ABSTRACT
Background
As the recognition of psychological factors in chronic illness management grows, this study examined the interplay of psychological traits – grit, self-efficacy, resilience, and nature-relatedness – and their collective impact on the Quality of Life (QoL) among patients with rheumatoid arthritis (RA) in Malaysia.
Methods
A cross-sectional study was conducted among 222 patients with RA at a private hospital in Malaysia. Utilizing validated scales, including the Connor-Davidson Resilience Scale, Short Grit Scale, Nature Relatedness Scale, and Arthritis Self Efficacy Scale, data were collected. Pearson Product-moment Correlation analyses assessed the relationships between variables, and a multiple mediation analysis explored the mediating effects of resilience, grit, and self-efficacy on the relationship between nature-relatedness and QoL.
Findings
Of the 222 participants (86% female, mean age = 56.03, S.D. = 13.42), the analysis revealed a significant mediating role of resilience in the relationship between nature-relatedness and QoL among RA patients (b = −.117, SE = .042, 95% BCa CI [−.208, –.046]). Although grit and self-efficacy positively correlated with QoL, they did not serve as significant mediators in the nature-relatedness – QoL relationship. This highlights the pivotal role of building a sense of resiliency among patients with RA.
Interpretation
Individuals with RA are not only resilient in terms of their psychological traits such as grit, self-efficacy, and general resilience but also exhibit resilience in their connection and interaction with the natural environment (nature-relatedness). This holistic concept recognizes that fostering resilience in both psychological aspects and the context of one's environment is crucial for promoting overall well-being, particularly in the management of chronic illnesses like RA. It emphasizes the interconnectedness of psychological factors and environmental engagement in contributing to an individual's ability to cope and thrive despite health challenges.
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune condition that profoundly impacts both the physical and psychosocial well-being of those affected (Matcham et al., Citation2016). Globally, this condition affects around 0.5–1% of the population, exhibiting a pronounced impact on women, and typically manifesting between the ages of 30 and 60, though it can arise at any age (Aletaha et al., Citation2010). A recent systematic review (see Almutairi et al., Citation2021) supports these findings, reporting a global prevalence of 0.46% during the period from 1980 to 2019. In Malaysia, the prevalence and challenges of RA align with global trends, complicated by specific cultural, environmental, and healthcare system factors. Patients with RA experience not only joint pain, stiffness, swelling, and reduced mobility but also systemic symptoms like severe fatigue, often overlooked by those not afflicted by the disease (Aletaha et al., Citation2010; Bai et al., Citation2020; Sarzi-Puttini et al., Citation2014; van der Linden et al., Citation2010).
This condition necessitates a lifetime of coping, leading to substantial psychological distress, including anxiety, depression, and a marked decrease in quality of life (QoL; Ahmed Ali et al., Citation2022; Machin et al., Citation2020). This distress is compounded in Malaysia by strong familial and community ties, extending the disease's impact on caregivers and the wider social environment (Jin et al., Citation2021; Lwin et al., Citation2020). The prevalence of depression and anxiety is significantly higher among patients with RA compared to the general population, exacerbating physical symptoms, and creating a vicious cycle that further diminishes QoL (Wan et al., Citation2016). The psychological burden, including unrelenting pain and profound fatigue, contributes to a downward spiral in mental health and overall well-being, underscoring the complexity of managing RA (Bai et al., Citation2020; Gettings, Citation2010; Houge et al., Citation2020; Lwin et al., Citation2020; Matcham et al., Citation2014; van Vilsteren et al., Citation2015).
Nature-relatedness
The concept of nature-relatedness or nature-connectedness, a psychological construct, describes an individual's subjective connection with nature (Nisbet & Zelenski, Citation2013). This relationship encompasses various environments, from man-made parks to pristine wilderness areas. These environments are classified into two main types: green environments, predominantly featuring vegetation such as forests and gardens (Aerts et al., Citation2020), and blue environments, characterized by water elements like rivers and coastlines (White et al., Citation2020). Research demonstrates that exposure to both green and blue natural environments positively influence mental well-being, aiding in stress reduction and enhancing positive emotional states (Bratman et al., Citation2012; McMahan & Estes, Citation2015; Olszewska-Guizzo et al., Citation2022; Sztainberg et al., Citation2010). In urbanized areas such as Malaysia, the inclusion of green spaces has been linked with improved happiness and mental health, underscoring its importance in managing psychological well-being and chronic diseases (Cervinka et al., Citation2012; Hermanski et al., Citation2021; White et al., Citation2021). Nature-relatedness has also been identified as a predictor of individual happiness (Zelenski & Nisbet, Citation2014), potentially leading to an increase in QoL.
However, the ability of patients with RA to enjoy green and blue environments could vary widely based on the severity of their symptoms, functional limitations, and personal preferences. Individuals with RA may find it challenging to navigate uneven landscapes, engage in prolonged walks, or endure exposure to various weather conditions, depending on the extent of joint involvement. The impact of nature-relatedness on the QoL of individuals with RA has not been extensively studied. The only study that incorporates nature and RA individuals was done in Denmark (see Knudsen et al., Citation2024), representing a significant gap in the literature. This aspect is particularly pertinent given the potential of nature-relatedness to positively affect the lives of patients with RA. The current study seeks to address this gap by examining the role of nature-relatedness in improving the QoL for individuals with RA in Malaysia.
Grit
Grit, defined as perseverance and long-term goal orientation, emerges as a potential coping mechanism for individuals with chronic diseases like RA (Duckworth & Quinn, Citation2009). Studies have found that individuals with high levels of grit, especially those dealing with chronic illnesses, are better at managing their healthcare and exhibit improved mental and physical health related QoL (Sharkey, Bakula, Baraldi, et al., Citation2017; Sharkey, Bakula, Gamwell, et al., Citation2017). Furthermore, grit serves as a protective factor against suicidal ideation and is also associated with better psychological well-being (Pennings et al., Citation2015; Vainio & Daukantaitė, Citation2015).
While the consensus in the literature points to a positive relationship between grit and QoL, variations exist (Sharkey, Bakula, Gamwell, et al., Citation2017; Singh & Jha, Citation2008; Traino et al., Citation2019). Some research highlights the role of grit in enhancing psychological well-being and reducing suicidal thoughts. In contrast, others focus on its practical aspects, like adherence to treatment and physical activity (Karkazian, Citation2021). The extent to which grit influences specific RA outcomes, such as pain management and disease progression, is less clear and warrants further investigation. Only one study addresses the substantial impact of RA on QoL (Matcham et al., Citation2014). Some studies adopt different approaches, examining related constructs such as resilience and self-efficacy, and how these interact with grit (Heise, Citation2023; Riklin, Citation2021). For example, the role of resilience in managing chronic illness, as explored in several studies, might offer insights into how grit contributes to coping strategies in patients with RA.
In RA management, grit can manifest as a steadfast commitment to adhering to treatment regimens, engaging in physical activity despite discomfort, and maintaining social and occupational roles to the best of one's ability. However, the relationship between grit and specific RA outcomes, such as pain management and disease progression, is still underexplored. This gap presents an opportunity for future research, particularly in exploring how grit can be nurtured and utilized as part of a comprehensive RA management strategy.
Self-efficacy
Self-efficacy, reflecting belief in one's capacity to achieve desired outcomes, plays a crucial role in managing rheumatoid arthritis (RA) (Brady, Citation2003). It positively impacts pain management, coping strategies, physical functioning, and overall well-being in RA individuals (Ahlstrand et al., Citation2016; Gong & Mao, Citation2016). High self-efficacy is associated with better adaptation to the disease, effective coping strategies, and improved QoL (Brekke et al., Citation2001; Suh et al., Citation2022). Proactive behaviors such as regular exercise, medication adherence, and pain management techniques are more common among individuals with high self-efficacy (Brady, Citation2003). This contributes to reduced pain and increased QoL (Knittle et al., Citation2011). Regardless of age, sex, or chronic illness, self-efficacy is linked to improved QoL, lower pain intensity, and better psychological health in RA patients (Martinez-Calderon et al., Citation2018). A meta-analysis confirms the significant association between self-efficacy and functional impairment, pain severity, and emotional distress in RA patients (Jackson et al., Citation2019), emphasizing the importance of enhancing self-efficacy in RA management.
Bandura (Citation1977) identifies four primary sources from which individuals construct their self-efficacy beliefs: enactive mastery experience, vicarious experience, verbal or social persuasion, and physiological and affective state. While self-efficacy is generally beneficial, its impact can vary depending on factors like disease stage, psychological state, and available support systems (Ahlstrand et al., Citation2016). To enhance self-efficacy in Malaysian RA patients, interventions should focus on these four sources. Individual interventions, community support, and healthcare system assistance can contribute to building self-efficacy. Success in managing RA symptoms firsthand empowers individuals (enactive mastery experience), while witnessing others’ successful management of RA (vicarious experience) and receiving encouragement from healthcare professionals, peers, and family (verbal or social persuasion) further boosts self-efficacy. Addressing emotional and physical well-being is crucial, and a holistic approach integrating traditional healthcare practices with modern digital interventions like mobile health (mHealth) can offer tailored support. By targeting these sources, interventions can effectively empower RA patients in Malaysia and enhance their QoL.
Resilience
In managing the complexities of RA, resilience, defined as the ability to recover and adapt to stress (Criss et al., Citation2002), emerges as a critical psychosocial factor. It is critical in improving the QoL for individuals with RA. It has been demonstrated that resilience aids in coping with the chronic stress and pain associated with RA, leading to better overall well-being (Liu et al., Citation2017). This is supported by Shaw et al. (Citation2019), who found that resilience, through adaptive coping mechanisms and positive emotional regulation, significantly mitigates the negative impacts of RA. The findings across studies are remarkably consistent in emphasizing the positive impact of resilience on RA. It has been suggested that resilience was fostered through therapeutic interventions and personal psychological resources, contributing to better mental health and QoL in patients with RA (Haskett et al., Citation2006; Klostermann, Citation2017). A study by Edward (Citation2005) also supports this, demonstrating resilience as a protective factor against depression, a common comorbidity in RA. Furthermore, resilience has been emphasized as a critical factor in coping with global health crises, such as the COVID-19 pandemic (Naeem et al., Citation2020), which can compound the stress experienced by individuals with chronic illnesses like RA. While most studies concur on the positive role of resilience, contrasting studies suggest that external factors such as cultural beliefs and practices and even environmental factors may play a role in shaping attitudes towards illness and coping strategies, affecting resilience levels in individuals with RA (Bartlett et al., Citation2003; Evers et al., Citation2011).
It was mentioned that resilience in RA is multifaceted, involving both individual psychological aspects and social support systems, emphasizing the need for a holistic approach to resilience-building (Amenya, Citation2020). There are diverse approaches to understanding and fostering resilience in RA. While some studies focus on psychological interventions (e.g. Cognitive Behavioral Therapy; Haskett et al., Citation2006), others, like Bartlett et al. (Citation2003), emphasize the importance of cultural and contextual factors in resilience building. Based on these findings, a new idea could be the development of a culturally sensitive, multi-dimensional approach to resilience-building in patients with RA. This approach would not only incorporate psychological interventions but also consider the unique cultural and environmental factors that influence resilience in different populations. Hence, the current study will closely study the resilience level of RA individuals in Malaysia and how it interacts with their QoL.
This study aims to investigate the interplay of grit, self-efficacy, resilience, nature-relatedness and QoL among patients with RA. While individual studies have explored these variables in isolation, their combined influence on patients with RA’ QoL has been less examined. This research seeks to bridge this gap, exploring how these factors synergistically enhance the QoL of individuals contending with RA, especially in the post-pandemic era and in the unique Malaysian context. It is anticipated that (1) nature-relatedness, resilience, grit, and self-efficacy are directly associated with QoL, and (2) there is a mediation effect of resilience, grit, and self-efficacy between nature-relatedness and QoL, respectively.
Methods
Participants
A total of 222 participants were recruited through purposive sampling by conducting data collection at a private hospital in Malaysia (Ethical Approval Code: SUREC 2023/0090). Purposive sampling refers to a non-random sampling technique where participants are selected based on specific inclusion and exclusion criteria set for the research objectives. This sampling approach ensures that the sample population is representative of the target population of interest and enables researchers to obtain in-depth insights into the research topic (Creswell & Creswell, Citation2017). The inclusion criteria consisted of individuals who are aged 18 and above, currently seeking/getting treatment from a rheumatologist and have been diagnosed with RA for at least 6 months. The participants’ ages ranged from 18 to 93 (M = 56.03, SD = 13.42). The duration of the participants being diagnosed with RA ranges from 1 month to 48 years. illustrates the demographic statistics for all the participants.
Table 1. Summary of demographic statistics (N = 222).
Measures
Connor-Davidson Resilience Scale
The Connor-Davidson Resilience Scale (CD-RISC) – there are three variations of CD-RISC which came in either 25-item, 10-items, or 2-items. They are a unidimensional self-reported scale with 5 options for each item ranging from 0 = not true at all to 4 = true nearly all the time (Connor & Davidson, Citation2003). The CD-RISC has a Cronbach’s alpha of .93 indicating an excellent internal consistency (Connor & Davidson, Citation2003). In this study, CD-RISC 10-item was utilized to measure resilience and has a Cronbach’s alpha of .85, indicating good internal consistency (Campbell-Sills & Stein, Citation2007). Operationally, resiliency was measured by summing the scores of all the items. Total possible scores for CD-RISC range from 0 to 40. Higher scores indicate higher resilience. An example item was ‘I tend to bounce back after illness, injury or other hardships’. A fee was paid to the author for the items to be used in a secure electronic format. In the current study, Cronbach’s alpha for CD-RISC is .84, indicating a good internal consistency.
Short Grit Scale
The Short Grit Scale (Grit-S) was utilized in the current study to measure trait-level perseverance and passion for long-term goals (Duckworth & Quinn, Citation2009). An example of item was ‘Setbacks don’t discourage me’. The Grit-S is an 8-item self-reported measure utilizing a 5-point Likert scale ranging from 1 (very much like me) to 5 (not like me at all) and 4 items needed to be reversed their scores (item 2, 4, 7 and 8). The scale had Cronbach’s alpha values ranging from .73 to .83 (acceptable to good internal consistency) based on four different samples in a validation study (Duckworth & Quinn, Citation2009). The total possible scores for Grit-S range from 8 to 40. Operationally, grit was calculated by summing up the item scores. Higher scores will indicate a higher grit. In the current study, Grit-S have an acceptable internal consistency with Cronbach’s alpha of .71.
Nature Relatedness Scale
The Nature Relatedness Scale (NR-6) was utilized to measure one’s differences in terms of their relationship with the natural world (Nisbet & Zelenski, Citation2013). The NR-6 is a 6-item self-reported measure with a 5-point Likert scale ranging from 1 (Disagree strongly) to 5 (Agree strongly). An example item was ‘I always think about how my actions affect the environment’. In the psychometric study of developing NR-6, Cronbach’s alpha of the scale ranged from .83 to .86, which indicates good internal consistency (Nisbet & Zelenski, Citation2013). The total possible scores for NR-6 range from 6 to 30. Operationally, nature-relatedness was calculated by summing up the item scores where a higher score indicates greater nature-relatedness. In the current study, NR-6 has a good internal consistency with Cronbach’s alpha of .82.
Arthritis Self-Efficacy Scale
The Arthritis Self-Efficacy Scale (ASES) was utilized to gauge individuals’ perceived self-efficacy in managing arthritis-related challenges (Lorig et al., Citation1989). Originally comprising 20 items across pain, function, and other symptoms subscales, the ASES utilizes a 10-point Likert scale. We employed the abbreviated 8-item version, ASES-8, incorporating two pain-related items, four items addressing other symptoms, and two additional items focusing on preventing pain and fatigue interference with daily activities and demonstrates good internal consistency (Cronbach’s alpha = .89) (Wilcox et al., Citation2014). Example item: ‘How certain are you that you can keep arthritis or fibromyalgia pain from interfering with the things you want to do?’ Scores range from 8 to 80, with higher scores denoting greater self-efficacy. In the current study, ASES-8 has a good internal consistency with Cronbach’s alpha of .89.
Rheumatoid arthritis-specific quality of life
The Rheumatoid Arthritis-Specific Quality of Life (RAQoL) was utilized to assess individuals’ QoL with rheumatoid arthritis (RA) (de Jong et al., Citation1997). This self-reported measure consists of 30 items, each with a binary response format (Yes/No). For instance, an item example includes ‘I find it difficult to walk to the shops.’ The RAQoL demonstrates excellent internal consistency, with a Cronbach’s alpha exceeding .90 (de Jong et al., Citation1997). Scores range from 0 to 30, with higher scores indicating lower QoL. In our study, the RAQoL exhibited good internal consistency, with a Cronbach’s alpha of .88.
Procedure
This quantitative, cross-sectional study utilized a combination of online and offline recruitment methods. This study received ethical approval from the University Research Ethical Committee under approval number SUREC 2023/009. Recruitment efforts included online outreach via social media platforms and offline distribution of posters on hospital notice boards. Questionnaires were in English and administered in English by a research assistant, were completed during patients’ visits to the doctor. Written informed consent, socio-demographic and medical information were obtained. Participants had the option to withdraw at any time, with their data immediately deleted. Upon completion, participants were directed to a debriefing page, and a token of appreciation (RM10) was offered for their participation.
Data analysis
IBM’s SPSS version 27 was utilized for correlation analysis and Hayes’ (2022) mediation analysis (Model 4) via the PROCESS SPSS Macro to examine the mediation effect of resilience, grit, and self-efficacy on the relationship between nature-relatedness and QoL. Pearson correlation assessed relationships between variables, while mediation results were obtained using Hayes’ recommended bootstrapping technique. Significance was determined by examining the 95% confidence interval, with non-zero intervals indicating statistical significance. This rigorous approach aimed to ensure the robustness and credibility of the detected mediation effects.
Results
Pearson Product-moment Correlation analyses were done to assess the relationship between the variables. It was found that there is a significant medium negative relationship between resilience and RAQoL (r = −.37, p < .001), which means when one’s resilience is high, their RAQoL score is lower, which indicates a better QoL. Next, grit was found to have a small negative link with RAQoL (r = −.17, p = .012), indicating that higher grit reduces one’s RAQoL score, which means they have a better QoL. Furthermore, nature-relatedness was found to have no significant relationship with QoL (r = −.06, p = .373). Finally, self-efficacy was calculated to have a medium positive association with QoL (r = −.33, p < .001), meaning a higher self-efficacy contributes to lower RAQoL score, indicating a better QoL.
A mediation analysis was done to assess the complex relationship of nature-relatedness, resilience, grit, and self-efficacy on QoL. After determining the mediators, multiple mediation analysis was conducted via PROCESS SPSS Macro (Hayes, Citation2022) to investigate the mediating effects of resilience (M1), grit (M2) and self-efficacy (M3) between nature relatedness (X) and QoL (Y). As age was associated with RAQoL scores, (r = −.15, p = .028; See ), it was treated as a covariate in the mediation analysis to avoid contamination of the estimates of both direct and indirect effects.
Table 2. Pearson Product-Moment Correlations between Independent Variables (N = 222).
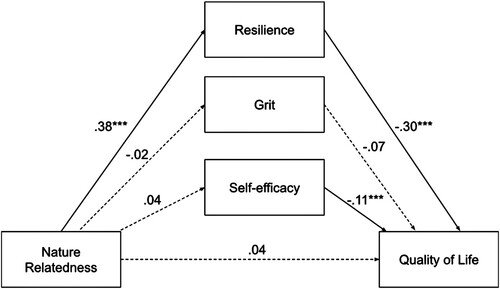
The first indirect effect is the specific indirect effect of nature relatedness on QoL via resilience, (X → M1 → Y) was significant (b = −.117, SE = .042, 95% BCa CI [−.208, −.046]). The second indirect effect would be the specific indirect effect of nature relatedness on QoL via grit, (X → M2 → Y) was reported as insignificant (b = .001, SE = .008, 95% BCa CI [−.013, .020]). The third indirect effect is the specific indirect effect of nature-relatedness on QoL through self-efficacy, (X → M3 → Y) which was insignificant (b = −.004, SE = .025, 95% BCa CI [−.057, .042]). The total indirect effect (cumulative indirect effect) was found to be significant (b = −.120, SE = .054, 95% BCa CI [−.233, −.022]).
Furthermore, the direct effect of nature-relatedness on QoL in the presence of mediators (resilience, grit, and self-efficacy) was found insignificant (b = .041, SE = .085, 95% BCa CI [−.126, .208], p = .630). The total effect of the model is insignificant (b = −.079, SE = .088, 95% BCa CI [−.252, .094], p = .371). Although the direct effect of nature-relatedness on QoL was not significant, modern mediation analysis frameworks allow for the examination of indirect effects in the absence of a significant direct relationship (Hayes, Citation2022, p. 156). Hence, there is a complete mediation of resilience in the relationship between nature-relatedness on QoL. The mediation summary is presented in .
Figure 1. Mediation Model 4 in predicting quality of life in individuals living with rheumatoid arthritis
Note. Statistics are regression coefficients. Dotted lines represent non-significant paths, while bold lines represent significant paths. Age as covariate for QoL. R2 = .21 ***p < .001.
Discussion
In the context of RA, understanding how psychological traits interact with QoL offers insightful perspectives on patient management. Grit, self-efficacy, and resilience are three different traits that have varying degrees of impact on QoL, especially when considering their relationship with NR.
Individual psychological traits on quality of life
Individuals with RA who have higher grit were found to have better QoL. Grit contributes to better QoL by fostering persistent and proactive coping strategies in RA management (Heise, Citation2023; Sharkey, Bakula, Baraldi, et al., Citation2017; Singh & Jha, Citation2008). This trait enables individuals to maintain focus and effort despite the chronic nature of RA, potentially leading to improved life outcomes. However, the impact of grit may not be sufficient to mediate the NR-QoL pathway. This suggests that while grit is beneficial for overall QoL, its influence is not directly linked to how individuals connect with nature and their subsequent QoL.
Self-efficacy also correlated significantly with QoL in patients with RA. This trait impacts QoL by enhancing an individual's confidence in managing the demands of disease (Akten et al., Citation2023). High levels of self-efficacy are associated with better disease management and improved life satisfaction. However, grit, self-efficacy did not mediate the relationship between NR and QoL. Although self-efficacy is a crucial component of QoL, other factors, notably resilience, play a more significant role in linking NR to life quality.
NR generally positively impacts mental health (Nisbet & Zelenski, Citation2013; White et al., Citation2020), but the current study revealed an insignificant direct relationship between NR and QoL in patients with RA. Though surprising, NR may have contributed to QoL for RA patients. Specifically, engagement in nature-based activities fosters resilience by promoting vitality, alleviating pain, enhancing well-being, and strengthening community ties (Knudsen et al., Citation2024). These benefits suggest that while direct effects might be elusive, the indirect pathways through which NR influences QoL are substantial and meaningful. This indirect pathway is further discussed in the next section.
The mediating role of resilience
Resilience is recognized as a vital factor in improving QoL in patients with RA (Criss et al., Citation2002; Liu et al., Citation2017). In the current study, resilience stands out as it significantly mediated the relationship between NR and QoL. Studies have consistently shown that resilience, fostered through therapeutic interventions and psychological resources, positively impacts mental health and QoL in patients with RA (Haskett et al., Citation2006; Klostermann, Citation2017). The current findings revealed that while NR alone did not significantly impact QoL, its combination with resilience contributed to a better QoL. This suggests that the benefits of NR in patients with RA are enhanced when coupled with resilience-building strategies.
The current study highlighted the importance of resilience as it significantly mediated the relationship between NR and QoL. While NR alone did not significantly impact QoL, when combined with resilience, it contributed to a better QoL. This suggests that the benefits of NR in patients with RA may be enhanced when coupled with resilience-building strategies. When patients can adapt and cope with stress, it is crucial to connect them with nature to improve the QoL in patients with RA.
These insights emphasize the multifaceted nature of QoL determinants in patients with RA. It suggests that while environmental factors like NR have potential benefits, their efficacy in improving QoL is significantly influenced by psychological factors such as resilience. This highlights the need for a holistic approach in RA management, considering both environmental engagement and psychological empowerment.
Strengths and practical implications
This study used psychometrically validated tools to rigorously evaluate key variables such as resilience, grit, nature-relatedness, self-efficacy, and QoL. These established scales, known for their strong psychometric properties, underpin the reliability of the findings. A significant sample of patients with RA (n = 222) was carefully chosen, ensuring statistical robustness. Notably, this research focuses on the Malaysian context, which provides fresh perspectives, distinct from predominant Western-centric studies. This cultural consideration is crucial, as psychosocial and environmental factors vary globally. The study's empirical exploration of the interplay between nature, resilience, and QoL offers practical insights, advocating for nature-based interventions in RA therapy to enhance patient well-being. The methodology's rigor, cultural relevance, and practical implications are the study's key strengths.
Natural environments may be a potential intervention, as exposure to natural settings such as forests, mountains, and waterscapes has been linked to decreased stress, inflammation, and pain (Hansen et al., Citation2017). Incorporating pictures of forests and mountains and playing recordings of nature sounds, such as birds chirping and ocean ways in rheumatologists or counseling clinics, could complement our findings. These cues may create a calming and soothing environment for patients, potentially reducing stress and anxiety associated with medical appointments. Additionally, the use of natural colors, placement of indoor plants for a touch of greenery or natural materials furniture, and displaying images of natural landscapes can evoke positive emotions and encourage patients to consider engaging in nature-based activities outside of the clinic setting. This visual enhancement aligns with the holistic approach to healthcare, promoting overall well-being by addressing not only physical symptoms but also emotional and psychological needs. Moreover, it reinforces the message that nature plays a significant role in promoting resilience and QoL for individuals living with chronic conditions like rheumatoid arthritis.
Besides the indoor visual enhancement, activities such as walking and hiking in these settings have shown benefits not only for cardiovascular fitness but also for immune function, as seen in the increase of Natural Killer cells (NK cells), and mental well-being (Haluza et al., Citation2014; Li, Citation2010). As such, the Alpine settings may be a viable option as a nature-based intervention as this distinct environment offers unique opportunities for health tourism, leveraging its clean air, diverse flora, and opportunities for physical activity, such as hiking, which are conducive to both physical and mental well-being (Spoladore & Pessot, Citation2023).
This study emphasizes the significance of resilience as a mediator between nature-relatedness and QoL. While nature-based intervention is important for patients with RA, the effectiveness could be further enhanced when combined with resilience-building strategies and counseling approaches. Resilience-building strategies often involve fostering a sense of connection with nature, which aligns with the principles of planetary health. Counseling approaches that encourage individuals to engage with natural environments, such as spending time outdoors, practicing mindfulness in nature, or participating in ecotherapy, promote not only personal well-being but also environmental stewardship and appreciation.
The efficacy of nature-based interventions, such as aquatic exercise and balneotherapy, in chronic health conditions is well-established (Kamioka et al., Citation2014) where it could be tailored for RA-specific programs that combine psychological empowerment with environmental engagement. Additionally, virtual reality simulations of natural environments present a promising avenue, where 360-degree videos of blue/green spaces significantly alleviated pain and anxiety in hospitalized patients (White et al., Citation2018). Virtual reality, particularly when paired with psychotherapeutic methods, has shown effectiveness in chronic pain management (Bilika et al., Citation2023; Wong et al., Citation2022), offering an accessible treatment option for RA patients unable to interact with natural settings directly. The findings advocate for further investigation into nature-based, resilience-building interventions for RA management.
Incorporating natural elements into RA treatment strategies reflects a holistic health perspective, addressing not only the physical aspects of RA but also its emotional and psychological dimensions. This holistic approach is in line with the current healthcare trend towards patient-centered and non-invasive treatments, underscoring the complexity of chronic diseases and the importance of diverse, innovative treatment methods.
Limitations and recommendations
While novel, this study has some limitations that provide opportunities for future research. For instance, more objective assessments could be incorporated to help validate and triangulate the measurements of the variables, such as nature exposure and resilience in future studies. For nature exposure, GPS tracking or geospatial mapping of participants’ locations and movements (Kestens et al., Citation2018) could provide objective confirmation of time spent in natural environments. Clinician interviews and observations evaluating coping strategies over time could also complement self-reported resilience scores (Min et al., Citation2013). Multi-modal assessments combining self-reports, clinician inputs, geospatial tracking and other tools could yield a more comprehensive evaluation, thus enhancing the validity and rigor of future studies. Additionally, most of our patients are in the remission stage with a DAS28 score of less than 2.6, which could limit our findings. We might not produce a similar result if our patients have moderate or high disease activity.
Additionally, more diverse samples would improve generalizability, as this study primarily comprised middle-aged Chinese women. Examining multicultural perspectives or exploring gender-specific differences in the experience and management of RA could reveal nuances in how nature and resilience interact. Along similar lines, geographic factors may influence nature accessibility and type. Comparing effects across urban versus rural settings and socioeconomic status (income level, household size, geographic location) could be insightful. Future research could examine additional potential cultural factors and other socioeconomic status factors and extend the study to hospitals located in an area with a non-Chinese population to gain a more comprehensive understanding.
Additionally, disease-related factors like functional disability, pain levels, and flare status could moderate resilience and nature's impact on QoL (Katz, Citation2016; Matcham et al., Citation2013). Accounting for variations in RA disease activity (level of inflammation and disease severity), specific disease stages or conditions (e.g. early-stage disease, late-stage disease, or sustained remission), and symptoms may reveal differences in how psychological traits and nature exposure affect patient-reported outcomes. A multi-faceted approach considering social, psychological, environmental, and disease-related factors could provide deeper, more nuanced insights into QoL determinants.
Conclusion
In conclusion, this study on RA highlights the interplay between psychological factors such as grit, self-efficacy, resilience, nature-relatedness, and their impact on QoL. Our study revealed that resilience plays a pivotal mediating role in improving QoL, overshadowing the direct effects of nature-relatedness, grit, and self-efficacy. While the study’s rigorous methodology, significant sample size, and use of validated scales underscore its reliability and provide a culturally nuanced understanding of RA management, its limitations suggest future research avenues. These include incorporating more objective assessments and a diverse sample for broader generalizability, as well as exploring additional mediators and moderators like social support and disease-related factors. Overall, the study advocates for holistic, patient-centered therapeutic strategies that integrate psychological empowerment with environmental and cultural considerations, underscoring the importance of resilience and psychological traits in enhancing the QoL of patients with RA.
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by an Institutional Review Board/Ethics Committee. See details under Methods.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement7
Data is available upon request from the corresponding author.
Additional information
Funding
References
- Aerts, R., Dujardin, S., Nemery, B., Van Nieuwenhuyse, A., Van Orshoven, J., Aerts, J.-M., Somers, B., Hendrickx, M., Bruffaerts, N., Bauwelinck, M., Casas, L., Demoury, C., Plusquin, M., & Nawrot, T. S. (2020). Residential green space and medication sales for childhood asthma: A longitudinal ecological study in Belgium. Environmental Research, 189, 109914. https://doi.org/10.1016/j.envres.2020.109914
- Ahlstrand, I., Vaz, S., Falkmer, T., Thyberg, I., & Björk, M. (2016). Self-efficacy and pain acceptance as mediators of the relationship between pain and performance of valued life activities in women and men with rheumatoid arthritis. Clinical Rehabilitation, 31(6), 824–834. https://doi.org/10.1177/0269215516646166
- Ahmed Ali, S., Riaz, H., Arslan, A., Ahmad, A., & Iqbal, M. (2022). Effect of Stress on quality of life in patients with chronic rheumatoid arthritis. Pakistan BioMedical Journal, 5(5), 94–98. https://doi.org/10.54393/pbmj.v5i5.452
- Akten, I. M., Akin, S., Ozdemir, O., Avcioglu, Z., & Yasar, N. (2023). Evaluation of quality of life and self efficacy perception in chronic diseases. ProQuest, 16(2), 771–786. https://www.proquest.com/scholarly-journals/evaluation-quality-life-self-efficacy-perception/docview/2865401068/se-2?accountid=41453
- Aletaha, D., Neogi, T., Silman, A. J., Funovits, J., Felson, D. T., Bingham, C. O., Birnbaum, N. S., & Burmester, G. R. (2010). 2010 rheumatoid arthritis classification criteria: An American college of rheumatology/European league against rheumatism collaborative initiative. Arthritis & Rheumatism, 62(9), 2569–2581. https://doi.org/10.1002/art.27584
- Almutairi, K. B., Nossent, J. C., Preen, D. B., Keen, H. I., & Inderjeeth, C. A. (2021). The prevalence of rheumatoid arthritis: A systematic review of population-based studies. The Journal of Rheumatology, 48(5), 669–676. http://dx.doi.org/10.3899/jrheum.200367
- Amenya, G. S. (2020, November 1). Self-esteem, resilience and quality of life of persons with rheumatoid arthritis at korle-bu teaching hospital, ghana. Ir.ucc.edu.gh. https://ir.ucc.edu.gh/xmlui/handle/123456789/10358
- Bai, B., Chen, M., Fu, L., Liu, H., Jin, L., Wei, T., & Xin, F. (2020). Quality of life and influencing factors of patients with rheumatoid arthritis in Northeast China. Health and Quality of Life Outcomes, 18(1), 1–10. https://doi.org/10.1186/s12955-020-01355-7
- Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. https://doi.org/10.1037/0033-295X.84.2.191
- Bartlett, S. J., Piedmont, R., Bilderback, A., Matsumoto, A. K., & Bathon, J. M. (2003). Spirituality, well-being, and quality of life in people with rheumatoid arthritis. Arthritis Care & Research, 49(6), 778–783. https://doi.org/10.1002/art.11456
- Bilika, P., Karampatsou, N., Stavrakakis, G., Paliouras, A., Theodorakis, Y., Strimpakos, N., & Kapreli, E. (2023). Virtual reality-based exercise therapy for patients with chronic musculoskeletal pain: A scoping review. Healthcare, 11(17), 2412–2412. https://doi.org/10.3390/healthcare11172412
- Brady, T. J. (2003). Measures of self-efficacy, helplessness, mastery, and control: The arthritis helplessness index (ahi)/rheumatology attitudes index (RAI), arthritis self-efficacy scale (ASES), children’s arthritis self-efficacy scale (CASE), generalized self-efficacy scale (GSES), mastery scale, multi-dimensional health locus of control scale (MHLC), parent’s arthritis self-efficacy scale (PASE), rheumatoid arthritis self-efficacy scale (RASE), and self-efficacy scale (SES). Arthritis & Rheumatism, 49(S5), S147–S164. https://doi.org/10.1002/art.11413
- Bratman, G. N., Hamilton, J. P., & Daily, G. C. (2012). The impacts of nature experience on human cognitive function and mental health. Annals of the New York Academy of Sciences, 1249(1), 118–136. https://doi.org/10.1111/j.1749-6632.2011.06400.x
- Brekke, M., Hjortdahl, P., & Kvien, T. K. (2001). Self-efficacy and health status in rheumatoid arthritis: A two-year longitudinal observational study. Rheumatology, 40(4), 387–392.
- Campbell-Sills, L., & Stein, M. B. (2007). Psychometric analysis and refinement of the Connor–Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress, 20(6), 1019–1028. https://doi.org/10.1002/jts.20271
- Cervinka, R., Röderer, K., & Hefler, E. (2012). Are nature lovers happy? On various indicators of well-being and connectedness with nature. Journal of Health Psychology, 17(3), 379–388. https://doi.org/10.1177/1359105311416873
- Connor, K. M., & Davidson, J. R. T. (2003). Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety, 18(2), 76–82. https://doi.org/10.1002/da.10113
- Creswell, J. W., & Creswell, J. D. (2017). Research design qualitative, quantitative, and mixed methods approaches (4th ed.). Sage.
- Criss, M. M., Pettit, G. S., Bates, J. E., Dodge, K. A., & Lapp, A. L. (2002). Family adversity, positive peer relationships, and children’s externalizing behavior: A longitudinal perspective on risk and resilience. Child Development, 73(4), 1220–1237. https://doi.org/10.1111/1467-8624.00468
- de Jong, Z., van der Heijde, D., McKenna, S. P., & Whalley, D. (1997). The reliability and construct validity of the RAQoL: A rheumatoid arthritis-specific quality of life instrument. Rheumatology, 36(8), 878–883. https://doi.org/10.1093/rheumatology/36.8.878
- Duckworth, A. L., & Quinn, P. D. (2009). Development and validation of the short grit scale (Grit–S). Journal of Personality Assessment, 91(2), 166–174. https://doi.org/10.1080/00223890802634290
- Edward, K. (2005). Resilience: A protector from depression. Journal of the American Psychiatric Nurses Association, 11(4), 241–243. https://doi.org/10.1177/1078390305281177
- Evers, A. W. M., Zautra, A., & Thieme, K. (2011). Stress and resilience in rheumatic diseases: A review and glimpse into the future. Nature Reviews Rheumatology, 7(7), 409–415. https://doi.org/10.1038/nrrheum.2011.80
- Gettings, L. (2010). Psychological well-being in rheumatoid arthritis: A review of the literature. Musculoskeletal Care, 8(2), 99–106. https://doi.org/10.1002/msc.171
- Gong, G., & Mao, J. (2016). Health-related quality of life among Chinese patients with rheumatoid arthritis. Nursing Research, 65(1), 55–67. https://doi.org/10.1097/NNR.0000000000000137
- Haluza, D., Schönbauer, R., & Cervinka, R. (2014). Green perspectives for public health: A narrative review on the physiological effects of experiencing outdoor nature. International Journal of Environmental Research and Public Health, 11(5), 5445–5461. https://doi.org/10.3390/ijerph110505445
- Hansen, M. M., Jones, R., & Tocchini, K. (2017). Shinrin-Yoku (forest bathing) and nature therapy: A state-of-the-art review. International Journal of Environmental Research and Public Health, 14(8), 851. https://doi.org/10.3390/ijerph14080851
- Haskett, M. E., Nears, K., Sabourin Ward, C., & McPherson, A. V. (2006). Diversity in adjustment of maltreated children: Factors associated with resilient functioning. Clinical Psychology Review, 26(6), 796–812. https://doi.org/10.1016/j.cpr.2006.03.005
- Hayes, A. F. (2022). Introduction to mediation, moderation, and conditional process analysis. Third Edition. A regression-based approach. Guilford Press.
- Heise, M. (2023). Grit, Resilience and Chronic Pain [PhD].
- Hermanski, A., McClelland, J., Pearce-Walker, J., Ruiz, J., & Verhougstraete, M. (2021). The effects of blue spaces on mental health and associated biomarkers. International Journal of Mental Health, 51(3), 203–217. https://doi.org/10.1080/00207411.2021.1910173
- Houge, I. S., Hoff, M., Thomas, R., & Videm, V. (2020). Mortality is increased in patients with rheumatoid arthritis or diabetes compared to the general population – the Nord-Trøndelag Health Study. Scientific Reports, 10(1), 3593. https://doi.org/10.1038/s41598-020-60621-2
- Jackson, T., Xu, T., & Jia, X. (2019). Arthritis self-efficacy beliefs and functioning among osteoarthritis and rheumatoid arthritis patients: A meta-analytic review. Rheumatology, 59, 948–958. https://doi.org/10.1093/rheumatology/kez219
- Jin, Y., Bratzke, L., & Baumann, L. C. (2021). Helping persons with multiple chronic conditions overcome barriers to selfmanagement. The Nurse Practitioner, 46(3), 20–28.
- Kamioka, H., Tsutani, K., Maeda, M., Hayasaka, S., Okuizum, H., Goto, Y., Okada, S., Kitayuguchi, J., & Abe, T. (2014). Assessing the quality of study reports on spa therapy based on randomized controlled trials by the spa therapy checklist (SPAC). Complementary Therapies in Clinical Practice, 20(4), 317–333.
- Karkazian, A. M. (2021). Thriving with rehumatoid arthritis (RA): A self-management program for young and middle-aged adults with RA [PhD].
- Katz, P. (2016). Physical activity and psychosocial aspects of arthritis. Springer EBooks, 213–239. https://doi.org/10.1007/978-3-319-22858-7_13
- Kestens, Y., Thierry, B., Shareck, M., Steinmetz-Wood, M., & Chaix, B. (2018). Integrating activity spaces in health research: Comparing the VERITAS activity space questionnaire with 7-day GPS tracking and prompted recall. Spatial and Spatio-Temporal Epidemiology, 25, 1–9. https://doi.org/10.1016/j.sste.2017.12.003
- Klostermann, M. (2017, June). Can wellbeing be predicted by resilience, positive emotions, acceptance and valued living among patients with rheumatism? University of Twente. https://purl.utwente.nl/essays/72753
- Knittle, K. P., De Gucht, V., Hurkmans, E. J., Vlieland, T. P. M. V., Peeters, A. J., Ronday, H. K., & Maes, S. (2011). Effect of self-efficacy and physical activity goal achievement on arthritis pain and quality of life in patients with rheumatoid arthritis. Arthritis Care & Research, 63(11), 1613–1619. https://doi.org/10.1002/acr.20587
- Knudsen, J. B., Simonÿ, C., Tang, L. H., Skou, S. T., & Beck, M. (2024). Nature-based group exercises for people with arthritis: A qualitative along-side interview study of lived experiences. Qualitative Health Research. https://doi.org/10.1177/10497323241227151
- Li, Q. (2010). Effect of forest bathing trips on human immune function. Environmental Health and Preventive Medicine, 15(1), 9–17. https://doi.org/10.1007/s12199-008-0068-3
- Liu, L., Xu, X., Xu, N., & Wang, L. (2017). Disease activity, resilience and health-related quality of life in Chinese patients with rheumatoid arthritis: A multi-center, cross-sectional study. Health and Quality of Life Outcomes, 15(1). https://doi.org/10.1186/s12955-017-0725-6
- Lorig, K., Chastain, R. L., Ung, E., Shoor, S., & Holman, H. R. (1989). Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis & Rheumatism, 32(1), 37–44. https://doi.org/10.1002/anr.1780320107
- Lwin, M. N., Serhal, L., Holroyd, C., & Edwards, C. J. (2020). Rheumatoid arthritis: The impact of mental health on disease: A narrative review. Rheumatology and Therapy, 7(3), https://doi.org/10.1007/s40744-020-00217-4
- Machin, A. R., Babatunde, O., Haththotuwa, R., Scott, I., Blagojevic-Bucknall, M., Corp, N., Chew-Graham, C. A., & Hider, S. L. (2020). The association between anxiety and disease activity and quality of life in rheumatoid arthritis: A systematic review and meta-analysis. Clinical Rheumatology, 39(5), 1471–1482. https://doi.org/10.1007/s10067-019-04900-y
- Martinez-Calderon, J., Meeus, M., Struyf, F., & Luque-Suarez, A. (2018). The role of self-efficacy in pain intensity, function, psychological factors, health behaviors, and quality of life in people with rheumatoid arthritis: A systematic review. Physiotherapy Theory and Practice, 36(1), 21–37. https://doi.org/10.1080/09593985.2018.1482512
- Matcham, F., Norton, S., Scott, D. L., Steer, S., & Hotopf, M. (2016). Symptoms of depression and anxiety predict treatment response and long-term physical health outcomes in rheumatoid arthritis: Secondary analysis of a randomized controlled trial. Rheumatology, 55(2), 268–278. https://doi.org/10.1093/rheumatology/kev306
- Matcham, F., Rayner, L., Steer, S., & Hotopf, M. (2013). The prevalence of depression in rheumatoid arthritis: A systematic review and meta-analysis. Rheumatology, 52(12), 2136–2148. https://doi.org/10.1093/rheumatology/ket169
- Matcham, F., Scott, I. C., Rayner, L., Hotopf, M., Kingsley, G. H., Norton, S., Scott, D. L., & Steer, S. (2014). The impact of rheumatoid arthritis on quality-of-life assessed using the SF-36: A systematic review and meta-analysis. Seminars in Arthritis and Rheumatism, 44(2), 123–130. https://doi.org/10.1016/j.semarthrit.2014.05.001
- McMahan, E. A., & Estes, D. (2015). The effect of contact with natural environments on positive and negative affect: A meta-analysis. The Journal of Positive Psychology, 10(6), 507–519. https://doi.org/10.1080/17439760.2014.994224
- Min, J.-A., Yu, J. J., Lee, C.-U., & Chae, J.-H. (2013). Cognitive emotion regulation strategies contributing to resilience in patients with depression and/or anxiety disorders. Comprehensive Psychiatry, 54(8), 1190–1197. https://doi.org/10.1016/j.comppsych.2013.05.008
- Naeem, F., Irfan, M., & Javed, A. (2020). Coping with COVID-19: Urgent need for building resilience through cognitive behaviour therapy. Khyber Medical University Journal, 12(1), 1–3. https://doi.org/10.35845/kmuj.2020.20194
- Nisbet, E. K., & Zelenski, J. M. (2013). The NR-6: A new brief measure of nature relatedness. Frontiers in Psychology, 4(813). https://doi.org/10.3389/fpsyg.2013.00813
- Olszewska-Guizzo, A., Sia, A., Fogel, A., & Ho, R. (2022). Features of urban green spaces associated with positive emotions, mindfulness and relaxation. Scientific Reports, 12(1). https://doi.org/10.1038/s41598-022-24637-0
- Pennings, S. M., Law, K. C., Green, B. A., & Anestis, M. D. (2015). The impact of grit on the relationship between hopelessness and suicidality. International Journal of Cognitive Therapy, 8(2), 130–142. https://doi.org/10.1521/ijct.2015.8.2.130
- Riklin, E. (2021). Examining the role of resilience and grit on the functioning of youth with chronic medical conditions [Doctoral dissertation].
- Sarzi-Puttini, P., Salaffi, F., Franco, M. D., Bazzichi, L., Cassisi, G., Casale, R., Cazzola, M., Stisi, S., Battellino, M., & Atzeni, F. (2014). Pain in rheumatoid arthritis: A critical review. Reumatismo, 66(1), 18–27. https://doi.org/10.4081/reumatismo.2014.760
- Sharkey, C. M., Bakula, D. M., Baraldi, A. N., Perez, M. N., Suorsa, K. I., Chaney, J. M., & Mullins, L. L. (2017). Grit, illness-related distress, and psychosocial outcomes in college students with a chronic medical condition: A path analysis. Journal of Pediatric Psychology, 43(5), 552–560. https://doi.org/10.1093/jpepsy/jsx145
- Sharkey, C. M., Bakula, D. M., Gamwell, K. L., Mullins, A. J., Chaney, J. M., & Mullins, L. L. (2017). The role of grit in college student health care management skills and health-related quality of life. Journal of Pediatric Psychology, 42(9), 952–961. https://doi.org/10.1093/jpepsy/jsx073
- Shaw, Y., Bradley, M., Zhang, C., Dominique, A., Michaud, K., McDonald, D., & Simon, T. A. (2019). Development of resilience among rheumatoid arthritis patients: A qualitative study. Arthritis Care & Research, 72(9), 1257–1265. https://doi.org/10.1002/acr.24024
- Singh, K., & Jha, S. D. (2008). Positive and negative affect, and grit as predictors of happiness and life satisfaction. Journal of the Indian Academy of Applied Psychology, 34(Special Issue), 40–45.
- Spoladore, D., & Pessot, E. (2022). An ontology-based decision support system to foster innovation and competitiveness opportunities of health tourism destinations. SpringerBriefs in Applied Sciences and Technology, 61–71. https://doi.org/10.1007/978-3-031-15457-7_4
- Suh, C.-H., Lee, K., Kim, J.-W., & Boo, S. (2022). Factors affecting quality of life in patients with rheumatoid arthritis in South Korea: A cross-sectional study. Clinical Rheumatology, 41(2), 367–375. http://dx.doi.org/10.1007/s10067-021-05944-9
- Sztainberg, Y., Kuperman, Y., Tsoory, M., Lebow, M., & Chen, A. (2010). The anxiolytic effect of environmental enrichment is mediated via amygdalar CRF receptor type 1. Molecular Psychiatry, 15(9), 905–917. https://doi.org/10.1038/mp.2009.151
- Traino, K. A., Bakula, D. M., Sharkey, C. M., Roberts, C. M., Ruppe, N. M., Chaney, J. M., & Mullins, L. L. (2019). The role of grit in health care management skills and health-related quality of life in college students with chronic medical conditions. Journal of Pediatric Nursing, 46, 72–77. https://doi.org/10.1016/j.pedn.2019.02.035
- Vainio, M. M., & Daukantaitė, D. (2015). Grit and Different Aspects of Well-Being: Direct and Indirect Relationships via Sense of Coherence and Authenticity. Journal of Happiness Studies, 17(5), 2119–2147. https://doi.org/10.1007/s10902-015-9688-7
- van der Linden, M. P. M., le Cessie, S., Raza, K., van der Woude, D., Knevel, R., Huizinga, T. W. J., & van der Helm-van Mil, A. H. M. (2010). Long-term impact of delay in assessment of patients with early arthritis. Arthritis & Rheumatism, 62(12), 3537–3546. https://doi.org/10.1002/art.27692
- van Vilsteren, M., Boot, C. R., Knol, D. L., van Schaardenburg, D., Voskuyl, A. E., Steenbeek, R., & Anema, J. R. (2015). Productivity at work and quality of life in patients with rheumatoid arthritis. BMC Musculoskeletal Disorders, 16(107). https://doi.org/10.1186/s12891-015-0562-x
- Wan, S. W., He, H.-G., Mak, A., Lahiri, M., Luo, N., Cheung, P. P., & Wang, W. (2016). Health-related quality of life and its predictors among patients with rheumatoid arthritis. Applied Nursing Research, 30, 176–183. http://dx.doi.org/10.1016/j.apnr.2015.07.004
- White, M. P., Elliott, L. R., Gascon, M., Roberts, B., & Fleming, L. E. (2020). Blue space, health and well-being: A narrative overview and synthesis of potential benefits. Environmental Research, 191, 110169. https://doi.org/10.1016/j.envres.2020.110169
- White, M. P., Elliott, L. R., Grellier, J., Economou, T., Bell, S., Bratman, G. N., Cirach, M., Gascon, M., Lima, M. L., Lõhmus, M., Nieuwenhuijsen, M., Ojala, A., Roiko, A., Schultz, P. W., van den Bosch, M., & Fleming, L. E. (2021). Associations between green/blue spaces and mental health across 18 countries. Scientific Reports, 11(1), 8903. https://doi.org/10.1038/s41598-021-87675-0
- White, M. P., Yeo, N., Vassiljev, P., Lundstedt, R., Wallergård, M., Albin, M., & Lõhmus, M. (2018). A prescription for “nature” – the potential of using virtual nature in therapeutics. Neuropsychiatric Disease and Treatment, 2018(14), 3001–3013. https://doi.org/10.2147/NDT.S179038
- Wilcox, S., Schoffman, D. E., Dowda, M., & Sharpe, P. A. (2014). Psychometric properties of the 8-item english arthritis self-efficacy scale in a diverse sample. Arthritis, 2014, 1–8. https://doi.org/10.1155/2014/385256
- Wong, K. P., Tse, M. M. Y., & Qin, J. (2022). Effectiveness of virtual reality-based interventions for managing chronic pain on pain reduction, anxiety, depression and mood: A systematic review. Healthcare, 10(10), 2047. https://doi.org/10.3390/healthcare10102047
- Zelenski, J. M., & Nisbet, E. K. (2014). Happiness and feeling connected: The distinct role of nature relatedness. Environment and Behavior, 46(1), 3–23. https://doi.org/10.1177/0013916512451901
