Speake et al., Citation2016).
The current synthesis drew connections across domains which influence the implementation of behaviour change practices in exercise settings, however, no researchers explored the explanatory mechanisms that influence implementation. Moreover, at the time of writing this review, it has not been possible to uncover how context interacts with implementation attempts of behaviour change practice in PARS.
Conclusion
The review aimed to provide a critical interpretive account of the field and examine the factors that influence the implementation of behaviour change practices in PARS. Greater utilisation of implementation science is needed to overcome the challenges that endure in behaviour change research. Moreover, there is a need for future research to employ methods that address the implementation processes and move beyond examining the reach, dose, fidelity, and changes to attendee outcomes, which cannot explain how implementation occurs. The recognition of behaviour change practices has exceeded research on how evidence can be translated to applied settings. Future work should invest in describing and planning the expectations of practice and employ well-known behaviour change techniques taxonomies to guide practice. There is a need to cultivate a learning climate that values quality improvement through greater surveillance, reporting practice, and encouraging peer reviews focusing on both the intervention content and the quality of delivery. Lastly, researchers should adopt designs which can accumulate an understanding on how contextual factors directly influence the decision making of practitioners to implement or abandon behaviour change practices.
Ethics statement
The study was except from ethical committee approval as it was a narrative review which synthesised the established evidence base.
Acknowledgments
Elena Golder, Dr Paula Watson.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Andersen, P., Lendahls, L., Holmberg, S., & Nilsen, P. (2019). Patients’ experiences of physical activity on prescription with access to counsellors in routine care: A qualitative study in Sweden. BMC Public Health, 19(1), 1–11. https://doi.org/10.1186/s12889-018-6343-3
- Arsenijevic, J., & Groot, W. (2017). Physical activity on prescription schemes (PARS): Do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses. BMJ Open, 7(2), 1–14. https://doi.org/10.1136/bmjopen-2016-012156
- Ashdown-Franks, G., DeJonge, M., Arbour-Nicitopoulos, K. P., & Sabiston, C. M. (2022). Exploring the feasibility and acceptability of a physical activity programme for individuals with serious mental illness: A case study. Qualitative Research in Sport, Exercise and Health, 14(6), 933–55. https://doi.org/10.1080/2159676X.2021.2019098
- Balducci, S., D’Errico, V., Haxhi, J., Sacchetti, M., Orlando, G., Cardelli, P., & Vitale, M. (2019). Effect of a behavioral intervention strategy on sustained change in physical activity and sedentary behavior in patients with Type 2 Diabetes: The IDES-2 randomized clinical trial. JAMA - Journal of the American Medical Association, 321(9), 880–90. https://doi.org/10.1001/jama.2019.0922
- Beck, F. E., Gillison, F. B., Koseva, M. D., Standage, M., Brodrick, J. L., Graham, C., & Young, H. (2016). The systematic identification of content and delivery style of an exercise intervention. Psychology & Health, 31(5), 605–21. https://doi.org/10.1080/08870446.2015.1132718
- Blom, E. E., Aadland, E., Solbraa, A. K., & Oldervoll, L. M. (2020). Healthy life centres: A 3-month behaviour change programme’s impact on participants’ physical activity levels, aerobic fitness and obesity: An observational study. BMJ Open, 10, 1–9. https://doi.org/10.1136/bmjopen-2019-035888
- Booth, A., Harris, J., Croot, E., Springett, J., Campbell, F., & Wilkins, E. (2013). Towards a methodology for cluster searching to provide conceptual and contextual ‘richness’ for systematic reviews of complex interventions: Case study (CLUSTER). BMC Medical Research Methodology, 13(1), 1–14. https://doi.org/10.1186/1471-2288-13-118
- Borek, A. J., Abraham, C., Greaves, C. J., Gillison, F., Tarrant, M., Morgan-Trimmer, S., McCabe, R., & Smith, J. R. (2019). Identifying change processes in group-based health behaviour-change interventions: Development of the mechanisms of action in group-based interventions (MAGI) framework. Health Psychology Review, 13(3), 227–47. https://doi.org/10.1080/17437199.2019.1625282
- Braithwaite, J., Churruca, K., Long, J. C., Ellis, L. A., & Herkes, J. (2018). When complexity science meets implementation science: A theoretical and empirical analysis of systems change. BMC Medicine, 16(1), 1–14. https://doi.org/10.1186/s12916-018-1057-z
- Buckley, B. J. R., Thijssen, D. H. J., Murphy, R. C., Graves, L. E. F., Whyte, G., Gillison, F. B., Crone, D., Wilson, P. M., & Watson, P. M. (2018). Making a move in exercise referral: Co-development of a physical activity referral scheme. Journal of Public Health, 40(4), e586–93. https://doi.org/10.1093/pubmed/fdy072
- Caperchione, C. M., Sharp, P., Phillips, J. L., Agar, M., Liauw, W., Harris, C. A., Marin, E., McCullough, S., & Lilian, R. (2021). Bridging the gap between attitudes and action: A qualitative exploration of clinician and exercise professional’s perceptions to increase opportunities for exercise counselling and referral in cancer care. Patient Education and Counseling, 105, 0–1. https://doi.org/10.1016/j.pec.2021.11.002
- Carr, S., Burke, A., Chater, A. M., Howlett, N., & Jones, A. (2021). An evolving model of best practice in a community physical activity program: A case study of ‘active Herts’. Journal of Physical Activity and Health, 18(October), 1555–1562. https://doi.org/10.1123/jpah.2021-0078
- Cronin, M. A., & George, E. (2020). The why and how of the integrative review. Organizational Research Methods, 26(1), 168–192. https://doi.org/10.1177/1094428120935507
- Czosnek, L., Rankin, N., Zopf, E., Richards, J., Rosenbaum, S., & Cormie, P. (2020). Implementing exercise in healthcare settings: The potential of implementation science. Sports Medicine, 50(1), 1–14. https://doi.org/10.1007/s40279-019-01228-0
- Czosnek, L., Richards, J., Zopf, E., Cormie, P., Rosenbaum, S., & Rankin, N. M. (2021). Exercise interventions for people diagnosed with cancer: A systematic review of implementation outcomes. BMC Cancer, 21(1), https://doi.org/10.1186/s12885-021-08196-7
- Department of Health. (2001). Exercise referral systems. Crown Publications.
- Dineen, T. E., Banser, T., Bean, C., & Jung, M. E. (2021). Fitness facility staff demonstrate high fidelity when implementing an evidence-based diabetes prevention program. Translational Behavioral Medicine, 11(10), 1814–22. https://doi.org/10.1093/tbm/ibab039
- Dineen, T. E., Bean, C., Cranston, K. D., MacPherson, M. M., & Jung, M. E. (2021). Fitness facility staff can be trained to deliver a motivational interviewing-informed diabetes prevention program. Frontiers in Public Health, 9(December), 1–9. https://doi.org/10.3389/fpubh.2021.728612
- Dineen, T. E., Bean, C., & Jung, M. E. (2022). Implementation of a diabetes prevention program within two community sites: A qualitative assessment. Implementation Science Communications, 3(13), 1–17. https://doi.org/10.1186/s43058-021-00234-6
- Dryden-Palmer, K. D., Parshuram, C. S., & Berta, W. B. (2020). Context, complexity and process in the implementation of evidence-based innovation: A realist informed review. BMC Health Services Research, 20(1), 1–15. https://doi.org/10.1186/s12913-019-4778-6
- Duda, J. L., Williams, G. C., Ntoumanis, N., Daley, A., Eves, F. F., Mutrie, N., Rouse, P. C., Lodhia, R., Blamey, R. V., & Jolly, K. (2014). Effects of a standard provision versus an autonomy supportive exercise referral programme on physical activity, quality of life and well-being indicators: A cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity, 11(1), 1–15. https://doi.org/10.1186/1479-5868-11-1
- Dugdill, L., Graham, R. C., & McNair, F. (2005). Exercise referral: The public health panacea for physical activity promotion? A critical perspective of exercise referral schemes; their development and evaluation. Ergonomics, 48(11-14), 1390–1410. https://doi.org/10.1080/00140130500101544
- Falagas, M. E., Pitsouni, E. I., Malietzis, G. A., & Pappas, G. (2008). Comparison of PubMed, scopus, Web of science, and google scholar: Strengths and weaknesses. The FASEB Journal, 22(2), 338–42. https://doi.org/10.1096/fj.07-9492LSF
- Gagnon, J. C., Fortier, M., McFadden, T., & Plante, Y. (2018). Investigating the behaviour change techniques and motivational interviewing techniques in physical activity counselling sessions. Psychology of Sport and Exercise, 36(August 2017), 90–99. https://doi.org/10.1016/j.psychsport.2018.02.002
- Galbraith, N., Rose, C., & Rose, P. (2021). The roles of motivational interviewing and self-efficacy on outcomes and cost-effectiveness of a community-based exercise intervention for inactive middle-older aged adults. Health and Social Care in the Community, 1–13(April), https://doi.org/10.1111/hsc.13510
- Gallegos-Carrillo, K., García-Peña, C., Salmerón, J., Salgado-de-Snyder, N., & Lobelo, F. (2017). Brief counseling and exercise referral scheme: A pragmatic trial in Mexico. American Journal of Preventive Medicine, 52(2), 249–59. https://doi.org/10.1016/j.amepre.2016.10.021
- Gray, J. (2019). The hazards of a biomedical exercise paradigm: Exploring the praxis of exercise professionals. Philosophies, 4(3), 54. https://doi.org/10.3390/philosophies4030054
- Green, J. (2000). The role of theory in evidence-based health promotion practice. Health Education Research, 15(2), 125–29. https://doi.org/10.1093/her/15.2.125
- Greenhalgh, T. (2018). How to implement evidence based healthcare. Wiley Blackwell.
- Grimmett, C., Bradbury, K., Dalton, S. O., Fecher-Jones, I., Hoedjes, M., Varkonyi-Sepp, J., & Short, C. E. (2021). The role of behavioral science in personalized multimodal prehabilitation in cancer. Frontiers in Psychology, 12(February), https://doi.org/10.3389/fpsyg.2021.634223
- Gustavsson, C., Nordqvist, M., Bröms, K., Jerdén, L., Kallings, L. V., & Wallin, L. (2018). What is required to facilitate implementation of Swedish physical activity on prescription? - interview study with primary healthcare staff and management. BMC Health Services Research, 18(1), 1–11. https://doi.org/10.1186/s12913-018-3021-1
- Hagger, M. S., Moyers, S., McAnally, K., & McKinley, L. E. (2020). Known knowns and known unknowns on behavior change interventions and mechanisms of action*. Health Psychology Review, 14(1), 199–212. https://doi.org/10.1080/17437199.2020.1719184
- Hawkes, R. E., Miles, L. M., Bower, P., Cotterill, S., & French, D. P. (2022). Assessing and ensuring fidelity of the nationally implemented English NHS diabetes prevention programme: Lessons learned for the implementation of large-scale behaviour change programmes. Health Psychology and Behavioral Medicine, 10(1), 498–513. https://doi.org/10.1080/21642850.2022.2077205
- Henderson, H. E., Evans, A. B., Allen-Collinson, J., & Siriwardena, N. A. (2018). The ‘wild and woolly’ world of exercise referral schemes: Contested interpretations of an exercise as medicine programme. Qualitative Research in Sport, Exercise and Health, 10(4), 505–23. https://doi.org/10.1080/2159676X.2017.1352018
- Hoekstra, F., Hettinga, F. J., Breejen, M. D., Duijf, M., Van Der Woude, L. H. V., Dekker, R., & Van Der Schans, C. P. (2017a). Professionals’ perceptions of factors Affecting implementation and continuation of a physical activity promotion programme in rehabilitation: A qualitative study. Journal of Rehabilitation Medicine, 49(5), 385–94. https://doi.org/10.2340/16501977-2220
- Hoekstra, F., van Offenbeek, M. A. G., Dekker, R., Hettinga, F. J., Hoekstra, T., van der Woude, L. H. V., & van der Schans, C. P. (2017b). Implementation fidelity trajectories of a health promotion program in multidisciplinary settings: managing tensions in rehabilitation care. Implementation Science, 12(1), 1–17. https://doi.org/10.1186/s13012-017-0667-8
- James, E. L., Ewald, B. D., Johnson, N. A., Stacey, F. G., Brown, W. J., Holliday, E. G., Jones, M., Yang, F., Hespe, C., & Plotnikoff, R. C. (2017). Referral for expert physical activity counseling: A pragmatic RCT. American Journal of Preventive Medicine, 53(4), 490–99. https://doi.org/10.1016/j.amepre.2017.06.016
- Jones, H., George, K. P., Scott, A., Buckley, J. P., Watson, P. M., Oxborough, D. L., Thijssen, D. H., Graves, L. E., Whyte, G. P., McGregor, G. & Naylor, L. H. (2021). Charter to establish clinical exercise physiology as a recognised allied health profession in the UK: A call to action. BMJ Open Sport & Exercise Medicine, 7(3), 1–7. https://doi.org/10.1136/bmjsem-2021-001158
- Lambert, J. D., Greaves, C. J., Farrand, P., Cross, R., Haase, A. M., & Taylor, A. H. (2017). Assessment of fidelity in individual level behaviour change interventions promoting physical activity among adults: A systematic review. BMC Public Health, 17(1), 1–13. https://doi.org/10.1186/s12889-016-3954-4
- Lobczowska, K., Banik, A., Romaniuk, P., Forberger, S., Kubiak, T., Meshkovska, B., Neumann-Podczaska, A., Kaczmarek, K., Scheidmeir, M., Wendt, J. & Scheller, D. A. (2022). Frameworks for implementation of policies promoting healthy nutrition and physically active lifestyle: Systematic review. International Journal of Behavioral Nutrition and Physical Activity, 19(1), 1–12. https://doi.org/10.1186/s12966-021-01238-0
- Lobelo, F., Stoutenberg, M., & Hutber, A. (2014). The exercise is medicine global health initiative: A 2014 update. British Journal of Sports Medicine, 48(22), 1627–33. https://doi.org/10.1136/bjsports-2013-093080
- Luszczynska, A. (2020). It’s time for effectiveness-implementation hybrid research on behaviour change. Health Psychology Review, 14(1), 188–92. https://doi.org/10.1080/17437199.2019.1707105
- Maiorana, A., Levinger, I., Davison, K., Smart, N., & Coombes, J. (2018). Exercise prescription is not just for medical doctors: The benefits of shared care by physicians and exercise professionals. British Journal of Sports Medicine, 52(13), 879–80. https://doi.org/10.1136/bjsports-2016-096994
- Mazzoni, A. S., Brooke, H. L., Berntsen, S., Nordin, K., & Demmelmaier, I. (2020). Exercise adherence and effect of self-regulatory behavior change techniques in patients undergoing curative cancer treatment: Secondary analysis from the phys-can randomized controlled trial. Integrative Cancer Therapies, 19. https://doi.org/10.1177/1534735420946834
- McEwan, D., Beauchamp, M. R., Kouvousis, C., Ray, C. M., Wyrough, A., & Rhodes, R. E. (2019). Examining the active ingredients of physical activity interventions underpinned by theory versus no stated theory: A meta-analysis. Health Psychology Review, 13(1), 1–17. https://doi.org/10.1080/17437199.2018.1547120
- Moore, G. F., Moore, L., & Murphy, S. (2011). Facilitating adherence to physical activity: Exercise professionals’ experiences of the national exercise referral scheme in Wales. A qualitative study. BMC Public Health, 11(1), 935. https://doi.org/10.1186/1471-2458-11-935
- Moore, G. F., Moore, L., & Murphy, S. (2012). Integration of motivational interviewing into practice in the national exercise referral scheme in Wales: A mixed methods study. Behavioural and Cognitive Psychotherapy, 40(3), 313–30. https://doi.org/10.1017/S1352465811000531
- Moore, G. F., Raisanen, L., Moore, L., Din, N. U., & Murphy, S. (2013). Mixed-method process evaluation of the Welsh national exercise referral scheme. Health Education, 113(6), 476–501. https://doi.org/10.1108/HE-08-2012-0046
- Moore, J., Merchant, Z., Rowlinson, K., McEwan, K., Evison, M., Faulkner, G., Sultan, J., McPhee, J. S., & Steele, J. (2021). Implementing a system-wide cancer prehabilitation programme: The journey of greater Manchester’s ‘Prehab4cancer.’ European Journal of Surgical Oncology, 47(3), 524–32. https://doi.org/10.1016/j.ejso.2020.04.042
- Moore, L., Britten, N., Lydahl, D., Naldemirci, Ö, Elam, M., & Wolf, A. (2017). Barriers and facilitators to the implementation of person-centred care in different healthcare contexts. Scandinavian Journal of Caring Sciences, 31(4), 662–73. https://doi.org/10.1111/scs.12376
- Myers, J., McAuley, P., Lavie, C. J., Despres, J. P., Arena, R., Kokkinos, P., Dontje, M. L. (2015). Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: Their independent and interwoven importance to health status. Progress in Cardiovascular Diseases, 57(4), 306–14. https://doi.org/10.1016/j.pcad.2014.09.011
- National Institute for Health and Care Excellence. (2014). “Physical activity: Exercise referral schemes.” NICE Guideline, no. September 2014: 50.
- O’Brien, M. W., Bray, N. W., Kivell, M. J., & Fowles, J. R. (2021). A scoping review of exercise referral schemes involving qualified exercise professionals in primary health care. Applied Physiology, Nutrition, and Metabolism, 46(9), 1007–18. https://doi.org/10.1139/apnm-2020-1070
- O’Halloran, P. D., Blackstock, F., Shields, N., Holland, A., Iles, R., Kingsley, M., Bernhardt, J., Lannin, N., Morris, M. E., & Taylor, N. F. (2014). Motivational interviewing to increase physical activity in people with chronic health conditions: A systematic review and meta-analysis. Clinical Rehabilitation, 28(12), 1159–71. https://doi.org/10.1177/0269215514536210
- Oliver, E. J., Hanson, C. L., Lindsey, I. A., & Dodd-Reynolds, C. J. (2016). Exercise on referral: Evidence and complexity at the nexus of public health and sport policy. International Journal of Sport Policy and Politics, 8(4), 731–36. https://doi.org/10.1080/19406940.2016.1182048
- O’Shea, O., McCormick, R., Bradley, J. M., & O’Neill, B. (2016). Fidelity review: A scoping review of the methods used to evaluate treatment fidelity in behavioural change interventions. Physical Therapy Reviews, 21(3-6), 207–14. https://doi.org/10.1080/10833196.2016.1261237
- Pavey, T. G., Taylor, A. H., Fox, K. R., Hillsdon, M., Anokye, N., Campbell, J. L., Foster, C., Green, C., Moxham, T., Mutrie, N. & Searle, J. (2011). Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: Systematic review and meta-analysis. BMJ, 343(7831), 980. https://doi.org/10.1136/bmj.d6462
- Prior, F., Coffey, M., Robins, A., & Cook, P. (2019). Long-term health outcomes associated with an exercise referral scheme: An observational longitudinal follow-Up study. Journal of Physical Activity and Health, 16, 288–293. https://doi.org/10.1123/jpah.2018-0442
- Purdy, G. M., Sobierajski, F. M., Dolgoy, N. D., & McNeely, M. L. (2022). Evaluating implementation and pragmatism of cancer-specific exercise programs: A scoping review. Journal of Cancer Survivorship, 16(2), 374–87. https://doi.org/10.1007/s11764-021-01032-8
- Quested, E., Ntoumanis, N., Thøgersen-Ntoumani, C., Hagger, M. S., & Hancox, J. E. (2017). Evaluating quality of implementation in physical activity interventions based on theories of motivation: Current challenges and future directions. International Review of Sport and Exercise Psychology, 10(1), 252–69. https://doi.org/10.1080/1750984X.2016.1217342
- Raposo, F. Z., Sánchez-Oliva, D., Veiga Carraça, E., Labisa Palmeira, A., & Silva, M. N. (2020). The dark side of motivational practices in exercise professionals: Mediators of controlling strategies. International Journal of Environmental Research and Public Health, 17(15), 1–14. https://doi.org/10.3390/ijerph17155377
- Raustorp, A., & Sundberg, C. J. (2014). The evolution of physical activity on prescription (FaR) in Sweden. Schweizerische Zeitschrift Fur Sportmedizin Und Sporttraumatologie, 62(2), 23–25. https://doi.org/10.34045/ssem/2014/10
- Reale, S., Turner, R. R., Sutton, E., Taylor, S. J. C., Bourke, L., Morrissey, D., Brown, J., Rosario, D. J., & Steed, L. (2021). Towards implementing exercise into the prostate cancer care pathway: Development of a theory and evidence-based intervention to train community-based exercise professionals to support change in patient exercise behaviour (The STAMINA trial). BMC Health Services Research, 21(1), https://doi.org/10.1186/s12913-021-06275-w
- Rhodes, R. E., Janssen, I., Bredin, S. S. D., Warburton, D. E. R., & Bauman, A. (2017). Physical activity: Health impact, prevalence, correlates and interventions. Psychology & Health, 32(8), 942–75. https://doi.org/10.1080/08870446.2017.1325486
- Rogers, L. Q., Courneya, K. S., Anton, P. M., Hopkins-Price, P., Verhulst, S., Vicari, S. K., Robbs, R. S., Mocharnuk, R., & McAuley, E. (2015). Effects of the BEAT cancer physical activity behavior change intervention on physical activity, aerobic fitness, and quality of life in breast cancer survivors: A multicenter randomized controlled trial. Breast Cancer Research and Treatment, 149(1), 109–19. https://doi.org/10.1007/s10549-014-3216-z
- Rowley, N., Mann, S., Steele, J., Horton, E., & Jimenez, A. (2018). The effects of exercise referral schemes in the United Kingdom in those with cardiovascular, mental health, and musculoskeletal disorders: A preliminary systematic review. BMC Public Health, 18(1), 1–18. https://doi.org/10.1186/s12889-018-5868-9
- Rowley, N., Steele, J., Mann, S., Jimenez, A., & Horton, E. (2021). Delivery approaches within exercise referral schemes: A survey of current practice in England. Journal of Physical Activity and Health, 18(4), 357–73. https://doi.org/10.1123/jpah.2020-0388
- Sánchez-Oliva, D., Palmeira, A. L., Carraça, E. V., Teixeira, P. J., Markland, D., & Silva, M. N. (2021). Motivational strategies used by exercise professionals: A latent profile analysis. Journal of Physical Activity and Health, 18(8), 895–903. https://doi.org/10.1123/jpah.2020-0338
- Sarkies, M. N., Francis-Auton, E., Long, J. C., Pomare, C., Hardwick, R., & Braithwaite, J. (2022). Making implementation science more real. BMC Medical Research Methodology, 22(1), 1–8. https://doi.org/10.1186/s12874-022-01661-2
- Shore, C. B., Galloway, S. D. R., Gorely, T., & Hunter, A. M. (2022). “Exercise referral instructors’ perspectives on supporting and motivating participants to uptake, attend and adhere to exercise prescription : A qualitative study.”
- Shore, C. B., Hubbard, G., Gorely, T., Hunter, A. M., & Galloway, S. D. (2021). The match between what Is prescribed and reasons for prescribing in exercise referral schemes: A mixed method study. BMC Public Health, 21(1), 1–12. https://doi.org/10.1186/s12889-021-11094-z
- Shore, C. B., Hubbard, G., Gorely, T., Polson, R., Hunter, A., & Galloway, S. D. (2019). Insufficient reporting of factors associated with exercise referral scheme uptake, attendance, and adherence: A systematic review of reviews. Journal of Physical Activity and Health, 1–10. https://doi.org/10.1123/jpah.2018-0341
- Silva, M. N., Sánchez-Oliva, D., Brunet, J., Williams, G. C., Teixeira, P. J., & Palmeira, A. L. (2017). ‘What goes around comes around’: Antecedents, mediators, and consequences of controlling vs. need-supportive motivational strategies used by exercise professionals. Annals of Behavioral Medicine, 51(5), 707–17. https://doi.org/10.1007/s12160-017-9894-0
- Sjöling, M., Lundberg, K., Englund, E., Westman, A., & Jong, M. C. (2011). Effectiveness of motivational interviewing and physical activity on prescription on leisure exercise time in subjects suffering from mild to moderate hypertension. BMC Research Notes, 4(1), 1–7. https://doi.org/10.1186/1756-0500-4-352
- Smith, W., Martin, M., Pisu, M., Oster, R., Qu, H., Shewchuk, R., Sheffield, M., Minter, A., Baumann, A., & Rogers, L. (2021). Promoting physical activity in rural settings: Effectiveness and potential strategies. Translational Journal of the American College of Sports Medicine, 6(4), 1–11. https://journals.lww.com/acsm-tj/Fulltext/2021/10150/Promoting_Physical_Activity_in_Rural_Settings_.13.aspx.
- Sørensen, J. B., Kragstrup, J., Skovgaard, T., & Puggaard, L. (2008). Exercise on prescription: A randomized study on the effect of counseling vs counseling and supervised exercise. Scandinavian Journal of Medicine & Science in Sports, 18(3), 288–97. https://doi.org/10.1111/j.1600-0838.2008.00811.x
- Speake, H., Copeland, R. J., Till, S. H., Breckon, J. D., Haake, S., & Hart, O. (2016). Embedding physical activity in the heart of the NHS: The need for a whole-system approach. Sports Medicine, 46(7), 939–46. https://doi.org/10.1007/s40279-016-0488-y
- Spence, R. R., Sandler, C. X., Singh, B., Tanner, J., Pyke, C., Eakin, E., Vagenas, D., & Hayes, S. C. (2022). A randomised, comparative, effectiveness trial evaluating low-versus high-level supervision of an exercise intervention for women with breast cancer: The SAFE trial. Cancers, 14(6), 1528. https://doi.org/10.3390/cancers14061528
- Stacey, D., Hopkins, M., Adamo, K. B., Shorr, R., & Prud’homme, D. (2010). Knowledge translation to fitness trainers: A systematic review. Implementation Science, 5(1), 1–9. https://doi.org/10.1186/1748-5908-5-1
- Stevens, M., Rees, T., Cruwys, T., & Olive, L. (2022). Equipping physical activity leaders to facilitate behaviour change: An overview, call to action, and roadmap for future research. Sports Medicine - Open, 8(1), https://doi.org/10.1186/s40798-022-00423-0
- Taylor, A. H., Taylor, R. S., Ingram, W. M., Anokye, N., Dean, S., Jolly, K., Mutrie, N., Lambert, J., Yardley, L., Greaves, C. & King, J. (2020). Adding Web-based behavioural support to exercise referral schemes for inactive adults with chronic health conditions: The e-coacher RCT. Health Technology Assessment, 24(63), 1–106. https://doi.org/10.3310/hta24630
- Thompson, W. R., Sallis, R., Joy, E., Jaworski, C. A., Stuhr, R. M., & Trilk, J. L. (2020). Exercise is medicine. American Journal of Lifestyle Medicine, 14(5), 511–23. https://doi.org/10.1177/1559827620912192
- Toms, G., Williams, L., Rycroft-Malone, J., Swales, M., & Feigenbaum, J. (2019). The development and theoretical application of an implementation framework for dialectical behaviour therapy: A critical literature review. Borderline Personality Disorder and Emotion Dysregulation, 6(1), 1–16. https://doi.org/10.1186/s40479-019-0102-7
- Toomey, E., Hardeman, W., Hankonen, N., Byrne, M., McSharry, J., Matvienko-Sikar, K., & Lorencatto, F. (2020). Focusing on fidelity: Narrative review and recommendations for improving intervention fidelity within trials of health behaviour change interventions. Health Psychology and Behavioral Medicine, 8(1), 132–51. https://doi.org/10.1080/21642850.2020.1738935
- Toronto, C. E., & Remington, R. (2020). A step-by-step guide to conducting an integrative review. A step-by-step guide to conducting an integrative review. https://doi.org/10.1007/978-3-030-37504-1.
- Whittemore, R., & Knafl, K. (2005). The integrative review: Updated methodology robin. Methodological Issues in Nursing Research, 9(SUPPL), 11–21. https://doi.org/10.1016/j.pmn.2007.11.006
- Williamson, W., Kluzek, S., Roberts, N., Richards, J., Arden, N., Leeson, P., Newton, J., & Foster, C. (2015). Behavioural physical activity interventions in participants with lower-limb osteoarthritis: A systematic review with meta-analysis. BMJ Open, 5(8), e007642. https://doi.org/10.1136/bmjopen-2015-007642
- Wood, C. J., Barton, J., & Smyth, N. (2022). A cross-sectional study of physical activity behaviour and associations with wellbeing during the UK coronavirus lockdown. Journal of Health Psychology, 27(6), 1432–44. https://doi.org/10.1177/1359105321999710
- Wurz, A., Bean, C., Shaikh, M., Culos-Reed, S. N., & Jung, M. E. (2021). From laboratory to community: Three examples of moving evidence-based physical activity into practice in Canada. Health and Social Care in the Community, 1–11(August), https://doi.org/10.1111/hsc.13596
- Yang, H. J., Chen, K. M., Chen, M. D., Wu, H. C., Chang, W. J., Wang, Y. C., & Huang, H. T. (2015). Applying the transtheoretical model to promote functional fitness of community older adults participating in elastic band exercises. Journal of Advanced Nursing, 71(10), 2338–49. doi:10.1111/jan.12705
