ABSTRACT
Background: An active response to a rubella outbreak may interrupt disease transmission, and outbreak response immunization (ORI) can increase immunity among persons who might otherwise not be protected. On March 17, 2014, a rubella outbreak was reported in a middle school in Guangzhou city, China. We conducted an investigation to assess impact of a policy of exclusion of cases from school and of ORI.
Methods: Active surveillance was used to find cases of rubella. Investigators interviewed teachers and reviewed the absentee records to determine implementation details of school exclusion. ORI was recommended on 2 occasions during the outbreak, one small-scale and one large-scale. Laboratory confirmation tests included serum IgM and IgG measurements to distinguish between acute infection and immunity. A serological survey in 4 classes was used to determine immunity status and identify symptomatic and asymptomatic cases.
Results: From February 17 to May 23, 2014, 162 rubella cases (24 laboratory-confirmed and 138 epidemiologically linked) were detected among 1,621 students. Cases ultimately occurred in 27 classes (72.97%) across 37 classes. In 11 classes in which exclusion from school was delayed by 1 or more days, the secondary attack rate was 12.30%, compared with 2.35% in 15 classes with immediate exclusion. ORI increased vaccine coverage from 25.83 % to 86.92%, and the final case of the epidemic was reported one month later. A serological survey of 91 students in 4 classes identified 15 cases, 6 of which were asymptomatic.
Conclusions: The outbreak happened in school with low rubella-containing vaccination coverage. Exclusion from school upon rash/fever onset was associated with lowering the secondary attack rate, but school exclusion alone was not able to stop this outbreak – a large ORI was needed. Assuring complete vaccination upon entry to school is likely to be necessary to ensure coverage is above the herd immunity threshold and prevent outbreaks from happening.
Introduction
Rubella is a generally mild disease transmitted through direct or droplet contact from nasopharyngeal secretions. Rubella infection in pregnant women can result in miscarriages, stillbirths, and congenital rubella syndrome (CRS), a constellation of birth defects that often includes cataracts, hearing loss, mental retardation, and congenital heart defects.Citation1 Prevention of CRS provides the motivation for prevention of rubella, which is highly contagious but preventable by use of rubella-containing vaccine (RCV).Citation2 In China, rubella vaccine was licensed in 1993, but was not recommended routinely for all children at that time. Instead, the vaccine was made available for individual protection and parents had to pay for the vaccine and its administration. In July 2008, China included rubella vaccine in the Expanded Program on Immunization (EPI), which not only made the vaccine free for all children up to 14 y of age, but it put rubella prevention into the immunization program's strategic planning.Citation3
Guangzhou has endemic transmission of rubella virus. Between 2007 and 2011, the average annual incidence of rubella was 3.71/100 000,Citation4 and the highest incidence was among children aged 0 to 19, accounting for 64.25% of reported cases. Rubella outbreaks often happen in settings such as schools and hospitals, in which nonimmune individuals are in close contact with a case. Active response to a rubella outbreak may interrupt disease transmission and, if response includes vaccination, can provide immunity to persons who might otherwise not be protected.
On March 17, 2014, a rubella outbreak was reported in a middle school in Guangzhou city, China. Because the outbreak spread quickly, Chinese Field Epidemiology Training Program fellows and Guangdong provincial CDC were invited to investigate and help control the outbreak, convening on April 24. We conducted an investigation to understand reasons for the outbreak, the impact of a school-exclusion policy and outbreak response immunization (ORI) in stopping the outbreak, and to develop strategies to prevent or manage similar outbreaks in the future. We report the findings of the investigation and response and our recommendations to the immunization program.
Results
The school had 1,621 students aged 13–16 y and 130 staff members. All students are day students, and they eat meals at home. The school canteen provides meals for some teachers. Students are not bussed to this school.
We identified a total of 168 rubella cases during the outbreak: 50 suspected cases, 88 probable cases, 24 confirmed cases, and 6 asymptomatic cases. The male to female ratio was 1.31:1, and the median age was 13.77 y (range: 10–17 years). Among the cases, 98 had not been vaccinated with rubella vaccine, 12 had received one RCV dose, 2 received at least 2 doses, and 52 had unknown rubella vaccination status. Initially, one class had cases, but by the end of the outbreak, cases had occurred in 27 of the 37 (72.97%) classes. The first epidemic peak was during Mar 10–24, and the second was from April 14 to May 5, based on the number of classes with new cases (). The school notified local health authorities of the outbreak on March 14. Local health authorities investigated the outbreak and implemented a school-exclusion policy in classes that had rubella cases. Children suspected to have rubella were required to be excluded from school immediately. Some classes had new teachers who were not familiar with the school's exclusion policy, and consequently, some students with rubella rashes were allowed to remain in school. In the 11 classes in which primary cases were allowed to stay in school one or more days while having a generalized rash, the secondary attack rate was 12.30%, compared with a secondary attack rate of 2.35% in the 15 classes in which students with generalized rashes were isolated immediately ().
Figure 1. Weekly distribution of the number of classes with new rubella cases, February 17 to May 23, 2014. The red line shows the percent of students vaccinated in the school.
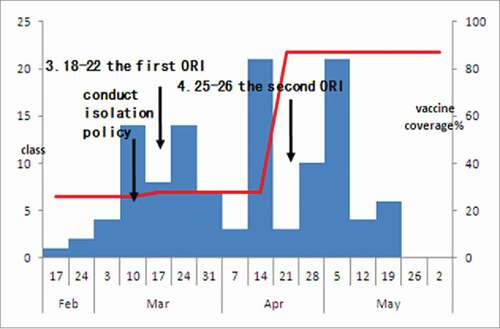
Table 1. Secondary attack rate of rubella by immediacy of school exclusion policy implementation
Table 2. Rubella serological results from 91 students in 4 random selected classes before the mass outbreak response immunization by their documented vaccination status
Outbreak response immunization was conducted as an emergency measure using contact tracing so that contacts of cases could be informed and vaccinated if they were not able to show documentation of receipt of at least one RCV dose. Based on vaccination record review, prior to the rubella outbreak, there were 419 students who had received RCV among the 1,621 students in the school. The average RCV coverage rate was 25.83% (419/1621), categorizing students who could not provide vaccination certificates as being unvaccinated.
ORI was conducted on 2 separate occasions during this outbreak (). The first ORI was based on contact tracing, in which school officials informed contacts of cases that they should receive rubella vaccine at a community service center on March 18. A total of 33 students received RCV by March 22. The average vaccine coverage rate increased to 27.88% (452/1621), and the outbreak continued. The second ORI was conducted at temporary vaccination points set up by a community service center at the school on April 26. In that vaccination effort, 957 students received RCV, and the average vaccine coverage rate increased to 86.92% (1409/1621). After the second ORI, 44 students were reported to have rubella before the epidemic ended. The last case happened on May 22.
Four classes were selected at random for a serological survey. The attack rates in these classes were 9.30%, 22.73%, 28.57% and 40.00%. We collected serum samples from 91 students. Based on IgM and IgG results, the rate of acute rubella infection was 16.48% (15 of 91). Among the 15 cases, 6 (40%) students did not show any symptoms of rubella. Of the 91 students tested, 30 (32.97%) were immune according to their IgG antibody results ().
Discussion
We have showed that (1) this school-based rubella outbreak was enabled by low rubella vaccine coverage, (2) a policy of exclusion from school immediately upon rash onset lowered the secondary attack rate of rubella virus, but was insufficient by itself to stop the outbreak, and (3) that a mass outbreak response immunization effort was necessary to stop the outbreak.
Rubella coverage was low at the start of the outbreak. Prior to the 2008 inclusion of rubella vaccines into China's Expanded Program on Immunization, RCVs were available, but parents had to pay out-of-pocket for rubella vaccine. Once included into the EPI system, RCVs were provided at no charge to parents. All of the students involved in the outbreak were born between 1998 and 2001 when the rubella vaccine coverage rate was low and when the national immunization program was not implementing a rubella prevention strategy. Low coverage with RCV created conditions that allowed this outbreak to occur.
At the beginning of outbreak, a school exclusion policy was not evenly implemented, as some teachers were unaware of the policy. Rubella virus spreads from primary cases to the secondary cases through air by coughing, sneezing or simply talking. Although the school exclusion policy was associated with a reduction of the rubella virus secondary attack rate from 12.30% to 2.35%, rubella virus transmission continued. The school exclusion policy was therefore partially effective at controlling the outbreak, but was insufficient to stop the outbreak. Because rubella vaccine coverage was low, we suggested that the school should conduct ORI, excluding students documented to have received RCV, who had any acute illness, or whose parents refused vaccination. After the second, much larger ORI, RCV coverage increased from 25.83% to 86.92%.In addition to the increased vaccine coverage, a certain number of asymptomatic rubella cases and the finish of the susceptible subjects along the outbreak likely build a immune barrier to stop transmission and end the outbreak. Our team evaluated the effect of ORI and school exclusion policy using Reed-Frost correction model.Citation5 The result showed if we did not conduct ORI, the disease maybe ended in August. It also showed if 70% of cases in each generation were isolated starting from the second generation, a decrease of 68.2% compared with not taking any control measures. During and following the outbreak, we educated teachers about rubella and CRS.
Our study provides supportive evidence that early detection and notification is important for successful control of a rubella outbreak. A school exclusion policy should be implemented immediately and comprehensively in order to reduce the secondary attack rate. An outbreak response immunization effort based on contact tracing was not successful, and ultimately, a large vaccination effort was needed to increase population immunity sufficient to stop transmission.
Our study was observational, rather than a controlled experiment, and so we can show associations only, not causality. However, our study was able to take advantage of a situation in which an intervention (exclusion from school for children with fever and rash) was unevenly applied across time, leading to a delay in the intervention for some classes. The differential delay allowed us to compare secondary attack rates between the classes using early or late exclusion to yield an estimation of impact of school exclusion policy. A limitation of our study is that our serological survey component was relatively small (n = 91). A second limitation is that not all cases had laboratory confirmation of rubella virus infection. However, all suspected and probable cases were geographically and temporally related to at least one laboratory-confirmed case. Asymptomatic rubella cases likely played an important role in the outbreak, as we identified 6 of 15 cases in the serological survey as being asymptomatic. But because not all students were tested, transmission patterns involving asymptomatic cases were not possible to determine.
Yang and colleagueCitation6 studied a rubella outbreak in a junior middle school and concluded that conducting emergency vaccination against rubella was necessary to control the outbreak. Our study supports their conclusion and provides additional information showing that exclusion from school was incompletely effective and controlling the outbreak, probably because immunization coverage levels were so low at the beginning of the outbreak. Exclusion measures are known to be important for reduction of transmission of respiration disease such as measles and varicella.Citation7-8
Lin and colleagueCitation9 compared a group that was vaccinated with a control group to estimate the effect of ORI. Although our study did not have a concurrent control group, we did have consistent findings. We were able to measure vaccine coverage over time to estimate ORI impact. Based on the R0 of rubella, the herd immunity coverage threshold is approximately 85%.Citation10 School facilitates spread rubella by crowding and bringing susceptible children to classes with low vaccine coverage. That the outbreak was stopped when coverage was above 80% is consistent with the herd immunity threshold.
As was seen in our study, a school was conducive to transmission of rubella. Making schools safe from rubella will require high RCV coverage. The school entry vaccination check program can ensure documentation of appropriate vaccination prior to school entry and should be strengthened to include all vaccine preventable diseases and help schools avoid the need for expensive outbreak responses. Therefore, we recommend strengthening the school entry vaccination check program as a preventive measure. In order to prevent CRS, we further recommend that health authorities consider developing a policy to vaccinate children born before 2008 and women of childbearing age before conception in order to control CRS.
Methods
For this school-based outbreak, we defined suspected cases as teachers or students with a generalized rash lasting 1–3 d that had onset between February 17 and May 23, 2014. A probable rubella case was defined as a suspected rubella case with fever >37.5°C and at least one of the following symptoms: arthralgia, arthritis, lymphadenopathy, or conjunctivitis.Citation11 Confirmed cases required a positive serologic test for rubella IgM antibody. Cases of asymptomatic rubella infection were considered in persons with a positive IgM result for rubella but without any of the following symptoms: rash, arthralgia, arthritis, lymphadenopathy, or conjunctivitis.
In the beginning of the outbreak, the local health authorities investigated the outbreak and implemented a school-exclusion policy in classes with rubella cases. Because the epidemic persisted, epidemiologists from the China Field Epidemiology Training Program and Guangdong CDC (authors) were invited to investigate the outbreak and make outbreak response recommendations. We reviewed medical records kept by the school's physician and absentee records kept by teachers to identify cases and to evaluate the degree of implementation of school-exclusion policy. Self-administered standardized questionnaires were sent to parents of all students to collect information about symptoms, results of physician consultations, disease histories, and school-exclusion times. Outbreak response immunization of students was recommended on 2 occasions, excluding students documented to have received rubella containing vaccine, who had any acute illness, or whose parents refused vaccination.
Serum samples were obtained to correlate immune status and vaccination documentation. We selected 4 classes at random to obtained blood specimens, with consent of their parents, on April 26, prior to conducting the second ORI. Laboratory tests included serum IgM and IgG measurements using enzyme-linked immunosorbent assay (Institute Virion/Serion, Germany), in combination, to distinguish between acute infection and immunity.Citation2
Data analysis
We performed the analyses in Excel software and Epi InfoTM 7.1.4 statistical software. We undertook a descriptive analysis of demographic data, clinical outcomes, vaccination history, and absentee records. Secondary attack rates (SARs) were calculated by dividing the number of secondary cases by the number of students with no history of current rubella minus those with primary and coprimary cases.Citation12 Secondary attack rates were used to calculate risk ratio (RR), and 95% confidence intervals (CIs).
Ethical considerations
This study was approved by the Institutional Ethics Committee of Guangdong Province Center for Disease Control and Prevention.
Disclosure of potential conflicts of interest
The authors declare no conflict of interest.
Acknowledgments
We gratefully acknowledge the health workers from Panyu CDC and their affiliated community health service center who participated in the field investigation. We thank teachers Peiqin Wei, Dr Chenggang Wu, Shuqing Zhao, Xiaoping Shao, Qi Zhu, Yu Liu, Qiru Su and Yan Li for critical support for this study. We thank Dr Lance Rodewald for critical support and review of the manuscript.
References
- Centers for Diseases Control and Prevention. Epidemiology and prevention of vaccine-preventable disease. 12th ed. Washington, DC: Public Health Foundation; 2011. p.275-90.
- World Health Organization. Rubella vaccine: WHO position paper. Wkly Epidemiol Rec 2011; 86:301-16; PMID:21766537
- Wu CG, Shu J, Han K, Tan Q, Lin JZ. Impact of different rubella immunization strategies on incidence of rubella in Guangdong province. Dis Surveill 2012; 27(2):110-3.
- Min C, Jianxiong X, Ming W. Analysis on the epidemiological characteristics of rubella in Guangzhou during 2007–2011. J Trop Med 2012; 12(12):1522-50.
- Mo XH, Chang CY, Jun L, et al. Evaluation on effect of case isolation and emergency vaccination in a rubella outbreak in Guangdong province [Chinese version]. Chinese J Vaccines Immun 2015; 21(5):233-538.
- Yang JX. Investigation and epidemic disposal of a rubella outbreak. Occup and Health 2013; 29(7):853-4.
- Delaporte E, Wyler CA, Iten A, Sudre P. Large measles outbreak in Geneva, Switzerland, January to August 2011: descriptive epidemiology and demonstration of quarantine effectiveness. Euro Surveil 2013; 18(6):1-8.
- Ma H, Fontaine R. Varicella outbreak among primary school students—Beijing, China, 2004. Morb Mortal Wkly Rep 2006; 55(Suppl 1):39-43.
- Yonggan L, Hanbin W, Chuangui L, et al. The observation of the emergency immunization with Attenuated Live Rubella Vaccine [Chinese version]. Chin J Prev Med 1996; 30(3):163.
- Fine PE. Herd immunity: history, theory, practice. Epidemiol Rev 1993; 15(2):265-302; PMID:8174658
- Centers for Diseases Control and Prevention. Epidemiology and prevention of vaccine-preventable disease. 12th ed. Washington, DC: Public Health Foundation; 2011. p.275-90.
- Ma H, Fontaine R. Varicella outbreak among primary school students-Beijing, China, 2004. MMWR Morb Mortal Wkly Rep 2006; 55(Suppl 1):39-43.
