ABSTRACT
Background
Approximately 40,000 new cases of anal cancer and 26,000 new cases of penile cancer occurred in 2012 worldwide. Human Papillomavirus (HPV) infection is responsible for 88.3% and 33.0% of these cancers, respectively. The aim of this study was to describe the hospital burden associated with malignant neoplasm (MN) and in situ carcinoma (ISC) in the anus and penis in Spain from 2009 to 2013.
Methods
This observational, retrospective study used discharge information obtained from the national surveillance system for hospital data, Conjunto Mínimo Básico de Datos, provided by the Ministry of Health.
Results
We found 3,668 hospitalizations due to MN and ISC in the anus for both genders, and more than 55% of these hospitalizations occurred in men and were associated with a lower median age of hospitalization (p < 0.001), higher average length of hospital stay (ALOS) (p = 0.0032), higher hospitalization costs (p < 0.001) and higher hospitalization rate (2.141 per 100,000 males aged > 14 y old and 1.604 per 100,000 women aged > 14 y old, p < 0.001) than in women. During the same period, 4,156 hospitalizations due to MN and ISC of the penis were registered. The hospitalization rate was 4.320 per 100,000 males aged > 14 y old. The hospitalization rate due to MN and ISC in the anus in males increased significantly during this period (p = 0.048).
Conclusion
Our study provides relevant information about the hospital burden of anal and penile MN and ISC in Spain. This information could be useful for cost effectiveness analysis of universal HPV vaccination and for future HPV vaccination impact monitoring in Spain, and for other countries of similar socioeconomic status.
Introduction
It is estimated that 40,000 new cases of anal cancer and 26,000 new cases of penile cancer occurred in 2012 worldwide. Citation1 Anal cancer is rare in the general population, but an increasing trend has been reported in developed regions. Citation2 In the United States, it is estimated to increase 2% per year. Citation3 The incidence rate is usually higher in women than in men, although men who have sex with men and immunocompromised subjects usually have higher rates of anal lesions. Citation2 Anal intraepithelial neoplasia (AIN) is the precursor lesion for anal cancer, but data about its prevalence and incidence are limited. Citation4
Penile cancer is also a rare condition and mostly affects men between 50 and 70 y old. This type of cancer is more common in less developed countries than in more developed ones. Citation2 In these regions, penile cancer can account for up to 10% of all male cancers. Citation5 There are several risk factors for penile cancer development: HPV infection, previous diagnosis of genital warts or other sexually transmitted diseases, local inflammation, tobacco or lack of circumcision. Citation6 Penile intraepithelial neoplasia (PeIN) is considered to be the precursor of penile cancer. Citation7
In Europe, it is estimated that 4,562 and 2,729 new cases of anal cancer and 1,545 and 1,093 new cases of AIN2/3 occur each year in females and males, respectively. Citation8
In Spain, according to the information provided by the Spanish Regional Cancer Registry REDECAN, it is estimated that the crude incidence rate for anal cancer ranges from 0.3–1.5 and 0.1–1.0 cases per 100,000 men or women, respectively; the crude incidence rate for penile cancer ranges from 1.5–3.9 cases per 100,000 men. Citation2 For AIN 2/3, the estimations, based on extrapolations from other countries with reliable registries for AIN, indicate that there are 99 and 138 new annual cases of AIN2/3 in men and women, respectively. Citation8
HPV infection is responsible for different percentages of anal and penile cancers as well as premalignant lesions across the world. According to the most recent studies, HPV DNA was detected in approximately 88.3% (95% CI: 85.1–91.0%) of anal cancer cases and 95.3% (95% CI: 84.2–99.4%) of AIN2/3 cases. Among these cancers, the highest prevalence of HPV infection was observed in the warty-basaloid subtype of squamous cell carcinomas, in younger patients and in the North America geographical region. Citation9
Among all HPV types, HPV 16 is the most prevalent genotype. It is estimated that infection by HPV 16/18 is present in 87% of all HPV positive anal cancers and 82.8% of all HPV positive high-grade precancerous lesions in the anus. Infection by HPV 31/33/45/52/58 is present in 7.9% of all HPV positive anal cancers and 3.4% of all HPV positive high-grade precancerous lesions. Citation10
For penile disease, the latest information indicates that HPV DNA was detected in 33.1% of penile cancers and 87.1% of high-grade squamous lesions in the penis. As happens in the anus, the warty basaloid histologic subtype has the highest HPV DNA prevalence. There were significant differences according to the geographic region, with the highest prevalence of HPV infection in Africa, Latin America and Europe and the lowest prevalence in Asia. The most frequent HPV type was 16 for both types of disease, precancerous lesions and cancers in the penis. Citation11
A previous study on the Spanish burden of hospitalizations due to malignant neoplasia (MN) of the penis and anus during 1997–2008 was published in 2012. This study showed that the hospitalizations due to anal and penis MN increased in Spain during the 11 y of the study period. Citation12
Approximately 85% and 80% of HPV positive anal cancer and AIN2/3 cases, respectively, are due to genotypes targeted by the available HPV vaccines: 6/11/16/18. It is expected that these percentages of coverage could increase with the use of the new nonavalent HPV vaccine, which also targets HPV31/33/45/52/58; these 9 types are responsible for 95% and 85% of anal cancer and AIN2/3, respectively. Citation13 In penile lesions and cancers, these 9 types are responsible for 46.9–63.1% of all HPV positive cases. Citation14, Citation15
Hospital discharge databases are useful for assessing the hospital burden of these diseases, and the national database of hospital discharge in Spain, provided by the Ministry of Health, Conjunto Mínimo Básico de Datos (CMBD), has been shown to be a reliable tool for studying hospitalizations associated with other infectious diseases. Citation16,Citation17
This epidemiological, descriptive, retrospective study aims to describe the burden of hospitalization associated with MN and in situ carcinoma (ISC) in the anus and penis, at a national level in Spain, during a 5-year period (2009–2013). This research is a follow-up to the previous study that explored the 11-year period from 1997–2008.
Results
Malignant neoplasia and in situ carcinoma in the anus
During the 5 y of the study period, we found 3,668 hospitalizations due to MN and ISC in the anus for both genders, and more than 55% of these hospitalizations occurred in men. Compared to females, these hospitalizations in males were associated with a lower median age of hospitalization (61.20 ± 13.98 versus 63.83 ± 14.90 y old; p < 0.001), higher average length of hospital stay (ALOS) (11.64 ± 16.80 vs. 10.16 ± 13.70 days; p = 0.0032) and higher hospitalization costs (6,565.67 ± 6,307.87 vs. 5,729.05 ± 4,783.60 euros; p < 0.001).
The hospitalization rate and mortality rate were also higher for men than women (p < 0.001 for both rates); however, we did not find significant differences in the case fatality rate between the genders (p = 0.128). In analyzing the hospitalization, mortality and case fatality rates according to age, we found a significant increasing trend (p < 0.001). However, in analyzing these rates according to the study period, these rates remained stable during these years without any significant changes.
443 of the 3,688 hospitalizations occurred in HIV patients, and most of them were males (300). An average patient without HIV coinfection (87.92% of all hospitalizations with anal cancer) had a predicted ALOS of 10.81 d (SE = 0.06), and a patient with HIV coinfection had a predicted ALOS of 12.00 d (SE = 0.18). Similarly, a patient without HIV coinfection incurred a predicted 5,676.02€ (SE = 98.30) of hospitalization costs, whereas a patient with HIV coinfection incurred a predicted 10,005.43€ (SE = 282.00). Additionally, coinfected patients were significantly younger (47.44, SD = .46) than patients without HIV (67.40 years, SD = 13.96).
Malignant neoplasia and in situ carcinoma in the anus in males
2,060 hospitalizations due to MN and ISC in the anus were registered in males from 2009 to 2013. Most of them (1,981) were coded as MN, and in 1,002 cases, MN was listed as the primary position. Only 79 hospitalizations were coded for ISC in males; however, their pattern was different: the mean age of hospitalization due to ISC was 53.95 ± 16.11 years, mean ALOS was 5.62 ± 7.49 and mean hospitalization costs were 5,363.75 ± 4,146.43 euros. These hospitalizations occurred in 1,776 men for MN and 72 men for ISC, corresponding to 1.16 average hospitalizations per male patient for MN and 1.10 average hospitalizations per male patient for ISC.
We observed no significant differences in the age of hospitalization or ALOS for MN and ISC by period. However, we observed significant differences in hospitalization costs (p = 0.0059) and a significant increasing trend in the hospitalization rate due to MN and ISC (p = 0.0408). The mean hospitalization rate over the period was 2.141 hospitalizations per 100,000 men aged > 14 y old (2.049–2.234); the highest peak was reached in 2013: 2.394 per 100,000 men (2.175–2.614).
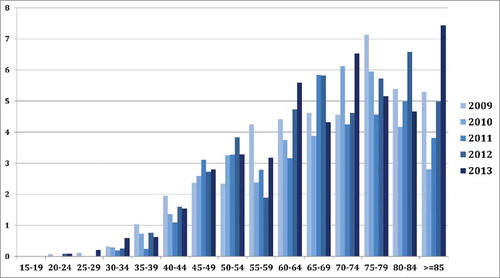
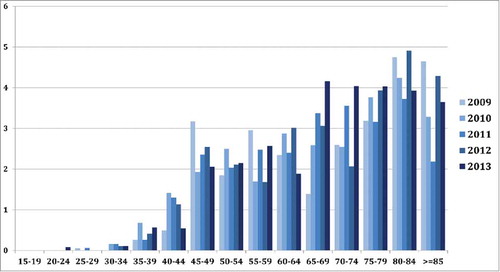
In and , we present all of the assessed variables for MN and ISC by age. We found significant differences in hospitalization costs by age (p = 0.072). We also observed a significant (p < 0.001) increase in the hospitalization rate, mortality rate and case fatality rate according to age (p < 0.001). In , the evolution of hospitalization rate according to the age group for the 5 y of the studied period is presented.
Table 1. Mean average length of hospital stay (ALOS) (days) and mean hospitalization cost (euros) of malignant neoplasia (MN) and in situ carcinoma (ISC) in anus in men and women and MN and ISC in penis in men, during the study period (2009–2013) per age group.
Table 2. Hospitalization rate (per 100,000 women or men aged > 14 y old), mortality rate (per 100,000 women or men aged > 14 y old) and case fatality rate (%) of MN and ISC in anus in men and women and MN and ISC in penis in men, during the study period (2009–2013) per age group.
Malignant neoplasia and in situ carcinoma in the anus in females
In females, 1,608 hospitalizations due to MN and ISC in the anus were coded during the 5 y of the study period. MN of the anus was coded more frequently than ISC (1,553 vs. 55, respectively). These hospitalizations occurred in 1,323 females for MN and 53 females for ISC, corresponding to 1.17 average hospitalizations per female patient for MN and 1.04 average hospitalizations per female patient for ISC. 739 of the 1,553 MN hospitalizations were coded as primary position. Compared with MN, hospitalizations due to ISC in females were associated with lower median age, 52.40 ±16.47 years; lower ALOS, 6.58 ± 11.05 days; and lower costs, 4,483.04 ± 3,608.57 euros.
We found no significant differences in ALOS for NM and ISC according to the study period (p = 0.5795), but hospitalization costs differed significantly during these years (p = 0.0298). The mean hospitalization rate was 1.604 per 100,000 women aged > 14 y old (1.526–1.683); mean mortality rate was 0.106 per 100,000 women aged > 14 y old (0.086–0.126); and mean case fatality rate was 6.592% (5.379–7.805%). These rates remained stable during the 5 y period.
We found significant differences for ALOS, hospitalization costs, hospitalization rate, mortality rate and case fatality rate by age group ( and ). We also observed significant increases in hospitalization rate (p < 0.001), mortality rate (p < 0.001) and case fatality rate (p = 0.030) with age. shows the hospitalization rates according to the age groups by year.
Malignant neoplasia and in situ carcinoma in the penis
4,156 hospitalizations due to MN and ISC of the penis were registered during the 5-year period. Most of them (n = 4,025) were related to MN of the penis, and only 158 were registered as ISC. These hospitalizations occurred in 3,326 patients for MN and in 144 patients for ISC, corresponding to 1.21 average hospitalizations per patient for MN and 1.10 hospitalizations per patient for ISC. In 2,610 of hospitalizations related to MN of the penis, MN was listed as the primary position. In the remaining cases, the most frequent first cause of hospitalization was MN in the lymph nodes in the inguinal region and lower limbs (CIE-9-MC: 196.5) in 152 hospitalizations and admission for antineoplasm chemotherapy (V58.11) in 143 hospitalizations. ISC appeared as the primary diagnosis in only 53.8% of the hospitalizations (n = 85) it was registered. In 8.2% and 4.4% of them, MN of the glands and unspecified MN of the penis were listed as the primary cause of hospitalization, respectively.
The mean age of hospitalizations of MN and ISC was 67.74 ± 14.49 y. The mean values for ALOS, hospitalization costs, hospitalization rate, mortality rate and case fatality rate are included in and .
No significant changes in the mean age of hospitalization were observed according to study period. However, we found significant differences for ALOS (p > 0.001) and hospitalizations costs; ALOS showed a decreasing trend during this period from 2009 to 2013 (8.91 ± 11.99 d in 2009, 6.99 ± 9.57 d in 2013). In contrast, the hospitalization rate, mortality rate and case fatality rate remained stable without significant changes.
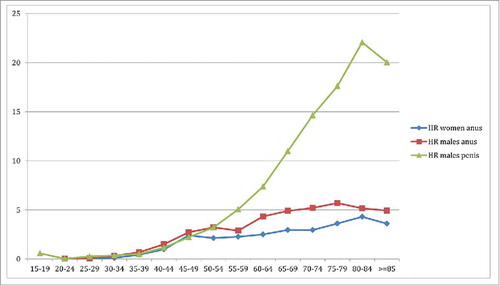
ALOS and hospitalization costs also differed significantly by age group (p = 0.0022 and p = 0.0037, respectively) (). The same happened for hospitalization rate, mortality rate and case fatality rate (p < 0.001). shows the hospitalization rate per age group from 2009 to 2013, and shows the hospitalization rate according to the age for MN and ISC in penis in males, MN and ISC in anus in males, and MN and ISC in anus in females. All the rates showed an increasing trend according to age; among the penis hospitalizations, this trend was even more pronounced.
Figure 3. Hospitalization rate (per 100,000 men aged > 14 y old) due to MN and ISC in penis in men per age group and by year of the study period.
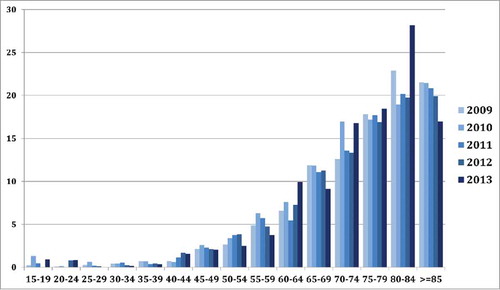
Figure 4. Hospitalization rate (HR) (per 100,000 women or men aged > 14 y old) due to anus NM+ISC in men; anus NM+ISC in women and penis NM+ISC in men during the study period (2009–2013) per age group.
An average patient without HIV coinfection (98.1% of all hospitalizations with penile cancer) had a predicted ALOS of 7.87 d (SE = 0.04), and a patient with HIV coinfection had a predicted ALOS of 9.62 d (SE = 0.36). Similarly, a patient without HIV coinfection incurred a predicted 5,176.31€ (SE = 56.06) of hospitalization costs, whereas a patient with HIV coinfection incurred a predicted 9,086.74€ (SE = 410.00). Additionally, coinfected patients were significantly younger (51.42 years, SD = 8.81) than patients without HIV (68.05 years, SD = 14.40).
Discussion
This study shows the hospital burden of MN and ISC in the anus and penis for both genders in Spain during a 5 y period from 2009–2013.
For anus location, the hospital burden has been shown to be higher in men than in women. Overall, more than half of the hospitalizations due to anal MN occurred in men. These results are consistent with data from the Spanish Regional Cancer Registry Citation2 but differ from findings from other countries. Citation8 These differences may be due to different sexual behaviors or by differences in the presence of HIV or other comorbidities in males and females. The mean age of hospitalization was lower in men, and moreover, the ALOS and mean hospitalization costs were also higher in men compared with women. Additionally, we observed a significant increasing trend of hospitalization rate due to anal MN and ISC in men by study period.
We also found an increase in hospitalization, mortality and case fatality rates for both genders by age. The same happened for penis MN and ISC.
It is important to mention that MN and ISC in the anus and penis presented with substantial differences. Hospitalization burden of MN was much more frequent than ISC, with several hospitalizations 25-fold higher than the number related to ISC. The mean age of hospitalization, ALOS, costs and case fatality rate were also lower for ISC than MN. It has to be considered that only ISC and MN requiring hospitalization are included in this database, so the reported ALOS may seem longer than expected, as only in-hospital treatments and no outpatient treatments are contributing to its calculation. Accordingly, invasive surgical treatments could be overrepresented. The significant increasing trend of the hospitalization rate due to MN and ISC in the anus in males could be explained in part by the overall increasing trend of anal cancer incidence that has been observed in other countries as UK. Citation18 Few data about hospital burden of these cancers is available, however, recent data from a literature review of the incidence trends of anal cancers in 18 countries of the 4 continents, Citation19 excluding Africa, showed that during 2006–2007, there was an increasing trend of this type of cancer in countries including Australia, Denmark, Canada, France, Italy, The Netherlands, USA and also UK, as previously mentioned. Some epidemiological studies have postulated that this increase is attributable to changes in sexual behavior that could lead to an increase in HPV infections. Citation18 These results are aligned with our findings in males. For females, we have observed no increasing trend; however, in Spain, the incidence rate of anal cancer is lower in females vs. males, probably due to sexual habits or lower incidence of risk factors such as HIV. Although CMBD does not allow us to differentiate men who have sex with men (MSM), the rates of anal cancer are highest in this population, and the incidence in this group is estimated to be equivalent to that for cervical cancer in an unscreened population, and even higher if we consider MSM HIV. Citation20 In this study, we also observed that an important number of anus cancer hospitalizations occurred in subjects with HIV.
We have estimated that the annual cost of hospitalizations due to MN and ISC in the anus and penis is more than 8.91 million euros. However, to assess the overall cost of anal and penis cancer, we should also consider other outpatient costs. In UK, the outpatient cost of anal cancer is estimated to range from 1,146–1,335 pounds per patient. Citation18 The highest hospitalization costs found in the youngest age cohort could be explained by specific characteristics of the tumor or by the present comorbidities, such as HIV which is more common in younger age groups.
Although there has been substantial progress in cervical cancer prevention due to screening in high developed countries, less progress has been made in the prevention of HPV related cancers in men, cancers for which screening interventions are not routinely available. Citation21
The quadrivalent HPV vaccine has been shown to be efficacious in preventing external genital lesions in men and, more specifically, to prevent AIN2/3 in men who have sex with men. Citation22,Citation23 The efficacy against PIN did not reach a significant level due to the small number of cases registered during the study. More recently, the nonavalent vaccine has shown to induce similar levels of immunogenicity for the 9 types of HPV in men aged 16–26 y old than in women aged 16–26 y old. The nonavalent vaccine provides similar levels of GMT (geometric mean titers) for anti HPV 6, 11, 16 and 18 as the tetravalent vaccine in men. These 2 findings strongly suggest that the new nonavalent vaccine could be as efficacious in men as in women, thereby offering men at least the same level of protection as the quadrivalent vaccine for the 4 common genotypes; and it should offer increased overall protection thanks to the inclusion of the new 5 genotypes. Citation24,Citation25
However, HPV vaccination in boys is not widespread. Countries including Australia, United States, Austria or Italy have already introduced a national universal vaccination program. Citation26,Citation27 The most common barrier to its introduction is its cost effectiveness. However, there are several factors to consider for an economic evaluation of a universal vaccination program, such as inclusion of high risk groups such as MSM, reductions in the vaccine costs during recent years, inclusion of non-cervical HPV related diseases, and the recent 2-dose schedule recommendation. Citation28 In Spain, the HPV vaccination program was introduced in 2007 but only targets 12-year old girls, with a 2-dose schedule and a vaccine coverage rate of 79%. Citation29-Citation31
This study presents some limitations due to the use of the CMBD database, which only records hospitalized cases, so we cannot estimate the incidence or prevalence rates. CMBD reliability is influenced by the quality of gathering clinical histories and hospital discharge codifications. Citation32 Moreover, there is a possibility of over-counting patients with multiple hospital admissions. Citation33 In any case, this study investigates the burden of hospitalization and not incidence, so we are interested in all episodes that require hospitalization, irrespective of the fact that they may occur in the same patient. We have to interpret mortality rate calculated with CMBD with caution, as deaths outside of the hospital were not considered. Despite these limitations, the hospital discharge database has shown to be an adequate tool for cancer surveillance. Citation34
In conclusion, our study presents the Spanish hospitalization burden of MN and ISC in the penis and anus for both genders from 2009–2013. These data are an important basis for public healthcare workers and payers to assess cost effectiveness of universal HPV vaccination and it could also be used to assess the future vaccination impact of a universal HPV vaccination program.
Methods
This analysis used information from CMBD, which contains data about admission and discharge dates, age, sex, geographical region, diagnosis, clinical procedures and discharge status for all hospitalizations in our country. It uses clinical codes from the Spanish version of the 9th Internal Classification of Diseases (CIE-9-MC). Citation35 It is estimated that it covers approximately 98% of public hospital admissions, covering 99.5% of the population in Spain Citation36 We assumed the same epidemiological characteristics for the population and hospitalizations not covered by CMBD and no difference in the age distribution of the population covered by public hospitals compared with the general population. Data are anonymized in origin by the Ministry of Health, and we received a waiver from the ethics committee for research of Rey Juan Carlos University.
We selected all hospital discharges related to MN of the anus (CIE-9-MC: 154.2 anal cancer, 154.3 unspecified anus), ISC of the anus (CIE-9-MC: 230.6 ISC of anus unspecified), MN of the penis (CIE-9-MC: 187, MN of the penis, and other male genital organs; 187.1 foreskin, 187.2 glans, 187.3 corpus of the penis, 187.4 unspecified penis, 184.5 epididymis, 187.6 spermatic cord, 187.7 scrotum, 187.8 other specified sites of male genital organs, 187.9 unspecified site male genital organ) and ISC of the penis (CIE-9-MC: 233.5, ISC of the penis) during a 5 y period (2009–2013). Citation35 We excluded data in patients up to 14 y of age, which is considered the pediatric population in Spain.
Statistical analysis: We calculated the average number of hospitalizations, the average length of hospital stay (ALOS) (days), the average hospitalization cost (euros), hospitalization and mortality rate (per 100,000 women/men aged > 14 y old), and case fatality rate (%), per year, age and gender, if diseases occurred in both females and males. For hospitalization and mortality rate calculations, we used the data of the female and male population aged > 14 y old from the municipal registries adjusted by the population targeted by hospitals covered by the CMBD as the denominator. The age, sex, and year-specific rates were calculated using the corresponding population as the denominator.
We used the Chi square test to assess significant differences in proportions and ANOVA for multiple comparisons. Poisson models were used to assess differences in the hospitalization and mortality rate (per 100,000 women or men aged > 14 y old) during the years of the study period (2009–2013), the age group and the gender. The hospitalization and mortality rates were used as dependent variables, and year, age and gender were used as independent variables if applicable.
All the results are reported with their corresponding 95% confidence intervals (95% CI). For all tests, we considered a p value less than 0.05 to be significant.
Disclosure of potential conflicts of interest
NL has worked for Sanofi Pasteur MSD Spain. AGM and RGP have received travel and research grants from Sanofi Pasteur MSD and GSK.
References
- Plummer M , de Martel C , Vignat J , Ferlay J , Bray F , Franceschi S. Global burden of cancers attribuitable to infections in 2012: a synthetic analysis. Lancet Global Health 2016; 4:e609-16; PMID:27470177
- Bruni L, Barrionuevo-Rosas L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Spain. Summary Report 7 October 2016. http://www.hpvcentre.net/statistics/reports/ESP.pdf. (Accessed 28 October 2016).
- Johnson LG , Madeleine MM , Newcomer LM , Schwartz SM , Daling JR . Anal cancer incidence and survival: the surveillance, epidemiology, and end results experience, 1973-2000. Cancer 2004; 101:281-8; PMID:15241824
- Nielsen A , Munk C , Kjaer SK . Trends in incidence of anal cancer and high-grade anal intraepithelial neoplasia in Denmark, 1978-2008. Int J Cancer 2012; 130:1168-73; PMID:21469144
- Ventimiglia E, Horenblas S, Muneer A, Salonia A. Human Papillomavirus Infection and Vaccination in males. European Urology Focus 2016; 2(4): 355-362. https://doi.org/10.1016/j.euf.2016.08.012
- Documento de Consenso de Sociedades Científicas Españolas: vacunación frente al virus del papilloma humano 2011. http://vacunasaep.org/sites/vacunasaep.org/files/VPH_Consenso_Sociedades_2011.pdf (Accessed 25 August 2016).
- Sudenga S , Ingles D , Pierce Campbell CM , Lin H , Fulp WJ , Messina JL , Stoler MH , Abrahamsen M , Villa LL , Lazcano-Ponce E , et al. Genital Human Papillomavirus infection progression to external genital lesions: the HIM study. European Urology 2015, 69(1):166-173; PMID:26051441
- Harwitg S, Baldauf JJ, Dominiak-Felden G, Simondon F, Alemany L, de Sanjose S, Castellsague X. Estimation of the epidemiological burden of HPV-related anogenital cancers, precancerous lesions, and genital warts in women and men in Europe: Potential additional benefit of a nine-valent second generation HPV vaccine compared to first generation HPV vaccines. Papillomavirus Research 2015; 1:90-100. http://www.sciencedirect.com/science/article/pii/S2405852115000099
- Alemany L , Saunier M , Alvarado-Cabrero I , Quirós B , Salmeron J , Shin H , Pirog EC , Guimerà N , Hernandez-Suarez G , Felix A , et al. Human papillomavirus DNA prevalence and type distribution in anal carcinomas worldwide. Int J Cancer 2015, 136:98-107; PMID:24817381
- Serrano B , de Sanjosé S , Tous S , Quiros B , Muñoz N , Bosch X , Alemany L . Human Papillomavirus genotype attribution for HPVs 6,11,16,18,31,33,45,52 and 58 in female anogenital lesions. European J Cancer 2015, 51(13):1732-41; PMID:26121913
- Alemany L , Cubilla A , Halec G , Kasamatsu E , Quirós B , Masferrer E , Tous S , Lloveras B , Hernández-Suarez G , Lonsdale R , et al. Role of Human Papillomavirus in Penile Carcinomas worldwide. European Urology 2016, 69 (5):953-961; PMID:26762611; https://doi.org/10.1016/j.eururo.2015.12.007
- Gil-Prieto R , Viguera Ester P , Alvaro-Meca A , San Martin Rodriguez M , Gil de Miguel A . The burden of hospitalizations for anus and penis neoplasm in Spain (1997-2008). Hum Vaccines Immunotherapeutics 2012; 8(2):201-207; PMID:22426377; https://doi.org/10.4161/hv.18388
- Pitisuttithum P , Velicer C , Luxembourg A . 9-valent HPV vaccine for cancers, pre-cancers and genital warts related to HPV. Expert Rev Vaccines 2015; 14 (11):1405-1419; PMID:26366475; https://doi.org/10.1586/14760584.2015.1089174
- De Sousa ID , Vidal FC , Branco Vidal JP , de Mello GC , do Desterro Soares Brandão Nascimento M , Brito LM . Prevalence of human papillomavirus in penile malignant tumors: viral genotyping and clinical aspects. BMC Urol 2015; 15:13; PMID:25887354; https://doi.org/10.1186/s12894-015-0007-8
- Miralles-Guri C , Bruni L , Cubilla AL , Castellsagué X , Bosch FX , de Sanjosé S . Human papillomavirus prevalence and type distribution in penile carcinoma. J Clin Pathol 2009; 62(10):870-878; PMID:19706632; https://doi.org/10.1136/jcp.2008.063149
- Gil A , San-Martín M , Gil R , Hernández V , Ribes J , González A . Burden of hospital admissions for cervical cancer in Spain during 1999-2002. Hum Vaccin 2007; 3:276-80; PMID:17938579; https://doi.org/10.4161/hv.4875
- Gil-Prieto R , Pascual-Garcia R , Walter S , Álvaro-Meca A , Gil-de-Miguel A . Risk of hospitalization due to pneumococcal disease in adults in Spain. The CORIENNE study . Hum Vaccines Immunotherapy 2016; 12(7):1900-5
- Keeping ST , Tempest MJ , Stephens SJ , Carroll SM , Nugent KP , O´Dwyer ST . The cost of anal cancer in England: retrospective hospital data analysis and Markov model. BMC Public Health 2014, 14: 1123; PMID:25361522; https://doi.org/10.1186/1471-2458-14-1123
- Islami F , Ferlay J , Lortet-Tieulent J , Bray F , Jemal A . International trends in anal cancer incidence rates. Int J Epidemiol 2016, 1-15; PMID:27433568
- Stanley M . HPV vaccination in boys and men. Human Vaccines Immunotherapeutics 2014, 10(7): 1-3; PMID:24832715; https://doi.org/10.4161/hv.29138
- Giuliano AR , Kreimer AR , de Sanjose S . The beginning of the end: vaccine prevention of HPV driven cancers. J Natl Cancer Institute 2015, 107(6):djv128; PMID:25911509; https://doi.org/10.1093/jnci/djv128
- Giuliano AR , Palefsky JM , Goldstone S , Moreira ED, Jr , Penny ME , Aranda C , Vardas E , Moi H , Jessen H , Hillman R , et al. Efficacy of quadrivalent HPV vaccine against HPV Infection and disease in males. N Engl J Med 2011; 364(5):401-11; PMID:21288094; https://doi.org/10.1056/NEJMoa0909537
- Palefsky JM , Giuliano AR , Goldstone S , Moreira ED, Jr , Aranda C , Jessen H , Hillman R , Ferris D , Coutlee F , Stoler MH , et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med 2011; 365(17):1576-85; PMID:22029979; https://doi.org/10.1056/NEJMoa1010971
- Castellsague X , Giuliano AR , Goldstone S , Guevara A , Mogensen O , Palefsky JM , Group T , Shields C , Liu K , Maansson R , et al. Immunogenicity and safety of the 9-valent HPV vaccine in men. Vaccine 2015; 33(48):6892-6901; PMID:26144901; https://doi.org/10.1016/j.vaccine.2015.06.088
- Van Damme P , Meijer C , Kieninger D , Schuyleman A , Thomas S , Luxembourg A , Baudin M . A phase III clinical study to compare the immunogenicity and safety of the 9-valent and quadrivalent HPV vaccines in men. Vaccine 2016; 34(35):4205-12; PMID:27354258; https://doi.org/10.1016/j.vaccine.2016.06.056
- Audisio RA , Icardi G , Isodori AM , Liverani CA , Lombardi A , Mariani L , Mennini FS , Mitchell DA , Peracino A , Pecorelli S , et al. Public health Value of universal HPV vaccination. Crit Rev Oncol Hematol 2016; 97:157-67; PMID:26346895; https://doi.org/10.1016/j.critrevonc.2015.07.015
- Piano Nazionale Prevenzione Vaccinale PNPV 2016-2018. http://www.quotidianosanita.it/allegati/allegato1955037.pdf (Accessed October 2016)
- Newman P , Lacombe-Duncan A . Human Papillomavirus vaccination for men: advancing policy and practice. Future Virol 2014, 9(12):1033-1047; https://doi.org/10.2217/fvl.14.91
- Consejo Interterritorial del sistema nacional de salud. Acuerdo no: 655 Pleno: 10 de octubre de 2007 Acta no: 79. http://www.msps.es/organizacion/consejoInterterri/docs/655.pdf. (Accessed 25 August 2016).
- Ministerio de Sanidad, Servicios Sociales e Igualdad [Web]. Calendarios de Comunidades y Ciudades Autónomas. https://www.msssi.gob.es/ciudadanos/proteccionSalud/vacunaciones/docs/CalendarioVacunacion2016.pdf (Accessed 29 October 2016 ).
- HPV vaccination coverage rates. http://www.msssi.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/docs/CoberturasVacunacion/Tabla8.pdf (Accessed 30 October 2016 ).
- Peiro S , Librero J . Evaluación de la calidad a partir del conjunto mínimo de datos básicos al alta hospitalaria. Rev Neurol 1999; 29:651-61; PMID:10599116
- Huff L, Bogdan G, Burke K, Hayes E, Perry W, Graham L, Lentzner H. Using hospital discharge data for disease surveillance. Public Health Rep 1996; 111(1):78. PMID:8610197
- Penberthy L , McClish D , Pugh A , Smith W , Manning C , Retchin S . Using hospital discharge files to enhance cancer surveillance. Am J Epidemiol 2003; 158:27-34; PMID:12835284; https://doi.org/10.1093/aje/kwg108
- Ministerio de Sanidad, Servicios Sociales e Igualdad. CLASIFICACIÓN INTERNACIONAL DE ENFERMEDADES 10.a REVISIÓN, MODIFICACIÓN CLÍNICA. EDICIÓN ESPAÑOLA. https://eciemaps.mspsi.es/ecieMaps/browser/index_9_mc.html#search=233.3&flags=111100&flagsLT=11111111&searchId=1471948733037&indiceAlfabetico=&listaTabular=233.3&expand=0&clasification=&version (Accessed 29 October 2016).
- Rivero Cuadrado A . Análisis y desarrollo de los GDR en el Sistema Nacional de Salud. http://www.msssi.gob.es/estadEstudios/estadisticas/docs/analisis.pdf. (Accessed 29 October 2016 ).