Abstract
This study aimed to describe the disparities in immunization coverage between National Immunization Program (NIP) vaccines and non-NIP vaccines in Yiwu and to identify potential determinants. A face-to-face interview-based questionnaire survey among 423 migrant children born from 1 June 2010 to 31 May 2013 was conducted. Immunization coverage was estimated according to the vaccines scheduled at different age, the birth cohorts, and socio- demographic characteristics. Single-level logistic regression analysis was applied to identify the determinants of coverage of non-NIP vaccines. We found that NIP vaccines recorded higher immunization coverage compared with non-NIP vaccines (87.9100%– vs 0%-74.8%). Among the non-NIP vaccines, varicella vaccine (VarV) recorded the highest coverage of 85.4%, which was introduced in 1998; while 7-valent pneumococcal conjugate vaccine(PCV7) recorded the lowest coverage of 0% for primary series, which was introduced recently. Lower coverage rate of non-NIP vaccines was significantly associated with more siblings in household, shorter duration of living in the surveyed areas, lower family income, mother with a job, mother with poor awareness of vaccination, and mother with lower education level. We found the immunization coverage rate of non-NIP vaccines was significant lower than that of NIP vaccines. Expansion of NIP to include non-NIP vaccines can provide better protection against the vaccine preventable diseases through increased immunization coverage.
Introduction
Vaccination is one of the most successful strategies available for the prevention of infection diseases.Citation1,2 Through the wide application of vaccines, the public health achievements included the eradication of smallpox and remarkable decrease in the morbidity and mortality of vaccine preventable diseases(VPDs) such as poliomyelitis, measles and hepatitis B.Citation3 Many countries have established a national immunization program (NIP) to organize public health leadership on immunization practice and to give technical and financial support for vaccination recommendations.
The China's NIP was established in 1978 and provided efforts to accommodate the demands of children at risk of VPDs. Since 2008, the Minister of Health(MoH, predecessor of National Health and Family Planning Committee) of China issued the vaccination schedule of NIP vaccines, which stipulats all children under 7 y of age should get following vaccines: Bacille Calmette-Guérin (BCG), hepatitis B vaccine (Hep B), diphtheria-tetanus-pertussis vaccine (DTP), oral poliovirus vaccine (OPV), measles containing vaccine (MCV), Japanese encephalitis vaccine (JEV), meningococcal polysaccharide vaccine type a(MPV-a), meningococcal polysaccharide vaccine type a and c(MPV-ac), hepatitis A vaccine (Hep A), diphtheria-tetanus vaccine(DT)Citation4 The budget for NIP vaccines is covered by Chinese central government and these NIP vaccines are provided to all children(including migrant children) free of charge, without any extra service fee. All children can get all the NIP and non-NIP vaccination in any immunization clinics when they traveled to other areas. The sustain improvement of accessibility and service quality of immunization clinic has resulted in an optimal increase in overall immunization coverage for most of areas in China in recent years.Citation5,6 Additionally, through supplementary immunization activities(SIAs) for OPV and MCV, the incidence of relevant VPDs remained at all-time low.Citation7,8
Despite these achievements, limited health financing restricted the China's NIP from expanding other vaccines. Many vaccines such as inactive poliovirus vaccine (IPV), varicella vaccine (VarV), Haemophilus influenzae type b vaccine(Hib), oral rotavirus vaccine(ORV), 7-valent pneumococcal conjugate vaccine(PCV7) have not been included in NIP. These non-NIP vaccines are paid by caregivers’ out-of-pocket expense, therefore, the vaccination fee may become a barrier to vaccinate children who live in a poorer resource environment, especially for the migrant children. Similar to other countries,Citation9 increasing population mobility coupled with lower vaccination coverage of migrants has been identified as one of the key contributors to VPDs outbreaks like varicella or pneumococcal pneumonia. Furthermore, the coverage rates of non-NIP vaccines for migrant children were lower than those for resident children. The main reasons for that may include the poor living condition and the poor awareness of immunization for migrant people. Recently, the consensus that the support for non-NIP vaccines has not been reached but the presence of inequalities of public health has been increasingly recognized.Citation10–12 The difference of immunization coverage between NIP and non-NIP vaccines among migrant children should be evaluated to provide evidence for the Chinese NIP policy decision in future. However, data on the coverage difference between NIP and non-NIP vaccines among migrant children have been scarcely reported.
In this face to face interview based survey, we aimed to identify and describe the difference in coverage between NIP and non-NIP vaccines among migrant children in Yiwu and to address the challenges facing current NIP policy.
Results
Demographic characteristics of children and their family
A total of 423 eligible children were interviewed and the immunization record booklets for all the surveyed children were available at the time of the interview. Of which 52% were male and 9.5% were preterm born. Almost 40% of the surveyed children were the only child in their family, and 63.8% were breast milk-fed. Twenty-five.3% of the surveyed children were attending the day-care center and 53.0% lived in Yiwu city for more than 6 months. More than half of the surveyed mothers were more than 30 y of age and 63.6% of them received junior middle school or less. Of all the surveyed mothers, 62.9% were housewives and only 38.3% of their family earned more than 500$(the exchange rate of RMB vs. $ is almost 6:1) per month. 70.4% of the surveyed mothers had a positive awareness of vaccination and 81.1% of them were satisfied with the immunization service they received ().
Table 1. Demographic characteristics of migrant children aged 1–4 y and their family, based on face to face interview in Yiwu, 2014
Overall immunization coverage
The immunization coverage rates for NIP and non-NIP vaccines were presented in. In general, all NIP vaccines showed higher coverage rates compared with the non-NIP vaccines. The coverage rates of vaccines scheduled at ≤ 12 m were 98.1100%– for NIP vaccines while 0%-27.7% for non-NIP vaccines. The coverage rates of vaccines scheduled at ≤ 24 m were 93.9%-96.3% for NIP vaccines while 0%-74.8% for non-NIP vaccines. The coverage rates of vaccines scheduled at ≤ 36 m were 87.9% for NIP vaccines while 4.5% for non-NIP vaccines. For NIP vaccines, the coverage rates of vaccines scheduled at ≤ 24 m were lower than that of vaccines scheduled at ≤ 12 m (93.9%-96.3% vs 98.1%-100.0%). However, the coverage rates of non-NIP vaccines scheduled at ≤ 24 m were higher than that of vaccines scheduled at ≤ 12 m (0%-74.8% vs 0%-27.7%). Among non-NIP vaccines, the VarV recorded the highest coverage of 74.8%, while the PCV7 record the lowest coverage of 0% for both primary doses (≥ 3 doses) and boost dose (≥ 4 dose).
Table 2. Estimated vaccination coverage among migrant children aged 1–4 y by selected vaccines and doses, based on face to face interview in Yiwu, 2014
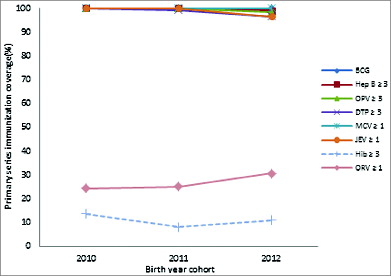
Coverage of primary series vaccination across birth cohorts
Among all 3 birth cohorts (born from 1 June 2010 to 31 May 2013), the primary series immunization coverage rates were higher for the NIP vaccines than that for the non-NIP vaccines(, N=423). The immunization coverage rates of BCG and MCV remained at 100% across all 3 birth cohorts, while the coverage for Hep B, OPV, DTP, JEV decreased slightly from 100% for 2010 birth cohort to 99.0%, 98.6%, 96.7%, 96.7% for 2012 birth cohort, respectively. The immunization coverage for ORV primary series was lowest in 2010 birth cohort by 24.2%, and highest in 2012 cohort with 30.6%. Although coverage of ORV remained relatively higher than that of Hib across all 3 cohorts, the coverage was still lower than that of NIP vaccines. The coverage for Hib fluctuated across all birth cohorts and tended to decrease slightly over the years.
Figure 1. Trends in primary series immunization coverage of migrant children for selected vaccines(doses), by birth cohorts(born from 1 June 2010 to 31 May 2013),based on face to face interview in Yiwu, 2014(N=423).PCV7 was excluded from the analysis due to the coverage of PCV7 was zero across all the 3 birth cohorts.
Determinants associated with coverage of non-NIP vaccines
We found born status, siblings, duration of living in surveyed areas, family income per month were associated with the coverage of Hib in the univariate analysis(P < 0.1) and these 4 determinants were included in the logistic regression analysis for uptake of Hib. Similarly, 6 determinants including siblings, duration of living in surveyed areas, mother's age, mother's occupation status, family income per month, mother’ s awareness of importance of vaccination were included in the logistic regression analysis for uptake of ORV as those variables with a P < 0.1 in the univariate analysis. Nine determinants including born status, siblings, breast milk feeding, duration of living in surveyed areas, mother's age, mother's education level, mother's occupation status, family income per month, mother’ s awareness of importance of vaccination were included in the logistic regression analysis for uptake of VarV as those variables with a P < 0.1 in the univariate analysis ().
Table 3. Determinants associated with coverage of Non-NIP vaccines among migrant children aged 1-4 years, based on face to face interview in Yiwu, 2014
The socio-demographic determinants associated with the coverage of 3 non-NIP vaccines(Hib, ORV, VarV) in the single-level logistic regression analysis were presented in. The risk factors significantly associated with a lower coverage of Hib for migrant children were more siblings in the family, shorter duration of living in the surveyed areas and lower family income per month. The risk factors significantly associated with a lower coverage of ORV for migrant children were more siblings, shorter duration of living in the surveyed areas, child with working mother, lower family income per month, and mother with a negative awareness of vaccination. The risk factors significantly associated with a lower coverage of VarV for migrant children were more siblings, shorter duration of living in the surveyed areas, mother with a lower education level, lower family income per month, as well as mother with a negative awareness of vaccination.
Discussion
The face-to-face interview survey of 423 children comparing coverage rates between NIP and non-NIP vaccines implicated that the immunization coverage rates of non-NIP vaccines were significantly lower than that of NIP vaccines in Yiwu. The coverage for NIP vaccines ranged between 87.9% and 100.0%, while the coverage for non-NIP vaccines ranged between 0% between 74.8%. Our observation agreed with previous reports from USCitation13 and SwitzerlandCitation14 that showed the lower immunization coverage for newly introduced vaccines compared to the traditionally recommended vaccines. The main reason for that in US was the shortage of vaccines, which might had affected accessibility to these new vaccines. These shortages affected children and health-care providers. For example, if vaccine was unavailable at an immunization clinic visit, another visit could have been made at a later time when vaccine was available. Furthermore, according to our previous study, the public perception and training of immunization staff require additional time since newly developed vaccines are introduced in the market. Besides, the limited existing public health resources would also restrict the utilization of the vaccine.Citation15 This delay in widely application of the vaccine would be accelerated by the inclusion of the vaccine into NIP. However, the expansion of NIP is limited not only in lower socio-economic developing areas but also in developed areas like Yiwu. The reasons for this lag are multi-factorial, but political commitment is crucial.
Although challenges in funding limited the impetus for expansion of NIP, rapid increase in coverage of NIP vaccines among migrant children had been made in recent years in Yiwu. It may be due to the intervention since 2009: first, financial reimbursements by local government to providers with a 5 CNY per doses for each child (including migrant child); second, vaccination training program toward the immunization staff; third, continuous improvement program on the accessibility and service quality of immunization clinics in Yiwu. By implementing the package of interventions, an increase in coverage for NIP vaccines was expected. Coverage of 98.1100%– for primary series of all NIP vaccines in this study was higher than the previous similar survey conducted in 2011 in Yiwu, which estimated the coverage of NIP vaccines among migrant children to be 63.9%-70.0%.Citation16
The difference in immunization coverage among non-NIP vaccines may resulted from the difference in the years of introduction of the vaccine. The VarV vaccine, which was introduced in the late 1990s, has now reached a plateau of coverage of up to 74.8%, however, was still lower than that of any NIP vaccine such as DTP, OPV and Hep B. The PCV7, which was introduced in 2008, showed a vaccination coverage of zero for a series of 3 doses scheduled at ≤ 12months, and for Hib and ORV, which was introduced in 2000–2002, now had coverage of up to10.4% and 27.7% for its primary vaccination, respectively. However, the coverage of Hib still remained lower compared with VarV which was introduced at a period. According to the previous studies,Citation17,18 misunderstanding of the disease burden and potential effect of the vaccine might be the main reasons. People always underestimate the hazard of bacterial infections disease like Haemophilus influenza type b for abuse of antibiotics in clinical treatment in China. The lower coverage of non-NIP vaccines may also result in the accumulation of susceptible population and increase of the risk of disease resurgence consequently.
The maternal determinants identified in our study for immunization coverage of non-NIP vaccines, such as lower education level, mother with a job, mother’ s poor awareness of vaccination, were in agreement with the findings of previous studies.Citation19–25 There were some reasons for that: first, education level may influence mother's knowledge of and attitude and behavior to take advantage of vaccination service for her child; second, mothers with jobs may not have enough time to spare for the primary healthcare including immunization, and may be less aware of the information on immunization.
Our study indicated that having more than one children, lower family income, and duration of living in the surveyed area were significant risk factors for lower uptake of non-NIP vaccines. There probably some reasons for that: first, parental attention may be diverted by the presence of multiple children in the household; second, as some non-NIP vaccines were expensive(e.g. the vaccination fee for PCV7 was approximately 133.3$), lower family income may restrict the expenses on the self-paid vaccines; third, we assumed that the migrant children with shorter duration living in the surveyed areas may face with the challenge to survive in a new environment with a higher cost of living and may have difficulties of adapting to a new sociocultural environment, while migrant children with a relative long time of living in the surveyed area, who were familiar with the city and enjoy some social support, were better able to avail themselves of health services.Citation16
There has been recent recognition of pneumococcus as a prevalent pathogen responsible for the child's invasive bacterial pulmonary infection in China. Among the pathogens isolated from these infections in children aged between 3 months and 5 years, pneumococcus has replaced H. influenza as the major etiologic agent.Citation26 Hence, an Immunization blank of PCV7 among migrant children was alarming and the impact factors of increasing coverage of PCV7 should be monitored and explored thoroughly in China as soon as possible.
Our findings are subject to 2 limitations. First, only children with immunization record booklet were included in this study, hence, these children were already at greater probability of being vaccinated. Second, timeliness of vaccination was not considered when calculating the immunization coverage and delayed vaccination was considered as vaccinated, therefore, immunization coverage for vaccines scheduled at 13–36 months may be underestimated compared to the vaccines scheduled at ≤ 12 months of age. Despite these limitations mentioned above, our study findings may well represent a median of immunization coverage between NIP vaccines and non-NIP vaccines in Yiwu. Therefore, our study provided meaningful estimates of NIP and non-NIP vaccines that were currently used and this study would be important for immunization program managers and for immunization policy makers.
Furthermore, the face-to-face survey method combined with immunization record booklet data guaranteed the quality of data of this study.
In conclusion, we reported disparities of immunization coverage between NIP vaccines and non-NIP vaccines currently used in Yiwu, east China. Although coverage of non-NIP vaccines has increased over time after introduction, it is important to note that the coverage rates of non-NIP vaccines still remain lower than that of NIP vaccines. We recommend continuing monitoring on the immunization coverage for both NIP and non-NIP vaccines to assess the vulnerability to the VPDs among Chinese children. The differences of coverage described in this study may provide evidence for public health decisions on identifying susceptible population and expanding the NIP to fulfill the demands of under-vaccinated children.
Materials and Methods
Background
As a developed city in east areas in China, Yiwu has a total area of 1105.5 KmCitation2 with a 2 million population. Yiwu has already attracted more than 1 million migrants for its rapid social-economic development in recent years.Citation27 Most of these migrant people are mainly from undeveloped middle or western areas of China. Immunization clinics in Yiwu adopt the vaccination schedule recommended by the Chinese MoH, which stipulates children should vaccinate 11 NIP vaccines (22 doses)before the 7th birthday (). For analysis, we selected 8 NIP vaccines, namely BCG, Hep B, OPV, DTP, MCV, Hep A, JEV, MPV-a and selected 4 non-NIP vaccines, namely VarV, Hib, ORV, PCV. The vaccnation schedule of included non-NIP vaccines were also summarized in. We excluded the MPV-ac and DT from analysis for the reason that our target children was age 1–4 y We excluded the IPV from the analysis for the reason that some children may substitute IPV for OPV and we considered these children as vaccinated.Citation28 The time of introduction of the 4 non-NIP vaccines in Yiwu are as follows: VarV in 1998, Hib in 2000, ORV in 2002, PCV7 in 2008.
Table 4. Recommended immunization schedule of NIP vaccines and partial non-NIP vaccines for children aged <7 years in Yiwu
Migrants in our study refer to people living in an area without a household registration card issued by public security bureau of their current living areas. In this study, we determined the immigration status of children or their caregivers by checking their Resident ID Card or asking their residence address. Migrant children aged 1–4 years(born from 1 June 2010 to 31 May 2013) who had lived in the surveyed areas continuously for more than one month, who should to be identified and registered by the local immunization clinics,Citation16 were investigated. Migrant children can receive the local immunization service such as vaccination notification, immunization, health education after registration. It seems that children living in an area for a little over a month may not have had adequate time to get vaccinated, while that was not our interest in this study. Our study focused on the coverage of NIP and non-NIP vaccines for migrant children but not the performance of the immunization service system in Yiwu city. We documented the date of the last immigration to the surveyed areas of each migrant children in our interview, so we can calculate the length of time of the latest continuously living in the surveyed areas.
Sampling and data collection
The demographic data of each 13 town of Yiwu were collected by the staff of Yiwu Center for Disease Control and Prevention (CDC). Villages or communities where migrant people accounted for more than half of the total population were selected as our investigation sites. Finally, a total of 57 villages and communities were selected. The sampling procedure of this study was based on simple random sampling method. The sample size was calculated based on the following 4 parameters: a desired precision of 5% in the estimate of vaccinated children, an assumption coverage of 85%, a significance level of 0.05 and a design effect level of 2. Finally, 7 children per cluster for 57 clusters were determined as our sample size.
We got household list of each investigation site from local administrative office and used the random number to select one household as the first one to be surveyed. The target children whose immunization record booklets (green book) were available at the time of the interview were included in our study. If there was more than one target child in a household, the child whose birthday was the closest to the survey day was interviewed. After found the first eligible child, we continued choosing subsequent household located at the right of the previous one until 7 eligible children for each investigation site were interviewed.
A standardized, pretested questionnaire was used for face-to-face interviews in June, 2014. The data on vaccination dates, doses, and the types of vaccine were extracted from the immunization record booklets. Variables such as gender, birth status (born as preterm or full term infant), and number of siblings were collected. Maternal age, education level, the awareness and satisfaction of immunization service including family income were collected as categorical variables. Whether the child was breast milk-fed or not and past or current attendance to the daycare center was investigated for further assessing impact on coverage of non-NIP vaccines.
Definition
The immunization coverage was defined as the percentage of children who had received the recommended number of doses according to age at the surveyed time. Delayed vaccination was included in the total number of vaccinated doses. The primary series vaccination was defined as the vaccines (doses) scheduled to be given at ≤ 12 months of age.
Data analysis
To compare immunization coverage of vaccines scheduled at different age, we stratified the denominators as follows: children born from 1 June 2010 to 31 May 2013 was defined as the denominator for calculating the coverage of the vaccines scheduled at ≤ 12 months; children born from 1 June 2010 to 31 May 2012 was defined as the denominator for calculating the coverage of the vaccines scheduled at ≤ 24 months; and children born from 1 June 2010 to 31 May 2011 was defined as the denominator for calculating the coverage of the vaccines scheduled at ≤ 36 months. We also compared the immunization coverage between NIP and non-NIP vaccines. The surveyed children were also stratified into 3 cohorts to reflect birth-year-specific immunization coverage for primary series vaccination(vaccines scheduled at ≤ 12 months). These cohorts were children born between 1 June 2010 and 31 May 2011 for the 2010 birth cohort; children born between 1 June 2011 and 31 May 2012 for the 2011 birth cohort; children born between 1 June 2012 and 31 May 2013 for the 2012 birth cohort. We compared the vaccination coverage between NIP and non-NIP vaccines for each birth cohort.
We employed the single-level logistic regression model to analyze the independent variables associated with the coverage of Hib and ORV for all the surveyed children and the coverage of VarV for children born from 1 June 2010 to 31 May 2012. Each of the dependent variable was dichotomized as “immunized/not immunized” and the single-level logistic regression analysis was carried out separately. The variables with a p value <0.1 in the univariable analysis were then included in the multivariable regression using backward likelihood ratio method. The use of a more usual p value (e.g., 0.05) often fails to identify variables known to be important, while the use of a higher p value has the disadvantage of including variables that are of questionable importance. Adjusted odds ratio with 95% confidence intervals (CIs) for each variable was also calculated. The significant level was set at a p value of 0.05. All the analysis above applied Statistics Package for Social Science (SPSS) software, version 13. 0 (SPSS Inc., Chicago, IL, USA).
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Ethics Statement
This study was approved by the Ethical Review Board of Zhejiang Provincial Center for Disease Control and Prevention. In each household surveyed, the informed consent form on behalf of children and their caregivers enrolled was discussed with children’ s caregivers, and signed by one of them once there was a decision to participate.
Acknowledgments
We would like to thank the Yiwu health bureau for their invaluable support, relative community leaders for their constant help. In addition, we would like to thank all the health workers from Yiwu CDC who conducted the interviews and data collection. Likewise, we thank Xu Zhu from UNICEF China, and Dr. Yiming Zhu from Zhejiang University for great assistance in this study.
Funding
Our study was funded by UNICEF China.
References
- Muhsen K, Abed El-Hai R, Amit-Aharon A, Nehama H, Gondia M, Davidovitch N, Goren S, Cohen D. Risk factors of underutilization of childhood immunizations in ultraorthodox Jewish communities in Israel despite high access to health care services. Vaccine 2012; 30:2109-15; PMID:22285273; http://dx.doi.org/10.1016/j.vaccine.2012.01.044
- Lee JW. Child survival: a global health challenge. Lancet 2003; 362:262; PMID:12892954; http://dx.doi.org/10.1016/S0140-6736(03)14006-8
- Okwo-Bele JM, Cherian T. The expanded programme on immunization: a lasting legacy of smallpox eradication. Vaccine 2011; 29 4:D74-9; PMID:22486980; http://dx.doi.org/10.1016/j.vaccine.2012.01.080
- Zheng J, Zhou Y, Wang H, Liang X. The role of the china experts advisory committee on immunization program. Vaccine 2010; 28 1:A84-7; PMID:20413004; http://dx.doi.org/10.1016/j.vaccine.2010.02.039
- Wu WD, Liu DW, Cao L. [Study on the estimation of routine immunization coverage of china, 2005-2007]. Zhongguo yi miao he mian yi 2009; 15:363-6; PMID:20077740
- Cui FQ, Gofin R. Immunization coverage and its determinants in children aged 12-23 months in gansu, china. Vaccine 2007; 25:664-71; PMID:17049682; http://dx.doi.org/10.1016/j.vaccine.2006.08.027
- Ma C, Hao L, Zhang Y, Su Q, Rodewald L, An Z, Yu W, Ma J, Wen N, Wang H., et al. Monitoring progress towards the elimination of measles in china: an analysis of measles surveillance data. Bull W H O 2014; 92:340-7; PMID:24839323; http://dx.doi.org/10.2471/BLT.13.130195
- Zou LP, Yang G, Ding YX, Wang HY. Two decades of battle against polio: opening a window to examine public health in china. Int J Infect Dis 2010; 14 3:e9-e13; PMID:20591714; http://dx.doi.org/10.1016/j.ijid.2010.02.2252
- Yaméogo KR, Perry RT, Yaméogo A, Kambiré C, Kondé MK, Nshimirimana D, Kezaala R, Hersh BS, Cairns KL, Strebel P. Migration as a risk factor for measles after a mass vaccination campaign, burkina faso, 2002. Int J Epidemiol 2004; 34: 556-64; PMID:15659463; http://dx.doi.org/10.1093/ije/dyi001
- Joe W. Intersectional inequalities in immunization in India, 1992-93 to 2005-06: a progress assessment. Health Policy Plan 2014; PMID:24740707
- Van Malderen C, Ogali I, Khasakhala A, Muchiri SN, Sparks C, Van Oyen H, Speybroeck N. Decomposing Kenyan socio-economic inequalities in skilled birth attendance and measles immunization. Int J Equit Heal 2013; 12:3; PMID:23294938; http://dx.doi.org/10.1186/1475-9276-12-3
- Khowaja AR, Zaman U, Feroze A, Rizvi A, Zaidi AK. Routine EPI coverage: subdistrict inequalities and reasons for immunization failure in a rural setting in pakistan. Asia-Pac J Public Health 2011; PMID:22186395
- Centers for Disease C, Prevention. National, state, and local area vaccination coverage among children aged 19-35 months-united states, 2011. MMWR Morb Mortal Weekly Rep 2012; 61:689-96; PMID:22951450
- Hug S, Weibel D, Delaporte E, Gervaix A, Heininger U. Comparative coverage of supplementary and universally recommended immunizations in children at 24 months of age. Ped Infect Dis J 2012; 31:217-20; PMID:22094628; http://dx.doi.org/10.1097/INF.0b013e31823cbaa5
- Li Q, Hu Y, Zhong Y, Chen Y, Tang X, Guo J, Shen L. Using the immunization information system to determine vaccination coverage rates among children aged 1-7 years: a report from zhejiang province, china. Int J Environ Res Public Health 2014; 11:2713-28; PMID:24603495; http://dx.doi.org/10.3390/ijerph110302713
- Hu Y, Li Q, Chen E, Chen Y, Qi X. Determinants of childhood immunization uptake among socio-economically disadvantaged migrants in east china. Int J Env Res Public Health 2013; 10:2845-56; PMID:23839061; http://dx.doi.org/10.3390/ijerph10072845
- Wagner AL, Sun X, Montgomery JP, Huang Z, Boulton ML. The impact of residency and urbanicity on haemophilus influenzae type b and pneumococcal immunization in shanghai children: a retrospective cohort study. PloS one 2014; 9:e97800; PMID:24828814; http://dx.doi.org/10.1371/journal.pone.0097800
- Hu YY, Yu SJ, Liu G, Gao W, Yang YH. Antimicrobial susceptibility of haemophilus influenzae among children in beijing, china, 1999-2000. Acta Paed 2002; 91:136-40; PMID:11951998; http://dx.doi.org/10.1111/j.1651-2227.2002.tb01684.x
- Bobo JK, Gale JL, Thapa PB, Wassilak SG. Risk factors for delayed immunization in a random sample of 1163 children from oregon and washington. Pediatrics 1993; 91:308-14; PMID:8424004
- Essex C, Smale P, Geddis D. Immunisation status and demographic characteristics of new zealand infants at 1 year and 2 years of age. New Zealand Med J 1995; 108:244-6; PMID:7617328
- Siedler A, Hermann M, Schmitt HJ, Von Kries R. Consequences of delayed measles vaccination in germany. Ped Infect Dis J 2002; 21:826-30; PMID:12352803; http://dx.doi.org/10.1097/00006454-200209000-00008
- Matsumura T, Nakayama T, Okamoto S, Ito H. Measles vaccine coverage and factors related to uncompleted vaccination among 18-month-old and 36-month-old children in kyoto, japan. BMC Public Health 2005; 5:59; PMID:15935101; http://dx.doi.org/10.1186/1471-2458-5-59
- Ndiritu M, Cowgill KD, Ismail A, Chiphatsi S, Kamau T, Fegan G, Feikin DR, Newton CR, Scott JA. Immunization coverage and risk factors for failure to immunize within the expanded programme on immunization in kenya after introduction of new haemophilus influenzae type b and hepatitis b virus antigens. BMC Public Health 2006; 6:132; PMID:16707013; http://dx.doi.org/10.1186/1471-2458-6-132
- Kitamura T, Komada K, Xeuatvongsa A, Hachiya M. Factors affecting childhood immunization in lao people's democratic republic: a cross-sectional study from nationwide, population-based, multistage cluster sampling. Bioscience Trend 2013; 7:178-85; PMID:24056168
- Baba K, Okuno Y, Tanaka-Taya K, Okabe N. Immunization coverage and natural infection rates of vaccine-preventable diseases among children by questionnaire survey in 2005 in Japan. Vaccine 2011; 29:3089-92; PMID:20870055; http://dx.doi.org/10.1016/j.vaccine.2010.09.022
- Li MC, Zhang Q, Ren HY. [Analysis on pneumococcus isolated from part of china using serotype and pulsed-field gel electrophoresis]. Zhongguo yi miao he mian yi 2010; 16:265-9; PMID:20726273
- Hu Y, Li Q, Luo S, Lou L, Qi X, Xie S. Timeliness vaccination of measles containing vaccine and barriers to vaccination among migrant children in east china. PloS one 2013; 8:e73264; PMID:24013709; http://dx.doi.org/10.1371/journal.pone.0073264
- Che YC, Jiang L, Shao CW. [Feasibility study of using sabin-IPV immunization in post-eradication era in china]. Zhongguo yi miao he mian yi 2010; 16:72-5; PMID:20450079
