ABSTRACT
Introduction
The aim of this study was to evaluate the German falls prevention program ‘Staying safe and active in old age – falls prevention’, which is already established in practice.
Methods
The single-arm intervention study consisted of two time points, 6 months apart, to evaluate the multifactorial falls prevention program (n = 125 at Time 2). We observed the groups and their trainers and assessed which behavior change techniques (BCTs) were used. According to our evaluation framework, changes in the following three domains were assessed: (a) fall-related variables (i.e. number of falls, fear of falling), (b) physical functioning (i.e. performance-based gait speed, coordination, self-reported leg strength, balance, as well as habitual execution of the exercises), and (c) psychosocial functioning (i.e. quality of life, activities of daily living, mobility, and loneliness). Linear mixed models were used to determine changes in each variable.
Results
Demonstration of behavior was the most frequently used BCT. The program showed significant benefits for fear of falling, balance, coordination, habitual execution, and loneliness over time (Cohen’s d between −0.59 and 1.73). Number of falls, gait speed, coordination (dual task), activities of daily living, and quality of life were maintained (Cohen’s d between −0.26 and 0.30), whereas leg strength and mobility decreased significantly at Time 2 (Cohen’s d = −0.55 and −0.36).
Discussion
Group-based falls prevention programs may facilitate social integration among older adults and may also enhance and maintain physical functioning in old age.
Trial registration: German Clinical Trials Register identifier: DRKS00012321.
Introduction
As a result of demographic changes, the large-scale implementation of falls prevention programs will become increasingly important and is a critical global challenge (e.g. dos Santos et al., Citation2021; Montero-Odasso et al., Citation2022). To prevent falls in older adults, it is important to address age-related declines in physical functioning, particularly, balance and muscle strength (Sherrington et al., Citation2019). Although some programs have been successfully implemented into practice and are an integral part of the German healthcare system, evaluation of these programs has not been a research priority. The aim of this study was, therefore, to evaluate the group-based, outpatient falls prevention program ‘Staying safe and active in old age – falls prevention’, which is already established in German health care practice. The original development by an interprofessional team from the German health insurance company AOK Nordost (statutory health insurance for the northeastern parts of Germany) was not theory-based or strictly guided by a specific intervention framework (e.g. Intervention Mapping), but rather based on existing evidence on falls prevention, expert consensus, and best practice principles. The falls prevention program, which has been in place since 2010, aims to prevent falls through targeted physical exercise (i.e. balance, strength, and coordination with cognitive exercises), in order to enable mobility and promote independence in old age. In this program, older adults exercise together as a group – at least once a week – under the guidance of a qualified volunteer or full-time exercise instructor, usually in a meeting place in their neighborhood (a few in residential care homes). In addition, the program is free of charge (even without being a member of the health insurance company) and is set up for the long-term (i.e. there is no time limit for participation).
The aim of the present study was to conduct a process and outcome evaluation of the falls prevention program. As part of the process evaluation, the behavior change techniques (Michie et al., Citation2013; Fleig et al., Citation2024) used by the instructors were evaluated. A behavior change technique (BCT) is hereby defined as ‘an observable, replicable, and irreducible component of an intervention designed to alter or redirect causal processes that regulate behavior’ (Michie et al., Citation2013, p. 4). We also evaluated the program’s within-subject effect on fall-related variables, objective, and subjective physical functioning, as well as psychosocial functioning.
Materials and methods
Intervention
The majority of the weekly lessons consist of balance exercises designed to improve the perception and processing of challenging environmental situations (e.g. standing on one leg). The strength exercises last about 15 minutes and are aimed at promoting the ability to compensate in situations where there is a high risk of falling. Each session ends with playful elements to practice the coordination of physical and cognitive skills (e.g. throwing a ball and counting backwards). Sessions last a minimum of 60 minutes. Instructors are staff members of the meeting places (or in a few instances, employees of the residential care homes where the program takes place), and undergo a comprehensive training program by the health insurance company before leading a group.
Design and procedure
The health insurance company provided contact information for meeting places and residential care homes that run the program on their behalf. To participate in the study, older adults were required to sign an informed consent form. Ethical approval was obtained from the Department of Education and Psychology of the Freie Universität Berlin (number 165/2017). Detailed information and pre-registration data are available through the German Clinical Trials Register (www.drks.de; ID = DRKS00012321).
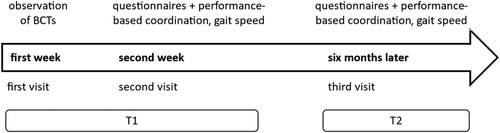
As shown in , the longitudinal design consisted of two time points, 6 months apart. Data from observations (22 out of 34 groups gave us permission to observe the training), questionnaires and performance-based measures (n = 34) were collected by research assistants between October 2017 and January 2019 (Time 1, T1) and between July 2018 and July 2019 (Time 2, T2), respectively.
Figure 1. Measurement points of the longitudinal study to evaluate the falls prevention program.
Note: BCTs = behavior change techniques, T1 = Time 1, T2 = Time 2.
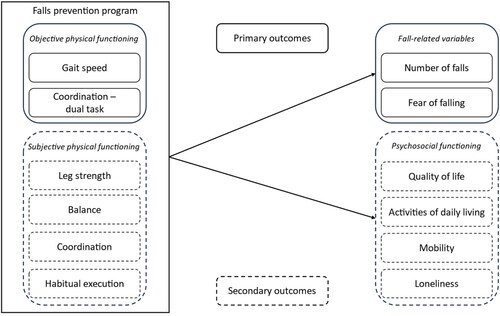
illustrates the evaluation framework. Efficacy was assessed using three criteria: (1) fall-related variables, (2) physical functioning, and (3) psychosocial functioning.
Measures
Two trained researchers independently observed 22 groups and their instructors, using a German translation (Fleig et al., Citation2024) of the standard behavior change taxonomy by Michie et al. (Citation2013). This taxonomy aims to systematically and reliably identify the content of behavior change interventions in 93 distinct BCTs (Michie et al., Citation2013). Techniques were coded as either absent or present (i.e. dichotomous coding). In addition, the participants’ enjoyment of the falls prevention program was assessed using the Physical activity enjoyment scale (Kendzierski & DeCarlo, Citation1991) at T1. Here, participants were asked to reflect on the previous group sessions and rate 11 items, each with two poles (e.g. ‘It’s a lot of fun – It’s no fun at all.’) on a seven-point scale.
The following constructs were assessed at both time points. Based on our evaluation framework (), fall-related variables were measured by the number of falls and fear of falling. The number of falls was assessed with the following question: ‘How many times have you fallen in the past 6 months?’. In addition, fear of falling was measured with two instruments. The following two items: ‘Have you been afraid that you might fall?’ and ‘Did you limit your activities at home or outside because you were afraid of falling?’ (based on Friedman et al., Citation2002) were rated on a 6-point scale ranging from (almost) never (1) to (almost) always (5). The correlation between the two items was .82 at T1 and .85 at T2. Fear of falling was also assessed using the German version of the Falls Efficacy Scale (Dias et al., Citation2006), in which participants rated 16 activities of daily living (e.g. cleaning the house, walking outside) in terms of their fear of falling during performance. The response scale ranged from not at all concerned (1) to very concerned (4) (total score ranging from 16-64). Internal consistency was excellent in this study (Cronbach’s αT1 = .92, αT2 = .92).
Figure 2. Framework for quantitative evaluation of outcomes.
Physical functioning was measured objectively by gait speed and coordination (dual task) using the Walking While Talking Test (WWT; Verghese et al., Citation2002). Research assistants timed older adults walking a standardized distance at their daily gait speed. The total walking distance was 5 meters, with only 3 meters being timed to avoid lower gait speeds at the start and end points. Gait speed (single task) was calculated in meters per second (m/s). Accordingly, higher levels of gait speed imply a shorter time to walk the distance. Verghese et al. (Citation2002) showed an interrater reliability of the WWT of r = .60. Objectively measured coordination was assessed in a dual-task condition, in which participants counted backwards from a given number by three while walking the same distance (adapted from Schwenk et al., Citation2010). The coordination (dual task) was calculated using the following formula: (dual task – single task)/single task x 100. Thus, high percentages indicate high costs of divided attention (Schwenk et al., Citation2010). Furthermore, we collected self-reports on leg strength, balance, coordination, and habitual execution. Leg strength and balance were measured with the two self-developed questions ‘How would you estimate your leg strength/balance?’. Participants rated their responses on a 6-point scale, ranging from very weak (0) to very strong (6). Self-reported coordination was assessed with the motor function status questionnaire (FFB-Mot; Bös et al., Citation2002). We used four items of the coordination subscale, which were rated on a 5-point scale from I cannot do this activity (1) to I have no problems (5). Internal consistency was acceptable in our sample (αT1 = .77, αT2 = .78). To measure habitual execution, a scale by Phillips and Gardner (Citation2016) was adapted to the target behavior and translated into German. Participants rated the four items on a 6-point scale ranging from strongly disagree (1) to strongly agree (6). The items showed a good to acceptable internal consistency in our study (αT1 = .83, αT2 = .68).
Psychosocial functioning was measured by self-reported quality of life, activities of daily living, mobility, and loneliness. We measured quality of life using the single index value of the EQ-5D (Rabin & de Charro, Citation2001), which consists of the following five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Participants rated each dimension on five levels ranging from no problems (1) to extreme problems (5). The index score comprised values from 0 to 1, with higher scores indicating higher reported quality of life. The results of a review by Haywood et al. (Citation2005) revealed good reliability and validity of the EQ-5D for older adults. Activities of daily living were assessed with a subscale of the German version of the SF-36 (Bullinger et al., Citation1995). Participants rated 10 items on a 3-point scale, ranging from not at all (1) to slightly limited (2) to strong (3), to assess whether they are restricted in their activities by their current state of health. Internal consistencies were good to excellent in our sample (αT1 = .93, αT2 = .88). To measure mobility in old age, four items of the Life Space Questionnaire (Stalvey et al., Citation1999) were answered with two response options (no (0), yes (1)). In our sample, the internal consistency was .93 at T1 and .88 at T2. Finally, we assessed loneliness with the De Jong Gierveld short scales for emotional and social loneliness (De Jong Gierveld & Van Tilburg, Citation2010). The six items were answered by the participants on a 3-point scale from no (1) to more or less (2) to yes (3) and showed acceptable consistencies at both measurement points (αT1 = .69, αT2 = .73).
Statistical analysis
Drop-out analyzes were calculated for all included measures. T-tests revealed differences in mobility between older adults who discontinued participation and those who remained in the study. Participants who dropped out reported a higher mobility score at T1 (Mean = 3.47, MeanDrop-out = 3.80, t(55.15) = 2.45, p = .009). Reasons for withdrawal were hospital admission, major health problems, time constraints, and vacation. Linear mixed models were set up for each outcome measure using the lme4 package in R (version 4.2.2). The reported p values are one-tailed.
Results
Sample
Study participants were individuals participating in the group-based prevention program ‘Staying safe and active in old age – falls prevention’. On average, individuals had already been engaged in their groups for 2 years and 3 months (SD = 1 year and 11 months) before our data collection began. We excluded six residential care homes from further data analysis due to instructors reporting that group members were diagnosed with moderate to severe dementia (preventing them from filling in self-reports). In total, 34 training groups from 26 institutions participated in the study, of which 20 were meeting places for older adults and six were residential care homes. In total, 22 out of 34groups gave us permission to observe their groups during training. The number of participants in the groups ranged from 2 in residential settings to 20 in community settings. A total of N = 174 participants completed the T1 questionnaire. Of these, n = 125 participants answered the follow-up questionnaire (72% of T1; main reasons for drop-out: not present at T2 training session due to health issues or vacation). The mean age at T1 was 76 years (M = 75.99, SD = 7.11, min = 51 max = 93). Almost two-thirds lived alone (60%) and were single or widowed (62%). Participants were predominantly female (86%) and rated their perceived health status as good (M = 70.50, SD = 18.81). On average, participants reported enjoying the training (M = 4.99, SD = 1.22).
Descriptive statistics
presents bivariate correlations of primary and secondary outcomes that revealed small to strong associations. Mean values and standard deviations are displayed in .
Table 1. Bivariate correlations in the longitudinal sample (n = 125).
Table 2. Effects on primary and secondary outcomes over 6 months.
Ratings and description of intervention content
We calculated Cohen’s Kappa statistic to estimate the inter-rater reliability of identified BCTs used within the intervention. Overall, ϰ indicated moderate to substantial agreement between the raters (0.54 −1.0; Landis & Koch, Citation1977). presents the identified BCTs. Of the 93 BCTs, 32 techniques were identified at least once within the included falls prevention groups. The majority of the BCTs identified belonged to the clusters feedback and monitoring, comparison of behavior, and social support (see ). Exercise sessions were complex, so the number of identified techniques per group ranged from 1 to 14 (median [p25, p75] = 5 [2, 8] BCTs/group). The most popular single BCTs were the demonstration of behavior, feedback on behavior, and instruction on how to perform the behavior.
Table 3. Identified behavior change techniques used by instructors across all observed falls prevention groups (n = 22).
Linear mixed models
displays the results of the linear mixed models. Regarding the primary outcomes, total scores of fear of falling decreased from T1 to T2. In contrast, total scores for objectively measured gait speed and coordination (dual task), as well as mean scores for self-reported number of falls and the Falls Efficacy Scale, did not show changes. Concerning secondary outcomes, participants self-reported an increase in balance and coordination over time, whereas subjective leg strength decreased. In addition, there was a significant increase in habitual execution. As shown in , the total scores for quality of life and activities of daily living did not show significant differences between measurement points. Although a decrease in mobility was reported, older adults reported feeling less lonely at follow-up in comparison to T1.
Discussion
In this mixed-methods study, we aimed to evaluate a group-based outpatient falls prevention program designed to promote mobility and independence in old age. In particular, we explored the use of behavior change techniques used by the group instructors through observation and evaluated changes in fall-related variables, physical, and psychosocial functioning. Our results showed that the most frequently used BCTs were demonstration of exercises, instruction on how to perform the behavior and providing feedback on the behavior. Regarding the primary outcomes, participants reported a reduced fear of falling at follow-up. However, there were no differences in mean values for self-reported number of falls, objectively measured gait speed, and coordination (dual task). Secondary outcomes showed an increase in self-reported balance and coordination over time. Both effect sizes can be considered large. Furthermore, there was an increase of medium effect size in habitual execution. In contrast, there was a self-reported decrease in leg strength and mobility. In terms of psychosocial outcomes, activities of daily living remained stable, and quality of life increased slightly. Participants also reported a decrease in loneliness at T2.
Results concerning behavior change techniques
Group instructors most often used behavior change techniques that focused on motivating older adults to perform specific exercises during the exercise sessions or providing adviceon how to execute the exercises correctly. BCTs aimed directly at motivating and empowering individuals to incorporate exercises into their daily lives were not used (e.g. action planning). One limitation of the ‘Staying safe and active in old age – falls prevention’ program is that it does not – in its current version – support older adults in integrating functional exercises into daily life. Previous research has shown that an ‘integrated lifestyle approach’, which encourages individuals to incorporate simple balance and strengthening exercises (e.g. one-legged stance) into their daily routines (e.g. brushing their teeth) (e.g. Clemson et al., Citation2012; Fleig et al., Citation2016; Kramer and Labudek et al., Citation2020; Labudek et al., Citation2023), can successfully reduce fall rates (Jansen et al., Citation2021). Such an approach, although limited in time (e.g. usually 21 weeks), would be an ideal addition to maximize the impact of the current program.
Quantitative evaluation of outcomes
The number of falls was maintained from T1 to T2, which can be positively interpreted for a falls prevention program, as falls usually increase with age (e.g. Kaveh et al., Citation2021; Sherrington et al., Citation2019). These results are consistent with those of a meta-analysis of multifactorial interventions in which Morris et al. (Citation2022) also found a trend toward reduced rates of falls. In our study, fear of falling was measured through the Falls Efficacy Scale (Dias et al., Citation2006) and through the following two items: ‘Have you been afraid that you might fall?’ and ‘Did you limit your activities at home or outside because you were afraid of falling?’ (based on Friedman et al., Citation2002). The means of the two items from Friedman et al. (Citation2002) revealed a significant reduction in fear of falling, which is consistent with the results of a study by Jansen et al. (Citation2021). Although the means of the Falls Efficacy Scale (Dias et al., Citation2006) showed the same trend, the difference was not statistically significant. In our sample, the two instruments were correlated strongly between both measurement points. The terms fear of falling and falls efficacy are often used interchangeably in the current literature (e.g. Kumar et al., Citation2016; Wu et al., Citation2020). However, some authors argue that these two constructs should be distinguished (Adamczewska & Nyman, Citation2018; Hadjistavropoulos et al., Citation2011). The term ‘falls efficacy’ is problematic because it implies a close relation to, or equation with, self-efficacy. Self-efficacy describes the subjective belief that one can perform activities of daily living, despite challenges (e.g. increased risk of falling). In terms of content, the German version of the Falls Efficacy Scale (Dias et al., Citation2006) measures risk perception and not self-efficacy, for example, see question ‘How concerned are you about the possibility of falling when performing one of the following activities?’ (e.g. cleaning the house, walking outside). From a health psychology perspective, the Falls Efficacy Scale is not optimal for assessing fear of falling. Instead of a general fear to fall in the sense of a perception of a risk, these items rather depict concerns about falling during specific everyday activities. As fear of falling can also be a barrier to participation in falls prevention programs (e.g. black ice; Nilsson et al., Citation2020), digital formats may offer a solution (Camicioli et al., Citation2023). However, it remains questionable whether the psychosocial benefits (e.g. reduction of loneliness) remain.
Given that this is an ongoing falls prevention program, it is notable that small to large effects on physical functioning could be observed. Both self-reported balance and coordination increased over time. The ‘world guidelines for falls prevention and management for older adults’ suggest that falls prevention programs for older adults should include functional and challenging balance exercises and should take place at least three times a week over a period of at least 12 weeks (Montero-Odasso et al., Citation2022). It is noteworthy that our sample reported a significant improvement in balance ability even though they only trained once a week. This may be due to the to the prolonged training period (M = 2 years and 3 months). Participants also reported an increase in habitual execution, indicating a higher degree of automated performance of the exercises during the training sessions. However, self-reported leg strength decreased significantly over time, which may be age-related. As mentioned above, constant values for objectively measured gait speed and coordination (dual task) can be seen as positive against the background of the sample’s age. It is interesting to note that self-reported coordination increased over time, while objectively measured coordination (dual task) remained constant. A closer look at the measures reveals that the items on the motor function status questionnaire depict the coordination of physical abilities, whereas the dual task measures capture the simultaneous coordination of physical and cognitive abilities.
Regarding psychosocial functioning, there was a medium-sized increase in quality of life. The results are in line with a study by Iglesias et al. (Citation2009), which suggests that falls prevention programs offer a cost-effective approach to promoting, or at least maintaining, quality of life in old age. In the current evaluation study, no significant differences in activities of daily living were observed. However, participants self-reported a decrease in mobility. Interestingly, participation in this group-based falls prevention program showed a positive effect on loneliness. Our results are in line with findings by Gellert et al. (Citation2012), indicating that affective outcome expectancies (anticipation of emotional and well-being benefits), as opposed to health outcome expectancies (anticipation of effects on physical health), predict physical exercise among older adults 6 months later. In a qualitative study, health care professionals described falls prevention programs as places where they can share experiences and learn from each other (Heng et al., Citation2021). Older adults often face reduced social contacts due to retirement, lower mobility, fewer opportunities to visit others, or even the death of significant persons in their social network. Participation in group-based exercise programs may provide secondary opportunities to compensate for these losses and to foster new and lasting relationships. For instance, Whaley (Citation2018) emphasizes the need to promote shared social identities in group-based prevention programs to increase physical activity in older age. This may be specifically most important for older adults, who are less socially integrated (Steckhan et al., Citation2022).
Strengths and limitations
A strength of this evaluation study is that both self-reported and objectively measured indicators for physical functioning were considered. The inclusion of both older adults in residential care homes as well as community-dwelling older adults provided a broad picture of the aging population, increasing the generalizability of the findings. The ‘world guidelines for falls prevention and management for older adults’ emphasize the importance for falls prevention, particularly in residential care homes and hospitals, where all residents should be regarded at high risk of falling (Montero-Odasso et al., Citation2022). However, current research shows that time constraints for health care professionals represent a barrier to implementation in the hospital setting (Heng et al., Citation2022). Given the shortage of professionals in Germany, outpatient falls prevention programs may be a good option for early prevention.
Nevertheless, there are also limitations to our study. Ideally, each participant would have been assessed before starting the program and followed up for a longer period of time. As this falls prevention program has been in place since 2010, and this study only covered a 6-month period, the effects over time may have been underestimated. An additional major limitation of this study is the lack of a randomized control group. We can therefore not compare the program’s effects against a similar group that might have shown age-related decline. Moreover, the attrition rate in the objectively measured variables of gait speed and coordination (dual task) was rather high. In the case of absence due to illness or vacation, questionnaires could be sent by mail, but repeated performance-based measurement was not feasible.
Conclusion
This article is not a typical intervention evaluation, but rather illustrates how best-practice programs can be evaluated while they are being implemented. Our study also highlights how practice and applied behavioral science can benefit from one another. The results of our one-arm intervention study indicate that the ‘Staying safe and active in old age – falls prevention program’ was able to maintain or even increase a number of health indicators in old age. Our findings suggest that the cost-free outpatient falls prevention program, which was implemented into practice by a German health insurance company, can be recommended for wider implementation.
Ethics statement
To participate in the study, older adults had to sign an informed consent form. Ethical approval was obtained from the Department of Education and Psychology of the Freie Universität Berlin (number 165/2017). Detailed information and pre-registration data are available at the German Clinical Trials Register (www.drks.de; ID = DRKS00012321).
Author contribution
Greta M. Steckhan: conception & design, analysis & interpretation of the data, drafting the paper. Lisa M. Warner: conception & design, revising & supervision. Lena Fleig: conception & design, revising & supervision.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data cannot be made available as the rights lie with the health insurance company.
Additional information
Funding
References
- Adamczewska, N., & Nyman, S. R. (2018). A new approach to fear of falls from connections with the posttraumatic stress disorder literature. Gerontology and Geriatric Medicine, 4, 233372141879623–7. https://doi.org/10.1177/2333721418796238
- Bös, K., Abel, T., Woll, A., Niemann, S., Schott, N., & Tittlbach, S. (2002). Der Fragebogen zur Erfassung des motorischen Funktionsstatus (FFB-Mot). Diagnostica, 48(2), 101–111. https://doi.org/10.1026//0012-1924.48.2.101
- Bullinger, M., Kirchberger, I., & Ware, J. (1995). Der deutsche SF-36 Health Survey Übersetzung und psychometrische Testung eines krankheitsübergreifenden Instruments zur Erfassung der gesundheitsbezogenen Lebensqualität. Journal of Public Health, 3(1), 21–36. https://doi.org/10.1007/BF02959944
- Camicioli, R., Morris, M. E., Pieruccini-Faria, F., Montero-Odasso, M., Son, S., Buzaglo, D., Hausdorff, J. M., & Nieuwboer, A. (2023). Prevention of falls in Parkinson's disease: Guidelines and gaps. Movement Disorders Clinical Practice, 10(10), 1459–1469. https://doi.org/10.1002/mdc3.13860
- Clemson, L., Fiatarone Singh, M. A., Bundy, A., Cumming, R. G., Manollaras, K., O’Loughlin, P., & Black, D. (2012). Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): Randomised parallel trial. BMJ, e4547–e4547. https://doi.org/10.1136/bmj.e4547
- De Jong Gierveld, J., & Van Tilburg, T. (2010). The De Jong Gierveld short scales for emotional and social loneliness: tested on data from 7 countries in the UN generations and gender surveys. European Journal of Ageing, 7(2), 121–130. https://doi.org/10.1007/s10433-010-0144-6
- Dias, N., Kempen, G. I. J. M., Todd, C. J., Beyer, N., Freiberger, E., Piot-Ziegler, C., Yardley, L., & Hauer, K. (2006). Die deutsche version der falls efficacy scale-international version (FES-I). Zeitschrift für Gerontologie und Geriatrie, 39(4), 297–300. https://doi.org/10.1007/s00391-006-0400-8
- dos Santos, R. B., Lago, G. N., Jencius, M. C., Barbosa, B. A., Lima, C. A., Paschoal, S. M., Hill, K. D., Leme, L. E. G., & Perracini, M. R. (2021). Antioxidant effect of Resveratrol: Change in MAPK cell signaling pathway during the aging process. Archives of Gerontology and Geriatrics, 92, 104266–9. https://doi.org/10.1016/j.archger.2020.104266
- Fleig, L., Labudek, S. E., & Warner, L. M. (2024, March 1). Verhalten ändern, aber wie? Eine Übersicht für Praxis und Wissenschaft I Eine deutsche Übersetzung der Taxonomie der Techniken der Verhaltensänderung Version 1 von Michie et al. (2013). Retrieved from: osf.io/w4pqh.
- Fleig, L., McAllister, M. M., Chen, P., Iverson, J., Milne, K., McKay, H. A., Clemson, L., & Ashe, M. C. (2016). Health behaviour change theory meets falls prevention: Feasibility of a habit-based balance and strength exercise intervention for older adults. Psychology of Sport and Exercise, 22, 114–122. https://doi.org/10.1016/j.psychsport.2015.07.002
- Friedman, S. M., Munoz, B., West, S. K., Rubin, G. S., & Fried, L. P. (2002). Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. Journal of the American Geriatrics Society, 50(8), 1329–1335. https://doi.org/10.1046/j.1532-5415.2002.50352.x
- Gellert, P., Ziegelmann, J. P., Lippke, S., & Schwarzer, R. (2012). Affective and health-related outcome expectancies for physical activity in older adults. Psychology & Health, 27(7), 816–828. https://doi.org/10.1080/08870446.2011.607236
- Hadjistavropoulos, T., Delbaere, K., & Fitzgerald, T. D. (2011). Reconceptualizing the role of fear of falling and balance confidence in fall risk. Journal of Aging and Health, 23(1), 3–23. https://doi.org/10.1177/0898264310378039
- Haywood, K. L., Garratt, A. M., & Fitzpatrick, R. (2005). Quality of life in older people: A structured review of generic self-assessed health instruments. Quality of Life Research, 14(7), 1651–1668. https://doi.org/10.1007/s11136-005-1743-0
- Heng, H., Kiegaldie, D., Slade, S. C., Jazayeri, D., Shaw, L., Knight, M., Jones, C., Hill, A. M., & Morris, M. E. (2022). Healthcare professional perspectives on barriers and enablers to falls prevention education: A qualitative study. PLoS One, 17(4), e0266797. https://doi.org/10.1371/journal.pone.0266797
- Heng, H., Slade, S. C., Jazayeri, D., Jones, C., Hill, A. M., Kiegaldie, D., Shorr, R. I., & Morris, M. E. (2021). Patient perspectives on hospital falls prevention education. Frontiers in Public Health, 9, 592440. https://doi.org/10.3389/fpubh.2021.592440
- Honaker, J. A., & Kretschmer, L. W. (2014). Impact of fear of falling for patients and caregivers: Perceptions before and after participation in vestibular and balance rehabilitation therapy. American Journal of Audiology, 23(1), 20–33. https://doi.org/10.1044/1059-0889(2013/12-0074)
- Iglesias, C. P., Manca, A., & Torgerson, D. J. (2009). The health-related quality of life and cost implications of falls in elderly women. Osteoporosis International, 20(6), 869–878. https://doi.org/10.1007/s00198-008-0753-5
- Jansen, C.-P., Nerz, C., Labudek, S., Gottschalk, S., Kramer-Gmeiner, F., Klenk, J., Dams, J., König, H.-H., Clemson, L., Becker, C., & Schwenk, M. (2021). Lifestyle-integrated functional exercise to prevent falls and promote physical activity: results from the LiFE-is-LiFE randomized non-inferiority trial. International Journal of Behavioral Nutrition and Physical Activity, 18(115), 1–12. https://doi.org/10.1186/s12966-021-01190-z
- Kaveh, M. H., Bahadori, F., Doosti, A., & Asadollahi, A. (2021). The effect of balance exercise training on balance status, and quality of life in elderly women: A randomized controlled trial. Malaysian Journal of Medicine and Health Sciences, 17(2), 129–136.
- Kendzierski, D., & DeCarlo, K. J. (1991). Physical activity enjoyment scale: Two validation studies. Journal of Sport and Exercise Psychology, 13(1), 50–64. https://doi.org/10.1123/jsep.13.1.50
- Kramer, F., Labudek, S., Jansen, C.-P., Nerz, C., Fleig, L., Clemson, L., Becker, C., & Schwenk, M. (2020). Development of a conceptual framework for a group-based format of the Lifestyle-integrated Functional Exercise (gLiFE) programme and its initial feasibility testing. Pilot and Feasibility Studies, 6(6), 1–18. https://doi.org/10.1186/s40814-019-0539-x
- Kumar, A., Delbaere, K., Zijlstra, G. A. R., Carpenter, H., Iliffe, S., Masud, T., Skelton, D., Morris, R., & Kendrick, D. (2016). Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and meta-analysis. Age and Ageing, 45(3), 345–352. https://doi.org/10.1093/ageing/afw036
- Labudek, S., Fleig, L., Jansen, C.-P., Kramer-Gmeiner, F., Nerz, C., Clemson, L., Klenk, J., Becker, C., & Schwenk, M. (2023). Changes in psychological determinants of behavior change after individual versus group-based lifestyle-integrated fall prevention: Results from the LiFE-is-LiFE trial. Gerontology, 69(2), 212–226. https://doi.org/10.1159/000524701
- Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. https://doi.org/10.2307/2529310
- Liu, M., Hou, T., Li, Y., Sun, X., Szanton, S. L., Clemson, L., & Davidson, P. M. (2021). Fear of falling is as important as multiple previous falls in terms of limiting daily activities: a longitudinal study. BMC Geriatrics, 21(1), 1–17. https://doi.org/10.1186/s12877-021-02305-8
- Merchant, R. A., Chen, M. Z., Wong, B. L. L., Ng, S. E., Shirooka, H., Lim, J. Y., Sandrasageran, S., & Morley, J. E. (2020). Relationship between fear of falling, fear-related activity restriction, frailty, and sarcopenia. Journal of the American Geriatrics Society, 68(11), 2602–2608. https://doi.org/10.1111/jgs.16719
- Michie, S., Richardson, M., Johnston, M., Abraham, C., Francis, J., Hardeman, W., Eccles, M. P., Cane, J., & Wood, C. E. (2013). The Behavior Change Technique Taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. https://doi.org/10.1007/s12160-013-9486-6
- Montero-Odasso, M., Van Der Velde, N., Martin, F. C., Petrovic, M., Tan, M. P., Ryg, J., Aguilar-Navarro, S., Alexander, N. B., Becker, C., Blain, H., Bourke, R., Cameron, I. D., Camicioli, R., Clemson, L., Close, J., Delbaere, K., Duan, L., Duque, G., Dyer, S. M., & Freiberger, A. (2022). World guidelines for falls prevention and management for older adults: a global initiative. Age and Ageing, 51. https://doi.org/10.1093/ageing/afac205
- Morris, M. E., Webster, K., Jones, C., Hill, A.-M., Haines, T., McPhail, S., Kiegaldie, D., Slade, S., Jazayeri, D., Heng, H., Shorr, R., Carey, L., Barker, A., & Cameron, L. (2022). Interventions to reduce falls in hospitals: a systematic review and meta-analysis. Age and Ageing, 51. https://doi.org/10.1093/ageing/afac077
- Nilsson, M. H., Jonasson, S. B., & Zijlstra, G. A. R. (2020). Predictive factors of fall-related activity avoidance in people with Parkinson disease—A longitudinal study With a 3-year follow-up. Journal of Neurologic Physical Therapy, 44(3), 188–194. https://doi.org/10.1097/NPT.0000000000000316
- Pereira, C., Bravo, J., Raimundo, A., Tomas-Carus, P., Mendes, F., & Baptista, F. (2020). Risk for physical dependence in community-dwelling older adults: The role of fear of falling, falls and fall-related injuries. International Journal of Older People Nursing, 15(3), 1–13. https://doi.org/10.1111/opn.12310
- Phillips, L. A., & Gardner, B. (2016). Habitual exercise instigation (vs. execution) predicts healthy adults’ exercise frequency. Health Psychology, 35(1), 69–77. https://doi.org/10.1037/hea0000249
- Rabin, R., & de Charro, F. (2001). EQ-SD: a measure of health status from the EuroQol Group. Annals of Medicine, 33(5), 337–343. https://doi.org/10.3109/07853890109002087
- Schwenk, M., Zieschang, T., Oster, P., & Hauer, K. (2010). Dual-task performances can be improved in patients with dementia. Neurology, 74(24), 1961–1968. https://doi.org/10.1212/WNL.0b013e3181e39696
- Sherrington, C., Fairhall, N. J., Wallbank, G. K., Tiedemann, A., Michaleff, Z. A., Howard, K., Clemson, L., Hopewell, S., & Lamb, S. E. (2019). Exercise for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews, 2019(1), 1–3. https://doi.org/10.1002/14651858.CD012424.pub2
- Stalvey, B. T., Owsley, C., Sloane, M. E., & Ball, K. (1999). The Life Space Questionnaire: A measure of the extent of mobility of older adults. Journal of Applied Gerontology, 18(4), 460–478. https://doi.org/10.1177/073346489901800404
- Steckhan, G. M., Warner, L. M., & Fleig, L. (2022). Preventing falls together: Social identification matters for engaging older adults in a group-based exercise program. Activities, Adaptation & Aging, 46(1), 31–45. https://doi.org/10.1080/01924788.2020.1871540
- Verghese, J., Buschke, H., Viola, L., Katz, M., Hall, C., Kuslansky, G., & Lipton, R. (2002). Validity of divided attention tasks in predicting falls in older individuals: A preliminary study. Journal of the American Geriatrics Society, 50(9), 1572–1576. https://doi.org/10.1046/j.1532-5415.2002.50415.x
- Whaley, D. E. (2018). Social relationships and promoting physical activity among older people. The Palgrave Handbook of Ageing and Physical Activity Promotion, 317–335.
- Whipple, M. O., Hamel, A. V., & Talley, K. M. C. (2018). Fear of falling among community-dwelling older adults: A scoping review to identify effective evidence-based interventions. Geriatric Nursing, 39(2), 170–177. https://doi.org/10.1016/j.gerinurse.2017.08.005
- Wu, S. Y. F., Brown, T., & Yu, M.-l. (2020). Older Adults’ psychosocial responses to a fear of falling: A scoping review to inform occupational therapy practice. Occupational Therapy in Mental Health, 36(3), 207–243. https://doi.org/10.1080/0164212X.2020.1735977
