Abstract
The Expanded Program on Immunization (EPI) in Vietnam began in 1981 and reached a 87% national coverage rate in 1987. To investigate the vaccination coverage and trends in time of the EPI in Vietnam, 2 vaccine coverage cluster surveys have been conducted in 2003 and 2009. Information on EPI-vaccine coverage in children (aged 0–23 months – 7 y of age), in women of childbearing age and in pregnant women, was collected through ‘30 cluster surveys’ in 2003 and 2009 (according to the World Health Organization (WHO) methodology) and through routine annual EPI coverage reports for the period 2001–2008. By comparing both cluster survey studies with each other, as well as with routinely collected data, we aim to improve future evaluation of the vaccination coverage in Vietnam and deduce recommendations for the immunization program. According to both methods, the national targets were reached for most of the vaccines: over 90% of children are fully immunized by 1 y of age, 80% Tetanus Toxoid 2 Plus (TT2+) coverage is reached for pregnant women, and 90% TT2+ for childbearing aged women. The cluster surveys identified higher coverage rates compared to the routinely reported data in some provinces regarding the percentage of fully immunized children by the age of 1 year, and confirmed a low coverage rate for hepatitis B birth dose vaccination in all surveyed sites. Conclusion: Both methods of coverage assessment suggest that national targets are reached, for most but not all vaccines and not in all regions. Managing stock pile issues, addressing safety issues and tailoring policy for remote areas, are important elements to maintain and further improve these coverage figures.
Introduction
Vietnam is a country in transition, with an estimated 90 million inhabitants (2012), a large birth cohort (1.4 million births/year) and a high mortality among children under the age of 5 (mortality rate of 22/1000 live births).Citation1 Around 69% of the population lives in the rural areas.Citation2 Over the past years, Vietnam has achieved significant improvements in public health. The health care administration is organized in a 3-level system.Citation1 The tertiary level is the Ministry of Health (MoH), which formulates and executes health policy and programs in the country. At provincial level there are 63 provincial health bureaus, which follow MoH policies, but are organic parts of the provincial local governments under the Provincial People's Committees (PPCs). The primary level, or basic health network, includes district health centers, commune health centers and village health workers.Citation3
Administratively, Vietnam is divided into 4 Regions (north, central, highland and south), 63 provinces, approximately 700 districts and 11,145 communes. The commune health center (CHC) is staffed by 4 to 6 commune health workers (CHWs) including nurses, an assistant doctor and a doctor. Village health workers (VHWs), who are trained 3–6 months on basic health care and primary health care, and who receive a small salary, play a role in monitoring the target population for immunization and in health program communication in their village. Six geographical regions can be recognized in the country according to geographical specificities.
The Expanded Program on Immunization (EPI) in Vietnam is implemented at province level by the Preventive Medicine Centers (PMCs), under the guidance of the regional and national EPI offices. The next level are the District Medical Centers (DMC) followed by the Commune Health Centers (CHC). Monthly immunization services, conducted through fixed immunization sites, are active in almost all communes. In some mountainous or otherwise hardly accessible areas, mobile teams attempt to reach remote communities to administer routine vaccines every 2 or 3 months. The national immunization schedule for the period 2003 – 2009 is shown in .
Table 1. National Immunization Schedule in 2003 – 2009
The EPI started in Vietnam in 1981. The EPI includes vaccines against tetanus, diphtheria, hepatitis B, polio, measles, pertussis and BCG (). Since the start, the EPI was rapidly implemented in the target population (infants, pregnant women and women of childbearing age (CBAW)) in the whole country. There were sharp increases in routine coverage between 1986 and 1990, resulting in associated sharp declines in reported vaccine preventable diseases.Citation3 Annual routine EPI reports show that in 1987 a national coverage of 87% was reached among children under 1 y of age.Citation3 In 1991, Vietnam initiated the implementation of the National Plan for Poliomyelitis Eradication and Maternal and Neonatal Tetanus Elimination. Hepatitis B vaccine was introduced in EPI in 1997, however, due to the limited production capacity of the local vaccine manufacturer, the vaccine was only used in a limited number of districts. Hepatitis B vaccination was fully implemented nationwide as of 2003. Mass campaigns for a second dose of measles vaccine have been implemented in 2002–2003 and a national plan for Measles Elimination including a routine second vaccine dose at school entry was adopted in 2006. Vietnam was certified Polio free in 2000 and Maternal and Neonatal Tetanus has been eliminated in 2005.Citation3
There are 4 local vaccine producers in Vietnam supplying most of the vaccines that are used in the EPI including BCG, Hepatitis B, OPV, Measles, Diphtheria – Tetanus – Pertussis (DTP) and Tetanus Toxoid (TT). The National EPI has a cold chain system for distribution of the vaccines to the commune health centers where routine vaccination is carried out monthly for the target population.
Annual data on the coverage of the EPI in Vietnam are available through monthly gathered data from the CHC in routine reports. Two national vaccine coverage surveys, one in 2003 and one in 2009 have been conducted to validate the vaccine coverage in Vietnam measured in routine EPI surveillance in the period 2002 – 2008, to evaluate if EPI targets are reached at national level and to detect subnational coverage differences and pockets of under-vaccinated populations within the target population.
In this paper results of both cluster surveys are presented and compared with each other as well as with the annual coverage data from the routine reporting system. This offers the opportunity to assess the validity of both sources for coverage data in Vietnam and formulate recommendations for better coverage and follow up of the EPI in Vietnam for the future.
Results
Overall coverage rates and timeliness of the vaccination
The yearly coverage of the EPI for infants in the period 2001 – 2008 was higher than 90% country-wide, according to routinely collected coverage data.Citation4–11 Timeliness (age-appropriateness) of the vaccination cannot be calculated from these routine coverage data.
In both cluster surveys, most provinces had high coverage rates (over 93 %) of fully immunized children by one year of age. The calculated crude national estimate for full immunization rates of children, was 96% for the 2003 cluster survey and 95.2% for 2009.
The difference between the reported fully immunized children (FIC) by routine EPI (at province level) and the 2003 survey was less than 8%, regardless of timeliness (). In the cluster survey in 2009, Ben Tre and Lam Dong provinces had the lowest FIC rate at 1 y of age: 75% and 78% respectively (). But countrywide, there was no large difference between the FIC reported by routine EPI and the 2009 survey data except for Dac Nong province.
Figure 2. Rate (%) of fully immunized children with all routine EPI vaccines in house hold surveys in 2003 and 2009 within 1 y of age (FIC) and by survey's time; I: 95% Confidence interval (CI).

Table 2. Population groups for investigation of immunization history
Table 3. Comparison between the reported coverage EPI routine data in 2002 and coverage found by 30 cluster survey in 2003
In the 2003 survey, delayed vaccination is clearly observed in the mountainous and remote provinces of Ha Giang and Kon Tum with respectively 48.1 and 66.1% FIC offered in time. These provinces are respectively located in the Northern mountain and Central highland area of Vietnam.
Coverage per vaccine
Some lower coverage rates were observed for specific vaccines ().
Figure 3. EPI vaccine coverage rate (%) in Vietnam, 2001 – 2008, based on the routine annual EPI reporting system. TT2 Plus (TT2+) = at least 2 doses of tetanus vaccine.
Figure 4. Rate (%) of Protection of infants at birth (PAB) in the 2003 and 2009 surveys. Note: * An infant is considered to be protected at birth against neonatal tetanus if the mother has received 2 doses of tetanus toxoid during the last pregnancy, or at least 3 doses of tetanus toxoid at any time in the past; I: 95% Confidence interval (CI).
Figure 5. Coverage rate (%) of Measles dose 2 in surveyed provinces in 2009; I: 95% Confidence interval (CI).
DTP
A DTP stock pile problem affected the rate of infants receiving DTP under one year of age in 2002. DTP dose 3 vaccine coverage decreased from 96.2% (2001) to 74.8% as measured by routine data collection; children who missed DTP in 2002 received it during routine vaccination in 2003, and the coverage rate recovered to 99.0% in 2003.
Measles
Similarly, in 2007, there was a 10% decline in the national coverage rate of measles vaccine from 93.0% to 83.0% for children at 9 months of age, which could be explained by a stockpile problem.In both cluster surveys in 2003 and 2009, coverage of measles dose 1 exceeded 90%.
In 2002–2003, a mass campaign of measles vaccination in children from 9 months to 10 y of age was implemented nationwide. The measles vaccine coverage during the second dose campaign in 2002–2003 was 95.8% when measured on card only (95.2% – 96.5%) and 97.4% (96.9% – 97.9%) measured through card + history in the 2003 survey.
Hepatitis B
Routine collected data showed a sharp decline in the coverage of the hepatitis B birth dose (coverage was 27% in 2007 versus 64% in 2006) and of the third dose of hepatitis B vaccine (67% in 2007 vs. 93% in 2006). The coverage did not recover afterwards.
The 2009 survey showed low coverage for the hepatitis B birth dose at all surveyed provinces (). Hypotheses for these low coverages are explained in the discussion. Comparison of hepatitis B birth dose within 24 hours shows lower coverage measured by the 2009 survey than by routinely reported EPI data (2007) ().
Table 4. Comparison between the reported coverage EPI routine data in 2007 and coverage found by 30 cluster surveys
Tetanus vaccine immunization
In the cluster survey in 2003, protection of infants at birth (PAB) ranged from 62.7% to 97.2%; the range was from 76.0% to 99.0% for the 2009 cluster survey. Provinces with the lowest PAB rates were Ha Giang and Kon Tum in 2003 and Khanh Hoa and Lao Cai in 2009, respectively ().
The calculated crude national PAB estimate from the survey results, was 89% in 2002 and 90% in 2009.
Discussion
According to the routinely collected EPI data, vaccine coverage of most antigens in Vietnam in the period 2001–2008 reached the targets set by Vietnamese EPI. These target coverage rates include not only fully immunized children by 1 y of age (90%), but also TT2 Plus for pregnant woman (80%) and for CBAW (90%). The vaccination coverage cluster surveys of 2003 and 2009 confirmed that most of the EPI vaccines reached the targets set by the Vietnamese EPI. However, for the surveyed provinces the cluster survey methodology was more sensitive for the identification of lower coverage rates for some vaccines and for the timeliness (age-appropriateness) of immunisation. The method is a valuable tool for EPI vaccine coverage measurement and ensures high quality output of the surveys with acceptable expenditure as it is specifically designed for the EPI vaccine coverage measurement.Citation12-15
Difficult access to the villages, especially in mountainous and remote provinces (Ha Giang, Kon Tum and Dac Nong) can explain difficulties related to monitor and vaccinate target populations. In these provinces, delayed vaccination has been described resulting in lower FIC at one year of age. Lower PAB rates and TT2 Plus rates in pregnant woman are reported in the routinely collected EPI data compared to the data obtained in the cluster surveys (in particular in Ha Giang and Vinh Long in 2003), indicating some incompleteness of the data in routine EPI. This might be explained by reporting or training issues of health staff, as well as by problems to access the target population, in particular in remote provinces in Vietnam.
During the period 2001 – 2008, some coverage declines or lower rates were found in the routine coverage data and the cluster data, for specific vaccines. A first reason that could be identified, were short-term stock pile problems for both DTP and measles. In 2002, DTP3 vaccine coverage decreased due to a national stockpile problem; the coverage rate recovered to 99.0% the following year, higher than the global and South East Asian DTP3 coverage rate, respectively 84% and 77% (12). Similarly, in 2007, there was a 10 % decline in the national coverage rate of measles vaccine for children at 9 months of age. This was again associated with a national stockpile problem due to delay in measles vaccine importation. The coverage of the routine second measles vaccine dose for children at 6 y of age was most severely impacted by this stockpile problem. Most of the provinces gave priority to the first measles vaccine dose since timeliness for the second dose was less stringent (). Only a few provinces continued with the second measles dose in 2007. Stock pile problems do not have long term implications in general. Priorities were set during the DTP and measles vaccine shortage.Citation16 Good vaccine management practice should always be implemented to assure sufficient stock of vaccine for the whole country in a specific period.Citation17 However, the EPI will always be affected by vaccine shortage due to limitation of vaccine production, unless more vaccine manufacturers are involved in the production and purchase process.
The hepatitis B birth dose vaccination coverage was low in 2007 and 2008 possibly as a consequence of serious Adverse Events Following Immunisation (AEFIs) after administration of a hepatitis B birth dose in 2007. The 2009 survey showed that coverage for the hepatitis B birth dose in all surveyed provinces did not recover yet: the health staff continues to refer to the negative impact of AEFI after hepatitis B birth dose immunization in 2007, which lead to a temporary suspension of hepatitis B vaccine administration by the Ministry of Health (MoH). Though causal relation was not evidenced, a sharp decline was seen in coverage of the hepatitis B birth dose (27% in 2007 versus 64% in 2006) as well as of the third dose of hepatitis B vaccine (67% in 2007 vs. 93% in the previous year) which did not recover in the following year. In 2013 the reported hepatitis B birth dose coverage was higher than the global one (38%) and the South East Asian one (26%), but still less than in 2006 (56% versus 64%).Citation18,19 Additional issues could negatively affect the vaccine coverage rate of the hepatitis B birth dose: cold chain limitations for keeping hepatitis B vaccines in CHCs as reported in the 2009 review;Citation16 the false contraindication for vaccination of an infants' birth weight under 2.5 kg or any birth complication, and at home delivery implying difficult logistics for vaccination. Training of the health staff and investments in logistics could meet these important issues.Citation20 Strengthening the AEFI surveillance system and AEFI case investigation which can effectively identify causality and adequately answer the public, should be one of the new priorities.
In both surveys, with respect to the source for collection of immunization histories, “card + history” gave the most complete results. Due to many reasons, the immunization card may not be kept, the children's parents may not remember which vaccine and how many doses of each specific vaccine were administered; therefore checking the immunization register book at CHCs is necessary. In the survey in 2003, the coverage rate based on “card only” was 0–5% lower than “card + history”.
Some limitations are encountered in the present analysis. The national EPI has developed a good system of estimating the target population for calculation of the EPI coverage, but inconsistent implementation at sub-national levels leads to uncertainty about the size of the target population. As a consequence, over 100% coverage rate has been reported in the EPI reporting system (see methods section). In several places, drop-out rates are reported and these are explained as a consequence of migrating populations, mainly due to agricultural labor. Calculating target population from previous year figures not taking such migration into account, leads to denominator errors.Citation16 Finding lower administrative coverage than survey-based coverage may mean that denominators are over-estimated. The denominator is the birth cohort per year and is available at each level per year. However, the link between the individual and the denominator cannot be made due to aggregated reporting. The strength of the cluster surveys is that they avoid this problem, and thus represent a more reliable source of information.
For better monitoring of timeliness of EPI vaccination, the National EPI should develop a registering and reporting system that can manage efficiently the vaccination date of the children and can report the most accurate figure of FIC.Citation21
In the Western Pacific region, the WHO regional office has set immunization milestones of maintaining polio eradication, maternal and neonatal tetanus elimination, measles elimination and for further reducing HBsAg prevalence among 5-year-old children to less than 1% by 2017. Vietnam has been working hard to obtain high coverage rates for most EPI vaccines, to maintain polio eradication and neonatal tetanus elimination, and head toward measles elimination and control of hepatitis B.Citation22 The data presented in this paper confirm that Vietnam reaches very high EPI vaccine coverage rates, but work remains to be accomplished in the future to address the specific immunization issues.
Conclusion
Despite some isolated lower vaccine coverage rates, vaccine coverage of most antigens in Vietnam in the period 2001–2008 reached the targets set by Vietnamese EPI for fully immunized children by 1 y of age (90%), for TT2 Plus for pregnant woman (80%) and for CBAW (90%). This is confirmed by 2 cluster surveys performed according the WHO methodology, however, some elements for improvement are identified in the present analysis.
As survey results and routine data were discordant for remote areas, a tailored policy for EPI reporting in mountainous and remote areas should be developed. For these areas recruitment of additional well-trained health staff should be considered.
Periodical EPI cluster survey should continue to be implemented as it offers useful information for management, guidance and monitoring of the EPI in all aspects, including the supply of sufficient vaccine stock piles and timeliness of the immunization programs. Periodic reviews of the EPI enable managers and stakeholders to assess progress, set priorities and plan future activities. Strengthening the AEFI surveillance system which can effectively identify causality and rapidly inform and reassure the public is one of the priorities in order to keep high coverage rates. The survey results help the EPI to evaluate the coverage rate of each individual vaccine, FIC and age-appropriateness and PAB. These recommendations support the Global Vaccine Action Plan of the WHO to improve equity in access and use of routine immunization services.Citation19 Strengthening this platform for routine immunization would in the future form the basis for introduction of new vaccines in Vietnam, like the second measles vaccine dose and rotavirus vaccination.Citation19
Materials and Methods
Data from cluster immunization coverage surveys are described together with data from the EPI routine reporting system.
Both systems report on all vaccines in EPI (): BCG, hepatitis B monovalent birth dose and infant doses, DTP, OPV and measles in children, and TT for pregnant women and childbearing aged women (CBAW). At individual level, the following definitions are used: 1) fully immunized child (FIC) means a child having received with one dose of BCG vaccine, 3 doses of DTP vaccine, 3 doses of OPV vaccine, 3 doses of hepatitis B vaccine and one dose of measles vaccine before the age of one year (); 2) An infant is considered to be protected at birth (PAB) against neonatal tetanus if the mother has received 2 doses of tetanus toxoid during the last pregnancy, or at least 3 doses of tetanus toxoid at any time in the past; 3) TT2plus in a woman means she has received at least 2 doses of tetanus vaccine after childhood and stating from the age of 15 y Administrative coverage data are reported annually to WHO and UNICEF. Administrative coverage is the number of vaccine doses administered to those in a specified target age group (numerator) divided by the estimated target population (denominator).Citation19,23 In Vietnam, numerator data are reported monthly in the routine reporting system as aggregated data. By day 5 of each month, the number of children who receive a specific dose of an EPI vaccine in the previous month, are reported from the commune level up to the district, the province, the regional levels and the National EPI as aggregated data. The number of FIC is also reported in the routine EPI data from the commune health level.
The denominator is the birth cohort per year and is available at each level per year. In monitoring immunization for under 1year old children, calculation of the denominator is based on the number of children born in the previous year and multiplied with the estimated population development rate. Denominators are also provided by the CHCs or Government Statistics Office (GSO) population, applied against the upcoming year's population as provided by GSO. In several places, drop-out rates are reported. Accumulated numbers and coverage rates for each vaccine are nationwide generated at the end of the year and included in the national EPI report: “Result of EPI activities.” National coverage and year-to-year trends are available from routine estimates for all vaccines in EPI.
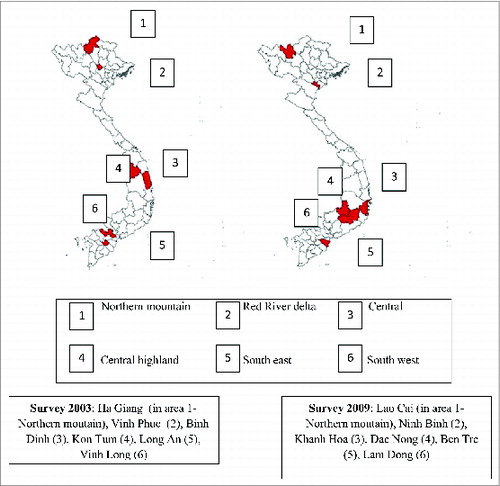
For the cluster surveys, a similar 3-stage sampling design was used for both surveys (2003 and 2009). In a first step, one province was selected at random from each of the 6 geographical areas (northern mountain, Red River delta, central, central highland, south east and south west). These areas were chosen based on geographical specificities to obtain geographical representativeness for the whole country, which are not represented in the 4 administrative regions. In a second step, within each province, 30 communes were randomly selected. In a third step, households were randomly chosen within the communes and visited at home, until the required number of individuals per target population (see ) of the cluster were included. This design is in accordance with the official WHO cluster survey methodology (WHO /EPI/ MLM/ 91.10).Citation24
In 2003, a total of 2526 children aged 0 to 23 months, 1800 children aged 16 months to 10 y of age and 1260 mothers of infants 0–11 months were investigated in 180 clusters within 6 randomly selected provinces in 6 geographical areas.
Similarly, a total of 1812 children aged 12 to 23 months, 1778 children aged 7 y of age and 1812 mothers of infants 0–11 months were included in 180 clusters of 6 randomized selected provinces in 6 geographical areas in the survey in 2009 ().
Investigation of the immunization history is based on: 1) interview with the principal caregiver of the child, 2) check of the child's immunization card and 3) check with the immunization registration book at the CHC. Standard questionnaires were designed and field-tested prior to each survey.
Administration and timing were collected for all vaccines in EPI to calculate the FIC. Receiving any of above mentioned vaccine doses later than 12 months of age is considered as delayed immunisation.
summarizes the target groups interviewed and cluster design of the sample for each of the investigated vaccinations.
The following definitions were used in both cluster surveys. 1)“Card only” means that information on vaccination history of the child is collected based on the immunization card available at home. 2) “Card + history” is when the information is collected based on immunization card and interview of the child's mother (parents) and/or checking information in the immunization register book at CHC. If the parents confirm the receipt of the vaccines, the vaccination is considered as given, even if it is not in the immunization registry book.
To calculate coverage estimates from the cluster survey data, first the coverage at provincial level was calculated as the average of the coverage in the selected communes, for each selected province. Confidence intervals at provincial level were calculated adjusting for the cluster design using Epi data for input data, and Stata for analysis data. The weighted average of the provincial coverages (weighted to the population of the geographical region they represent) was calculated to obtain a crude point estimate of the national coverage.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Funding
The manuscript was made possible with the help of FWO- Nafosted (project number FWO.2011.03). Nguyen Dac Trung received a SRS grant (short research stay) as a PhD student from VlirUos, Belgium, for the preparation of this manuscript. Elke Leuridan and Heidi Theeten are beneficiaries of a postdoctoral fellowship from the Fund for Scientific Research - Flanders (FWO). Support from a Methusalem grant of the Flemish government is awarded to Prof. Dr. Herman Goossens (University of Antwerp).
References
- GAVI. Vietnam country hub 2013. Available from: http://www.gavialliance.org/country/vietnam
- World Health Organization. A health financing review of Vietnam with a focus on social health insurance. 2011. Available from: http://www.who.int/health_financing/documents/oasis_f_11-vietnam.pdf
- National Expanded Programme on Immunization. 25 years Expanded Programme on Immunization. 2012.
- Vietnam EPI. Result of EPI activities in 2001, vaccine coverage. 2001.
- Vietnam EPI. Result of EPI activities in 2002, vaccine coverage. 2002.
- Vietnam EPI. Result of EPI activities in 2003 vaccine coverage. 2003.
- Vietnam EPI. Result of EPI activities in 2004, vaccine coverage. 2004.
- Vietnam EPI. Result of EPI activities in 2005, vaccine coverage. 2005.
- Vietnam EPI. Result of EPI activities in 2006, vaccine coverage. 2006.
- Vietnam EPI. Result of EPI activities in 2007, vaccine coverage. 2007.
- Vietnam EPI. Result of EPI activities in 2008, vaccine coverage. 2008.
- Harris JB, Gacic-Dobo M, Eggers R, Brown DW, Sodha SV. Global routine vaccination coverage, 2013. MMWR Morb Mortal Wkly Rep 2014; 63(46):1055-8; PMID:25412062
- Unicef. National EPI Review report, Vietnam, 2009. Available from: http://www.unicef.org/vietnam/EPI_NATIONAL _Review_Report_Vietnam_2009_Final.pdf
- World Health Organization. Effective Vaccine Management Initiative. Available from: http://www.who.int/immunization/programmes_systems/supply_chain/evm/en.
- Vietnam EPI. Result of EPI activities in 2013, vaccine coverage. 2013.
- World Health Organization. Immunization safety surveillance guideline. 2013. Available from: http://www.wpro.who.int/topics/immunization_safety/ImmunizationSafetySurveillance.pdf
- Burton A, Monasch R, Lautenbach B, Gacic-Dobo M, Neill M, Karimov R, et al. WHO and UNICEF estimates of national infant immunization coverage: methods and processes. Bull World Health Organ 2009; 87(7):535-41; PMID:19649368; http://dx.doi.org/10.2471/BLT.08.053819
- Henderson RH, Sundaresan T. Cluster sampling to assess immunization coverage: a review of experience with a simplified sampling method. Bull World Health Organ 1982; 60(2):253-60; PMID:6980735
- Lwanga SK, Abiprojo N. Immunization coverage surveys: methodological studies in Indonesia. Bull World Health Organ 1987; 65(6):847-53; PMID:3501738
- United Nations Children's Fund. Multiple Indicator Cluster Survey 3. 2005. Available from: http://www.childinfo.org/mics/mics3_background.html
- Luman ET, Barker LE, McCauley MM, Drews-Botsch C. Timeliness of childhood immunizations: a state-specific analysis. Am J Pub Health 2005; 95(8):1367-74; PMID:16043668; http://dx.doi.org/10.2105/AJPH.2004.046284
- World Health Organization. Immunization data by country. Available from: http://www.who.int/immunization/monitoring_surveillance/data/en/
- Zuber PL, Yameogo KR, Yameogo A, Otten MW, Jr. Use of administrative data to estimate mass vaccination campaign coverage, Burkina Faso, 1999. J Infect Dis 2003; 187(Suppl 1):S86-90. Epub 2003/05/02; PMID:12721897; http://dx.doi.org/10.1086/368052
- World Health Organization. Immunization coverage cluster survey. Reference manual. WHO/IVB/04/23. 2005. Available from: http://whqlibdoc.who.int/hq/2005/who_ivb_04.23.pdf
- Suarez-Castaneda E, Pezzoli L, Elas M, Baltrons R, Crespin-Elias EO, Pleitez OA, et al. Routine childhood vaccination programme coverage, El Salvador, 2011-In search of timeliness. Vaccine 2014; 32(4):437-44; PMID:24315884; http://dx.doi.org/10.1016/j.vaccine.2013.11.072