ABSTRACT
The cost-effectiveness of the 4 Pillars™ Practice Transformation Program to improve vaccination rates in adults <65-years-old is unknown. Two vaccines, influenza and Tdap (tetanus, diphtheria, acellular pertussis), were targeted for this age group. Cost-effectiveness of the intervention compared with control, with a primary outcome of cost per quality adjusted life year (QALY) gained, was estimated from societal and third party payer perspectives over a 10-year time horizon using a decision analysis model. Vaccination rates and intervention costs were derived from an intervention trial, and vaccine effectiveness, illness rates, and costs with/without vaccination were obtained from US databases and literature data. Future costs and effectiveness were discounted at 3%/year. The intervention cost was $1.78 per eligible patient/year. From the societal perspective, per patient total vaccination and illness costs with the intervention were $27.43 higher than control while gaining 0.00087 QALYs, costing $31,700/QALY gained. The intervention, extrapolated to the US population, could prevent 4.2 million cases, 87,489 hospitalizations, and 5,680 deaths due to influenza over 10 y in adults <65-years-old. In a probabilistic sensitivity analysis, the intervention was favored in 68.2% of model runs at a $50,000/QALY level and in 94.3% at $100,000/QALY. In a separate scenario analysis, the intervention became cost saving if influenza economic burden was >$2,099 per case (societal base case $846). Thus, the 4 Pillars Practice Transformation Program is an economically reasonable intervention to improve vaccination rates in adults <65-years-old, and could have a substantial public health impact.
Introduction
Vaccination coverage of adults younger than 65 y old is suboptimal, with vaccine uptake less than US goals. For example, the Healthy People 2020 objective for annual influenza vaccination in non-institutionalized adults less than 65 y old is 80%, Citation1 but only 33.9% of them were vaccinated during the 2015–16 influenza season Citation2 Similarly low uptake has been observed for other indicated vaccines in this age group. Citation2
The 4 Pillars™ Practice Transformation Program was developed, with the support of the Centers for Disease Control and Prevention (CDC), to facilitate vaccination rate improvements in medical practices. Citation3 The 4 Pillars Program, owned and licensed by the University of Pittsburgh, is a web-based tool offering step-by-step guidance and evidence-based strategies in 4 key domains (Pillars) to assist practices with making and maintaining changes to enhance adult vaccination. The 4 Pillars are convenient vaccination services, patient communication regarding the importance and availability of vaccination, enhanced office systems to facilitate immunization, and motivation through an office immunization champion. Citation3 , Citation4 The 4 Pillars Program has been found to be economically reasonable in persons aged ≥ 65 y. Citation5
This intervention was tested in a cluster randomized controlled trial in diverse practices in 2 US cities, finding that practices using the intervention had significant increases in adult vaccination rates compared with those without intervention. Citation3 , Citation4 , Citation6-Citation8 In this analysis, we concentrate on intervention public health effects and cost-effectiveness in general adult populations less than 65 y old, targeting influenza vaccine and the tetanus, diphtheria, and acellular pertussis (Tdap) vaccine.
Results
From a public health standpoint (), the model predicted an absolute decrease in influenza cases of 2.2% over 10 y with the program, with smaller decreases in hospitalized influenza cases and in total and hospitalized cases of pertussis. Similar small decreases were seen in deaths due to influenza and pertussis. This reduction in influenza, extrapolated to the US adult population aged <65 years, Citation9 represents a potential 4.2 million fewer influenza cases, 87,489 fewer hospitalizations and 5,680 fewer deaths from influenza over 10 y.
Table 1. Public health results of 4 Pillars™ Practice Transformation Program in Adults <65 over 10 years, expected illnesses per 10,000 cohort members.
We used quality adjusted life years (QALY) lost, the product of utility loss due to illness and the duration of that loss, as the effectiveness term in this analysis. In a cost-effectiveness analysis from the societal perspective over the 10-year model time horizon, the total per person vaccination and illness cost for the 4 Pillars Program was about $27 more than no program while gaining 0.00087 QALY (or about a third of a quality adjusted day), for an incremental cost-effectiveness ratio of $31,700 per QALY gained (). From the third-party payer perspective, the intervention cost $44,100/QALY gained.
One-way sensitivity analyses, varying parameters individually over their listed ranges (), were performed for all model parameters. From the societal perspective, individual variation of 3 parameters caused the intervention to cost >$100,000/QALY gained: 1) the program-related absolute increase in influenza vaccination 2) the yearly influenza probability, and 3) influenza vaccine effectiveness, as shown in . Results were not sensitive to individual variation of all other parameters. Thus, model results were largely driven by influenza-related parameters. If it is assumed that the intervention only increased Tdap vaccination and had no effect on influenza vaccination rates, the intervention cost >$390,000/QALY. However, when the intervention-related increase in influenza vaccine uptake returned to its base case value, 7.5%, the intervention was cost saving and more effective than no intervention if influenza total economic burden was >$2,099/case (societal base case cost $846, range $252–4,587).
Table 2. Cost effectiveness analysis results of 4 Pillars™ Practice Transformation Program in Adults <65 years over a 10-year time horizon.
Table 3. Model parameter values.
Table 4. One-way sensitivity analysis. Parameters whose variation caused the intervention to cost > $100,000/quality adjusted life year gained, societal perspective.
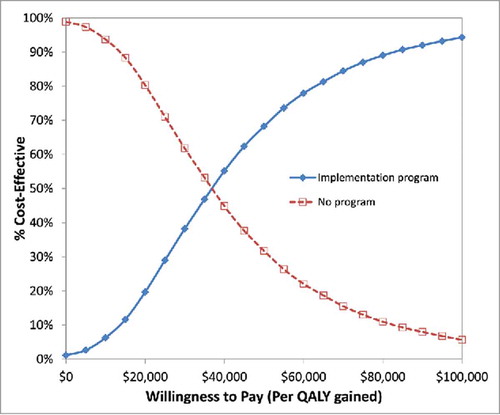
The results of a probabilistic sensitivity analysis, simultaneously varying all parameters over distributions 5000 times, are shown as an acceptability curve in . The 4 Pillars Program, from a societal perspective, was favored in 68.2% of the model iterations at a $50,000/QALY level and in 94.3% at $100,000 per QALY gained. From a third-party payer perspective, the program was favored in 50.1% at $50,000/QALY and 90.3% at a $100,000/QALY gained threshold.
Figure 1. Cost effectiveness acceptability curve, depicting probabilistic sensitivity analysis results of the 4 Pillars Practice™ Transformation Program. The y-axis shows the likelihood that a strategy will be favored over a range of willingness-to-pay (or acceptability) thresholds on the x-axis.
In a separate analysis, the intervention-related duration of increased vaccination coverage was varied from 1 y to 10 y (the base case value). If the intervention only increases vaccination for 1 year, it cost $87,300/QALY gained; 2 y of increased duration cost $53,700/QALY. These results are summarized in Figure S1.
Discussion
Adults aged <65 y have the lowest influenza vaccination rates among all age groups. Citation10 They are also least likely to suffer serious consequences of influenza infection, as morbidity and mortality from influenza are highest among the very young and the elderly. Citation11 Thus, the incentive for medical practices to invest resources in an intervention to promote vaccination among younger adults may seem less compelling. However, a favorable cost-effectiveness and public health profile for a practice-based intervention, such as the 4 Pillars Practice Transformation Program, may encourage medical practices to use the program to pursue this goal. This analysis indicates the value of implementing the 4 Pillars Program in primary care practices that serve adults. The cost-effectiveness ratio of $31,700/QALY gained from the societal perspective and $44,100/QALY gained from the third-party payer perspective are modest compared with the contemporary US benchmark acceptability threshold of $100,000/QALY gained. Citation12 From a public health standpoint, use of this program or similar programs to increase adult vaccination rates could potentially prevent millions of influenza cases and substantially decrease influenza hospitalizations and deaths.
Furthermore, sensitivity analyses confirmed the robustness of these results. With individual variation of model parameters, the intervention cost less $100,000/QALY gained unless average increases in influenza vaccination rates with the program were substantially less than observed (1.6% or less, compared with the observed 7.5%), influenza illness rates were possibly implausibly low (less than 2.2%, base case 6.6%), or influenza vaccine effectiveness was less than 23.9%. Over the past several years, influenza vaccine effectiveness has varied widely across vaccine strains and types, and from year to year. In 2014–15, influenza vaccine effectiveness was 11% against A/H3N2, the predominant circulating virus strain in a season when there was significant drift between vaccine and circulating strains. Citation13 However, influenza vaccine effectiveness has ranged in recent years from 47% in 2011–2012, Citation14 to 49% in 2012–2013, Citation15 and 54% in 2013–2014. Citation16 It is also worth noting that analysis results were not sensitive to variation of pertussis-related parameters, including intervention-related improvements in Tdap vaccination rates, which is unsurprising given the relative rarity of pertussis compared with the frequency and potential severity of influenza.
The intervention became cost-saving when the total economic burden of influenza rose above $2,099 per case. This analysis focused on the general population of adults aged <65 years, and did not specifically address those with high risk conditions conferring greater risk of costly influenza complications. With increasing rates of obesity, diabetes, and other chronic illnesses, the disease burden may rise, increasing the urgency to improve vaccine uptake among those at higher risk.
Limitations and strengths
This relatively simple model did not permit the modeling of possible indirect (or herd immunity) effects of vaccination. The direction and magnitude of the resulting bias is difficult to predict without the application of more complex transmission dynamic models. The model also had limited ability to examine year-to-year improvements or reductions in vaccination rates over the 10-year time horizon of the model and did not account for the benefits of simultaneous vaccination. One of the 4 Pillars’ strategies is to offer any indicated vaccines at the time of another, such as offering Tdap vaccine during influenza season. This strategy can be time and cost-saving for practices and may reduce the cost of the intervention, thus improving cost-effectiveness. When compared with Markov state-transition models and other more complex models, decision tree models can be limited in their ability to depict and account for recurrent events. In this analysis, we used assumptions regarding vaccination and illness characteristics to allow a simpler model to be used, a potential limitation. However, a simpler model would likely be easier for decision makers to use in their consideration of options to improve vaccination rates. One of the strengths of the study is the inclusion of implementation program costs derived from participants in the 4 Pillars trial; another is the inclusion of 2 vaccines within the model.
Conclusions
The 4 Pillars Practice Transformation Program is an economically reasonable intervention to improve vaccination rates in adults less than 65 y old that also has a potentially significant public health impact.
Methods
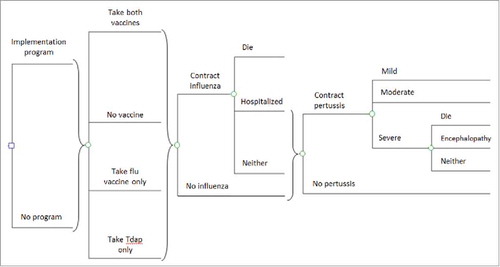
A decision tree model was used to estimate the cost-effectiveness of the 4 Pillars Program intervention compared with no intervention in adults less than 65 y of age, using TreeAge Pro 2016 software (TreeAge Software, Williamstown, MA). Vaccine uptake in adults <65 y old was calculated based on that observed in the trial, which included both adults aged <65 y and those aged ≥ 65 years, at baseline and changes in uptake post intervention. Citation6 , Citation7 Details of this calculation are shown in Table S1. US databases and medical literature data were used to estimate vaccine effectiveness and illness rates, and their associated costs. A societal perspective was taken in the base case analysis; a third-party payer analysis was also performed. Societal costs included direct medical and nonmedical costs and productivity costs. Costs from a third-party payer perspective included only direct medical costs. Citation17 Prior costs were inflated to 2015 US dollars using the Consumer Price Index. Citation18 Effectiveness was modeled as QALYs lost due to illness. The model had a 10 y time horizon and discounted future costs and effectiveness at 3% per year. The robustness of model results was examined through 1-way and probabilistic sensitivity analyses.
For this analysis, we used a relatively simple decision tree model for several reasons. Data for the analysis came not only from the 4 Pillars trial but also other sources, thus requiring some type of model to structure and synthesize that data. A fixed 10-year time horizon and an effectiveness term of QALY's lost due to illness allowed the use of a decision tree model rather than a more complex model, as did our modeling of illness as the only recurring event, facilitated by assumptions regarding constant yearly influenza rates and improvements in vaccination rates with the implementation program (see below). In addition, the logical graphical structure of a decision tree model may make presentation easier to follow for decision makers than more complex modeling structures. In the model (), identical hypothetical cohorts could receive the intervention or not, with downstream effects occurring due to differences in vaccination rates between strategies. To further simplify the model, we assumed that the probability of receiving each vaccine was not related to the probability of receiving the other vaccine; thus, the likelihood of receiving both vaccines was calculated by multiplying the likelihood of receiving each individual vaccine. Portions of the cohort could develop influenza and have health outcomes related to influenza, as well as develop pertussis and its associated outcomes, based on medical literature-based illness probabilities and vaccine effectiveness over the model's 10-year time horizon. For both infections, differences in vaccination rates between strategies resulted in differences in infection rates but did not affect case-fatality or case-hospitalization rates. Because the other components of the Tdap vaccine, tetanus and diphtheria, are so rare, they were not included in estimates of vaccine effectiveness against them in the model, potentially introducing a slight bias against the intervention. The model did not account for potential indirect (herd immunity) effects resulting from the vaccination of this age group.
The model tracked the disutility of influenza or pertussis cases, and their associated costs, occurring over a 10-year time horizon. Disutilities were modeled as QALYs lost due to these illnesses. Influenza cases could require no treatment, outpatient treatment, hospitalization, or could result in death, with disutilities, illness durations, and costs based on medical literature data. Similarly, pertussis could be mild, moderate, or severe (requiring hospitalization) and could be fatal, leading to disutilities, illness durations, and costs derived from the medical literature. The disutility of death due to either illness was calculated using an average age of adults < 65 y of age (35-years-old) and a life expectancy of 45.2 y at that age. Citation19 This value was then discounted at 3% per year, resulting in 25.52 discounted life years lost per illness-related death.
Model parameters, their base case values, and ranges examined in sensitivity analyses are shown in . A probabilistic sensitivity analysis was performed, simultaneously varying the listed parameters over distributions; β distributions were used for probabilities and utilities, and gamma distributions used for costs and disutilities. In the 4 Pillars trial, the intervention increased the absolute probability of vaccination by 7.5% for influenza vaccine and 12.9% for Tdap. The yearly influenza vaccination rate and improvements in uptake with either vaccine were modeled as constant functions, with variation in intervention-related vaccination rates modeled in sensitivity analyses, in which improvement in vaccination rates with the intervention was decreased to 0% and increased to twice the base case value to test the robustness of results. Vaccine effectiveness was 59% for influenza vaccine, assuming yearly vaccination, Citation20,Citation21 and an average of 24.5% over 10 y for Tdap protection against pertussis, based on evidence of waning pertussis protection after vaccination. Citation22 Influenza vaccine effectiveness was varied widely, reflecting observed effectiveness over the last several years. In the model, a cohort simulation was performed, thus vaccination uptake was modeled as a proportion of the population being vaccinated each year during the model's time horizon.
The 4 Pillars Program was estimated to cost $1.78 per eligible person per year, whether vaccinated or not, based on questionnaire data obtained from study sites regarding personnel and material costs to introduce and maintain the intervention. In the questionnaire, study sites were asked to estimate time spent by medical and administrative personnel to initiate and maintain the intervention and the supply costs for the intervention. Personnel time was costed based on average hourly wage estimates supplied by study sites. Total intervention costs across all study sites were divided by total patients enrolled, vaccinated or not, to derive the per eligible patient intervention cost. The range tested in sensitivity analyses ($0.70-$2.26) was based on differing cost calculation assumptions.
Disclosure of potential conflicts of interest
Drs. Zimmerman and Lin have a research grant from Sanofi Pasteur, Inc. Drs. Zimmerman, Nowalk, and Lin have research grants from Pfizer, Inc. and Merck & Co, Inc.
Supplemental_Material.docx
Download MS Word (17.2 KB)Funding
This investigation was supported by a grant (U01 IP000662) from the Centers for Disease Control and Prevention. The views expressed herein are those of the authors and not those of the Centers for Disease Control and Prevention. The project described was also supported by the National Institutes of Health through Grant Numbers UL1 RR024153 and UL1TR000005. The funding entities had no role in the identification, design, conduct, or reporting of the analysis.
References
- Healthy People 2020 . Immunization and Infectious Diseases. Objective IID-12.5. [accessed 2017 Apr 19]. https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives
- Centers for Disease Control and Prevention . National Early Season Flu Vaccination Coverage, United States , November 2015. http://www.cdc.gov/flu/fluvaxview/nifs-estimates-nov2015.htm
- Nowalk MP , Nolan BA , Nutini J , Ahmed F , Albert SM , Susick M , Zimmerman RK. Success of the 4 pillars toolkit for influenza and pneumococcal vaccination in adults. J Healthc Qual. 2014;36(6):5−15. doi:10.1111/jhq.12020. PMID:23777396
- Zimmerman RK , Nowalk MP , Lin CJ , Hannibal K , Moehling KK , Huang HH , Matambanadzo A , Troy J , Allred NJ , Gallik G , et al. Cluster randomized trial of a toolkit and early vaccine delivery to improve childhood influenza vaccination rates in primary care. Vaccine. 2014;32(29):3656−63. PMID:24793941. doi:10.1016/j.vaccine.2014.04.057
- Smith KJ , Zimmerman RK , Nowalk MP , Lin CJ . Cost-Effectiveness of the 4 Pillars Practice Transformation Program to Improve Vaccination of Adults Aged 65 and Older. J Am Geriatr Soc. 2017;65(4):763−8. doi:10.1111/jgs.14588. PMID:28024090
- Lin CJ , Nowalk MP , Pavlik VN , Brown AE , Zhang S , Raviotta JM , Moehling KK , Hawk M , Ricci EM , Middleton DB , et al. Using the 4 pillars™ practice transformation program to increase adult influenza vaccination and reduce missed opportunities in a randomized cluster trial. BMC Infect Dis. 2016;16(1):623. doi:10.1186/s12879-016-1940-1. PMID:27809793
- Nowalk MP , Lin CJ , Pavlik VN , Brown AE , Zhang S , Moehling KK , Raviotta JM , South-Paul JE , Hawk M , Ricci EM , et al. Using the 4 Pillars Practice Transformation Program to increase adult Tdap immunization in a randomized controlled cluster trial. Vaccine. 2016;34(41):5026−33. doi:10.1016/j.vaccine.2016.07.053. PMID:27576073
- Zimmerman RK , Brown AE , Pavlik VN , Moehling KK , Raviotta JM , Lin CJ , Zhang S , Hawk M , Kyle S , Patel S , et al. Using the 4 Pillars Practice Transformation Program to Increase Pneumococcal Immunizations for Older Adults: A Cluster-Randomized Trial. J Am Geriatr Soc. 2017;65(1):114−22. doi:10.1111/jgs.14451. PMID:27755655
- U.S. Census Bureau . Current Population Survey, Annual Social and Economic Supplement, 2013.
- Williams WW , Lu PJ , O'Halloran A , Kim DK , Grohskopf LA , Pilishvili T , Skoff TH , Nelson NP , Harpaz R , Markowitz LE , et al. Surveillance of Vaccination Coverage Among Adult Populations - United States, 2014. MMWR Surveill Summ. 2016;65(1):1−36. doi:10.15585/mmwr.ss6501a1. PMID:26844596
- Molinari NA , Ortega-Sanchez IR , Messonnier ML , Thompson WW , Wortley PM , Weintraub E , Bridges CB . The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086−96. doi:10.1016/j.vaccine.2007.03.046. PMID:17544181
- Neumann PJ , Cohen JT , Weinstein MC . Updating cost-effectiveness–the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796−7. doi:10.1056/NEJMp1405158. PMID:25162885
- Zimmerman RK , Nowalk MP , Chung J , Jackson ML , Jackson LA , Petrie JG , Monto AS , McLean HQ , Belongia EA , Gaglani M , et al. 2014-2015 Influenza Vaccine Effectiveness in the United States by Vaccine Type. Clin Infect Dis. 2016;63(12):1564−73. doi:10.1093/cid/ciw635. PMID:27702768
- Ohmit SE , Thompson MG , Petrie JG , Thaker SN , Jackson ML , Belongia EA , Zimmerman RK , Gaglani M , Lamerato L , Spencer SM , et al. Influenza vaccine effectiveness in the 2011-2012 season: protection against each circulating virus and the effect of prior vaccination on estimates. Clin Infect Dis. 2014;58(3):319−27. doi:10.1093/cid/cit736. PMID:24235265
- McLean HQ , Thompson MG , Sundaram ME , Kieke BA , Gaglani M , Murthy K , Piedra PA , Zimmerman RK , Nowalk MP , Raviotta JM , et al. Influenza vaccine effectiveness in the United States during 2012-2013: variable protection by age and virus type. J Infect Dis. 2015;211(10):1529−40. doi:10.1093/infdis/jiu647. PMID:25406334
- Gaglani M , Pruszynski J , Murthy K , Clipper L , Robertson A , Reis M , Chung JR , Piedra PA , Avadhanula V , Nowalk MP , et al. Influenza Vaccine Effectiveness Against 2009 Pandemic Influenza A(H1N1) Virus Differed by Vaccine Type During 2013-2014 in the United States. J Infect Dis. 2016;213(10):1546−56.
- Sanders GD , Neumann PJ , Basu A , Brock DW , Feeny D , Krahn M , Kuntz KM , Meltzer DO , Owens DK , Prosser LA , et al. Recommendations for Conduct, Methodological Practices, and Reporting of Cost-effectiveness Analyses: Second Panel on Cost-Effectiveness in Health and Medicine. JAMA. 2016;316(10):1093−103. doi:10.1001/jama.2016.12195. PMID:27623463
- US Bureau of Labor Statistics . Consumer Price Index. [accessed 2017 Apr 19]. http://www.bls.gov/cpi/home.htm
- Arias E . United States life tables, 2010. Natl Vital Stat Rep. 2014;63(7):1−63.
- Osterholm MT , Kelley NS , Sommer A , Belongia EA . Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(1):36−44. doi:10.1016/S1473-3099(11)70295-X. PMID:22032844
- Reed C , Kim IK , Singleton JA , Chaves SS , Flannery B , Finelli L , Fry A , Burns E , Gargiullo P , Jernigan D , et al. Estimated influenza illnesses and hospitalizations averted by vaccination–United States, 2013-14 influenza season. MMWR Morb Mortal Wkly Rep. 2014;63(49):1151−4. PMID:25503917
- Koepke R , Eickhoff JC , Ayele RA , Petit AB , Schauer SL , Hopfensperger DJ , Conway JH , Davis JP . Estimating the effectiveness of tetanus-diphtheria-acellular pertussis vaccine (Tdap) for preventing pertussis: evidence of rapidly waning immunity and difference in effectiveness by Tdap brand. J Infect Dis. 2014;210(6):942−53. doi:10.1093/infdis/jiu322. PMID:24903664
- Masseria C , Krishnarajah G . The estimated incidence of pertussis in people aged 50 years old in the United States, 2006-2010. BMC Infect Dis. 2015;15:534.
- McGarry LJ , Krishnarajah G , Hill G , Masseria C , Skornicki M , Pruttivarasin N , Arondekar B , Roiz J , Pelton SI , Weinstein MC . Cost-effectiveness of Tdap vaccination of adults aged >/ = 65 years in the prevention of pertussis in the US: a dynamic model of disease transmission. PLoS One. 2014;9(1):e72723. PMID:24416118. doi:10.1371/journal.pone.0072723
- CDC Vaccine Price List . Centers for Disease Control and Prevention. [accessed 2017 Apr 19]. http://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list /
- Medicare Physician Fee Schedule . [accessed 2017 Apr 19]. https://www.cms.gov/apps/physician-fee-schedule /
- Lee GM , Lebaron C , Murphy TV , Lett S , Schauer S , Lieu TA . Pertussis in adolescents and adults: should we vaccinate? Pediatrics. 2005;115(6):1675–84. doi:10.1542/peds.2004-2509. PMID:15930232
- Williams WW , Lu P-J , O'Halloran A , Bridges CB , Pilishvili T , Hales CM , Markowitz LE . Noninfluenza Vaccination Coverage Among Adults- United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(5):95–102.