ABSTRACT
Several innovations that can improve immunization systems already exist. Some interventions target service consumers within communities to raise awareness, build trust, improve understanding, remind caregivers, reward service users, and improve communication. Other interventions target health facilities to improve access and quality of vaccination services among others. Despite available empirical evidence, there is a delay in translating innovations into routine practice by immunization programmes.
Drawing on an existing implementation science framework, we propose an interactive, and multi-perspective model to improve uptake and utilization of available immunization-related innovations in the African region.
It is important to stress that our framework is by no means prescriptive. The key intention is to advocate for the entire immunization system to be viewed as an interconnected system of stakeholders, so as to foster better interaction, and proactive transfer of evidence-based innovation into policy and practice.
Introduction
Immunization has been lauded as one of the most successful public health interventions, both in terms of effectiveness and cost-effectiveness, for ensuring child survival.Citation1 According to World Health Organization (WHO), about 3 million deaths are averted yearly because of childhood immunization.Citation2 A recent study reported that the benefit in treatment cost and loss of productivity averted in the lifespan of immunized children is 16 times higher than the initial investment in immunization.Citation3 Further analysis using a full-income approach showed that every dollar invested in immunization yields an estimated return which is 44 times higher than the initial cost.Citation3 Thus indicating that immunizing a child contributes to overall national development.Citation3 To ensure universal access to vaccines for all children, the WHO, in 1974, launched the Expanded Programme on Immunization (EPI) as a framework for immunization systems globally.Citation4 To further advance equity in access, the World Health Assembly, in 2012, endorsed the Global Vaccine Action Plan (GVAP).Citation5 The GVAP, which is based on six principles, aims to prevent vaccine-preventable deaths.Citation5
Although top-level policy makers in the African region take cognizance of the broad social and economic value of immunization, many countries within the region continue to fall short on key targets in the GVAP.Citation6,Citation7 The 2017 assessment report of the GVAP revealed that the region achieved only 74% coverage level with third dose of diphtheria-tetanus-pertussis containing vaccine (DTP3), which is the lowest compared to other regions of the world.Citation6 According to recent estimates, 21 out of the 47 countries within the region have DTP3 coverage below 90%, with Equatorial Guinea, South Sudan and Nigeria reporting coverage levels as low as 35%, 45%, and 45% respectively.Citation8 In addition, disease eradication and elimination targets in the region have been set back by the appearance of new cases of paralytic poliomyelitis due to wild-type polio virus, and persistence of measles, rubella, and maternal and neonatal tetanus.Citation6 These setbacks are a result of the suboptimal performance of the immunization system in the African region resulting from factors linked to challenges with regards maintenance of the vaccine cold chain, vaccine distribution and delivery practices, and vaccine demand and uptake within countries.Citation9
Evidence based innovations
Several evidence-based innovations that can improve immunization systems already exist. In recent years, due to increasing mobile phone penetration and expansion of broadband internet access, the use of mobile health (mHealth) technology has evolved rapidly even in low- and middle-income countries.Citation10, Citation11 A mobile based application; the electronic Vaccine Intelligence Network (eVIN), which enables real-time vaccine stock tracking and cold chain temperature monitoring is currently in use, with promising results.Citation12 The success of this mHealth innovation has attracted the interest of some countries.Citation13
Other interventions to improve delivery of immunization services that target different levels of the immunization system have also been tested in some communities. Some interventions target the immunisation service consumers within communities to raise awareness, build trust, improve understanding, remind caregivers, reward service users, and improve communication. For instance, monetary incentives have been used to improve immunization coverage.Citation14 Studies have also shown that home visits and community health education are effective in improving immunization coverage rates.Citation15, Citation16 Other interventions target health systems to improve access and quality of vaccination services.Citation17
Bridging the know-do gap
Despite available evidence, there is a delay in translating innovations into routine practice by immunization programmes. Fortunately, a growing body of literature in the nascent field of implementation science on how to bridge this “know-do” gap now exist and can hasten the transfer of innovations with proven effectiveness into routine practice.Citation18 In fact, these concepts are already being applied in other health programmes to optimize service delivery.Citation19
Considering the current performance of immunization systems in the African region, it is imperative for national programmes to review current strategies and incorporate new and existing evidence-based innovations. To sustain uptake of these evidence-based innovations, country-level immunization systems would eventually need to be re-organized into knowledge translation systems that emphasize quick interaction between all stakeholders (from researchers to healthcare providers). Such systems would ensure that innovations are quickly translated into practice for the immunization systems to benefit individuals and communities in a timely manner.
Moreover, fiscal allocation to communicable disease control (including immunization) are likely to reduce in response to competing demands for funding due to the rising burden of non-communicable diseases. Thus, an efficient system is an exigent need.
A proposed model
Drawing on an existing implementation science framework, we propose an interactive, and multi-perspective model.Citation20 The proposed model (as shown in would reduce the time taken for national immunization systems to become aware of potentially valuable interventions and strategies, hasten the incorporation of these strategies into national programs, and enhance communication between all stakeholders for continuous improvement. This model leverages on already existing structures within national immunization programmes.
Figure 1. Proposed Model for timely transfer of innovation in national immunization systems in the African Region.
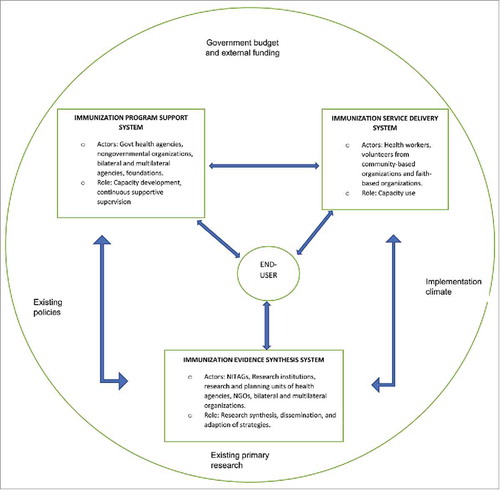
The original framework from which the model is derived combines aspects of research-to-practice and community-centered models.Citation20 It was developed by Wandersman and his colleagues out of the dire need for new approaches to addressing know-do gap.Citation20 One of the key feature of the framework is the bidirectional communication between all stakeholders to ensure that they understand each other's needs and perspectives.Citation20 The United States Center for Disease Control and Prevention (CDC) uses this framework in violence prevention program to bridge the gap between development of violence prevention strategies and application in the field.Citation21 In addition to the three categories of stakeholders (evidence synthesis, program support and service delivery) specified in the original framework, we added a fourth one; end-users, in our proposed model. This is in recognition of the value of client outcomes such as satisfaction, and implementation outcomes such as acceptability and appropriateness in informing how activities can be modified. We therefore grouped immunization stakeholders into four;
| a. | Immunization evidence synthesis system | ||||
| b. | Immunization program support system | ||||
| c. | Immunization service delivery system | ||||
| d. | Immunization service end-users | ||||
Immunization evidence synthesis system
The evidence synthesis system includes National Immunization Technical Advisory Groups (NITAGs) and other national entities with research capacity. Since NITAGS already have a formalized responsibility of providing evidence-based recommendations at national level, they should coordinate this system. Through a network of research entities, and in close collaboration with other stakeholders within the system, NITAGs should recommend strategies/innovations or packages of innovations that EPI leads can implement within their cultural and geographic context. Using program data including client and implementation indicators, this system should also recommend specific adaptation of innovations to attain best “fit” with culture, organizational climate and geographic characteristics.
Immunization program support system
The role of the immunization program support system is to build the general and specific technical capacity of immunization stakeholders in the delivery system. This is to enable proper implementation of recommended strategies with fidelity. This system can employ various kinds of facilitation strategies to meet its objectives. Stakeholders include national government agencies primarily responsible for immunization; nongovernmental, bilateral and multilateral organizations involved in immunization programming; and the National Inter-Agency Co-ordinating Committee.
Immunization service delivery system
The service delivery system would comprise the general and specific individuals and capacities required by the support system to provide quality and safe immunization services to all children, adolescents and adults that require it in a timely manner. They include health workers in hospitals and clinics, and volunteers from community and faith-based organizations among others. Example of general capacities include managerial and leadership skills, proper use of new and existing routine immunization recording and reporting tools, vaccine management among others.
Immunization service end-users
These stakeholders comprise of individual consumers of vaccines which comprise targeted individuals and communities. Their role is to provide valuable feedback that can be used for adaptation and improvement of immunization service.
Feedback loop
A key feature of this framework is the bidirectional arrows between all stakeholders. This indicates the need for information sharing and communication between stakeholder. Such communication would promote better understanding among stakeholders and encourage them to support each other's roles.
Similar to the original framework, budgetary allocation at all levels of government, external funding, routine immunization policies at national and state or provincial levels, implementation climate and availability of existing primary research are recognized factors that can affect knowledge translation and should be kept in mind at all time.
Conclusion
Bridging the know-do gap in immunization would take countries in the African Region closer to achieving immunization performance targets. It is important to stress that our framework is by no means prescriptive. The key intention is to advocate for the entire immunization system to be viewed as an interconnected system of stakeholders, so as to foster better interaction, and proactive transfer of evidence-based innovation into policy and practice in an iterative manner, using data from these stakeholders to continually adapt strategies to ensure equitable access to vaccines for all.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Additional information
Funding
References
- Ehreth J. The global value of vaccination. Vaccine. 2003;21(7):596–600. doi:10.1016/S0264-410X(02)00623-0. PMID:12531324.
- World Health Organization. Immunization 2018 [cited 2018 22nd January 2018 at 3:07pm SAST]. Available from: http://www.who.int/topics/immunization/en/.
- Ozawa S, Clark S, Portnoy A, Grewal S, Brenzel L, Walker DG. Return on investment from childhood immunization in low-and middle-income countries, 2011–20. Health Affairs. 2016;35(2):199–207. doi:10.1377/hlthaff.2015.1086. PMID:26858370.
- Keja K, Chan C, Hayden G, Henderson RH. Expanded programme on immunization. World health statistics quarterly Rapport trimestriel de statistiques sanitaires mondiales. 1987;41(2):59–63.
- World Health Organization. Global Vaccine Action Plan 2011 – 2020. Geneva: World Health Organization; 2013.
- World Health Organization. 2017 Assessment Report of the Global Vaccine Action Plan. Strategic Advisory Group of Experts on Immunization. Geneva: World Health Organization; 2017. Licence: CC BYNC-SA 3.0 IGO.
- World Health Organization and African Union Commission. The Addis Declaration on Immunization 2016.
- World Health Organization and United Nations Children's Fund. WHO/UNICEF National Immunization Coverage. 2017.
- Hadler S, Dietz V, Okwo-Bele J, Cutts F. Immunization in developing countries. Vaccines 5th ed. Philadelphia: Saunders Elsevier; 2008. p. 1541–71.
- Mechael PN. The case for mHealth in developing countries. innovations. 2009;4(1):103–18. doi:10.1162/itgg.2009.4.1.103.
- Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Globalization and health. 2006;2(1):9. doi:10.1186/1744-8603-2-9. PMID:16719925.
- United Nations Development Programme (UNDP). Improving Efficiency of Vaccination Systems in Multiple States India2015 [Available from:http://www.in.undp.org/content/dam/india/docs/GAVI-Factsheet.pdf.
- Government of India. eVIN Project of Health Ministry becomes global best practise in immunisation Delhi: Press Information Bureau; 2017 [Available from: http://pib.nic.in/newsite/PrintRelease.aspx?relid=161558.
- Barham T. The impact of the Mexican conditional cash transfer on immunization rates [Unpublished manuscript]. (CA): Department of Agriculture and Resource Economics, University of California at Berkeley; 2005.
- Brugha R, Kevany J. Maximizing immunization coverage through home visits: a controlled trial in an urban area of Ghana. Bull World Health Organ. 1996;74(5):517. PMID:9002332
- Andersson N, Cockcroft A, Ansari NM, Omer K, Baloch M, Foster AH, Shea B, Wells GA, Soberanis JL. Evidence-based discussion increases childhood vaccination uptake: a randomised cluster controlled trial of knowledge translation in Pakistan. BMC Int Health Hum Rights. 2009;9(1):S8. doi:10.1186/1472-698X-9-S1-S8. PMID:19828066.
- Wiysonge CS, Young T, Kredo T, McCaul M, Volmink J. Interventions for improving childhood vaccination coverage in low-and middle-income countries. SAMJ: South African Medical Journal. 2015;105(11):892–3. doi:10.7196/SAMJ.2015.v105i11.10177.
- Wilson PM, Petticrew M, Calnan MW, Nazareth I. Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. Implement Sci. 2010;5(1):91. doi:10.1186/1748-5908-5-91. PMID:21092164.
- Norton WE, Amico KR, Cornman DH, Fisher WA, Fisher JD. An agenda for advancing the science of implementation of evidence-based HIV prevention interventions. AIDS and Behavior. 2009;13(3):424–9. doi:10.1007/s10461-009-9556-8. PMID:19360464.
- Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, Stillman L, Blachman M, Dunville R, Saul J. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41(3–4):171–81. doi:10.1007/s10464-008-9174-z. PMID:18302018.
- Saul J, Duffy J, Noonan R, Lubell K, Wandersman A, Flaspohler P, et al. Bridging science and practice in violence prevention: Addressing ten key challenges. Am J Community Psychol. 2008;41(3–4):197–205. doi:10.1007/s10464-008-9171-2. PMID:18340524.
